Abstract
This open‐label drug–drug interaction study assessed whether blockade by dupilumab of interleukin (IL)‐4 and IL‐13 signaling affects the pharmacokinetics of drugs metabolized by cytochrome P450 (CYP450) enzymes. The pharmacokinetics of five CYP450 substrates given orally (midazolam, omeprazole, S‐warfarin, caffeine, and metoprolol, metabolized by CYP3A, CYP2C19, CYP2C9, CYP1A2, and CYP2D6, respectively) were evaluated before and 28 days after initiation of dupilumab treatment (subcutaneous 300 mg weekly) in 14 patients with moderate‐to‐severe atopic dermatitis. Dupilumab had no clinically relevant effects on the pharmacokinetics of CYP450 substrates, provided substantial clinical benefit, and was generally well tolerated. Only one serious adverse event was reported, an episode of systemic inflammatory response syndrome that resolved after treatment was discontinued. In summary, blockade of IL‐4/IL‐13 signaling in patients with type 2 inflammation does not appear to significantly affect CYP450 enzyme activities; the use of dupilumab in atopic dermatitis patients is unlikely to influence the pharmacokinetics of CYP450 substrates.
Study Highlights.
WHAT IS THE CURRENT KNOWLEDGE ON THIS TOPIC?
☑ It is not known whether the PK of drugs metabolized by CYP450 are influenced by IL‐4 and IL‐13 in patients with AD or other conditions characterized by Type 2 inflammation.
WHAT QUESTION DID THIS STUDY ADDRESS?
☑ This drug interaction study investigated whether treatment with dupilumab, which blocks the signaling of IL‐4 and IL‐13 by blocking IL‐4Rα, affects CYP450 enzyme activity in patients with moderate‐to‐severe AD.
WHAT THIS STUDY ADDS TO OUR KNOWLEDGE?
☑ Dupilumab appears to have little effect on CYP450 activity.
HOW MIGHT THIS CHANGE CLINICAL PHARMACOLOGY OR TRANSLATIONAL SCIENCE?
☑ These results suggest that dupilumab can be used in the treatment of AD without significant PK interactions with drugs metabolized by CYP3A, CYP2D6, CYP2C9, CYP2C19, or CYP1A2.
Atopic dermatitis (AD), also known as atopic eczema, is a pruritic skin condition characterized by a chronic, relapsing form of skin inflammation, a disturbance of the epidermal‐barrier function associated with immune changes in the skin, and a high prevalence of immunoglobulin E (IgE)‐mediated sensitization to food and environmental allergens.1 It is a common condition in industrialized countries, with a prevalence of 15–30% in children and 2–10% in adults; most cases develop before the age of 5 years.1, 2
Clinically, AD manifests as poorly defined erythema with edema, vesicles, and weeping in the acute stage and skin thickening (lichenification) in the chronic stage, with a predilection for skin flexures.3 Patients with moderate‐to‐severe disease experience intense pruritus and self‐inflicted skin excoriation, and can have markedly reduced quality of life, sleep disorders, anxiety, and/or depression.4, 5
Treatment consists primarily of topical treatment with corticosteroids or emollients; however, long‐term use of topical steroids increases the risk of significant adverse events (AEs).6 Systemic agents such as cyclosporine, methotrexate, azathioprine, mycophenolate mofetil, and prednisone have been used, but also have known side effects; evidence‐based guidance on their use is lacking.7
The Type 2/Th2 pathway is the predominant immune axis upregulated in AD patients. The burden of Type 2 inflammation in AD is demonstrated by high concentrations of circulating biomarkers such as serum total IgE and thymus and activation regulated chemokine (TARC, or CCL17), known to be regulated by interleukin (IL)‐4 and IL‐13. Serum lactate dehydrogenase (LDH) is also elevated in AD patients.8 Circulating TARC and LDH concentrations correlate with disease severity and response to treatment.9, 10 Thus, these markers can be used to assess AD disease status and treatment‐related disease modulation in a disease–drug interaction setting. A number of Type 2/Th2 pathway genes, including CCL17 (TARC), CCL18, and CCL26, are significantly upregulated in lesional skin of AD patients relative to nonlesional skin and controls and are suppressed with dupilumab treatment.11, 12 Furthermore, higher frequencies of circulating IL‐4 + T cells have been reported in AD, compared with controls.13
Dupilumab is a fully human monoclonal antibody against IL‐4 receptor‐α (IL‐4Rα), which inhibits signaling of IL‐4 and IL‐13, cytokines that are key drivers of atopic/allergic Type 2/Th2 immune diseases such as AD, asthma, allergic rhinitis, and food allergies.14 Dupilumab (300 mg, given every 2 weeks by subcutaneous injection) is approved by the US Food and Drug Administration and Health Canada for the treatment of adults with moderate‐to‐severe AD whose disease is not adequately controlled with topical prescription therapies or when those therapies are not advisable, and can be used with or without topical corticosteroids. Dupilumab is approved at the same dose by the European Medicines Agency for use in adults with moderate‐to‐severe AD who are candidates for systemic therapy. A clinical trial in pediatric patients with AD (NCT03054428) is currently in progress; in addition, dupilumab has shown efficacy and is in clinical development for the treatment of asthma,15, 16 chronic sinusitis with nasal polyposis,17 and eosinophilic esophagitis (NCT02379052).18 Cytochrome P450 (CYP450) isozymes are the major drug‐metabolizing enzymes in the liver. Although this class has more than 50 enzymes, six of them (CYP1A2, CYP2C9, CYP2C19, CYP2D6, CYP3A4, and CYP3A5) metabolize ∼90% of drugs.19 In vitro 20, 21 and in vivo 22, 23 studies have shown that some cytokines and cytokine modulators can influence the expression, stability, and activity of specific CYP450 enzymes, and can indirectly alter the pharmacokinetics (PK) of concomitantly administered drugs that are substrates of affected CYP450 enzymes. Liptrott et al.21 showed in vitro that the Type 2 cytokines IL‐4 and IL‐13 affected mRNA expression and increased protein expression for CYP2B6 and CYP3A4, and speculated that increases in CYP3A4 activity might explain the difference in atazanavir levels between healthy subjects and HIV‐infected patients. Overall, however, the literature evidence for effects of IL‐4 and IL‐13 on CYP450 activity is limited.
The reported concentrations of circulating IL‐4/IL‐13 are variable. In healthy individuals, IL‐4 concentrations range from nondetectable,24, 25 to 128.7 pg/mL,26 but are generally reported to be in the 3–10 pg/mL range.27, 28, 29 In AD patients concentrations of IL‐4/IL‐13 range from undetectable25, 30 to 12.9 pg/mL for IL‐1330 and 2.1–109 pg/mL for IL‐4.26, 31 These data suggest that there is considerable overlap in these cytokine concentrations between AD patients and the general population in the peripheral blood. Localized upregulation of IL‐4 and IL‐13 mRNA have been demonstrated in the inflamed skin of AD patients.32, 33 IL‐4 and IL‐13 regulate Type 2 inflammation and immune function by modulating gene expression downstream of receptor signaling. In AD patients with elevated IL‐4/IL‐13 concentrations in circulation, any cell type expressing a functional receptor has the potential for activation of the pathway, including liver cells. If IL‐4/IL‐13 down‐ or upregulate CYP450 activity, the metabolism of CYP450 enzyme substrates could be altered in these patients (disease–drug interaction).34 The frequent occurrence of multiple comorbid Type 2 diseases, such as comorbid asthma and AD, suggests systemic inflammation is likely present in atopic patients. Blockade of IL‐4/IL‐13 signaling by an IL‐4Rα antagonist such as dupilumab would be expected to dampen systemic inflammation and reverse any modulatory effect of IL‐4/IL‐13 on CYP450 activity in patients with AD (disease drug–drug interaction (disease‐DDI)), if the Type 2 cytokines regulate the enzymes.34
The primary objective of the present study was to investigate the effect of dupilumab (300 mg subcutaneous (SC) weekly) on the PK of a cocktail of CYP450 substrates.35 Patients with moderate‐to‐severe AD received single doses of midazolam (primarily metabolized by CYP3A), omeprazole (CYP2C19), S‐warfarin (CYP2C9), caffeine (CYP1A2), and metoprolol (CYP2D6) before and 4 weeks after initiation of weekly dupilumab treatment. A secondary objective of the study was to evaluate the safety and tolerability of repeated dosing with dupilumab in this patient population. The study used a dupilumab regimen (300 mg weekly) that is expected to have a maximal immunomodulatory effect on inflammation. In addition, data on the clinical condition of the skin, and on serum biomarkers of inflammation (TARC and lactate dehydrogenase (LDH)), were collected to verify changes in disease status and inhibition of Type 2 immune function.
RESULTS
A total of 30 patients were screened: four were excluded because they were poor metabolizers of CYP2C9, CYP2C19, or CYP2D6; 12 were excluded for other reasons (history of smoking/alcohol/drug abuse within previous 2 years, n = 4; unwillingness to comply with study procedures, n = 4; baseline and screening EASI score <16, n = 2; medical or psychological conditions presenting potential risk to participant, n = 2). Of the 14 patients enrolled, 13 completed the study; one patient withdrew after experiencing a systemic inflammatory response syndrome (SIRS) event on Day 23, 8 days after the second injection of dupilumab (see below).
Baseline demographic characteristics and disease history of the enrolled patients are summarized in Table 1 . Genotyping data on metabolizer status were available for CYP2C19, CYP2C9, and CYP2D6. Overall, six patients (42.9%) were ultrametabolizers of CYP2C19, and four each (28.6%) were extensive or intermediate metabolizers. For both CYP2C9 and CYP2D6, 13 patients (92.9%) were extensive metabolizers and one (7.1%) was an intermediate metabolizer (Supplementary Table S1).
Table 1.
Baseline demographic characteristics and disease history
| N | 14 |
|---|---|
| Gender (m/f), n/n (%/%) | 7/7 (50/50) |
| Age (years), mean (SD) | 38.3 (13.2) |
| Race, n (%) | |
| White | 8 (57.1) |
| Black or African American | 4 (28.6) |
| Asian | 1 (7.1) |
| Not reported | 1 (7.1) |
| Height (cm), mean (SD) | 168.6 (9.9) |
| Weight (kg), mean (SD) | 79.1 (20.9) |
| Body mass index (kg/m2), mean (SD) | 27.8 (7.2) |
| Baseline EASI, total score, mean (SD) | 29.2 (14.2) |
| Baseline IGA | 3.4 (0.5) |
| Baseline IGA, n (%) | |
| 3 (moderate disease) | 9 (64.3) |
| 4 (severe disease) | 5 (35.7) |
| BSA of AD, mean (SD) | 43.6 (25.7) |
AD, atopic dermatitis; BSA, body surface area; EASI, Eczema Area Severity Index; IGA, Investigator's Global Assessment; SD, standard deviation.
Dupilumab efficacy
The mean EASI score decreased markedly from baseline with dupilumab therapy (Figure 1). Improvement was apparent 2 weeks after the first dose of dupilumab. Mean improvement in EASI score from baseline was 59.2% at Day 35 and 87.1% at Day 50. A 50%, 75%, and 90% reduction in EASI score from baseline to Day 50 was achieved in 13 patients (92.9%), 11 patients (78.6%), and 7 patients (50%), respectively.
Figure 1.
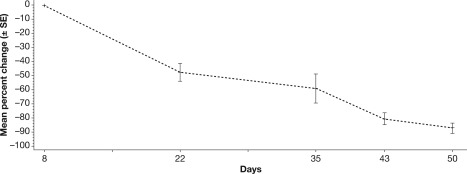
Mean (SE) percent change in EASI scores following initiation of dupilumab treatment. EASI, Eczema Area and Severity Index.
Seven patients (50%) had IGA scores of 0 or 1 (indicating clearing/almost clearing of lesions) at study Day 50 (Day 42 of dupilumab treatment). The mean BSA affected by AD decreased from baseline by 37.4% at Day 35 and 74.8% at Day 50. Dupilumab efficacy results are summarized in Table 2.
Table 2.
Overview of efficacy results
| Day 22 | Day 35 | Day 43 | Day 50 | |
|---|---|---|---|---|
| Percent change in EASI from baseline, mean ± SD | −47.46 ± 22.775 | −59.26 ± 37.646 | −80.78 ± 15.076 | −87.15 ± 13.396 |
| Patients achieving EASI‐50, n (%) | 7 (50.0) | 11 (78.6) | 13 (92.9) | 13 (92.9) |
| Patients achieving EASI‐75, n (%) | 0 | 6 (42.9) | 10 (71.4) | 11 (78.6) |
| Patients achieving EASI‐90, n (%) | 0 | 1 (7.1) | 5 (35.7) | 7 (50.0) |
| Patients achieving IGA 0 or 1, n (%) | 0 | 1 (7.1) | 4 (28.6) | 7 (50.0) |
| Percent change in AD affected body surface area from baseline, mean ± SD | −25.91 ± 29.182 | −37.40 ± 52.202 | −62.67 ± 23.553 | −74.82 ± 24.170 |
Results were based on all observed values. N = 13 for all measurements except for Day 35 (n = 14). AD, atopic dermatitis; EASI, Eczema Area and Severity Index; EASI‐50, ≥ 50% reduction in EASI from baseline; EASI‐75, ≥ 75% reduction in EASI from baseline; EASI‐90, ≥ 90% reduction in EASI from baseline; IGA, Investigator's Global Assessment; SD, standard deviation.
Dupilumab pharmacodynamics
At baseline, mean (standard deviation (SD)) serum concentrations of TARC and LDH were 8,060 (17,200) pg/mL and 253 (127) IU/L, respectively. Concentrations decreased to 1,180 (1,180) pg/mL and 216 (79) IU/L, respectively, at Day 22 and 667 (402) pg/mL and 189 (53) IU/L, respectively, at Day 35. This corresponded to median reductions in TARC and LDH levels of 64% and 20%, respectively, from baseline to Day 35, 28 days after the first dose of dupilumab (Figure 2).
Figure 2.
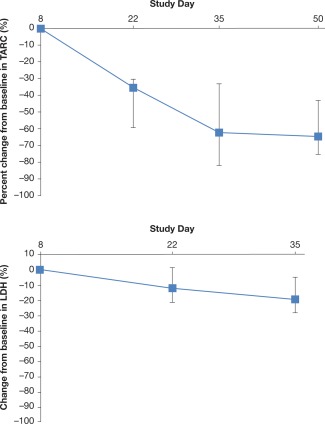
Median percent change from baseline (Q1–Q3 range) in serum concentrations of (a) TARC and (b) LDH. LDH, lactate dehydrogenase; TARC, thymus and activation regulated chemokine. [Color figure can be viewed at http://wileyonlinelibrary.com]
Exposure to functional dupilumab
The median functional dupilumab concentration was: 54.7 mg/L (range 18.7–87.4 mg/L) on Day 15; 74.0 mg/L (range 25.8–130 mg/L) on Day 22; 99.8 mg/L (range 2.7–151 mg/L) on Day 29; 93.1 mg/L (range 4.1–161 mg/L) on Day 35, and 134 mg/L (range 7.6–190 mg/L) on Day 50.
Safety and tolerability
Five AEs (fatigue, systemic inflammatory response syndrome, breast mass, toothache, and AD) were reported by three patients during the course of the study. One female patient experienced a serious AE (SAE), an episode of SIRS, 8 days after she received the second dose of dupilumab. The patient was hospitalized and treated with intravenous antibiotics and oral corticosteroids. The patient subsequently recovered completely; however, she was withdrawn from the study. This event was considered to be treatment‐related. All other AEs were mild or moderate in severity. Two patients exhibited a treatment‐emergent antidrug antibodies (ADA) response. A sensitivity analysis was performed, excluding patients with samples that were positive in the ADA assay; the results were very similar to the primary statistical analysis (data not shown), suggesting that the presence of ADA did not influence the estimated effects of dupilumab treatment on the PK of the cocktail.
Pharmacokinetics of CYP450 substrates
The PK parameters (peak plasma concentration (Cmax), AUClast, AUCinf, time to Cmax (Tmax), and observed terminal phase half‐life (t½)) for the five CYP450 substrates given with or without dupilumab are listed in Table S2. The geometric mean ratios of Cmax (with/without dupilumab) and of the area under the plasma concentration–time curve (AUC) extrapolated to the time of last positive concentration (AUClast) for the five CYP450 substrates when given with or without dupilumab are summarized in Table 3; plasma concentration–time profiles are shown in Figure 3. For all analytes the observed geometric means for both Cmax and AUClast were similar before and after dupilumab administration. There was no meaningful effect (defined as a greater than 2‐fold increase in AUClast observed geometric means, based on the point estimates/90% CI for the geometric mean ratios on each analyte) of dupilumab treatment on the metabolism of these analytes (as measured by PK properties), and therefore no evidence for a meaningful influence of dupilumab treatment on CYP3A, CYP2C19, CYP2C9, CYP1A2, and CYP2D6 activity. The largest observed effect was a geometric mean ratio for metoprolol AUClast (with/without dupilumab) of 1.29 (90% CI 1.10–1.51), which was judged not to be of clinical relevance for CYP2D6 substrates.
Table 3.
Geometric mean pharmacokinetic parameters of CYP450 substrates alone and in the presence of dupilumab
| Substrate | Parameter | Study period 1 (cocktail only) | Study period 2 (cocktail + dupilumab) | Geometric mean ratio (Day 36/Day 1) | 90% CI |
|---|---|---|---|---|---|
| Midazolam | Cmax (ng/mL) | 6.50 | 7.54 | 1.13 | 0.93–1.36 |
| AUClast (h*ng/mL) | 16.9 | 17.1 | 0.98 | 0.87–1.09 | |
| Omeprazole | Cmax (ng/mL) | 218 | 204 | 0.98 | 0.83–1.15 |
| AUClast (h*ng/mL) | 455 | 433 | 1.00 | 0.88–1.12 | |
| S‐warfarin | Cmax (ng/mL) | 700 | 662 | 0.96 | 0.83–1.11 |
| AUClast (h*ng/mL) | 20,100 | 18,000 | 0.90 | 0.83–0.98 | |
| Caffeine | Cmax (ng/mL) | 2,190 | 2,300 | 1.05 | 0.95–1.17 |
| AUClast (h*ng/mL) | 17,200 | 19,600 | 1.12 | 0.87–1.45 | |
| Metoprolol | Cmax (ng/mL) | 101 | 117 | 1.22 | 1.05–1.41 |
| AUClast (h*ng/mL) | 615 | 769 | 1.29 | 1.10–1.51 |
N = 13 for all measurements except for caffeine (one patient had significant concentrations of caffeine in plasma prior to administration of the CYP substrate cocktail in both study periods and was thus excluded for the analysis of caffeine).
AUClast, area under concentration‐time curve to last measurable concentration; CI, confidence interval; Cmax, peak plasma concentration.
Figure 3.
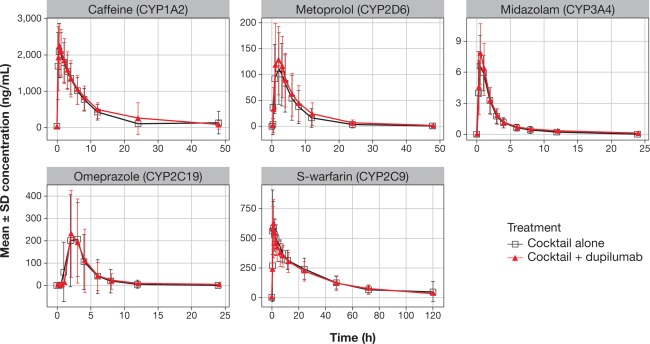
Concentration–time curves for the five CYP substrates in plasma before and after dupilumab treatment. Data presented as mean (±SD). SD, standard deviation.
DISCUSSION
The current DDI study is the first to explore potential shifts in CYP450‐mediated metabolism after treatment with a biological drug modulating IL‐4/IL‐13 signaling through the IL4Rα pathway. Indeed, formal DDI evaluations for other biologic agents targeting Type 2 cytokines have not been reported for patients with atopic disease. The current study investigated the effect of dupilumab 300 mg weekly on the PK of CYP450 probe substrates in patients with moderate‐to‐severe AD and found no clinically relevant effect on CYP3A, CYP2C19, CYP2C9, CYP1A2, or CYP2D6. Prior to this study, it was not clear whether antagonism of IL‐4 and IL‐13 activity or suppression of atopic inflammation might influence CYP activities and hence drug disposition. We now demonstrate that CYP enzyme activities in vivo do not shift during blockade of IL‐4α receptors, despite a marked suppression of inflammation (based on skin condition scores and serum LDH) and inhibition of IL‐4/IL‐13‐dependent pathways (as indicated by suppression of serum TARC).
The CYP450 isoforms evaluated in this study (CYP3A, CYP2C19, CYP2C9, CYP1A2, and CYP2D6) are predominantly responsible for the metabolism of most small‐molecule drugs, and the doses of probe substrates given are commonly used in drug interaction studies.35 Using these substrates,35, 36 dupilumab treatment was shown to have little or no effect on CYP enzyme activities. The results therefore suggest that dupilumab should have little effect on the activity of most medications likely to be encountered concomitantly in clinical practice.
Previous drug interaction studies have shown that certain cytokines and cytokine modulators can significantly influence the expression, stability, and activity of specific CYP450 enzymes, and can indirectly alter the PK of concomitantly administered drugs that are substrates of the affected CYP450 enzymes.20, 21, 22, 23 For example, IL‐6 causes a reduction in mRNA for CYP3A4, and to a lesser extent for CYP1A2, CYP3A, CYP2C19, CYP2C9, CYP1A2, and CYP2D6 in human hepatocyte cultures; coincubation with the IL‐6R antagonist tocilizumab prevents those changes.37 In rheumatoid arthritis (RA) patients, intravenous infusion of tocilizumab (IL‐6 receptor blocker) was associated with a significant decrease in systemic exposure to orally administered simvastatin, a CYP3A4 substrate.22 Similar decreases in simvastatin exposure were reported after subcutaneous administration of sarilumab (IL‐6 receptor blocker) in patients with RA.38 Consistent with these observations, a drug interaction study in which an oral cocktail of CYP probe substrates was administered to RA patients before and then after subcutaneous injection of sirukumab, an antibody that directly binds IL‐6, showed diminished exposures to midazolam, omeprazole, and S‐warfarin after sirukumab administration, providing evidence that antagonism of IL‐6 during treatment of RA reverses IL‐6‐induced suppression of not only CYP3A4 activity but also that of CYP2C19 and CYP2C9.39 An effect on CYPs that metabolize anticoagulants is suggested by observed cases of thrombosis in anticoagulated patients treated with tocilizumab.40 Such drug–disease interactions appear to have some specificity for the targeted cytokine and disease and do not consistently shift drug metabolism in the same direction. Brodalumab, an antibody targeting IL‐17R, increased exposure to midazolam by 24% in patients with plaque psoriasis following a single SC dose of brodalumab.41 In contrast, no interaction was seen in a study of postmenopausal women with osteoporosis between denosumab (binds to RANKL) and midazolam,42 and no interaction in patients with multiple sclerosis was seen for daclizumab (IL‐2 receptor blocker) with a cocktail of CYP substrates.43
An effect of IL‐4 and IL‐13 on local CYP activities in inflamed skin cannot be ruled out, in that the orally administered probe substrates used in this study are likely primarily eliminated by hepatic metabolism. In general, Type 2 inflammation during atopic disease does not directly involve the liver, and the reported concentrations of circulating IL‐4 and IL‐13 in atopic diseases are only modestly elevated, even during more severe inflammation, with considerable overlap in these cytokine concentrations between AD patients and the general population.25, 26, 27, 28, 29, 30, 31 Elevation of C‐reactive protein (CRP), an acute phase protein produced in the liver and primarily regulated by IL‐6,44 has been reported in some patients with AD.45 This suggests some degree of influence of Type 2 inflammation on liver metabolism. However, this contrasts with RA, in which there is a marked elevation of circulating plasma IL‐6,46 an associated increase in CRP, and an apparent suppression of CYP activities, in particular CYP3A4, that is reversed by parenteral IL‐6 antagonists.
Although DDI studies are often conducted in healthy volunteers, this study enrolled patients with moderate‐to‐severe AD. Patients with moderate‐to‐severe disease would be expected to have the most pronounced inflammation, and thus the greatest potential for cytokine effects on CYP450 activity.34 The within‐subject design was expected to minimize confounding due to interpatient variability in baseline CYP450 enzyme activity, as each patient served as their own control. An open‐label design was deemed acceptable because the primary endpoint was a PK assessment based on the activity of CYP450 enzymes (the variability of which was accounted for by the within‐subject design).
The interval between first dupilumab administration and second cocktail dosing (28 days) was chosen because it was anticipated that if IL‐4 or IL‐13 modulated the expression of CYP450 enzymes there would be a time lag between IL‐4Rα inhibition and changes in CYP450 enzyme activities. The choice of dupilumab dose for this study was based on data from prior studies in patients with AD and expected to achieve and maintain target saturation for a reasonable period of time before the second administration of CYP450 substrates. Notably, the dose regimen used in this study (600 mg loading dose followed by 300 mg weekly) was higher than that now approved in the US/Canada/EU for patients with AD (600 mg loading dose followed by 300 mg every 2 weeks). The hypothetical mechanism of an interaction between dupilumab and CYP450 substrates was based on reduction of inflammation that might modulate enzyme activities; evidence of marked reduction in inflammation at the time of the second administration of CYP450 substrates indicates that the duration of dupilumab treatment in this study was sufficiently long to have observed any potential interaction.
The minimal effect of dupilumab on the PK of the CYP450 substrates in AD patients suggests that signaling by IL‐4 or IL‐13 does not influence the activity of CYP450 enzymes. This is further supported by the similar PK parameters for the probe substrates observed in these AD patients with historical data in healthy subjects.35 IL‐4 and IL‐13 are also involved in other atopic diseases such as asthma, where these cytokines play a pivotal role in sustaining inflammation.14, 47, 48 The applicability of the findings of this study to other atopic diseases may be reasonable, since the magnitude of the Type 2 inflammatory burden appears to be greater in AD than in other atopic diseases. For example, circulating levels of Type 2 biomarkers, such as TARC and IgE, are substantially higher in AD patients than in those with asthma.14, 16, 49
Dupilumab was well tolerated in this study with weekly SC administration at 300 mg; only one SAE, an episode of SIRS, was reported (considered treatment‐related due to the immunomodulatory effects of dupilumab). No other new safety signals emerged during the study. A marked improvement in AD severity (measured by change in EASI score from baseline) was observed at Day 35 and Day 50 (mean reductions of 59.3% and 87.2%, respectively). In addition, marked reductions in circulating TARC and LDH concentrations indicate significant reductions in inflammation with dupilumab treatment. Efficacy data appear similar to those seen in previous studies, in which dupilumab provided substantial clinical benefit to participants as measured by a change in EASI, the proportion of patients achieving EASI 50/75, and the proportion of patients achieving IGA 0/1 at Week 4 and Week 6 after the start of dupilumab dosing. However, safety and efficacy findings from the current study should be interpreted with caution given the study design limitations, including the small number of patients, lack of a control arm, and concomitant use of a nonstandardized regimen of topical corticosteroids.
In conclusion, this study showed no meaningful effects of dupilumab on the PK of the CYP450 substrates, suggesting that IL‐4/IL‐13 signaling has no significant effect on the activity of CYP3A4, CYP2C19, CYP2C9, CYP1A2, or CYP2D6.
METHODS
Study design
This was an open‐label, single‐sequence, phase I DDI study (http://ClinicalTrials.gov identifier NCT02647086) conducted at four sites in the US; two additional sites were selected for participation but did not recruit patients. The study design is shown in Figure 4. The study was conducted in accordance with the ethical principles of the Declaration of Helsinki, and the protocol approved prior to initiation of the study by an Institutional Review Board as described in the International Council for Harmonisation guidelines for Good Clinical Practice. Written informed consent was obtained from all participants prior to enrolment.
Figure 4.
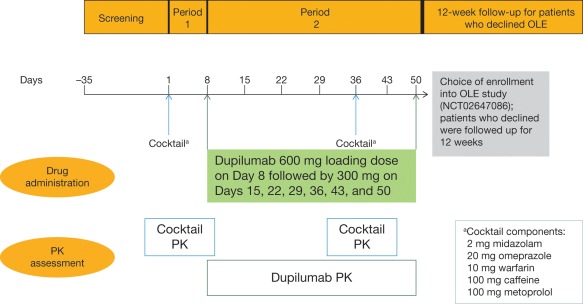
Study design. OLE, open‐label extension; PK, pharmacokinetic.
Patients
Eligible patients were adults (aged ≥18 years) who had moderate‐to‐severe AD that was inadequately controlled with topical medications or for whom topical therapy was considered inadvisable. Key inclusion criteria were chronic AD present for ≥3 years before screening; Eczema Area and Severity Index (EASI) score ≥16; Investigator's Global Assessment (IGA) score of ≥3; AD involvement of ≥10% body surface area (BSA); and inadequate response to topical therapy within the last 6 months or reasons to consider topical therapy inadvisable. Patients were excluded if they had had treatment with systemic corticosteroids, immunosuppressive/immunomodulating therapy, or phototherapy for AD within the last 4 weeks; treatment with rituximab within the last 6 months, or other biological therapies within the longer of 16 weeks or five half‐lives; administration of known inhibitors or inducers of CYP3A, CYP2C19, CYP2C9, CYP2D6, or CYP1A2 within five times the elimination half‐life or 14 days prior to baseline, whichever was longer; administration of any of the components of the cocktail of CYP450 substrates (midazolam, omeprazole, warfarin, caffeine, metoprolol) within five times the elimination half‐life or 14 days prior to baseline, whichever was longer; or consumption of grapefruit/grapefruit juice, apple/apple juice, orange/orange juice, lemons/lemon juice, limes/lime juice, vegetables from the mustard green family (e.g., broccoli), charbroiled meats, or caffeinated beverages/foods/drugs prior to baseline. Patients were also excluded if they were poor metabolizers of CYP2C9, CYP2C19, or CYP2D6 (based on genotype), or had a history of alcohol abuse, drug abuse, or smoking within the last 2 years. Female patients were excluded if they were pregnant, breastfeeding, or planning to become pregnant or breastfeed during the study; unwilling to use adequate birth control if of reproductive potential and sexually active; or using any form of hormonal contraceptives.
Procedures
On Days 1 and 36, each participant received single oral doses of each of the following CYP450 substrates after a fast of at least 8 hours: midazolam 2 mg (2 mg/mL syrup), omeprazole 20 mg (capsule), S‐warfarin 10 mg (tablet), caffeine 100 mg (20 mg/mL oral solution of caffeine citrate), and metoprolol 100 mg (tablet). No food was permitted for 2 hours after dosing. On Day 8, participants received a loading dose of 600 mg dupilumab followed by 300 mg weekly on Days 15, 22, 29, 36, 43, and 50. Dupilumab was given by SC injection; the injection site (abdomen, upper thigh, or upper arm) was alternated so that injections were not given at the same site on 2 consecutive weeks. The first dupilumab dose was administered by study site staff; subsequently, dupilumab was administered at home by the patient, unless dosing coincided with a clinic visit.
Concomitant treatment with systemic corticosteroids, systemic nonsteroidal immunomodulators, or known inhibitors/inducers of the CYP450 enzymes listed above was not permitted during the study. The consumption of certain food items and beverages (grapefruit/grapefruit juice, apple/apple juice, orange/orange juice, lemons/lemon juice, limes/lime juice, vegetables from the mustard green family, charbroiled meats, caffeinated beverages/foods/drugs) was prohibited during 7‐day periods before and after administration of cocktail substrates. Administration of any of the cocktail components (midazolam, omeprazole, warfarin, caffeine, and metoprolol) was only allowed as a single dose on Days 1 and 36 during the study. The consumption of alcohol and smoking was prohibited through the duration of the study. The use of topical medications for AD (e.g., topical corticosteroids, topical calcineurin inhibitors, and emollients) was permitted. Rescue treatment for AD could be given if the investigator considered it medically necessary.
Blood samples were taken for measurement of CYP450 substrates at various times over 3 days after each dose of the cocktail for measurement of midazolam, omeprazole, caffeine, and metoprolol, and over 15 days for S‐warfarin. These analytes were measured by validated high‐performance liquid chromatography (HPLC) assays with tandem mass spectrometry. The lower limits of quantitation for the analytes were 0.100 ng/mL for midazolam, 1.00 ng/mL for omeprazole, 5.00 ng/mL for S‐warfarin, 25.0 ng/mL for caffeine, and 0.200 ng/mL for metoprolol (data on file). PK parameters assessed included AUC extrapolated to infinity (AUCinf), AUClast, Cmax, Tmax, and t½. Values for Cmax and Tmax were derived from concentration vs. time profiles. AUClast was calculated by means of the linear trapezoidal rule. AUCinf was AUC from time zero extrapolated to infinity.
PK parameters were calculated using Phoenix WinNonLin 6.4 software (Certera, Princeton, NJ).
Efficacy of dupilumab was assessed by measuring EASI, IGA, and BSA affected by AD. EASI is a composite score ranging from 0 to 72.50 Each of four disease characteristics (erythema, thickness, scratching, and lichenification) were rated on a scale ranging from 0 (absent) to 3 (severe); the area of AD involvement is expressed on a 0–6 scale for the head, trunk, upper limbs, and lower limbs. IGA assesses the severity of AD and response to treatment on a 5‐point scale ranging from 0 (clear) to 4 (severe). BSA affected by AD was assessed for each section of the body and expressed as a percentage of all major body sections combined; the highest possible scores for each area ranged from 36% for lower limbs to 1% for genitals.
Serum functional dupilumab was analyzed using a validated enzyme‐linked immunosorbent assay (ELISA). In this functional assay, dupilumab was used as the assay standard and human IL‐4Rα served as the capture reagent. Concentrations of dupilumab with either one or two available binding sites were measured (functional drug). The assay does not detect dupilumab when both binding sites are occupied by sIL‐4Rα (soluble form) or when at least one site is bound to mIL‐4Rα (membrane‐bound form). The lower limit of quantitation of functional dupilumab is 0.0780 mg/L in undiluted human serum.
Dupilumab's pharmacodynamics were assessed by measuring serum concentrations of TARC and LDH. TARC was measured by a commercial ELISA (R&D Systems, Minneapolis, MN). LDH was measured by Roche Cobas c502 or C702 chemical analyzers (Roche Diagnostics, Indianapolis, IN).
Safety and tolerability were assessed by monitoring of AEs throughout the study, and by laboratory investigations, electrocardiograms, physical examination, and measurement of vital signs at various times during the study.
At Day 50, all patients were offered the opportunity to enroll into an open‐label extension study (http://ClinicalTrials.gov identifier NCT01949311).
Study endpoints
The primary endpoint was the ratio of geometric means of AUClast and Cmax for CYP450 substrates pre‐dupilumab administration at baseline (Day 1) and 4 weeks after initiating a weekly dupilumab regimen (Day 36). The secondary endpoint was the incidence of AEs from first dupilumab administration (Day 8) to end of study.
Statistical analysis
The PK analysis set included all patients who received dupilumab and had at least one result for CYP450 substrate concentrations on Days 1 and 36. Descriptive statistics were used for PK parameters of each of the CYP450 substrates. Log‐transformed values of Cmax and AUClast for each of the five CYP450 substrates were analyzed using a linear mixed‐effects model with treatment (substrate alone or coadministered with dupilumab) as a fixed factor and patient as a random factor. Point estimates of the Day 1/36 ratio (with corresponding 90% confidence interval (CI)) were back‐transformed to yield the geometric mean ratio and 90% CI for each substrate.
Efficacy and safety analyses were performed on the safety analysis set, which included all patients who received at least one dose of dupilumab. Efficacy measurements such as EASI, IGA, and percent involvement of BSA, and key safety parameters such as incidence of AEs and SAEs, were summarized using descriptive statistics.
FUNDING
Research sponsored by Sanofi and Regeneron Pharmaceuticals, Inc. http://ClinicalTrials.gov Identifier: NCT02647086. Editorial assistance provided by Mihai Surducan, PhD, and Ronald van Olffen, PhD, of Excerpta Medica, funded by Sanofi Genzyme and Regeneron Pharmaceuticals, Inc.
CONFLICT OF INTEREST
J.D.D., A.B., B.A., J.H., and A.T.DiC. are employees and shareholders of Regeneron Pharmaceuticals, Inc. D.H. is an investigator for Regeneron Pharmaceuticals, Inc. M.L., Z.L., and B.S. are employees of and may hold stocks and/or stock options in Sanofi.
AUTHOR CONTRIBUTIONS
J.D.D., A.B., D.H., B.A., M.L., Z.L., B.S., J.H., and A.T.DiC wrote the article; J.D.D., A.B., M.L., Z.L., B.S., J.H., and A.T.DiC designed the research; J.D.D. and D.H. performed the research; J.D.D., A.B., B.A., M.L., Z.L., B.S., J.H., and A.T.DiC analyzed the data.
Supporting information
Table S1. Summary of metabolizer status for patients included in the trial
Table S2. Summary of pharmacokinetic parameters for the CYP probe substrates
References
- 1. Bieber, T. Atopic dermatitis. N. Engl. J. Med. 358, 1483–1494 (2008). [DOI] [PubMed] [Google Scholar]
- 2. Silverberg, J.I. & Hanifin, J.M. Adult eczema prevalence and associations with asthma and other health and demographic factors: a US population‐based study. J. Allergy Clin. Immunol. 132, 1132–1138 (2013). [DOI] [PubMed] [Google Scholar]
- 3. Williams, H.C. Clinical practice. Atopic dermatitis. N. Engl. J. Med. 352, 2314–2324 (2005). [DOI] [PubMed] [Google Scholar]
- 4. Silverberg, J.I. et al Sleep disturbances in adults with eczema are associated with impaired overall health: a US population‐based study. J. Invest. Dermatol. 135, 56–66 (2015). [DOI] [PubMed] [Google Scholar]
- 5. Simpson, E.L. et al Patient burden of moderate to severe atopic dermatitis (AD): insights from a phase 2b clinical trial of dupilumab in adults. J. Am. Acad. Dermatol. 74, 491–498 (2016). [DOI] [PubMed] [Google Scholar]
- 6. Eichenfield, L.F. et al Guidelines of care for the management of atopic dermatitis: section 2. Management and treatment of atopic dermatitis with topical therapies. J. Am. Acad. Dermatol. 71, 116–132 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Sidbury, R. et al Guidelines of care for the management of atopic dermatitis: section 3. Management and treatment with phototherapy and systemic agents. J. Am. Acad. Dermatol. 71, 327–349 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Kou, K. et al Association of serum interleukin‐18 and other biomarkers with disease severity in adults with atopic dermatitis. Arch Dermatol Res. 304, 305–312 (2012). [DOI] [PubMed] [Google Scholar]
- 9. Kakinuma, T. et al Thymus and activation‐regulated chemokine in atopic dermatitis: serum thymus and activation‐regulated chemokine level is closely related with disease activity. J. Allergy Clin. Immunol. 107, 535–541 (2001). [DOI] [PubMed] [Google Scholar]
- 10. Hijnen, D. et al Serum thymus and activation‐regulated chemokine (TARC) and cutaneous T cell‐attracting chemokine (CTACK) levels in allergic diseases: TARC and CTACK are disease‐specific markers for atopic dermatitis. J. Allergy Clin. Immunol. 113, 334–340 (2004). [DOI] [PubMed] [Google Scholar]
- 11. Gittler, J.K. et al Progressive activation of T(H)2/T(H)22 cytokines and selective epidermal proteins characterizes acute and chronic atopic dermatitis. J. Allergy Clin. Immunol. 130, 1344–1354 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Hamilton, J.D. et al Dupilumab improves the molecular signature in skin of patients with moderate‐to‐severe atopic dermatitis. J. Allergy Clin. Immunol. 134, 1293–1300 (2014). [DOI] [PubMed] [Google Scholar]
- 13. La Grutta, S. et al CD4(+)IL‐13(+) cells in peripheral blood well correlates with the severity of atopic dermatitis in children. Allergy 60, 391–395 (2005). [DOI] [PubMed] [Google Scholar]
- 14. Gandhi, N. , Pirozzi, G. & Graham, N.M.H. Commonality of the IL‐4/IL‐13 pathway in atopic diseases. Expert Rev. Clin. Immunol. 13, 425–437 (2017). [DOI] [PubMed] [Google Scholar]
- 15. Wenzel, S. et al Dupilumab efficacy and safety in adults with uncontrolled persistent asthma despite use of medium‐to‐high‐dose inhaled corticosteroids plus a long‐acting β2 agonist: a randomised double‐blind placebo‐controlled pivotal phase 2b dose‐ranging trial. Lancet 388, 31–44 (2016). [DOI] [PubMed] [Google Scholar]
- 16. Wenzel, S. et al Dupilumab in persistent asthma with elevated eosinophil levels. N. Engl. J. Med. 368, 2455–2466 (2013). [DOI] [PubMed] [Google Scholar]
- 17. Bachert, C. et al Effect of subcutaneous dupilumab on nasal polyp burden in patients with chronic sinusitis and nasal polyposis: a randomized clinical trial. JAMA 315, 469–479 (2016). [DOI] [PubMed] [Google Scholar]
- 18. Hirano, I. et al Dupilumab efficacy and safety in adult patients with active eosinophilic esophagitis: a randomized double‐blind placebo‐controlled phase 2 trial. World Congress of Gastroenterology/American College of Gastroenterology Conference (Oct. 2017).
- 19. Lynch, T. & Price, A. The effect of cytochrome P450 metabolism on drug response, interactions, and adverse effects. Am. Fam. Physician. 76, 391–396 (2007). [PubMed] [Google Scholar]
- 20. Abdel‐Razzak, Z. et al Cytokines down‐regulate expression of major cytochrome P‐450 enzymes in adult human hepatocytes in primary culture. Mol. Pharmacol. 44, 707–715 (1993). [PubMed] [Google Scholar]
- 21. Liptrott, N.J. et al The impact of cytokines on the expression of drug transporters, cytochrome P450 enzymes and chemokine receptors in human PBMC. Br. J. Pharmacol. 156, 497–508 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Schmitt, C. et al Disease‐drug‐drug interaction involving tocilizumab and simvastatin in patients with rheumatoid arthritis. Clin. Pharmacol. Ther. 89, 735–740 (2011). [DOI] [PubMed] [Google Scholar]
- 23. Gorski, J.C. et al In vivo effects of interleukin‐10 on human cytochrome P450 activity. Clin. Pharmacol. Ther. 67, 32–43 (2000). [DOI] [PubMed] [Google Scholar]
- 24. Reiser M. et al Serum interleukin 4 and interleukin 10 levels in patients with chronic hepatitis C virus infection. J. Hepatol. 26, 471–478 (1997). [DOI] [PubMed] [Google Scholar]
- 25. Niwa Y. et al Evidence for degradation of cytokines in the serum of patients with atopic dermatitis by calcium‐dependent protease. Arch. Dermatol. Res. 292, 391–396 (2000). [DOI] [PubMed] [Google Scholar]
- 26. Källström E. et al Decreased frequency of intracellular IFN‐gamma producing T cells in whole blood preparations from patients with atopic dermatitis. Exp. Dermatol. 11, 556–563 (2002). [DOI] [PubMed] [Google Scholar]
- 27. Kleiner G. et al Cytokine levels in the serum of healthy subjects. Mediators Inflamm. 434010 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Corcos M. et al Correlation between serum levels of interleukin‐4 and alexithymia scores in healthy female subjects: preliminary findings. Psychoneuroendocrinology 29, 686–691 (2004). [DOI] [PubMed] [Google Scholar]
- 29. Szarka A. et al Circulating cytokines, chemokines and adhesion molecules in normal pregnancy and preeclampsia determined by multiplex suspension array. BMC Immunol. 11, 59 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Kaminishi K. et al Flow cytometric analysis of IL‐4, IL‐13 and IFN‐gamma expression in peripheral blood mononuclear cells and detection of circulating IL‐13 in patients with atopic dermatitis provide evidence for the involvement of type 2 cytokines in the disease. J. Dermatol. Sci. 29, 19–25 (2002). [DOI] [PubMed] [Google Scholar]
- 31. Ricci G. et al, Cytokines levels in children affected by atopic and nonatopic eczema. Open Dermatol. J. 2, 18–21 (2008). [Google Scholar]
- 32. Jeong, C.W. et al Differential in vivo cytokine mRNA expression in lesional skin of intrinsic versus extrinsic atopic dermatitis patients using semiquantitative RT‐PCR. Clin. Exp. Allergy 33, 1717–1724 (2003). [DOI] [PubMed] [Google Scholar]
- 33. Suárez‐Fariñas, M. et al Intrinsic atopic dermatitis shows similar TH2 and higher TH17 immune activation compared with extrinsic atopic dermatitis. J. Allergy Clin. Immunol. 132, 361–370 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Wang, J. , Wang, Y.M. & Ahn, H.Y. Biological products for the treatment of psoriasis: therapeutic targets, pharmacodynamics and disease‐drug‐drug interaction implications. AAPS J. 16, 938–947 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Turpault, S. et al Pharmacokinetic assessment of a five‐probe cocktail for CYPs 1A2, 2C9, 2C19, 2D6 and 3A. Br. J. Clin. Pharmacol. 68, 928–935 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Food and Drug Administration . Drug development and drug interactions: table of substrates, inhibitors and inducers. 2016. <https://www.fda.gov/drugs/developmentapprovalprocess/developmentresources/druginteractionslabeling/ucm093664.htm#table3-1>. Accessed 28 July 2017.
- 37. Mimura, H. et al Effects of cytokines on CYP3A4 expression and reversal of the effects by anti‐cytokine agents in the three‐dimensionally cultured human hepatoma cell line FLC‐4. Drug Metab. Pharmacokinet. 30, 105–110 (2015). [DOI] [PubMed] [Google Scholar]
- 38. Lee, E.B. et al Disease‐drug interaction of sarilumab and simvastatin in patients with rheumatoid arthritis. Clin. Pharmacokinet. 56, 607–615 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Zhuang, Y. et al Evaluation of disease‐mediated therapeutic protein‐drug interactions between an anti‐interleukin‐6 monoclonal antibody (sirukumab) and cytochrome P450 activities in a phase 1 study in patients with rheumatoid arthritis using a cocktail approach. J. Clin. Pharmacol. 55, 1386–1394 (2015). [DOI] [PubMed] [Google Scholar]
- 40. Clarivet, B. et al Tocilizumab and mesenteric arterial thrombosis: drug‐drug interaction with anticoagulants metabolized by CYP 450 and/or by P‐glycoprotein. Eur. J. Clin. Pharmacol. 72, 1413–1414 (2016). [DOI] [PubMed] [Google Scholar]
- 41. Food and Drug Administration . Siliq. Highlights of Prescribing Information. <https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/761032lbl.pdf> (2017).
- 42. Jang, G. et al A clinical therapeutic protein drug‐drug interaction study: goadministration of denosumab and midazolam in postmenopausal women with osteoporosis. Pharmacol. Res. Perspect. 2, e00033 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Tran, J.Q. Therapeutic protein‐drug interaction assessment for daclizumab high‐yield process in patients with multiple sclerosis using a cocktail approach. Br. J. Clin. Pharmacol. 82, 160–167 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Salazar, J. et al C‐reactive protein: an in‐depth look into structure, function, and regulation. International Scholarly Research Notices. Article ID 653045, 11 pp. doi: 10.1155/2014/653045 (2014). [DOI] [PMC free article] [PubMed]
- 45. Hanifin, J.M. et al The Eczema Area and Severity Index (EASI): assessment of reliability in atopic dermatitis. EASI Evaluator Group. Exp. Dermatol. 10, 11–18 (2001). [DOI] [PubMed] [Google Scholar]
- 46. Kokkonen, H. et al Up‐regulation of cytokines and chemokines predates the onset of rheumatoid arthritis. Arthritis Rheum. 62, 383–391 (2010). [DOI] [PubMed] [Google Scholar]
- 47. May, R.D. & Fung, M. Strategies targeting the IL‐4/IL‐13 axes in disease. Cytokine 75, 89–116 (2015). [DOI] [PubMed] [Google Scholar]
- 48. Chung, K.F. Targeting the interleukin pathway in the treatment of asthma. Lancet 386, 1086–1096 (2015). [DOI] [PubMed] [Google Scholar]
- 49. Beck, L.A. et al Dupilumab treatment in adults with moderate‐to‐severe atopic dermatitis. N. Engl. J. Med. 371, 130–139 (2014) [DOI] [PubMed] [Google Scholar]
- 50. Vekaria, A.S. et al Moderate‐to‐severe atopic dermatitis patients show increases in serum C‐reactive protein levels, correlating with skin disease activity (version 2; referees: 3 approved) F1000Research 2017, 6:1712 (doi: 10.12688/f1000research.12422.2) [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Summary of metabolizer status for patients included in the trial
Table S2. Summary of pharmacokinetic parameters for the CYP probe substrates


