Since the first successful transplant in 1989,1,2 multivisceral transplantation including the small intestine, pancreas, and liver has been established as the optimal treatment option for children with short gut syndrome and concomitant liver disease. The number of pediatric multivisceral transplants performed in the United States peaked at 89 transplants in 2007, but has since declined. This decline has been partly attributed to a reduction in liver injury with newer formulations of total parenteral nutrition (TPN) lipids. In 2016, only 35 pediatric multivisceral transplants were performed in the United States, with 11 in the children 1 year or younger.
We performed a literature search to investigate the incidence and nature of any arterial thrombotic complications in pediatric multivisceral transplantation. Using the search terms “pediatric” + “multivisceral” + “transplant” in PubMed and reviewing cited works, we identified 7 primary series reporting outcomes following pediatric multivisceral transplantation.3-9 Among these studies, Tzakis et al report 2 “disruptions of aortic anastomosis” resulting in death within 30 days of transplant. However, no arterial thrombotic complications are described in any of these series. Interestingly, arterial complications are also infrequent following multivisceral transplantation in adults.8,10
Here, we present the case of a young girl who lost her second multivisceral graft due to thrombosis of a retained aortic conduit from her initial graft.
CASE DESCRIPTION
The patient is a girl born at 35 weeks and 6 days gestation by spontaneous vaginal delivery. She had been diagnosed with gastroschisis prenatally and shortly after birth was found to have proximal jejunal atresia and midtransverse colon atresia presumably due to constriction by the gastroschisis ring. Over the first few months of life, she underwent small-bowel resections due to bowel necrosis and a serial transverse enteroplasty (STEP) procedure in order to increase intestinal absorptive length. She was maintained on partial enteral feeds and TPN. She developed TPN-associated liver disease and was ultimately listed for multivisceral transplantation. She underwent her initial multivisceral transplant at 9 months of age: this graft included a liver, small bowel, and pancreas, implanted en bloc. For graft inflow, the donor thoracic aorta was anastomosed end to side with the recipient's infrarenal aorta. Over the next several months, she experienced multiple episodes of acute cellular rejection that were refractory to steroids and thymoglobulin. This ultimately resulted in severe graft dysfunction, and she was listed for redo multivisceral transplantation.
Eleven months after the initial transplant, she underwent repeat multivisceral transplant, again with an en bloc liver, small bowel, and pancreas graft. For inflow to the second graft, the donor thoracic aorta was anastomosed in end-to-end fashion to the stump of the aortic conduit retained from the initial graft. This transplant proved to be successful, and she was weaned from TPN and maintained on enteral feeds for the next several years.
At 5 years of age (3 years and 11 months after the second transplant), she presented with abdominal distention after a week of nausea and vomiting. The workup included a computed tomography demonstrating increased bowel distention and mesenteric lymphadenopathy. A colonoscopy demonstrated mild acute colitis, and she was treated with intravenous methylprednisolone for presumed graft rejection. Three days later, a repeat computed tomography demonstrated complete thrombosis of the aortic conduit with extensive bowel pneumatosis (Figure 1). The proximal aortic conduit, which had been retained from the initial transplant, was also noted to be heavily calcified. She was urgently taken to the OR for exploratory laparotomy and underwent resection of the entire transplanted bowel, which was found to be necrotic and unsalvageable. Her postoperative course was difficult and complicated by biloma, tracheostomy placement, and several bleeding complications. She continued on tacrolimus for her remaining liver graft and eventually relisted for multivisceral transplant. Assessment of donor specific antibodies demonstrated low titers of class II antibodies (DQ6, DP15, and DP18) against the first donor (from which the original aortic conduit was derived), but no class I DSAs.
FIGURE 1.
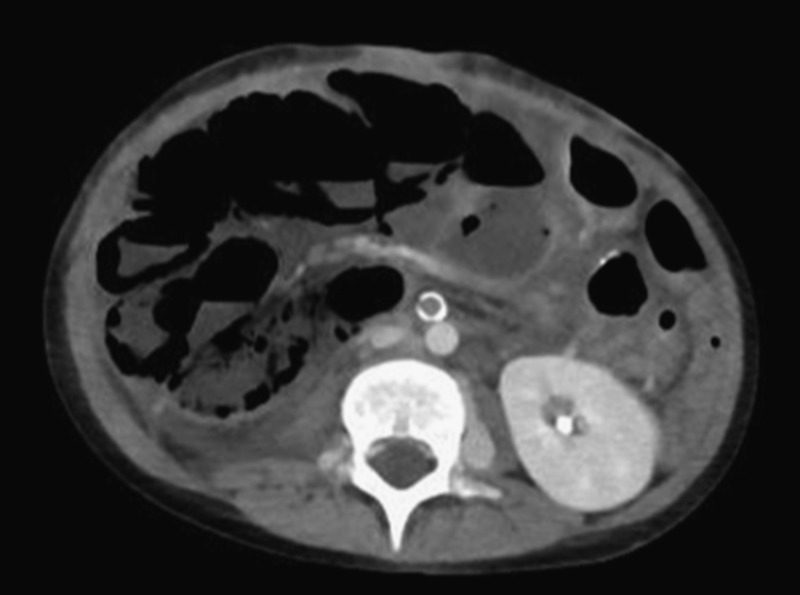
Calcification and thrombosis of aortic conduit.
Approximately a year later, she underwent a third multivisceral transplant. The original aortic conduit remained heavily calcified and was left in place; a new aortic conduit using donor thoracic aorta was placed on the infrarenal aorta at a different site, in end-to-side fashion with running 6-0 Prolene. During the perioperative period, she was anticoagulated and discharged on therapeutic-dose enoxaparin. Her most recent transplant course has been complicated by multiple episodes of ACR treated with steroid pulses and plasmapheresis/IVIG. However, currently at 8 years of age, the patient continues to do well off of TPN.
DISCUSSION
In contrast to pediatric liver transplantation, arterial thrombosis appears to be rare in pediatric multivisceral transplantation. At present, there are no published reports of arterial complications leading to graft loss, even in a retransplant series.11 This may be due to the large caliber of the inflow anastomosis, which commonly consists of an aortic conduit derived from donor thoracic aorta.
Here, we present the first report of a late arterial conduit thrombus following repeat multivisceral transplantation. During the second transplant, the original aortic conduit from the first graft was used to provide inflow to the second graft. This aortic segment became heavily calcified over time, which we presume to be a manifestation of chronic rejection. In the setting of acute illness and dehydration, this leads to acute thrombosis and graft loss.
In the United States, only 85 repeat multivisceral transplants have been performed in children, 22 of these in infants. With such a small cohort, it is difficult to establish an evidence-based approach for vascular reconstruction in pediatric repeat multivisceral transplantation. Based on our experience from this case, we suggest that in a repeat multivisceral transplant, the prior arterial conduit should not be utilized for inflow. Instead, we recommend performing a new anastomosis at a different site in the interest of avoiding a rare but serious complication.
Footnotes
Published online 27 November, 2018.
Research involving human subjects: This manuscript is exempt from institutional human subjects review due to minimal anticipated risk.
The authors declare no funding or conflicts of interest.
M.L.S. and A.S.B. participated in data collection and writing of the article. K.V.R., D.S.V., and D.L.S. were involved the patient's surgical care and participated in data collection. D.S.V. additionally participated in the writing of the article.
REFERENCES
- 1.Williams JW, Sankary HN, Foster PF, et al. Splanchnic transplantation. An approach to the infant dependent on parenteral nutrition who develops irreversible liver disease. JAMA. 1989;261:1458–1462. [DOI] [PubMed] [Google Scholar]
- 2.Starzl TE, Rowe MI, Todo S, et al. Transplantation of multiple abdominal viscera. JAMA. 1989;261:1449–1457. [PMC free article] [PubMed] [Google Scholar]
- 3.Borst AJ, Sudan DL, Wang LA, et al. Bleeding and thrombotic complications of pediatric liver transplant. Pediatr Blood Cancer. 2018;65:e26955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Goss JA, Shackleton CR, McDiarmid SV, et al. Long-term results of pediatric liver transplantation: an analysis of 569 transplants. Ann Surg. 1998;8:411–420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kato T, Selvaggi G, Gaynor J, et al. Expanded use of multivisceral transplantation for small children with concurrent liver and intestinal failure. Transplant Proc. 2006;38:1705–1708. [DOI] [PubMed] [Google Scholar]
- 6.Kwon YK, Llore N, Kaufman SS, et al. The use of vascular homografts in pediatric small bowel transplantation: single-center experience over a decade. Pediatr Transplant. 2018;65 (5). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mangus RS, Tector AJ, Kubal CA, et al. Multivisceral transplantation: expanding indications and improving outcomes. J Gastrointest Surg. 2013;17:179–186. [DOI] [PubMed] [Google Scholar]
- 8.Tzakis AG, Kato T, Levi DM, et al. 100 multivisceral transplants at a single center. Ann Surg. 2005;242:480–490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vianna RM, Mangus RS, Tector AJ. Current status of small bowel and multivisceral transplantation. Adv Surg. 2008;42:129–150. [DOI] [PubMed] [Google Scholar]
- 10.Fägerlind M, Gäbel M, Zachrisson-Jönsson K, et al. Vascular complications after intestinal transplantation—a single center experience. Transplantation. 2017;101(6S2):S105. [Google Scholar]
- 11.Trevizol AP, David AI, Yamashita ET, et al. Intestinal and multivisceral retransplantation results: literature review. Transplant Proc. 2013;45:1133–1136. [DOI] [PubMed] [Google Scholar]


