Supplemental Digital Content is available in the text
Keywords: coronary bifurcation lesion, crush, culotte, provisional
Abstract
Background and objective:
The modified double-stent and provisional stenting strategies have been widely used in patients with coronary bifurcation lesions, but what is the optimization has not been clearly defined. This meta-analysis is to elucidate the benefits from modified double-stent and provisional stenting strategies in patients with coronary bifurcation lesions.
Methods:
Electronic databases were searched to identify studies comparing the modified double-stent and provisional stenting strategies in patients with coronary bifurcation lesions. The clinical outcomes were divided into early (≤6 months) and late (>6 months) events according to the follow-up duration. The early endpoints included cardiac death, myocardial infarction, target lesion revascularization or target vessel revascularization, and major adverse cardiac events (MACE), and the late endpoints also include stent thrombosis in addition to the early endpoints index. The angiographic endpoint was in-stent restenosis. Data were analyzed by the statistical software RevMan (version 5.3).
Results:
A total of 6 studies involving 1683 patients with coronary bifurcation lesions were included in this meta-analysis, which found that the modified double-stent strategy was associated with a lower risk of cardiac death (odds ratio [OR] = 0.29, 95% confidence intervals [CI] 0.11–0.78, P = .01), myocardial infarction (OR = 0.41, 95% CI 0.21–0.82, P = .01), target lesion revascularization or target vessel revascularization (OR = 0.31, 95% CI 0.15–0.63, P = .001), and MACE (OR = 0.41, 95% CI 0.22–0.74, P = .003) compared with provisional stenting in the early follow-up endpoint events, while the risk of cardiac death and stent thrombosis were similar between both strategies (OR = 0.59, 95% CI 0.31–1.10, P = .09; and OR = 0.62, 95% CI 0.34–1.15, P = .13; respectively) in the late follow-up endpoint events. There were significant differences between both strategies in myocardial infarction (OR = 0.42, 95% CI 0.24–0.75, P = .003), MACE (OR = 0.44, 95% CI 0.31–0.62, P < .00001), and target lesion revascularization or target vessel revascularization (OR 0.35, 95% CI 0.25–0.49, P < .00001) between both strategies in the late follow-up endpoint events. The risk of in-stent restenosis favored the modified double-stent strategy (OR 0.29, 95% CI 0.20–0.43, P < .00001).
Conclusion:
The modified double-stent strategy is associated with excellent clinical and angiographic outcomes except for the occurrence of cardiac death and stent thrombosis late-term outcome compared with provisional stenting strategy in patients with coronary bifurcation lesions. These findings suggest that the modified double-stent strategy can be recommended as an optimization in patients with coronary bifurcation lesions.
1. Introduction
The coronary bifurcation is a common site of atherosclerosis formation due to blood eddy currents and increased vessel wall pressure. Patients with coronary bifurcation lesions account for approximately 15% to 20% of all coronary lesions in coronary interventional procedures.[1] However, percutaneous coronary intervention (PCI) for bifurcation lesions remains a technical challenge due to the low procedural success rate and high risk of procedural complications,[2–4] for which no optimal strategy has been well established. Multiple randomized controlled clinical trials (RCTs) reported that the provisional stenting strategy (stenting the main vessel and the additional stenting of the side branch only in case of occlusion risk) was similar or even superior to the 2-stent technique (planned stenting of the main vessel and side branch) for bifurcation lesions in terms of the clinical outcome.[1,5–7] Therefore, the current guidelines recommended the provisional stenting strategy as the preferred treatment for bifurcation lesions due to those RCTs.[8]
The double kissing double crush (DK crush) technique was first described by Chen et al[9,10] for decades ago, and both double kissing mini-culotte stenting (DK mini-culotte) and mini-crush techniques have also been introduced into clinical practice.[11,12] Several studies demonstrated that the modified double-stent strategy could significantly reduce potential target lesion revascularization and major adverse cardiac event (MACE) in patients with complex bifurcation lesions,[13,14] and which effect was more pronounced in the case of increased risk for plaque displacement and bifurcation change. However, the procedural complications were significantly higher in the modified double-stent strategy than those of the provisional stenting strategy, such as contrast volume, fluoroscopy time, and operative time. Up to date, the optimal strategy remains controversial in patients with coronary bifurcation lesions. The present study is to compare the clinical outcomes between modified double-stent and provisional stenting strategies, to identify the assumption that the modified double-stent strategy might be superior to provisional stenting in patients with coronary bifurcation lesions.
2. Methods
2.1. Data source and search strategy
A standard principle was presented for data extraction and analysis based on the current Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) guidelines.[15] PubMed, Embase, Web of Science, the Cochrane Library, CNKI, and WANFANG database were searched from inception until May 1, 2018. Meeting abstracts were also searched. The search strategy included Medical Subject Heading terms (MeSH) and keyword searches, and all searches had no language restrictions. Search keywords included coronary bifurcation lesions, provisional, crush, and culotte.
This meta-analysis included randomized control trials and non-randomized controlled studies comparing the modified double-stent and provisional stenting strategies in patients with coronary bifurcation lesions. The following criteria had to be fulfilled to consider a study eligible for this meta-analysis: all patients with coronary bifurcation lesions; (2) inclusion of subjects only to modified double-stent versus provisional stenting strategies (modified double-stent = DK crush, DK mini-culotte, mini-crush); complete reporting of clinical outcomes, for example, clinical endpoints (cardiac death, myocardial infarction, target lesion revascularization or target vessel revascularization, MACE, stent thrombosis, and in-stent restenosis); all studies included long-term cardiac death. Studies only comparing 2 different strategies of the modified double stenting were excluded. Studies with incomplete data concerning the above outcomes, studies without availability of full-text articles, and ongoing studies were also excluded.
2.2. Outcome definition
The outcome of this analysis included clinical and angiographic endpoints. The clinical endpoints were divided into early and late events according to the follow-up duration. The early endpoint events limited to trials with a follow-up duration ≤6 months, including cardiac death, myocardial infarction, target lesion revascularization or target vessel revascularization, and MACE. The late endpoint events limited to trials with a follow-up duration >6 months, including stent thrombosis in addition to the above mentioned early endpoint events. The angiographic endpoint included in-stent restenosis. All patients with coronary artery disease were eligible with a Medina 1,1,1,1,0,1 or 0,1,1 de novo coronary bifurcation lesions in the present study.[16] The myocardial infarction was defined as elevation of cardiac enzymes (data for cardiac enzymes >1 times the upper normal limit (UNL) in the DKCRUSH-II and DKCRUSH-Vtrial[17,18] and ≥3 times the UNL in the remaining studies [11,19–21]), with or without new pathological Q waves. The cardiac enzymes, assessed for this aim, varied among the studies, being total creatine kinase (CK), CK-myocardial band isoenzyme (CK-MB) isoenzyme or troponin T or I. All-cause death was considered cardiac death unless non-cardiac reasons were indicated. The MACE was defined as the composite endpoint of death, myocardial infarction, and target vessel revascularization or stroke (only 1 study[19]). The stent thrombosis was defined according to the academic research consortium definition.[22] The target vessel/lesion revascularization was the repeat target vessel/lesion therapy after PCI.
2.3. Data collection and quality assessment
Four reviewers (Y.H.L., C.G., M.B.Z., and M.L.) independently extracted data from the identified studies. A standard data extraction form was designed before extraction. To reduce bias, the method section and the result section were extracted on separate forms, and extractors were blinded to the information that may influence their judgment (such as authors, titles, journal's impact) during the whole process. The following information was derived from each article: the first author, year of publication, follow-up duration, and the number, baseline characteristics, as well as clinical and angiographic outcomes of the patients involved. Any disagreement or uncertainty was resolved by a consensus or, if necessary, by a third party (Z.L.W.). The quality evaluation of eligible studies was assessed by the Cochrane Collaboration's tool for RCTs.[23] Non-randomized studies were assessed by the Newcastle–Ottawa scale.[24] Quality evaluation of each study was also performed independently. The quality of studies was not used to change their weight in this analysis, but as an indicator of validity. As all analyses were based on previously published studies, no ethical approval and patient consent are required.
2.4. Statistical analysis
In this study, data were analyzed by the statistical software RevMan (Review Manager (RevMan). Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014). Continuous variables of baseline characteristics as mean ± SD were counted by mean difference. The data regarding the outcomes assessed in this study were dichotomous, and Mantel–Haenszel odds ratio (OR) and the corresponding 95% confidence intervals (CI) were calculated. The Higgins I2-test was used for heterogeneity test, and the bound of I2 > 50% was used to identify significant heterogeneity. The fixed effects models (Mantel–Haenszel method) were applied unless there was evidence of heterogeneity (I2 > 50%), where random effects model was used. Sensitivity analysis was completed by comparing the treatment influences obtained with each trial removed consecutively from the analysis with the overall treatment influences to find potential sources of heterogeneity. In addition, subgroup analysis based on the baseline characteristics was also performed to explore the sources for heterogeneity. Publication bias was assessed by funnel plots. All P values were 2 sided, a P < .05 was considered statistically significant.
3. Results
3.1. Search results
The initial search retrieved 76 studies. After removal of duplicate records and ineligible studies, 11 articles remained were fully reviewed based on the inclusion criteria. Finally, 6 of them met the predefined inclusion criteria are included in the meta-analysis[11,17–21] (flow diagram). Quality assessment of the included trials is reported (appendix supplementary).
3.2. Study characteristics
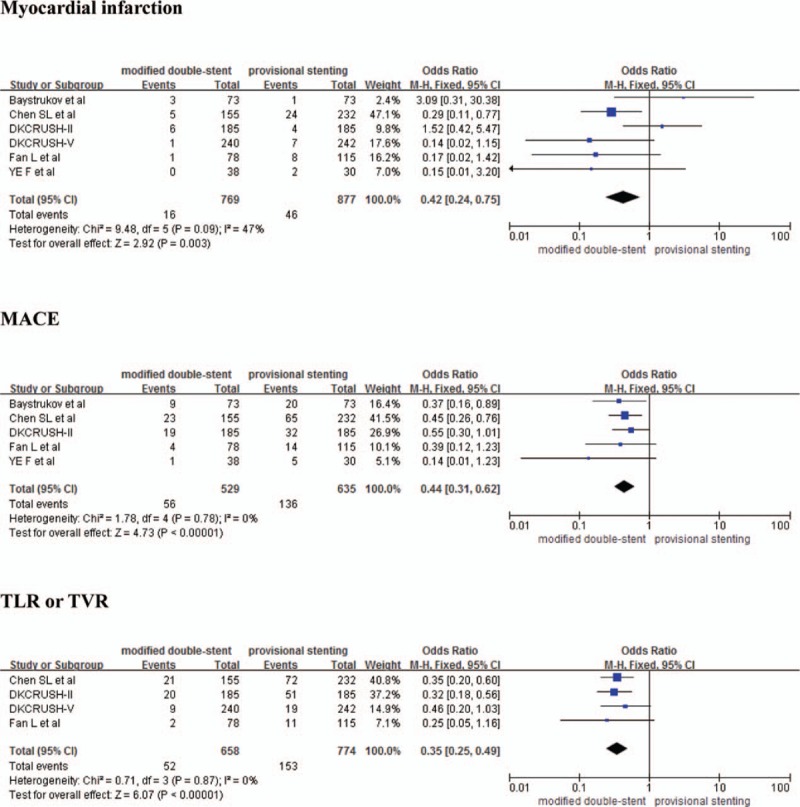
The general characteristics of the included trials are listed in Table 1. Four randomized trials and 2 observational studies included a total of 1683 patients were enrolled into this analysis. Among them, there were 782 patients with coronary bifurcation lesions in the modified double-stent strategy and 901 patients with those in the provisional stenting strategy, with an average age of 63.5 ± 9.8 years. The proportion of patients with diabetes, hypertension, and hyperlipidemia was 25.4%, 69.3%, and 43.6%, respectively. Of the 1683 patients with coronary bifurcation lesions, 21.3% had a previous history of PCI, and 0.5% had a previous history of coronary artery bypass grafting. In addition, 60.8% patients with coronary bifurcation lesions involved lesion site in the left anterior descending artery, 32.3% patients with those involved lesion site in the left circumflex artery, and 36.4% patients with those involved lesion site in the right coronary artery. Following Medina stratification, 80.1%, 86.9%, and 29.1% patients with coronary bifurcation lesions belong to 1,1,1;1,0,1; and 0,1,1, respectively. The modified double-stent strategy was associated with a longer operative time (62.97 ± 32.0 vs. 53.96 ± 27.0 min), longer fluoroscopy time (31.05 ± 17.8 vs. 25.88 ± 15.7 min), and higher volume of the contrast used compared with provisional stenting strategy (191.5 ± 84.2 vs. 169.37 ± 80.9 mL).
Table 1.
Baseline characteristics of the included studies.
3.3. Comparison of clinical outcomes between modified double-stent and provisional stenting strategies
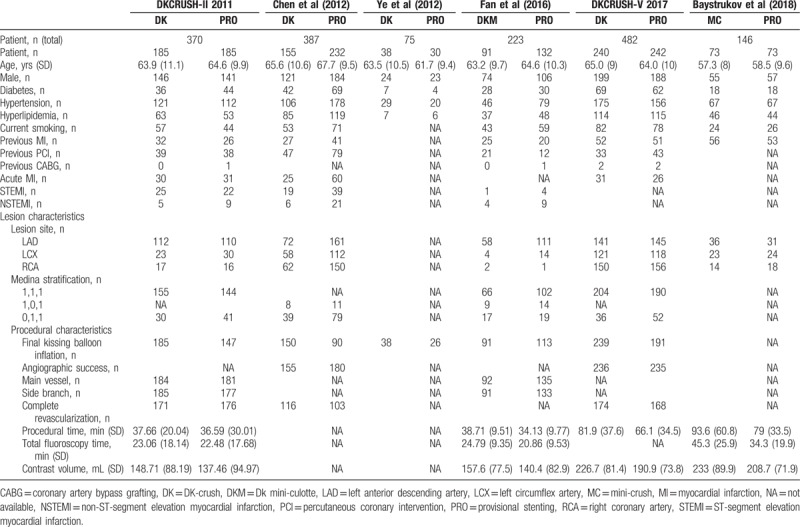
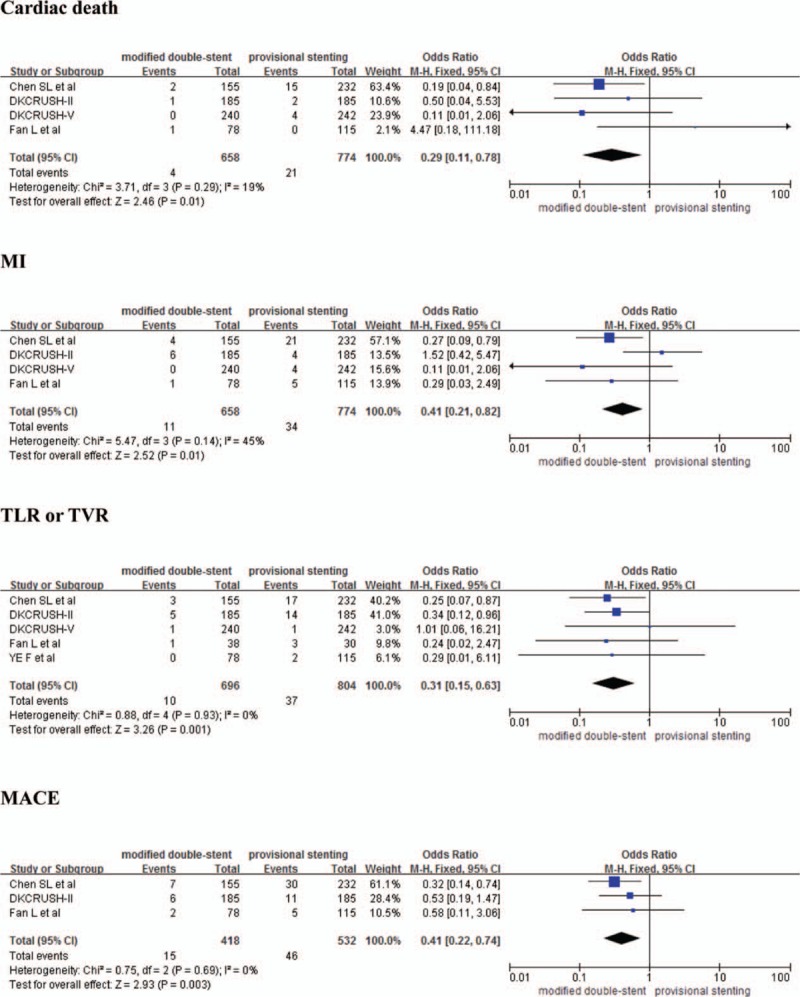
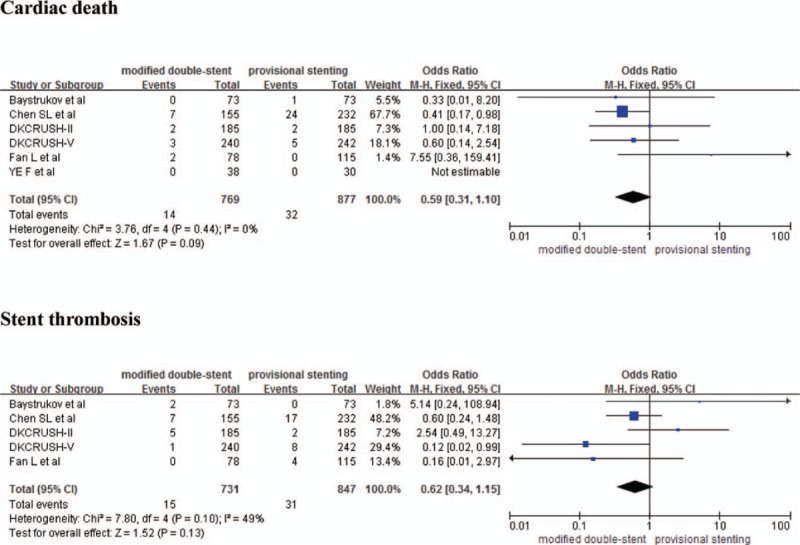
The risk of early follow-up cardiac death (OR = 0.29, 95% CI 0.11–0.78, P = .01), myocardial infarction (OR = 0.41, 95% CI 0.21–0.82, P = .01), target lesion revascularization or target vessel revascularization (OR = 0.31, 95% CI 0.15–0.63, P = .001), and MACE (OR = 0.41, 95% CI 0.22–0.74, P = .003) is lower in the modified double-stent strategy than those of provisional stenting strategy in patients with coronary bifurcation lesions (Fig. 1). There are no significant differences in cardiac death and stent thrombosis between modified double-stent and provisional stenting strategies in the late follow-up duration (OR = 0.59, 95% CI 0.31–1.10, P = .09 and OR = 0.62, 95% CI 0.34–1.15, P = .13) (Fig. 2). Meanwhile, the modified double-stent strategy is associated with a reduced risk of myocardial infarction (OR = 0.42, 95% CI 0.24–0.75, P = .003), MACE (OR = 0.44, 95% CI 0.31–0.62, P < .00001), and target lesion revascularization or target vessel revascularization compared with provisional stenting strategy (OR 0.35, 95% CI 0.25–0.49, P < .00001) (Fig. 3). There was no significant heterogeneity in clinical endpoints. The result of sensitivity analysis indicated that each OR for cardiac death (early and late), myocardial infarction (early and late), target lesion revascularization or target vessel revascularization (early and late), MACE (early and late), stent thrombosis did not show substantial change, which meant that these outcomes were stable and reliable in this study. The publication bias test was not performed due to the limited number of the studies (<10) in this meta-analysis.
Figure 1.
Forest plots comparing early endpoint of cardiac death, myocardial infarction, target lesion revascularization or target vessel revascularization, and major adverse cardiac events between modified double-stent and provisional stenting strategy. MI = myocardial infarction, TLR or TVR = target lesion revascularization or target vessel revascularization, MACE = major adverse cardiac events.
Figure 2.
Forest plots comparing late endpoint of cardiac death and stent thrombosis between modified double-stent and provisional stenting strategy.
Figure 3.
Forest plots comparing late endpoint of myocardial infarction, major adverse cardiac events and target lesion revascularization or target vessel revascularization between modified double-stent and provisional stenting strategy. MI = myocardial infarction, TLR or TVR = target lesion revascularization or target vessel revascularization, MACE = major adverse cardiac events.
3.4. Comparison of angiographic outcomes between modified double-stent and provisional stenting strategies
The studies of Chen et al[20] and Ye et al were excluded[21] because of the absence of scheduled follow-up angiographic examinations. Pooling of the remaining 4 studies shows that the modified double-stent strategy had a lower risk of in-stent restenosis compared with provisional stent strategy (OR 0.29, 95% CI 0.20–0.43, P < .00001) (Fig. 4). Another insignificant heterogeneity was found in the in-stent restenosis (I2 = 0%). Similarly, the in-stent restenosis did not show substantial change in the sensitivity analysis, the publication bias test was also not performed.
Figure 4.
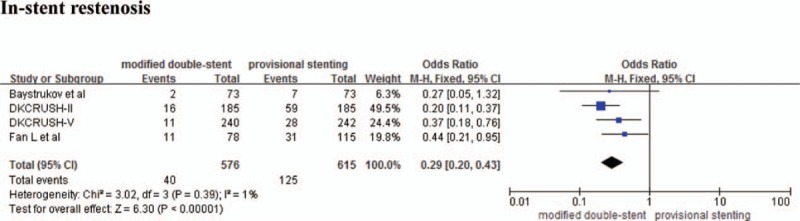
Forest plots comparing angiographic endpoint of in-stent restenosis between modified double-stent and provisional stenting strategy.
4. Discussion
This meta-analysis is the first time to assess clinical and angiographic profile between both different strategies in patients with coronary bifurcation lesions. The major findings of the present study are as follows: the modified double-stent strategy was associated with a significant reduction of early-term cardiac death, myocardial infarction, target lesion revascularization or target vessel revascularization, MACE, and in-stent restenosis; and no significant difference was showed in late-term cardiac death and stent thrombosis between both strategies.
The current guidelines and consensus recommend the provisional stenting strategy (class I; level of evidence A) for patients with coronary bifurcation lesions based on previous clinical data.[1,8,25] Those previous clinical data showed that the provisional stenting strategy was associated with a lower incidence of procedure-related myocardial necrosis,[26] while both conventional crush and culotte techniques had high risk of side-branch occlusion. Meanwhile, the conventional crush technique would cause a vast number of stent struts crushed at or near bifurcation arena with somehow being nonapposed, which may delay neointimal coverage.[27] In addition, the culotte technique also would lead to high rates of intraprocedural events, in-stent restenosis, and in-stent thrombosis.[28] With the emergence of the modified double-stent strategy, the fact that the improvement of clinical and angiographic outcomes compared with those in whom provisional stenting was identified in this study, which may be as a guideline recommend for patients with coronary bifurcation lesions in clinical practice according to this study.
There was significant difference in MACE between modified double-stent and provisional stenting strategies, which was different from the result reported in most previous studies[11] but was consistent with that of Definitions and impact of complEx biFurcation lesIons on clinical outcomes after percutaNeous coronary IntervenTIOn using drug-eluting steNts (DEFINITION) registry (16.8% vs. 8.9%, P < .001).[29] Additionally, this meta-analysis found that the lower risk of myocardial infarction (2.1% vs. 5.2%) and target lesion revascularization or target vessel revascularization event (10.6% vs. 21.4%) benefited from the modified double-stent strategy. Therefore, the lower MACE further originated from lower risk of myocardial infarction and target lesion revascularization or target vessel revascularization in the modified double-stent strategy. This study showed that there was no significant difference in stent thrombosis between both strategies. Similar to this study, Chen et al[30] and Maeng et al[31] also reported no significant difference in long-term stent thrombosis (0% vs. 1.1%, 1.5% vs. 3%) between conventional stenting (crush and culotte) and provisional stenting during the follow-up of 5 years. The standard of dual antiplatelet therapy after PCI is 12 months at least; discontinuous antiplatelet therapy may be the important reason for stent thrombosis event. Although there was no significant difference in stent thrombosis between both strategies, it could not be simply attributed to single or double-stent strategy, and the reasons may be more complex. Interestingly, this study demonstrated that the risk of cardiac death that reached a statistical difference was limited to trials with a follow-up duration ≤6 months. However, there were no significant difference in cardiac death between both difference strategies when the follow-up duration was extended to more than 6 months, which also was similar to the study of Chen et al[30] (2.2% vs. 3.3%, P = .513). Among the different studies included in this meta-analysis, only trial of Chen et al demonstrated that there was no significant difference in late-term cardiac death between the 2 stenting and provisional stenting strategies.[20] This difference in cardiac death may be related to the discrepancies in baseline characteristics compared with the study of Chen et al[20], such as the lesion site in the left anterior descending artery was 60.8%, and 80.1% Medina stratification belonged to 1,1,1. It is likely that the long-term cardiac death is multifactorial, for instance, different strategies may produce different hemodynamic disturbances at the bifurcations,[32] which were responsible for cardiac death event. In addition, insignificant stent thrombosis events may also be responsible for cardiac death events. There may also be other factors contributing to cardiac death. Unfortunately, they were not included in this analysis. Currently, many experts concerned about the risk of stent restenosis and deformation of stenting the side branch in the two-stent strategy, which could reduce the clinical benefits of this strategy. However, our meta-analysis confirmed there was significant clinical benefits in in-stent restenosis no matter side branch or main vessel in the modified double-stent strategy. These results may be explained by the higher success rate of final kissing balloon inflation (99.2% vs. 69.1%) at the operation process in the modified double-stent strategy. The DKCRUSH-VI (Double Kissing Crush Versus Provisional Stenting Technique for Treatment of Coronary Bifurcation Lesions VI) study found that final kissing balloon inflation after bailed-out side branch stenting or side branch angioplasty alone was associated with a higher rate of in-stent restenosis in the distal main vessel.[33] One study illustrated that the flow reserve fraction of the side branch in the DK group was significantly higher than that of the one-stent group,[34] which showed that the DK crush technique could achieve a better hemodynamic and functional profile for side-branch stenting compared with provisional technique, and these benefits may reduce the risk of in-stent restenosis. These meta-analysis authors recommend that the modified double-stent strategy should be used as a preferred option for patients with coronary bifurcation lesions based on the above results.
Nevertheless, these results should be explained carefully. First, an operation strategy mainly depended on the intention of the operator and characteristics of patients, the success of operation was related to the operator's experience. Second, longer operative time, fluoroscopy time, and higher contrast load were occurrence in the modified double-stent strategy compared with provisional stenting strategy, which might result in the lost benefit of the modified double-stent strategy. Third, discontinuation of antiplatelet therapy also was a predictor of postprocedural stent thrombosis, although no specific anti-platelet therapy data about each study were obtained in this study. Meanwhile, the follow-up duration of all studies included was less than 12 months in present study. Therefore, it is necessary to extend the follow-up duration or more studies of stent thrombosis events. In addition, only the DKCRUSH-III study examined clinical outcomes between modified double-stent and conventional double-stent strategy,[35] which showed that the double-kiss crush strategy was associated with a lower MACE (6.2% vs. 16.3%, P = .001) in the distal left main disease during the 3-year follow-up period compared with culotte technique. The study of Freixa et al[36] found that the crush technique was more frequently used for left anterior descending lesions, while the culotte technique was more often used in the left main and left circumflex artery lesions, despite the absence of long-term follow-up outcomes. For this reason, the modified double-stent strategy could lead to significant clinical outcomes in patients with coronary bifurcation lesions were not examined. Furthermore, in respect of late-term cardiac death, the DEFINITION II trial would provide further evidence[37] (NCT02284750).
4.1. Limitations
This meta-analysis was not based on patient-level data, the effect of different patient characteristics and different stent strategies on clinical and angiographic outcomes have not been explored. Which type of the patients treated by addition stent is impossible to be determined in the provisional stenting strategy. The clinical outcomes reported in this study were followed up for less than 12 months. If the follow-up duration was prolonged, the differences in clinical outcomes might not be confirmed between both different strategies in patients with coronary bifurcation lesions. Meanwhile, the clinical outcomes of this study are also affected by relatively small sample size. In addition, various strategies (DK crush, DK mini-culotte, and mini-crush) have been used in the modified double-stent strategy, which may have different impact on the outcome. Therefore, further studies are needed to detect a possible difference among these strategies. Finally, the adjusted analysis is not performed for the inevitable selection bias.
5. Conclusion
In summary, the modified double-stent strategy has a significant advantage over the provisional stenting, except for stent thrombosis and cardiac death in the late follow-up endpoint. However, it is still necessary to compare the difference between modified double-stent and provisional stenting strategies in patients with coronary bifurcation disease.
Author contributions
Conceptualization: Zhi-Lu Wang.
Data curation: Yong-Hui Lv.
Formal analysis: Yong-Hui Lv, Chen Guo, Min Li, Ming-Bo Zhang.
Investigation: Yong-Hui Lv, Chen Guo, Min Li, Ming-Bo Zhang.
Methodology: Yong-Hui Lv, Chen Guo, Min Li, Ming-Bo Zhang.
Project administration: Zhi-Lu Wang.
Resources: Yong-Hui Lv.
Software: Yong-Hui Lv.
Supervision: Zhi-Lu Wang.
Validation: Zhi-Lu Wang.
Writing – original draft: Yong-Hui Lv.
Writing – review & editing: Yong-Hui Lv.
Supplementary Material
Footnotes
Abbreviations: MACE = major adverse cardiac events, PCI = percutaneous coronary intervention.
YHL, CG, ML, and MBZ contributed equally to this work.
Funding: This study received no specific grant from any funding agency in the public, commercial, or not-profit sectors.
The authors have no funding and conflicts of interest to disclose.
Supplemental Digital Content is available for this article.
References
- [1].Steigen TK, Maeng M, Wiseth R, et al. Randomized study on simple versus complex stenting of coronary artery bifurcation lesions: the Nordic bifurcation study. Circulation 2006;114:1955–61. [DOI] [PubMed] [Google Scholar]
- [2].Lassen JF, Holm NR, Stankovic G, et al. Percutaneous coronary intervention for coronary bifurcation disease: consensus from the first 10 years of the European Bifurcation Club meetings. Eurointervention 2014;10:545–60. [DOI] [PubMed] [Google Scholar]
- [3].Kornowski R. The complexity of stenting in bifurcation coronary lesions. JACC Cardiovasc Interv 2013;6:696–7. [DOI] [PubMed] [Google Scholar]
- [4].Al SJ, Berger PB, Rihal CS, et al. Immediate and long-term outcome of intracoronary stent implantation for true bifurcation lesions. J Am Coll Cardiol 2000;35:929–36. [DOI] [PubMed] [Google Scholar]
- [5].Colombo A, Bramucci E, Saccà S, et al. Randomized study of the crush technique versus provisional side-branch stenting in true coronary bifurcations: the CACTUS (Coronary Bifurcations: Application of the Crushing Technique Using Sirolimus–Eluting Stents) study. Circulation 2009;119:71–8. [DOI] [PubMed] [Google Scholar]
- [6].Hildick-Smith D, de Belder AJ, Cooter N, et al. Randomized trial of simple versus complex drug-eluting stenting for bifurcation lesions: the British Bifurcation Coronary Study: old, new, and evolving strategies. Circulation 2010;121:1235–43. [DOI] [PubMed] [Google Scholar]
- [7].Ferenc M, Gick M, Kienzle RP, et al. Randomized trial on routine vs. provisional T-stenting in the treatment of de novo coronary bifurcation lesions. Eur Heart J 2008;29:2859–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Stankovic G, Lefèvre T, Chieffo A, et al. European Bifurcation Club. Consensus from the 7th European Bifurcation Club meeting. Eurointervention 2013;9:36–45. [DOI] [PubMed] [Google Scholar]
- [9].Chen SL, Ye F, Zhang JJ, et al. DK crush technique: modified treatment of bifurcation lesions in coronary artery. Chin Med J 2005;118:1746–50. [PubMed] [Google Scholar]
- [10].Chen SL, Zhang JJ, Ye F, et al. Study comparing the double kissing (DK) crush with classical crush for the treatment of coronary bifurcation lesions: the DKCRUSH-1 Bifurcation Study with drug-eluting stents. Eur J Clin Invest 2008;38:361–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Fan L, Chen LL, Luo YK, et al. DK mini-culotte stenting in the treatment of true coronary bifurcation lesions: a propensity score matching comparison with T-provisional stenting. Heart Vessels 2016;31:308–21. [DOI] [PubMed] [Google Scholar]
- [12].Galassi AR, Tomasello SD, Capodanno D, et al. Mini-crush versus T-provisional techniques in bifurcation lesions: clinical and angiographic long-term outcome after implantation of drug-eluting stents. JACC Cardiovasc Interv 2009;2:185–94. [DOI] [PubMed] [Google Scholar]
- [13].Galassi AR, Colombo A, Buchbinder M, et al. Long-term outcomes of bifurcation lesions after implantation of drug-eluting stents with the “mini-crush technique”. Catheter Cardiovasc Interv 2007;69:976–83. [DOI] [PubMed] [Google Scholar]
- [14].Jim MH, Ho HH, Chan AO, et al. Stenting of coronary bifurcation lesions by using modified crush technique with double kissing balloon inflation (sleeve technique): immediate procedure result and short-term clinical outcomes. Catheter Cardiovasc Interv 2007;69:969–75. [DOI] [PubMed] [Google Scholar]
- [15].Moher D, Liberati A, Tetzlaff J, et al. PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 2009;339:b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Medina A, Suárez LJ, Pan M. A new classification of coronary bifurcation lesions. Rev Esp Cardiol 2006;59:183–183. [PubMed] [Google Scholar]
- [17].Chen SL, Santoso T, Zhang JJ, et al. A randomized clinical study comparing double kissing crush with provisional stenting for treatment of coronary bifurcation lesions: results from the DKCRUSH-II (double kissing crush versus provisional stenting technique for treatment of coronary bifurcation lesions) trial. J Am Coll Cardiol 2011;57:914–20. [DOI] [PubMed] [Google Scholar]
- [18].Chen SL, Zhang JJ, Han Y, et al. Double kissing crush versus provisional stenting for left main distal bifurcation lesions DKCRUSH-V randomized trial. J Am Coll Cardiol 2017;70:2605–17. [DOI] [PubMed] [Google Scholar]
- [19].Baystrukov VI, Kretov EI, Boukhris M, et al. A randomized trial of bifurcation stenting technique in chronic total occlusions percutaneous coronary intervention. Coron Artery Dis 2018;29:30–8. [DOI] [PubMed] [Google Scholar]
- [20].Chen SL, Zhang Y, Xu B, et al. Five-year clinical follow-up of unprotected left main bifurcation lesion stenting: one-stent versus two-stent techniques versus double-kissing crush technique. Eurointervention 2012;8:803–14. [DOI] [PubMed] [Google Scholar]
- [21].Ye F, Chen SL, Zhang JJ, et al. Hemodynamic changes of fractional flow reserve after double kissing crush and provisional stenting technique for true bifurcation lesions. Gin Med J 2012;125:2658–62. [PubMed] [Google Scholar]
- [22].Mauri L, Hsieh WH, Massaro JM, et al. Stent thrombosis in randomized clinical trials of drug-eluting stents. N Engl J Med 2007;356:1020–9. [DOI] [PubMed] [Google Scholar]
- [23].Higgins JP, Altman DG, Gøtzsche PC, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomized trials. Brit Med J 2011;343:889–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Wells GA, Shea B, O’Connell D, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality if nonrandomized studies in meta-analyses. 2014. Available at: URL: http://www.ohri.ca/programs/clinical_epidemiology/oxford.htm [Google Scholar]
- [25].Levine GN, Bates ER, Blankenship JC, et al. 2011 ACCF/AHA/SCAI guideline for percutaneous coronary intervention: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. J Am Coll Cardiol 2011;58:2550–83. [DOI] [PubMed] [Google Scholar]
- [26].Song YB, Park TK, Hahn JY, et al. Optimal strategy for provisional side branch intervention in coronary bifurcation lesions: 3-year outcomes of the SMART-STRATEGY randomized trial. JACC Cardiovasc Interv 2016;9:517–26. [DOI] [PubMed] [Google Scholar]
- [27].Costa RA, Mintz GS, Carlier SG, et al. Bifurcation coronary lesions treated with the “crush” technique: an intravascular ultrasound analysis. J Am Coll Cardiol 2005;46:599–605. [DOI] [PubMed] [Google Scholar]
- [28].Chevalier B, Glatt B, Royer T, et al. Placement of coronary stents in bifurcation lesions by the “culotte” technique. Am J Cardiol 1998;82:943–9. [DOI] [PubMed] [Google Scholar]
- [29].Chen SL, Sheiban I, Xu B, et al. Impact of the complexity of bifurcation lesions treated with drug-eluting stents: the DEFINITION study (Definitions and impact of complEx biFurcation lesIons on clinical outcomes after percutaNeous coronary IntervenTIOn using drug-eluting steNts). JACC Cardiovasc Interv 2014;7:1266–76. [DOI] [PubMed] [Google Scholar]
- [30].Chen SL, Santoso T, Zhang JJ, et al. Clinical outcome of double kissing crush versus provisional stenting of coronary artery bifurcation lesions the 5-year follow-up results from a randomized and multicenter DKCRUSH-II study (randomized study on double kissing crush technique versus provisional stenting technique for coronary artery bifurcation lesions). Circ Cardiovasc Interv 2017;10:e004497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Maeng M, Holm NR, Erglis A, et al. Nordic-Baltic Percutaneous Coronary Intervention Study Group. Long-term results after simple versus complex stenting of coronary artery bifurcation lesions: Nordic bifurcation study 5-year follow-up results. J Am Coll Cardiol 2013;62:30–4. [DOI] [PubMed] [Google Scholar]
- [32].Zheng XW, Zhao DH, Peng HY, et al. Randomized comparison of the crush versus the culotte stenting for coronary artery bifurcation lesions. Chin Med J (Engl) 2016;129:505–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Chen SL, Ye F, Zhang JJ, et al. Randomized comparison of FFR-guided and angiography-guided provisional stenting of true coronary bifurcation lesions: the DKCRUSH-VI trial (Double Kissing Crush Versus Provisional Stenting Technique for Treatment of Coronary Bifurcation Lesions VI). JACC Cardiovasc Interv 2015;8:536–46. doi:10.1016/j.jcin [DOI] [PubMed] [Google Scholar]
- [34].Ye F, Zhang JJ, Tian NL, et al. The acute changes of fractional flow reserve in DK (double kissing), crush, and 1-stent technique for true bifurcation lesions. J Interv Cardiol 2010;23:341–5. [DOI] [PubMed] [Google Scholar]
- [35].Chen SL, Xu B, Han YL, et al. Clinical outcome after DK crush versus culotte stenting of distal left main bifurcation lesions: the 3-year follow-up results of the DKCRUSH-III study. JACC Cardiovasc Interv 2015;8:1335–42. [DOI] [PubMed] [Google Scholar]
- [36].Freixa X, Almasood AA, Asif N, et al. Long-term outcomes using a two-stent technique for the treatment of coronary bifurcations. Int J Cardiol 2013;168:446–51. [DOI] [PubMed] [Google Scholar]
- [37].Zhang JJ, Gao XF, Han YL, et al. Treatment effects of systematic two-stent and provisional stenting techniques in patients with complex coronary bifurcation lesions: rationale and design of a prospective, randomised and multicentre DEFINITION II trial. BMJ Open 2018;8:e020019. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


