Abstract
Case series study.
To report the clinical outcomes of posterior temporary C1-2 fixation for 3-part fracture of the axis (Type II odontoid fracture according to Grauer classification combined with Hangman fracture).
The 3-part fracture of the axis is rare and the treatment is controversy.
A total of 8 patients with 3-part fracture of the axis were included in this study. X-rays, CT, and MRI prior to surgery were used to evaluate the cervical spine injury. Grauer classification, fracture angulation, and fracture translation were used to evaluate the fracture of dens. The neck disability index (NDI) and range of neck rotary motion were used to assess the neck function.
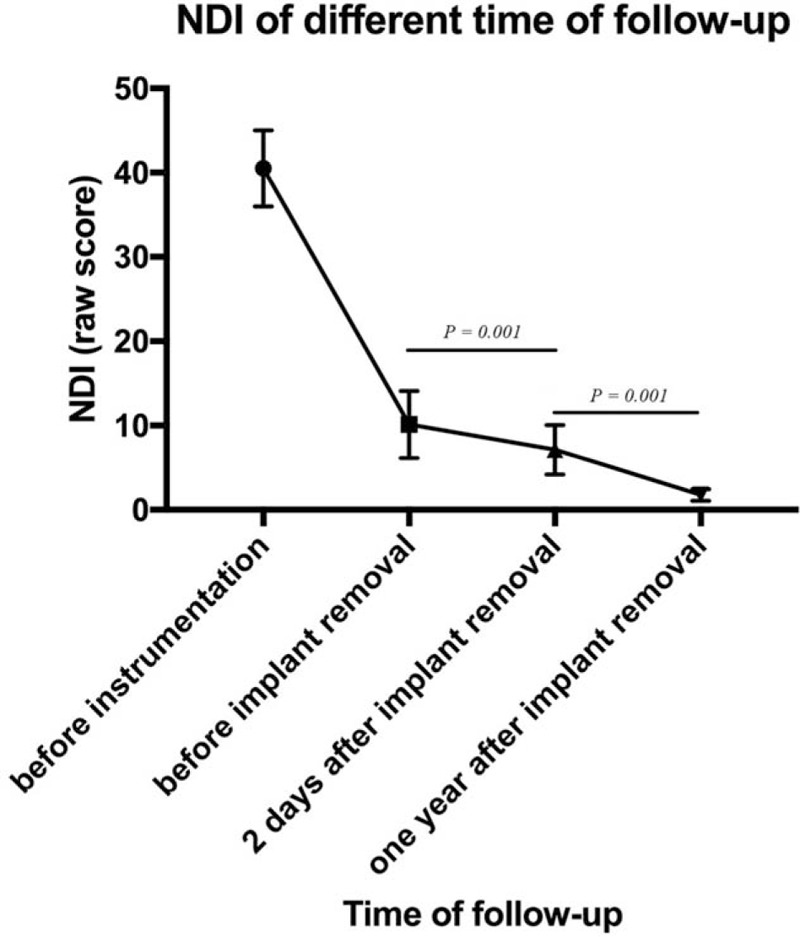
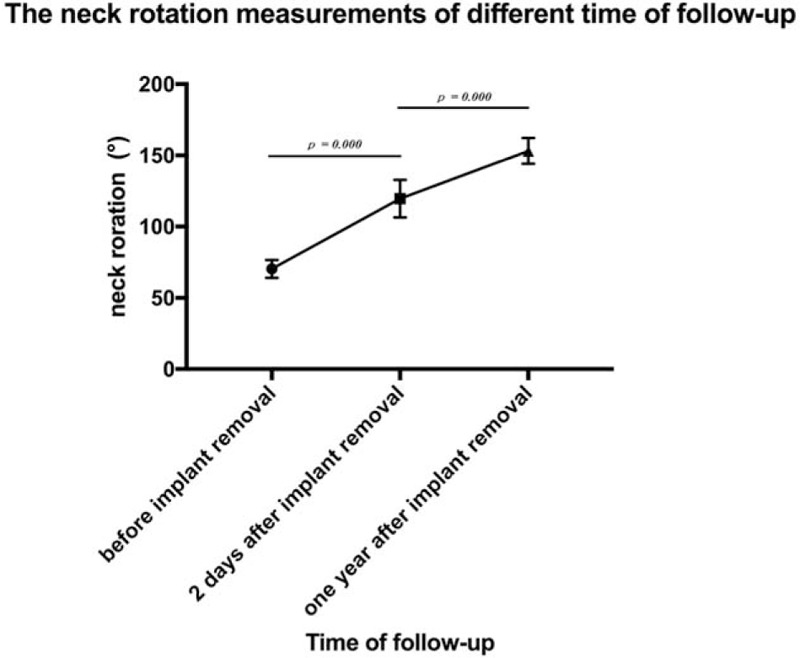
The preoperative fracture angulation and fracture translation were 4.6 ± 1.3° and 2.4 ± 0.6 mm, respectively. The average operation time and blood loss were 109 ± 27 minutes and 49 ± 15 mL. No infection, vascular injuries or neural structure injuries was observed. All patients acquired bone healing at 5.9 ± 2.0 months. The temporary instrumentation was removed at 10.8 ± 1.3 months. The average NDI before and 2 days after removal of instrumentation were 10.1 ± 4.0 and 7.1 ± 3.0, respectively. At 1-year follow-up after instrumentation removal, the NDI was 1.8 ± 0.7, which was much better than immediate NDI after instrumentation removal. The neck rotary motion (left rotation + right rotation) before and 2-day after instrumentation removal were 70.4 ± 6.3° and 119.6 ± 13.1°, respectively. At 1-year follow-up, the average neck rotary motion was 153.1 ± 9.1°, which had significant different with rotary motion 2-day after the removal of temporary instrumentation.
With regard to the high fracture fusion rates, low complications, and excellent predictable outcomes in patients treated with posterior temporary C1-2 pedicle screw fixation, the technique may be a suitable choice for 3-part fracture of the axis.
Keywords: Hangman fracture, odontoid fracture, temporary fixation, 3-part fracture
1. Introduction
Axis fracture accounts for almost 20% of all acute cervical spinal fractures. The rates of neurological deficit and acute mortality associated with axis fractures from the largest institutional series of axis fractures were 8.5% and 2.4%, respectively.[1]
For the treatment of Type II odontoid fractures (Grauer classification), it remains controversial. The reported union rate for Type II fractures treated with immobilization in either a halo vest or a sternal occipital mandibular immobilizer brace was 76%.[2] The anterior cannulated screws fixation (ACSF) is still golden standard for the treatment of Type II odontoid fractures. The reported union rates of ACSF ranged from 88% to 100%.[3–8] Posterior C1-2 fusion can provide strong fixation and acquire high rate of bone healing. However, the sacrifice of atlantoaxial rotary function is inevitable. To preserve the atlantoaxial rotary function, the C1 lateral mass (or pedicle) and C2 pedicle fixation without fusion via posterior approach has been tried. Ma et al[9] reported the preliminary outcome of posterior nonfusion screw-rod fixation for fresh Type II odontoid fracture. All the odontoid fractures acquired bony healing and the atlantoaxial rotary function recovered to the normal 6 to 12 months after the instrumentation was removed. Han et al concluded that temporary pedicle screw fixation is a feasible technique for motion preservation of Type II odontoid fractures unsuitable for anterior screw.[10]
The 3-part fracture of the axis (Type II odontoid fracture combined with Hangman fracture) is rare. Daum and Archer first reported multiple fractures to the axis consisting of an odontoid fracture with traumatic spondylolisthesis, where a halo vest was used for the treatment.[11] Korres et al[12] reported that only 9 (1%) of 674 patients (6 men and 3 women) had multiple fractures of the axis, which consisted of a combination of traumatic spondylolisthesis and an odontoid process fracture.
The reported treatment varies from conservative treatment to a variety of surgical treatments. Daum and Archer[11] and Korres et al[12] used traction and immobilization (halo vest) for the conversation treatment. The drawback of the conservative therapy is its longer duration, ranging from about 6 to 12 weeks. Koller et al[13] present a case of a combined traumatic spondylolisthesis of C2-3, fracture of the lateral mass of C2, and odontoid fracture Type IIA. The fracture was treated with simultaneous anterior arthrodesis of C2-3 and anterior screw fixation of the odontoid. Blondel et al[14] reported same method for one case of multiple fractures of the axis. Shinbo et al[15] performed surgery confined to the axis by concurrently inserting an anterior odontoid screw and posterior bilateral pedicle screws without arthrodesis of C2-3.
In this series, we present 8 cases of odontoid fracture combined with Hangman fracture. All cases were managed with posterior temporary C1-2 pedicle screw fixation. The feasibility, advantage, and disadvantage of this method for such complex fractures were analyzed.
2. Clinical materials and methods
2.1. Patient population
From March 2003 to March 2015, a total of 8 patients (7 males, 1 female) received a diagnosis of 3-part fracture of the axis (odontoid dens and Hangman fracture, Fig. 1). The average age was 42.9 ± 4.5 years (range from 27 to 66 years). The patients associated with disruption of the disc at C2/3 were excluded in this series. The injuries were caused by traffic accident in 6 cases and fall accident in 2 cases. The average time interval from injury to operation was 3.5 ± 2.1 days (range 1–7 days). There was no spinal cord injury observed in all patients. One patient was associated with tibia fracture. All patients were treated with posterior temporary C1-2 pedicle screw fixation. Table 1 shows the demographic and clinical characteristics of the patients. All patients signed informed consent for their participation in this study, which was approved by the Ethics Committee and Institution review board of the Qilu Hospital of Shandong University.
Figure 1.
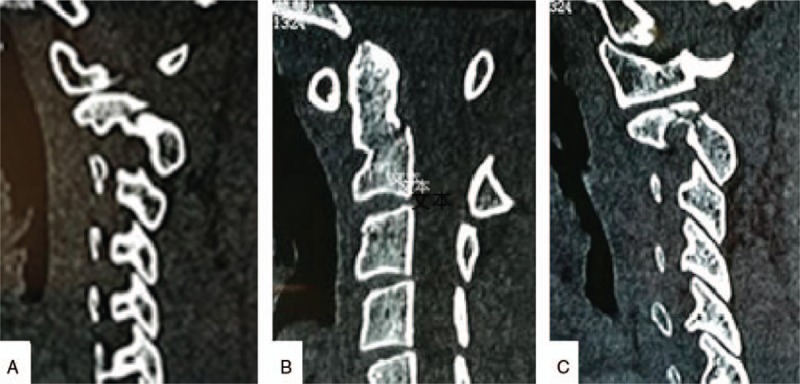
Preoperative radiology: Sagittal computed tomography reconstruction showing a combined fracture with both a Type IIC odontoid fracture (B) and bipedicular fracture (A and C).
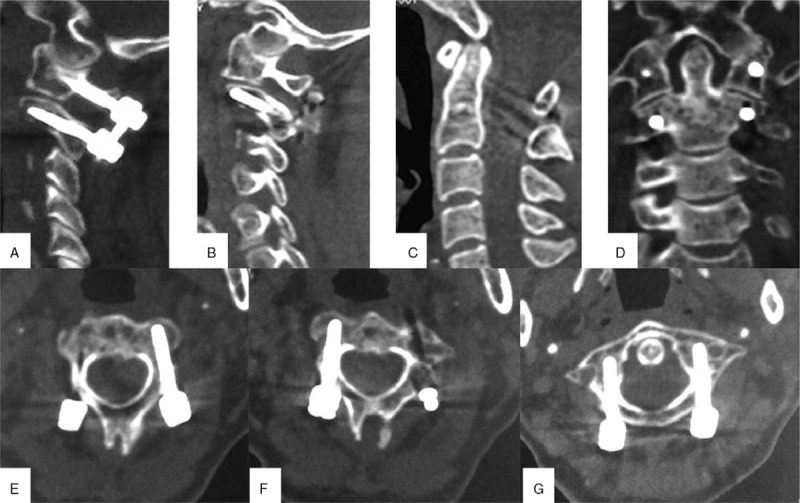
Table 1.
The demographic and clinical characteristics of the patients.
2.2. Surgical technique
General anesthesia, continuous skull traction, and neuromonitoring were used during the operations. After general anesthesia, the patients were put in prone position. A posterior midline incision about 4 to 5 cm is used. The paravertebral muscles from the spinous processes and lamina were detached to expose the surgical levels with a combination of monoplar and bipolar cautery. With a Penfield elevator, the inferior half of posterior surface of the C1 ring is exposed carefully until the entry point of C1, which is measured preoperatively on the axial CT, is visualized. The cranial aspect of the C2 pedicle is palpated using a winged-tip elevator to determine the entry point of C2. The C1-2 posterior venous plexus is remained intact to avoid bleeding.
The entry point of C2 screw is determined by palpating the medial wall of the C2 pedicle with a Penfield elevator. A 2-mm burr is used to create a starting point. The screw path is directly in line with the visualized C2 dorsal pedicle. A series of hand drills with different lengths are used to create the trajectory along the pedicle direction. After tapping, a proper length of screw is placed bilaterally. The C1 pedicle screw starting point is placed on the lower half of the posterior ring, which is close to the inferior edge of C1 ring, to maintain a safe distance to vertebral artery. A 2-mm burr is used to create the starting point. As described previously, the screw trajectory is prepared with hand drill under lateral fluoroscopy. A ball-tipped feeler is used to palpate 4 walls of the trajectory to make sure there are no breaches. The screw length is then measured, and the screw is placed. At last, the rods sized at an appropriate length were placed without arthrodesis at C1-2.
Philadelphia collar was used after surgery for 6 to 8 weeks. The temporary internal fixation was removed at 6 to 12 months if the computed tomography (CT) scans showed solid bone healing.
2.3. Radiographic measurements and clinical evaluation
X-rays, CT, and MRI prior to surgery were used to evaluate the cervical spine injury. CT angiogram was also performed preoperatively to evaluate the possible variations–anomalies of the vertebral artery. Grauer classification[16] and measurement technique described by Bono et al[17] (fracture angulation and fracture translation) were used to evaluate the fracture of dens.
Grauer classification includes 3 types of dens fracture. Type I: oblique fracture through the upper part of the odontoid process itself and probably represents an avulsion fracture where the alar ligament attaches to the tip of the odontoid process. Type II: fracture occurring at the junction of the odontoid process with the body of the second cervical vertebra. Type II is divided into 3 subtypes. Type IIA fracture is a minimally or nondisplaced fracture without comminution; Type IIB fracture line extends craniocaudal anterior–superior to posterior–inferior; Type IIC fractures extend caudocranially from anterior–inferior to posterior–superior with or without comminution. Type III is a fracture line that extends downward.
A mid-sagittal CT image was used to measure the fracture angulation and fracture translation.
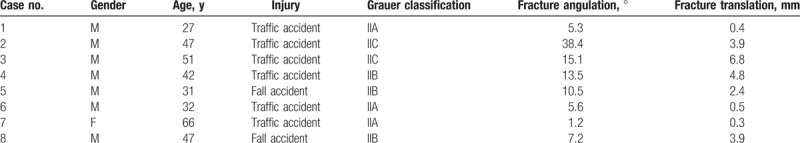
Fracture translation measurement: A tangent line is drawn along the anterior aspect of the odontoid fragment and the anterior aspect of the C2 body. At the level of the fracture, a transverse line is drawn connecting these 2 lines. This distance is measured in millimeters and represents sagittal fracture displacement. Fracture angulation measurement: A tangent line is drawn along the posterior aspect of the odontoid fragment and the posterior aspect of the C2 body. The angle subtended by these lines would be the degree of fracture angulation (Fig. 2). The neck disability index (NDI) was used to assess the neck function. The range of neck rotary motion was evaluated at each visit and calculated as the sum of right and left rotation degree.
Figure 2.
Measurements of fracture angulation and translation. (a) Fracture translation is the distance between 2 tangent lines drawn along the anterior aspect of the odontoid fragment and the anterior aspect of the C2 body at the level of the fracture. (b) Fracture angulation is the angle between 2 tangent lines drawn along the posterior aspect of the odontoid fragment and the posterior aspect of the C2 body.
All patients underwent clinical examinations at approximately 3 months, 6 months, 9 months, and annually after surgeries. All fractures were evaluated with serial X-rays and CT scans of the cervical spine at each follow-up visit. Bone fusion was considered successful if solid bony fusion, seen as trabeculation across the fracture site, was present on both X-films and sagittal and coronary reconstruction of cervical CT scans.
2.4. Statistical analysis
Statistical analysis was performed using SPSS 12.0 for windows (SPSS, IBM Corporation, Chicago). In the event of statistical significance, unpaired nonparametric test (Wilcoxon text) was performed. The level of significance was set at P < .05.
3. Results
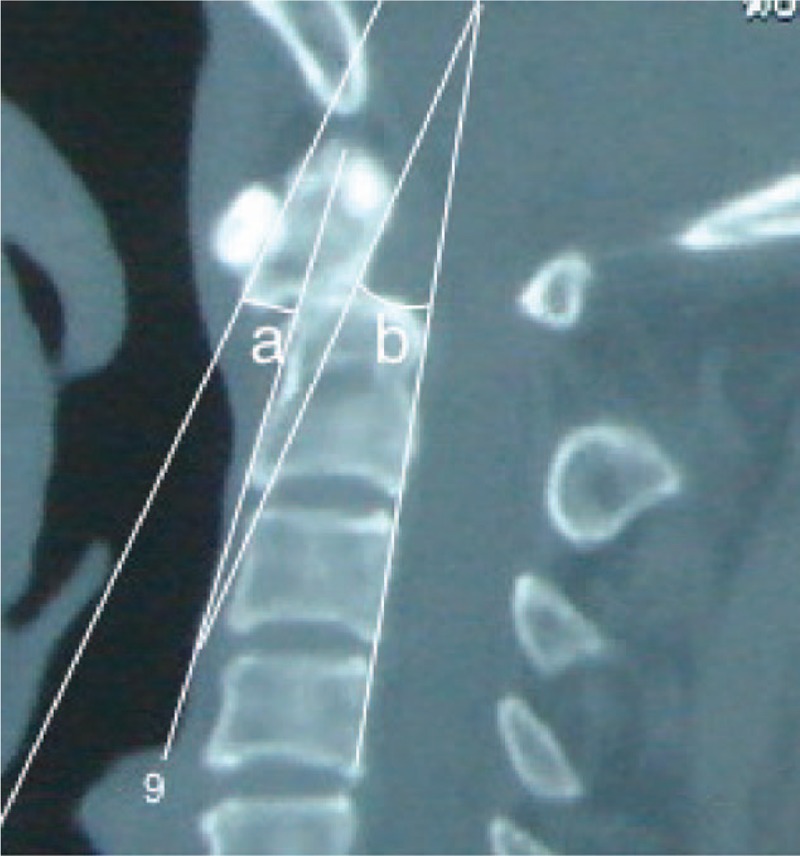
According to Grauer classification, the dens fractures were Type IIA in 3 cases, Type IIB in 3 cases, and Type IIC in 2 cases, all alar ligaments were completed. The preoperative NDI (raw score), fracture angulation, and fracture translation were 40.5 ± 4.5, 4.6 ± 1.3°, and 2.4 ± 0.6 mm, respectively. The average operation time and blood loss were 109 ± 27 minutes and 49 ± 15 mL, respectively. No infection, vascular injuries, or neural structure injuries was observed. All patients acquired bone healing at 5.9 ± 2.0 months (3–9 months), according to CT scans (Fig. 3). The temporary instrumentation was removed at 10.8 ± 1.3 months (9–13 months).
Figure 3.
Postoperative radiology: Sagittal computed tomography reconstruction obtained 6 months after surgery demonstrating good positioning of the screws (A, B, E, F, and G) and complete bone union of both pars fracture (A and B) and dens fracture (C and D).
Mean follow-up was 37 ± 12 months (range 22–60 months). After the implant was removed, the neck discomfort was partially relieved. The average NDI (raw score) before and 2 days after instrumentation removal were 10.1 ± 4.0 and 7.1 ± 3.0, respectively (P = .001). At 1-year follow-up after instrumentation removal, the NDI was 1.8 ± 0.7, which was much better than that of 2 days after instrumentation removal (P = .001). The neck rotary motion (left rotation + right rotation) before and 2-day after instrumentation removal were 70.4 ± 6.3° and 119.6 ± 13.1°, respectively (P = .000). At 1-year follow-up, the average neck rotary motion was 153.1 ± 9.1°, which had significant different with rotary motion 2-day after the removal of temporary instrumentation (P = .000) (Figs. 4 and 5). Repeated measures analysis of variance also demonstrated the NDI and neck rotary motion was significantly improved at 1 year after implant removal (P = .000).
Figure 4.
Neck rotation measurements of different time of follow-up.
Figure 5.
Neck disability index of different time of follow-up.
4. Discussion
Anderson and D’Alonzo classified odontoid fractures as Type I, II, or III.[16] The classification was modified by Grauer.[17] According to Grauer classification, the dens fractures were Type IIA in 3 cases, Type IIB in 3 cases, and Type IIC in 2 cases in this series. Single Type II fracture can be treated by external fixation (IIA), anterior screw (IIB), and posterior C1-2 fusion (IIC). As to Type II odontoid fracture combined with Hangman fracture, the treatment remains controversial. In this series, all cases were managed with posterior temporary C1-2 pedicle screw fixation. There were a few advantages to using this technique for such cases.
First, posterior internal screw fixation gives immediate direct fixation of the fracture and offers a high rate of fusion without requiring prolonged halo vest immobilization. In 2001, Harms and Melcher described C1 lateral mass and C2 pedicle screws used to achieve posterior atlantoaxial stabilization with polyaxial screw-rod system.[7] Biomechanically, the overall rigidity achieved using this technique is similar to that achieved with transarticular screws. In this series, all patients acquired bone healing at 3 to 9 months after surgeries. We chose pedicle screws instead of lateral mass screws for C1 temporary fixation. C1 pedicle screw has a few advantages than lateral mass screw: pedicle screws have superior resistance to pullout via axial load compared with lateral mass screws in the atlas[18]; C1 pedicle screw does not require extensive dissection to expose the C1 lateral mass for screw placement, this technique decreased occipital neuralgia and blood loss.[19]
Second, posterior temporary C1-2 pedicle screw fixation preserves the normal mobility of C1-2. Traditional bony fusion of C1-2 was canceled to preserve the atlantoaxial rotary function. Guo et al[20] compared clinical results of 22 patients who underwent posterior C1-2 temporary fixation of an odontoid fracture and 21 patients treated with posterior C1-2 fixation and fusion. Significantly better outcomes were observed in the temporary-fixation group for visual analog scale score for neck pain, NDI, and neck stiffness. The outcomes in the temporary-fixation group were superior to those in the fusion group in all dimensions of the 36-Item Short Form Health Survey. There were no significant differences in fracture healing rate and time to fracture healing between the 2 techniques. In our study, the neck disability caused by posterior fixation was obvious. The average NDI (raw score) before and 2 days after instrumentation removal were 10.1 ± 4.0 and 7.1 ± 3.0, respectively. The neck rotary range was obviously limited and decreased to 70.4 ± 6.3°. After the implant was removed, the neck rotary function was immediately improved to 119.6 ± 13.1°. At 1-year follow-up, the neck rotary function and NDI were significantly improved.
Third, posterior temporary C1-2 pedicle screw fixation can be used in some cases which are not suitable for ACSF. Anterior screw was first reported in 1980 by Nakanishi. The reported union rates of surgical treatment ranged from 88% to 100%.[6–8,21] There is a number of advantages including immediate stabilization, less postoperative pain, no requirement for bone graft, and preservation of the normal atlantoaxial rotational movement. However, there are also a few contraindications for anterior fixation. Type IIC dens fracture provides only a small part of the C2 body for anchorage of the screw and the fracture line parallel to the screw trajectory can easily result in anterior displacement of the fragment under compression, and significantly more likely to result in nonanatomical union, nonunion, or fibrous union than posterior oblique and horizontally oriented fractures.[22] Moreover, contraindications of odontoid screws also included fracture comminution, severe cardiothoracic kyphosis, severe osteoporosis, late fractures, and ligament transverse rupture.[23] Posterior temporary C1-2 pedicle screw fixation is an appropriate option for such cases. In this series, 1 Type IIC dens fracture with Hangman fracture was successfully treated by this technique. According to our data (unpublished), bone-healing rate of Type IIC dens fracture was much better than anterior screws (96% vs. 90.6%, P < .05).
There are some shortcomings of posterior temporary C1-2 pedicle screw fixation for 3-part fracture of the axis: The patients need second surgery to remove the instrumentation. After temporary fixation, it eliminates the normal C1-2 rotatory motions, which is responsible for approximately 54.03% of cervical rotary motion according to our data; cervical rotary motion may be affected by temporary fixation even after hardware removal. The patients may need a long time to recover to the normal motions. In this series, the neck rotary motion 2-day after instrumentation removal was only 119.6 ± 13.1°. At 1-year follow-up, the average neck rotary motion was improved to 153.1 ± 9.1°; this technique cannot be used for the treatment of the patients associated with disruption of the disc at C2/3; although all cases in this series were treated successfully, complications of posterior fixation may include blood loss, vertebral artery injury, infection, and others according to the literature.[23] The present study is a retrospective case series study that only included 8 patients, the study design and the small sample size may be a major limitation of the strength of the conclusion. Further researches with large sample size or with the design of prospective randomized control trial may be more convincing for clinical implication.
5. Conclusions
With regard to the high fracture fusion rates, low complications, and excellent predictable outcomes in patients treated with posterior temporary C1-2 pedicle screw fixation, the technique may be a suitable choice for 3-part fracture of the axis.
Author contributions
Data curation: Suomao Yuan, Bin Wei, Yonghao Tian.
Formal analysis: Suomao Yuan, Bin Wei, Yonghao Tian.
Funding acquisition: Lianlei Wang, Xinyu Liu.
Investigation: Suomao Yuan, Bin Wei, Jun Yan, Wanlong Xu, Lianlei Wang, Xinyu Liu.
Methodology: Suomao Yuan, Bin Wei, Jun Yan, Wanlong Xu, Lianlei Wang, Xinyu Liu.
Resources: Yonghao Tian.
Software: Bin Wei, Yonghao Tian, Jun Yan, Wanlong Xu.
Supervision: Yonghao Tian, Wanlong Xu, Lianlei Wang, Xinyu Liu.
Writing – original draft: Suomao Yuan.
Writing – review & editing: Suomao Yuan, Xinyu Liu.
Footnotes
Abbreviations: ACSF = anterior cannulated screws fixation, NDI = neck disability index.
This study is supported by the National Natural Science Foundation of China (project number 81272024). We did not receive payments or other benefits or a commitment or agreement to provide such benefits from any commercial entity.
SY and BW contributed equally to this study.
The authors have no conflicts of interest to disclose.
References
- [1].Greene KA, Dickman CA, Marciano FF, et al. Acute axis fractures. Analysis of management and outcome in 340 consecutive cases. Spine 1997;22:1843–52. [DOI] [PubMed] [Google Scholar]
- [2].Harms J, Melcher RP. Posterior C1-C2 fusion with polyaxial screw and rod fixation. Spine 2001;26:2467–71. [DOI] [PubMed] [Google Scholar]
- [3].Govender S, Maharaj JF, Haffajee MR. Fractures of the odontoid process. J Bone Joint Surg Br 2000;82:1143–7. [DOI] [PubMed] [Google Scholar]
- [4].Coyne TJ, Fehlings MG, Wallace MC, et al. C1-C2 posterior cervical fusion: long-term evaluation of results and efficacy. Neurosurgery 1995;37:688–92. [DOI] [PubMed] [Google Scholar]
- [5].Marcotte P, Dickman CA, Sonntag VK, et al. Posterior atlantoaxial facet screw fixation. J Neurosurg 1993;79:234–7. [DOI] [PubMed] [Google Scholar]
- [6].Grob D, Jeanneret B, Aebi M, et al. Atlanto-axial fusion with transarticular screw fixation. J Bone Joint Surg Br 1991;73:972–6. [DOI] [PubMed] [Google Scholar]
- [7].Apfelbaum RI, Lonser RR, Veres R, et al. Direct anterior screw fixation for recent and remote odontoid fractures. J Neurosurg 2000;93suppl:227–36. [DOI] [PubMed] [Google Scholar]
- [8].Henry AD, Bohly J, Grosse A. Fixation of odontoid fractures by an anterior screw. J Bone Joint Surg Br 1999;81:472–7. [DOI] [PubMed] [Google Scholar]
- [9].Xiangyang M, Jincheng Y, Qingshui Y, et al. The primary outcome of posterior nonfusion screw-rod fixation for preserving the atlantoaxial rotary function due to fresh type II odontoid fracture. Chinese J Spine Spinal Cord 2013;23:411–5. [Google Scholar]
- [10].Han B, Li F, Chen G, et al. Motion preservation in type II odontoid fractures using temporary pedicle screw fixation: a preliminary study. Eur Spine J 2015;24:686–93. [DOI] [PubMed] [Google Scholar]
- [11].Daum W, Archer CR. Fracture of the odontoid associated with pedicle fracture of the axis: a previously undescribed entity. J Trauma 1977;17:381–6. [DOI] [PubMed] [Google Scholar]
- [12].Korres DS, Papagelopoulos PJ, Mavrogenis AF, et al. Multiple fractures of the axis. Orthopedics 2004;27:1096–9. [DOI] [PubMed] [Google Scholar]
- [13].Koller H, Assuncao A, Kammermeier V, et al. Simultaneous anterior arthrodesis C2-3 and anterior odontoid screw fixation for stabilization of a 4-part fracture of the axis—a technical description. J Spinal Disord Tech 2006;19:362–7. [DOI] [PubMed] [Google Scholar]
- [14].Blondel B, Metellus P, Fuentes S, et al. Single anterior procedure for stabilization of a three-part fracture of the axis (odontoid dens and Hangman fracture): case report. Spine 2009;34:E255–7. [DOI] [PubMed] [Google Scholar]
- [15].Shinbo J, Sameda H, Ikenoue S, et al. Simultaneous anterior and posterior screw fixations confined to the axis for stabilization of a 3-part fracture of the axis (odontoid, dens, and Hangman fractures): report of 2 cases. J Neurosurg Spine 2014;20:265–9. [DOI] [PubMed] [Google Scholar]
- [16].Anderson LD, D’Alonzo RT. Fractures of the odontoid process of the axis. J Bone Joint Surg Am 1974;56:1663–74. [PubMed] [Google Scholar]
- [17].Grauer JN, Shafi B, Hilibrand AS, et al. Proposal of a modified, treatment-oriented classification of odontoid fractures. Spine J 2005;5:123–9. [DOI] [PubMed] [Google Scholar]
- [18].Zarro CM, Ludwig SC, Hsieh AH, et al. Biomechanical comparison of the pullout strengths of C1 lateral mass screws and C1 posterior arch screws. Spine J 2013;13:1892–6. [DOI] [PubMed] [Google Scholar]
- [19].Pan J, Li L, Qian L, et al. C1 lateral mass screw insertion with protection of C1-C2 venous sinus: technical note and review of the literature. Spine 2010;35:E1133–6. [DOI] [PubMed] [Google Scholar]
- [20].Guo Q, Deng Y, Wang J, et al. Comparison of clinical outcomes of posterior C1-C2 temporary fixation without fusion and C1-C2 fusion for fresh odontoid fractures. Neurosurgery 2016;78:77–83. [DOI] [PubMed] [Google Scholar]
- [21].Song GS, Theodore N, Dickman CA, et al. Unilateral posterior atlantoaxial transarticular screw fixation. J Neurosurg 1997;87:851–5. [DOI] [PubMed] [Google Scholar]
- [22].Denaro V, Papalia R, Di Martino A, et al. The best surgical treatment for type II fractures of the dens is still controversial. Clin Orthop Relat Res 2011;469:742–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Joaquim AF, Patel AA. Surgical treatment of type II odontoid fractures: anterior odontoid screw fixation or posterior cervical instrumented fusion? Neurosurg Focus 2015;38:E11. [DOI] [PubMed] [Google Scholar]


