Abstract
Background:
Acute perioperative hypertension has been associated with poor outcomes of surgery, and the role of calcium channel blockers (CCB) on controlling perioperative blood pressure (BP) remains controversial. Thus, this meta-analysis was designed to assess the efficacy and safety of CCB in treating perioperative hypertension compared with other antihypertensive agents.
Methods:
PubMed, Medline, Cochrane, and EMABSE databases was systematically searched up to January 2018 for randomized control trials (RCTs) or other control studies comparing the efficacy of CCB versus other antihypertensive medicines for perioperative hypertension modulation. The efficacy and safety of CCB in treating perioperative hypertension were assessed through pooling mean difference (MD) with its 95% confidence interval (CI) or risk ratio (RR) with its 95% CI.
Results:
In total, 14 studies were included in the meta-analysis. There is no significant difference regarding successful treatment (RR = 2.64, 95% CI: 0.95, 7.29; I2 = 97%, P <.05), systolic blood pressure (SBP) (MD = −7.05, 95% CI: −16.27, 2.17; I2 = 78%, P <.05), overall adverse events (RR = 0.88, 95% CI: 0.66, 1.16; I2 = 54%, P = .02), atrial fibrillation (RR = 0.80, 95% CI: 0.60, 1.07; I2 = 32%, P = .20) and heart rates (MD = −1.05, 95% CI: −7.81, 5.71; I2 = 84%, P < .05) between patients treated by CCB and other drugs. In the subgroup analysis, statistical significance can be observed regarding successful treatment (RR = 3.46, 95%CI: 1.67, 7.18; I2 = 84%, P <.05) and postoperative SBP (MD = −9.98, 95%CI: −20.03, 0.08; I2 = 97%, P <.05) in the RCTs subgroup.
Conclusion:
CCB was highly effective and well tolerated for treating perioperative hypertension.
Keywords: calcium channel blockers, hypertension, meta-analysis, perioperative period
1. Introduction
According to a report by the Centers for Disease Control and Prevention, 1 of every 3 Americans has hypertension,[1] which represents one of the most prevalent pathology worldwide. And perioperative blood pressure (BP) has been recognized as one of the main factors associated with worse outcomes, such as acute end-organ damage.[2] Up to 80% of patients undergoing cardiac surgeries and 25% of patients undergoing non-cardiac procedures was affected by acute perioperative hypertension.[3] Moreover, the performance of surgery might be postponed when pre-existing hypertension occurred.
Calcium channel blockers (CCBs) are a kind of drug inhibiting the flow of extracellular calcium through ion-specific channels that span the cell wall. There are 2 kinds of frequently used CCB with different effects on vasodilation and myocardium inotropism. One is dihydropyridines including clevidipine, amlodipine, felodipine, isradipine, lacidipine, nicardipine, nifedipine, and nisoldipine, which decreases BP by dilating arterial vascular tree. Another is nondihydropyridines including diltiazem, and verapamil, which perform by reducing heart rate, contractility, and slightly increasing arteriodilation.[4] As the development of technology, some new drug belongs to CCB has been researched.[5]
The BP-lowering effect of CCB combinations are supported by long-term evidence, but CCB has not yet been widely used in clinical practice.[6] Several studies have shown the potency of CCB in BP maintenance.[7] For example, by meta-analysis, Espinosa et al put forward that clevidipine play highly effective role for management of perioperative arterial hypertension.[8] Additionally, other CCBs, such as nicardipine and perdipine, has also been assessed the role of managing perioperative arterial hypertension in clinical evidence.[9] However, CCB has not been assessed as a whole for its role in hypertensive management.
In this study, we hypothesized that CCB was a better kind of medicine for lowering BP on perioperative hypertension comparing with other antihypertensive agents. Thus, this meta-analysis was designed to assess the efficacy and safety of CCB in treating perioperative hypertension compared with other antihypertensive agents.
2. Material and methods
This article was undertaken followed the PRISMA Guidelines for meta-analysis. Since this is a meta-analysis, ethical approval is no applicable.
2.1. Search strategy
Relevant articles published in English before January 2018 were systematically searched throughout PubMed, Medline, Cochrane, and EMABSE databases. The main key words used for the search were as follows: “Calcium channel blockers” or “CCB” or “nifedipine” or “amlodipine” or “lercanidipine” or “nimodipine” or “nicardipine” or “nitrendipine” or “nisoldipine” or “felodipine” or “benidipine” or “lacidipine” or “barnidipine” or “lercanidipine” or “clevidipine” or “benzothiazole” or “diltiazem” or “phenylalkylamines” or “verapamil” or “triphenylpiperazine” or “siberlium” or “flunarizine” or “cinnarizine” or “lidoflazine” and “blood pressure” or “hypertension”.
2.2. Selection criteria
Randomized control trials (RCTs) or non-randomized control trials (non-RCTs) published in English conforming to the following selection criteria were enrolled in the meta-analysis:
-
(1)
patients were diagnosed with hypertension during the surgery;
-
(2)
the efficacy of CCBs in BP control during perioperative period was evaluated;
-
(3)
adverse events regarding the treatment were reported;
-
(4)
treatment success was defined as the ability to decrease systolic blood pressure (SBP) by 15% from baseline in the study.[10]
Studies would be excluded if data within could not be used for statistical analysis. In addition, the non-original studies included reviews, letters, and comments were also excluded.
All titles and abstracts from the initial search were screened by reviewers. If the title and abstract did not contain enough information to include or excluded the study from the analysis, the study was reviewed in full-text. Citation lists of relevant articles and reviews were additionally scanned to identify further studies of interest.
2.3. Data extraction and quality assessment
Data extraction was performed by the 2 investigators independently, and the extraction form was previously designed. Discrepancies were resolved by referring the original articles. The information, including the first author's name, year of publication, number, and age of the enrolled patients, region, follow-up duration, the design of the included trails, and intervention method was extracted.
According to the Cochrane Handbook of Systematic Review of Interventions, RCTs were assessed by using Review Manager 5.3 based on seven perspectives (random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting, and others) and scored as unclear, low, or high risk of bias (Fig. 1). The Newcastle-Ottawa Scale (NOS) with a maximum of 9 points was applied to evaluate the quality of non-RCTs with three categories for scoring: selection of the study groups, quality of the adjustment for confounding and ascertainment of the outcome of interest in the cohorts.
Figure 1.
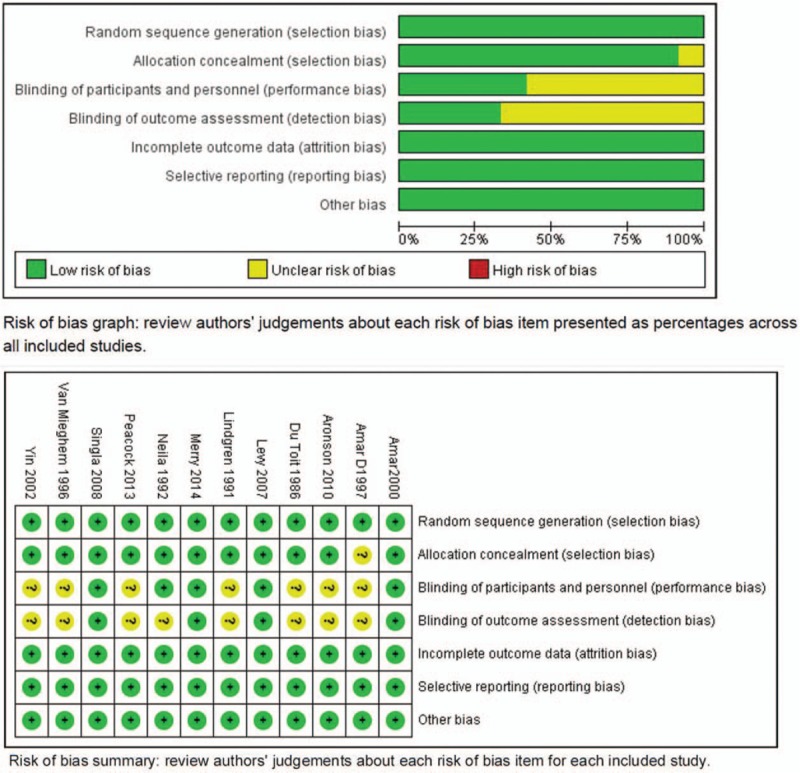
Bias assessment of RCTs. Low risk of bias can be detected across all the studies. RCT = randomized control trial.
2.4. Statistical analyses
Statistical analyses were performed by Review Manager 5.3 (The Nodic Cochrane Centre, The Cochrane Collaboration, Copenhagen, Denmark, 2014). Dichotomous data were analyzed by risk ratio (RR) for RCTs and odd ratio (OR) for non-RCTs with its 95% confidence interval (CI), including the prevalence of successful success rate and the rate of adverse events occurrence. Continuous data were analyzed by mean difference (MD) with its 95% CI. Heterogeneity among individual studies was examined by Cochran's Q statistic and I2 test. Significant heterogeneity occurred if P value <.05 (Q statistic) and/or I2 > 50%, and then the random effects model was selected, otherwise, the fixed effect model would be used. Sensitivity analysis was performed to confirm the robustness of the results through omitting 1 study at a time.
3. Results
3.1. Studies selection
As shown in Figure 2, according to the search criteria, 15899 articles were identified and 6630 were originally enrolled, with 6619 from database searching and 11 from manual searching in citation lists. In total, 1432 articles were remained after eliminating duplicates and obvious irrelevance. After that, 1241 studies were excluded for non-control studies and low relevance. Then 47 articles were fully assessed. After checking the full texts, 33 articles were excluded, including 20 articles without raw data and 13 articles without valuable endpoints. Finally, 14 eligible studies were included in this meta-analysis.[7,10–22]
Figure 2.
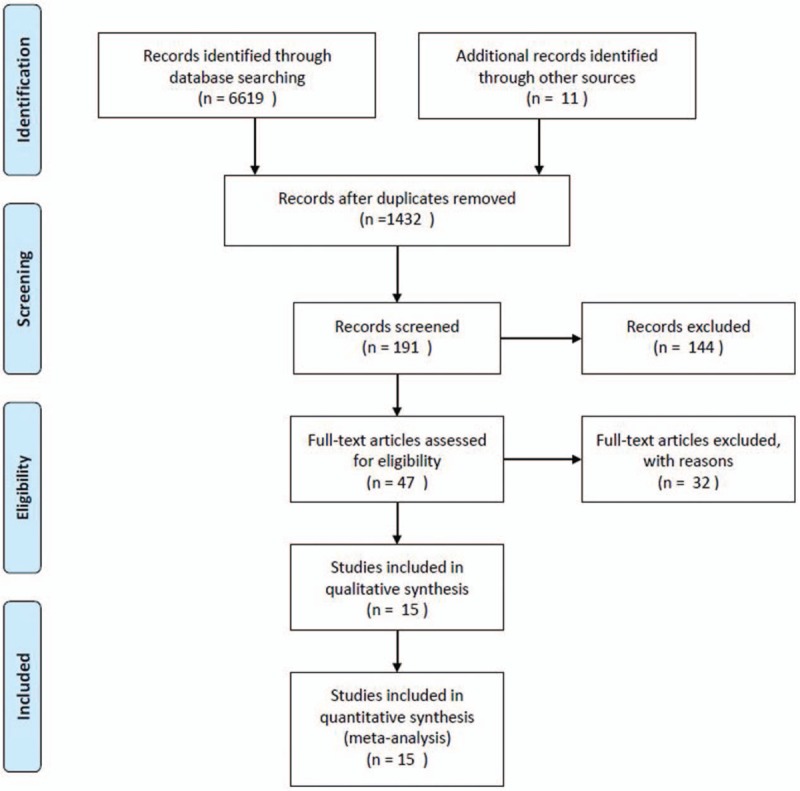
Flow chart of selection process.
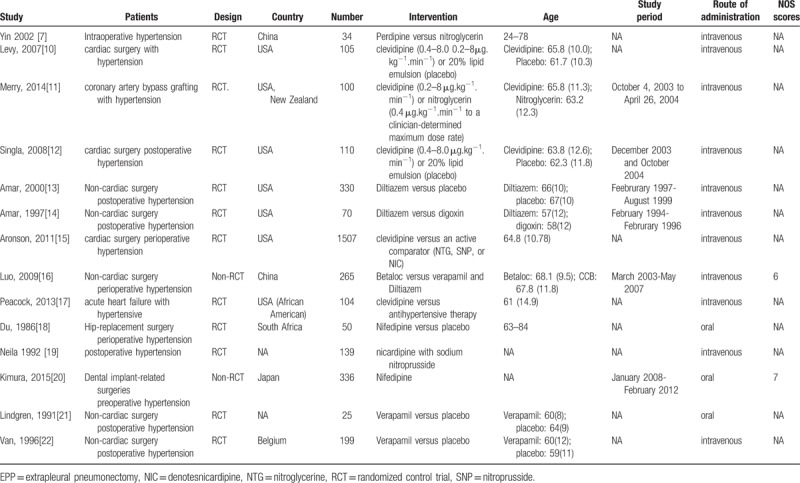
3.2. Characteristics and quality of the enrolled studies
Table 1 shows the basic information of the meta-analysis. All included studies were published from 1986 to 2015. Among the enrolled 14 studies, patients in 7 studies were from America. 6 studies researched on clevidipine, 2 studies on nicardipine or perdipine, 3 studies on diltiazem, 2 studies on nifedipine, 3 studies on verapamil. Most of the control groups of the included studies received placebo. In addition, four studies were muti-center studies. Twelve studies were assessed by Revman 5.3, and risk of bias in all studies is low. Only 2 studies are non-RCTs assessed by NOS, and the scores were all more than 5.
Table 1.
Characteristics of 14 included studies.
3.3. Analysis of antihypertensive effect: CCB versus control
Four studies[10,12,16,17] with a total of 449 participants reported the number of patient with successful treatment. As shown in Figure 3.1, significant heterogeneity was observed among enrolled studies (I2 = 97%, P <.05), therefore effect size was pooled under random effects model. There is no significant difference between CCB and the control group (RR = 2.64, 95% CI: 0.95, 7.29).
Figure 3.
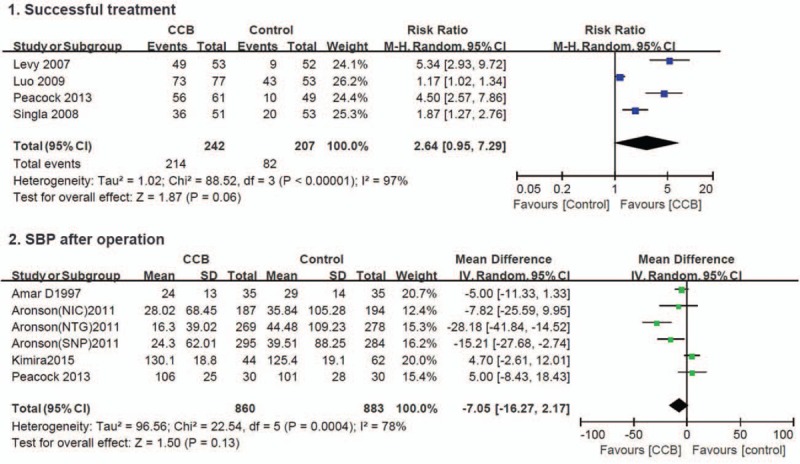
Forest plot of the efficacy of CCBs versus other medicines. Four studies with a total of 449 participants reported the number of patient with successful treatment. Significant heterogeneity was observed among enrolled studies (I2 = 97%, P <.05). No significant difference between CCB and the control group (RR = 2.64, 95% CI: 0.95, 7.29). CCB = calcium channel blockers, CI = confidence interval, RR = risk ratio.
Four studies[14,15,17,20] with a total of 1743 participant reported postoperative SBP, as shown in Figure 3.2. Significant heterogeneity was observed among the enrolled studies (I2 = 78%, P <.05), therefore effect size was pooled under random effects model. No significant difference was detected in patients treated by CCB versus patients treated by other antihypertensives (MD = −7.05, 95% CI: −16.27, 2.17).
3.4. Adverse events
Ten studies[10–14,17–19,21,22] with a total of 1231 participants reported overall adverse events. Significant heterogeneity occurred among the enrolled studies (I2 = 54%, P = .02), therefore random effects model was adopted. No significant difference was observed on adverse events for hypertensive patients treated by CCB versus other strategies (RR = 0.88, 95% CI: 0.66, 1.16). The result remained unchanged after sensitivity analysis. Details are shown in Figure 4.1. Since there are enough studies regarding overall adverse events, we generated a funnel plot to visualize the bias and heterogeneity. As shown in Figure 5, the distribution of the studies is very symmetric indicating low risk of bias and heterogeneity, except the study by Lindgre.
Figure 4.
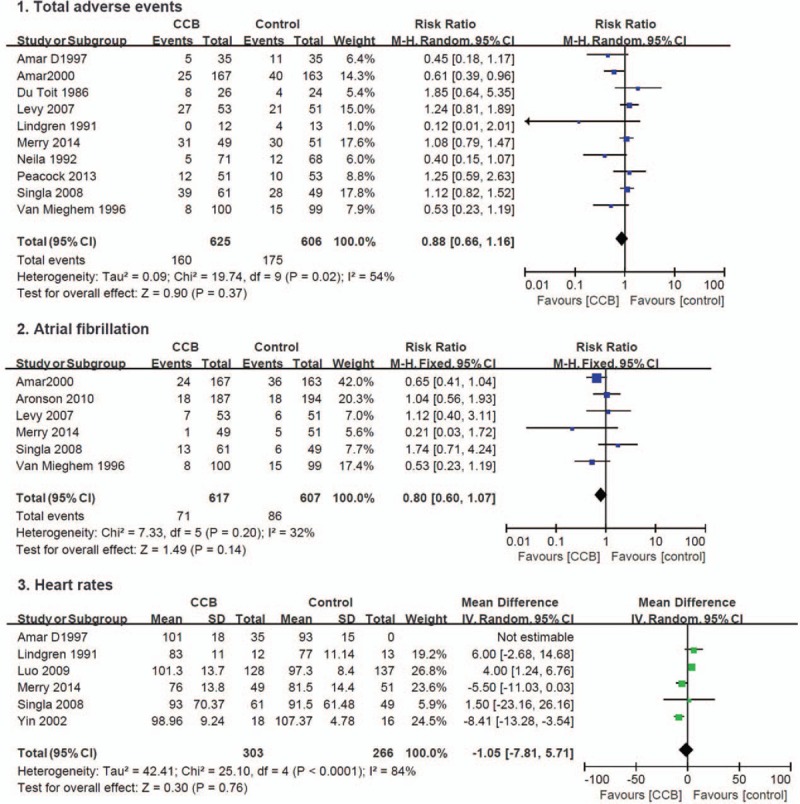
Forest plot of the adverse events of CCBs versus other medicines. 4.1 Total adverse events. Ten studies with a total of 1231 participants reported overall adverse events. Significant heterogeneity occurred among the enrolled studies (I2 = 54%, P = .02). No significant difference was observed on adverse events for hypertensive patients treated by CCB versus other strategies (RR = 0.88, 95% CI: 0.66, 1.16). 4.2 Atrial fibrillation. Six studies with a total of 1224 participants reported atrial fibrillation, which is one of the most common adverse events. No significant heterogeneity was found (I2 = 32%, P = .20). There no statistical difference was observed between the 2 groups regarding the prevalence of atrial fibrillation ((RR = 0.80, 95% CI: 0.60, 1.07). 4.3 Heart rates. Six studies with a total of 569 participants referred heart rate after surgery. Significant heterogeneity was observed among studies (I2 = 84%, P <.05). No significant difference on heart rates between CCB and other antihypertensive measures (MD = −1.05, 95% CI: −7.81, 5.71). CCB = calcium channel blockers, CI = confidence interval, MD = mean difference.
Figure 5.
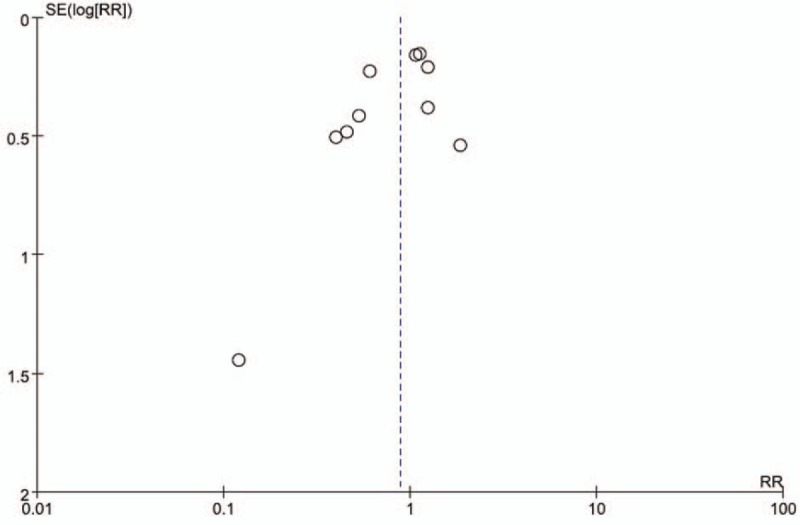
Funnel plot of adverse events. Low risk of bias and heterogeneity can be detected except the study by Lindgre.
Six studies with a total of 1224 participants reported atrial fibrillation, which is one of the most common adverse events. No significant heterogeneity was found (I2 = 32%, P = .20), therefore fixed effects model was used. There no statistical difference was observed between the two groups regarding the prevalence of atrial fibrillation ((RR = 0.80, 95% CI: 0.60, 1.07). However, the diamond of pooled point would favor CCB group and the heterogeneity would be less if excluded Singla et al's study[12] (RR = 0.72, 95% CI: 0.53, 0.99, I2 = 3%, P = .39). Details are presented in Figure 4.2.
Six studies[7,11,12,14,16,21] with a total of 569 participants referred heart rate after surgery. Significant heterogeneity was observed among studies (I2 = 84%, P <.05), therefore random effect model was employed. Figure 4.3 shows that there is no significant difference on heart rates between CCB and other antihypertensive measures (MD = −1.05, 95% CI: −7.81, 5.71), and the result remained unchanged after sensitivity analysis.
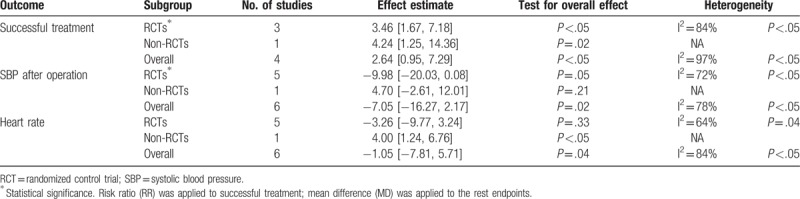
3.5. Subgroup analysis
Subgroup analysis was performed by stratified the studies into RCTs subgroup and non-RCTs subgroup. Significant difference can be observed regarding successful treatment (RR = 3.46, 95% CI: 1.67, 7.18; I2 = 84%, P <.05) and postoperative SBP (MD = −9.98, 95% CI: −20.03, 0.08; I2 = 72%, P <.05) in the RCTs subgroup. However, no significant difference can be detected in terms of total adverse events, atrial fibrillation, and heart rate. Details are presented in Table 2.
Table 2.
Subgroup analysis of successful treatment, SBP after operation and heart rate.
4. Discussion
This meta-analysis found that CCB can significantly decreased perioperative BP and would not lead to serious adverse events compared with other antihypertensive drugs, which indicate its high effectiveness and well tolerance in with the treatment of perioperative hypertension.
In the combined analysis of successful treatment and SPB, no significant difference can be detected between the 2 groups, but CCB group still had high prevalence of successful treatment and lower SBP than the control group. Furthermore, in the subgroup analysis by stratified the studies into RCTs and non-RCTs groups, we found that more CCB-treated patients received successful treatment that the SBP was decreased by 15% from the baseline with lower SBP compared with those received other medicines in RCTs subgroup, which was consistent with previous researches.
Adverse events were assessed from the time of drug initiation to hospital discharge or 7 days postoperatively. Common adverse effects of CCBs include edema, flushing, headache, dizziness, constipation (particularly with high-dose verapamil), nausea, rash, and drowsiness.[23,24] Although there is no significant difference between CCB group and the control group regarding overall adverse events, atrial fibrillation, and heart rate, statistical significance can be detected with lower heterogeneity regarding atrial fibrillation if excluded Singal et al's study.[12] We further went through this study, and a potential explanation for such difference may be the larger population of valvular surgery in the CCB group who were at increased risk for postoperative complications.[25] As shown in the funnel plot, the study by Lindgren[21] may higher risk of bias and heterogeneity than other studies, which may account for the small number of patients.
There are some limitations should be noted in this meta-analysis. Although the evaluation criteria was in line with each other, significant heterogeneity was still observed on most endpoints. The natural condition, including the background of the patients, the technology and experience of the examining doctor, and the dose of the drugs might be one source of such heterogeneity.[26,27] Moreover, five kinds of CCBs were included in the meta-analysis and different types of drugs may have different antihypertensive efficiency and adverse effect, which may also be the source of heterogeneity. In addition, according to the limited data of included studies, subgroup analysis stratified by the kinds of CCB could not be performed. These limitations may compromise the reliability of our findings; therefore this study demonstrated the possible effect and adverse events of CCBs on perioperative hypertension.
5. Conclusions
We performed a meta-analysis to assess the efficacy of CCBs in the treatment of perioperative hypertension, and to our knowledge, this is the first meta-analysis with various CCBs on perioperative BP management. Our results demonstrated that CCBs may be effective for treating perioperative hypertension with a good safety profile compared with other medicines, which should be encouraged for hypertensive patients who would undergo surgery.
Author contributions
Conceptualization: Yu Lin.
Data curation: Yu Lin.
Formal analysis: Lina Ma.
Methodology: Lina Ma.
Software: Lina Ma.
Writing – original draft: Yu Lin.
Footnotes
Abbreviations: BP = blood pressure, CCB = calcium channel blockers, CI = confidence interval, MD = mean difference, NOS = Newcastle-Ottawa Scale, RCTs = randomized control trials, RR = risk ratio, SBP = systolic blood pressure.
YL and LM contributed equally to this work.
The authors report no conflicts of interest.
References
- [1].Merai R, Siegel C, Rakotz M, et al. CDC grand rounds: a public health approach to detect and control hypertension. MMWR Morb Mortal Wkly Rep 2016;65:1261–4. [DOI] [PubMed] [Google Scholar]
- [2].Takamatsu Y. History of clinical research and education in hematological diseases by the Kyushu hematology organization for treatment study group. Rinsho Ketsueki 2008;49:483–8. [PubMed] [Google Scholar]
- [3].Awad AS, Goldberg ME. Role of clevidipine butyrate in the treatment of acute hypertension in the critical care setting: a review. Vasc Health Risk Manag 2010;6:457–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Weber MA, Schiffrin EL, White WB, et al. Clinical practice guidelines for the management of hypertension in the community. J Clin Hypertens 2014;16:14–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Cheng XL, He JG, Liu ZH, et al. Pulmonary vascular capacitance is associated with vasoreactivity and long-term response to calcium channel blockers in idiopathic pulmonary arterial hypertension. Lung 2016;194:613–8. [DOI] [PubMed] [Google Scholar]
- [6].Lu Z, Chen Y, Li L, et al. Combination therapy of renin|[ndash]|angiotensin system inhibitors plus calcium channel blockers versus other two-drug combinations for hypertension: a systematic review and meta-analysis. J Hum Hypertens 2017;31:1–3. [DOI] [PubMed] [Google Scholar]
- [7].Chuang SY, Pan WH, Chang HY, et al. Protective effect of calcium channel blockers against frailty in older adults with hypertension. J Am Geriatr Soc 2016;64:1356–8. [DOI] [PubMed] [Google Scholar]
- [8].Espinosa A, Ripollésmelchor J, Casansfrancés R, et al. Perioperative use of clevidipine: a systematic review and meta-analysis. PLoS One 2016;11:e0150625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Mastropietro CW, Arango UD. Nicardipine for hypertension following aortic coarctectomy or superior cavopulmonary anastomosis. World J Pediatr Congenit Heart Surg 2016;7:32–5. [DOI] [PubMed] [Google Scholar]
- [10].Levy JH, Mancao MY, Gitter R, et al. Clevidipine effectively and rapidly controls blood pressure preoperatively in cardiac surgery patients: the results of the randomized, placebo-controlled efficacy study of clevidipine assessing its preoperative antihypertensive effect in cardiac surgery-1. Anesth Analg 2007;105:918–25. [DOI] [PubMed] [Google Scholar]
- [11].Merry AF, Avery EG, Nussmeier NA, et al. Clevidipine compared with nitroglycerin for blood pressure control in coronary artery bypass grafting: a randomized double-blind study. Can J Anesth 2014;61:398–406. [DOI] [PubMed] [Google Scholar]
- [12].Singla N, Warltier DC, Gandhi SD, et al. Treatment of acute postoperative hypertension in cardiac surgery patients: an efficacy study of clevidipine assessing its postoperative antihypertensive effect in cardiac surgery-2 (ESCAPE-2), a randomized, double-blind, placebo-controlled trial. Anesth Analg 2008;107:59–67. [DOI] [PubMed] [Google Scholar]
- [13].Amar D. Effects of diltiazem prophylaxis on the incidence and clinical outcome of atrial arrhythmias after thoracic surgery. J Thorac Cardiov Sur 2000;120:790–8. [DOI] [PubMed] [Google Scholar]
- [14].Amar D, Roistacher N, Burt ME, et al. Effects of diltiazem versus digoxin on dysrhythmias and cardiac function after pneumonectomy. Ann Thorac Surg 1997;63:1374–81. [PubMed] [Google Scholar]
- [15].Aronson S, Dyke CM, Levy JH, et al. Does perioperative systolic blood pressure variability predict mortality after cardiac surgery? An exploratory analysis of the ECLIPSE trials. Anesth Analg 2011;113:19–30. [DOI] [PubMed] [Google Scholar]
- [16].Luo XP, Huan-Chun NI, Shan Y, et al. An effect comparison of perioperative intravenous metoprolol bolus in 137 cases and intravenous calcium iron antagonist injection in 128 cases with noncardiac surgery. Int J Cardiovas 2009;36:120–3. [Google Scholar]
- [17].Peacock WF, Chandra A, Char D, et al. Clevidipine in acute heart failure: results of the a study of blood pressure control in acute heart failure-a pilot study (PRONTO). Am Heart J 2014;167:529–36. [DOI] [PubMed] [Google Scholar]
- [18].Du TH, Weich HF, Weymar HW, et al. Effects of nifedipine on the peri-operative ECG, as determined by continuous Holter monitoring. A double-blind study. S Afr Med J 1986;69:427–31. [PubMed] [Google Scholar]
- [19].Halpern NA, Goldberg M, Neely C, et al. Postoperative hypertension: a multicenter, prospective, randomized comparison between intravenous nicardipine and sodium nitroprusside. Crit Care Med 1992;20:1637–43. [PubMed] [Google Scholar]
- [20].Kario K, Hoshide S, Uchiyama K, et al. Dose timing of an angiotensin ii receptor blocker/calcium channel blocker combination in hypertensive patients with paroxysmal atrial fibrillation. J Clin Hypertens 2016;18:1036–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Lindgren L, Lepäntalo M, Knorring JV, et al. Effect of verapamil on right ventricular pressure and atrial tachyarrhythmia after thoracotomy. Br J Anaesth 1991;66:205–11. [DOI] [PubMed] [Google Scholar]
- [22].Van MW, Tits G, Demuynck K, et al. Verapamil as prophylactic treatment for atrial fibrillation after lung operations. Ann Thorac Surg 1996;61:1083–5. [DOI] [PubMed] [Google Scholar]
- [23].Dingemanse J, Otasevic P, Shakerinejad K, et al. Efficacy and safety of the dual L- and T-type calcium channel blocker, ACT-280778: a proof-of-concept study in patients with mild-to-moderate essential hypertension. J Hum Hypertens 2015;29:229–35. [DOI] [PubMed] [Google Scholar]
- [24].Rakugi H, Ogihara T, Saruta T, et al. Preferable effects of olmesartan/calcium channel blocker to olmesartan/diuretic on blood pressure variability in very elderly hypertension: COLM study subanalysis. J Hypertens 2015;33:2165–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Vohra A, Mathew JP, Fontes ML, et al. and the McSPI Research Group, Inc. A multicenter risk index for atrial fibrillation after cardiac surgery. JAMA 2004;291:1720–9. [DOI] [PubMed] [Google Scholar]
- [26].Rich S, Kaufmann E, Levy PS. The effect of high doses of calcium-channel blockers on survival in primary pulmonary hypertension. N Engl J Med 1992;327:76–81. [DOI] [PubMed] [Google Scholar]
- [27].He T, Liu X, Li Y, et al. High-dose calcium channel blocker (CCB) monotherapy vs combination therapy of standard-dose CCBs and angiotensin receptor blockers for hypertension: a meta-analysis. J Hum Hypertens 2016. [DOI] [PubMed] [Google Scholar]


