Abstract
Rationale:
Infective endocarditis (IE) complicated with obstructive ST elevation myocardial infarction (STEMI) has been reported in the literature and which were mostly related to coronary artery embolism, obstruction, or compression. However, there has been no reported case discussing about IE complicated with nonobstructive STEMI.
Patient concerns:
In this report, we report a 38-year-old female suffering from intermittent fever and was later diagnosed as IE. Initially antibiotic was given and mitral valve surgery was also arranged due to large vegetation with severe mitral regurgitation. Nevertheless, sudden conscious loss with desaturation happened and brain computed tomography (CT) showed intracranial and subdural hemorrhage related to possible septic embolism. In addition, electrocardiography (ECG) revealed ST elevation over precordial leads, and elevation of cardiac enzymes was also noted.
Diagnoses:
Emergent coronary angiography was arranged but result showed normal coronary arteries without any evidence of stenosis. The diagnoses of IE complicated with nonobstructive STEMI were made.
Interventions:
After coronary angiography, the patient underwent craniotomy and subdural hematoma removal. Surprisingly, follow-up ECG also revealed ST segment resolution.
Outcomes:
The patient received full course antibiotic treatment and follow-up brain CT also showed improvement of intracranial hemorrhage (ICH) and subdural hemorrhage. Because follow-up echocardiography still revealed severe mitral regurgitation with mitral valve prolapse due to leaflet destruction with partially decreased vegetation size, mitral valve replacement with bioprosthetic valve was performed and the patient was finally discharged smoothly.
Lessons:
In our knowledge, this case should be the 1st case of IE complicated with nonobstructive STEMI, which reminds physicians that nonobstructive STEMI is still an extremely rare but possible complication of IE and septic embolism related ICH should be carefully surveyed in this rare patient group.
Keywords: embolism, infective endocarditis, intracranial hemorrhage, ST elevation myocardial infarction
1. Introduction
Infective endocarditis (IE) complicated with ST elevation myocardial infarction (STEMI) is a rare condition, which may be attributed to coronary embolism, obstruction of the coronary ostia by large vegetation, or coronary artery compression due to abscess formation.[1–7] However, there has been no reported case discussing about IE complicated with nonobstructive STEMI. Herein, we reported a 38-year-old female, who presented with IE complicated with nonobstructive STEMI related to septic embolism with intracranial hemorrhage (ICH). Informed consent was obtained from the patient for the publication of this case report.
2. Case report
This 38-year-old female without any known systemic disease had intermittent fever for 1 month. She also presented with loss of appetite and body weight loss of 10 kg within half year. There was no respiratory tract, urinary tract, or gastrointestinal complaint. No history of recent travel, sick contacts, animal contacts, insect bites, or intravenous drug abuse. Due to above reasons, she was brought to local hospital and was admitted for further evaluation.
On examination, there were no peripheral stigmata of IE, but heart sound revealed an apical pansystolic murmur. The initial workup revealed white blood cell count: 9170 cells/μL with 87% segmented neutrophil; hemoglobin: 8.8 g/dL; platelet count: 352,000/mm3. Beta thalassemia was also confirmed via hemoglobin electrophoresis. Elevation of C-reactive protein (205 mg/dL) and erythrocyte sedimentation rate (99/mL) were also noted. Other biochemistry data including thyroid function, ANA, C3, C4, and rheumatoid factor were within normal limit. Urine analysis and chest radiograph did not reveal abnormal finding. Transthoracic echocardiogram identified a large vegetation (size 1.2 × 1.7 cm) on anterior mitral leaflet and submitral apparatus with severe mitral regurgitation (Fig. 1). Four sets of blood culture were positive for Streptococcus cristatus which was sensitive to all cephalosporin antibiotics. Therefore, the diagnosis of IE was made and antibiotic Cefazolin was used for treatment of IE. Intermittent fever then gradually subsided after antibiotic use.
Figure 1.
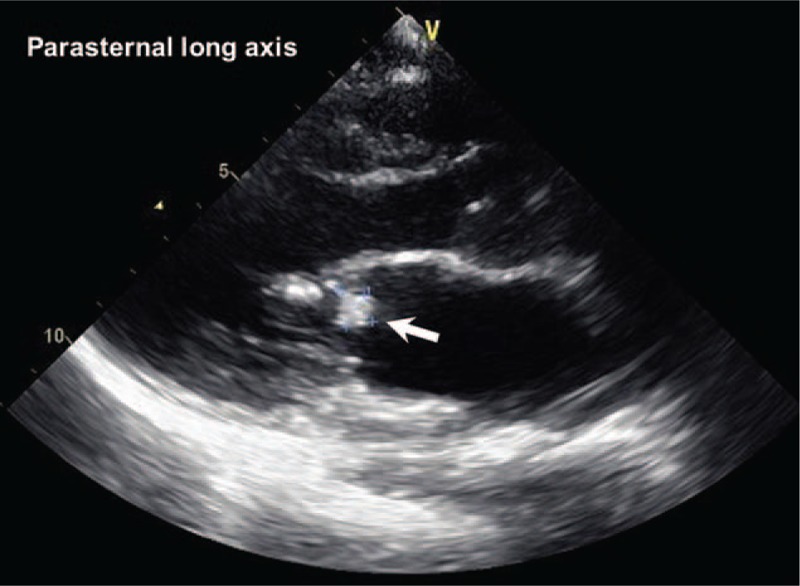
Echocardiography revealed large vegetation (size 1.2 × 1.7 cm) on anterior mitral leaflet and submitral apparatus.
Further surgical intervention for mitral valve replacement was still considered due to large vegetation size. However, the patient suffered from sudden onset of severe headache and loss of consciousness with desaturation after 21 days of hospitalization. Intubation was immediately performed for desaturation episode. Brain computed tomography (CT) was also arranged and it showed ICH at the right occipital lobe, subdural hemorrhage (SDH) adjacent to right fronto-parieto-temporal lobe, along the cerebral falx and right tentorium (Fig. 2). Initially the operation for ICH was arranged; however, preoperation electrocardiogram (ECG) showed ST elevation over V2-V5 and ST depression over lead II, III, and aVF (Fig. 3A). Elevation of cardiac enzymes was also noted, which showed: CPK: 91 IU/L, CK-MB: 6.8 ng/mL, and troponin-I: 2.436 ng/mL. Due to high suspicion of STEMI, emergency coronary angiography was performed. Surprisingly, coronary angiography revealed normal coronary arteries without any evidence of stenosis. After that craniotomy and SDH removal was performed. ECG after operation revealed ST segment resolution (Fig. 3B), and cardiac enzymes also gradually declined. Then the patient received full course antibiotic treatment and follow-up brain CT also showed improvement of ICH and SDH. Because follow-up echocardiography still revealed severe mitral regurgitation with mitral valve prolapse due to leaflet destruction with partially decreased vegetation size (1.2 cm × 0.7 cm), mitral valve replacement with bioprosthetic valve was performed and the patient was finally discharged smoothly.
Figure 2.
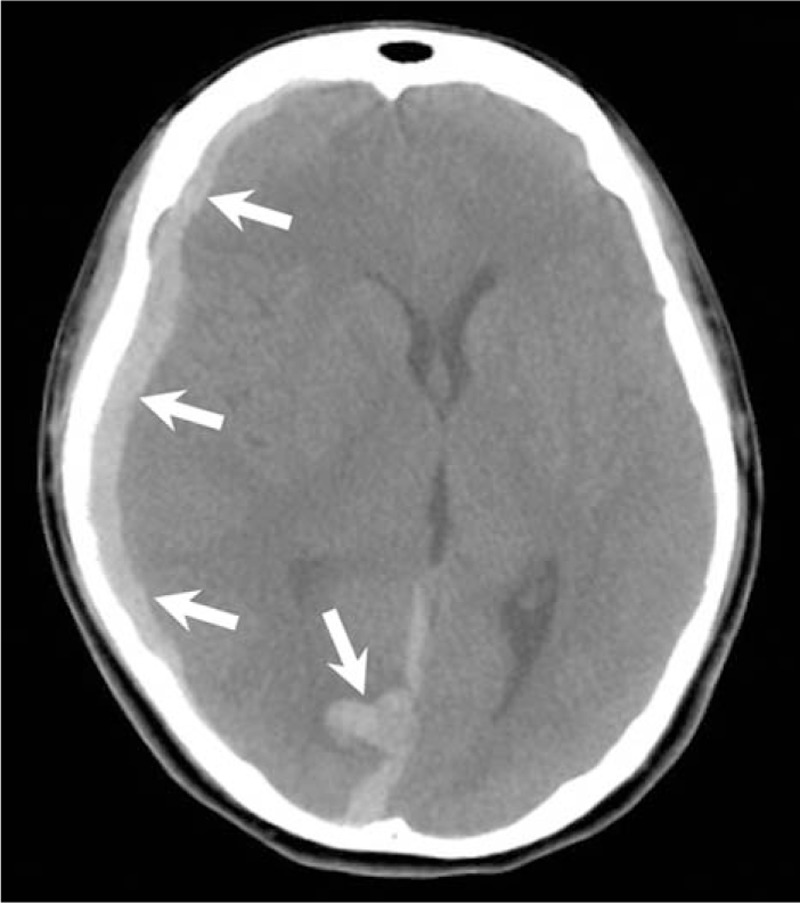
Brain computed tomography revealed intracranial hemorrhage at the right occipital lobe, subdural hemorrhage adjacent to right fronto-parieto-temporal lobe.
Figure 3.
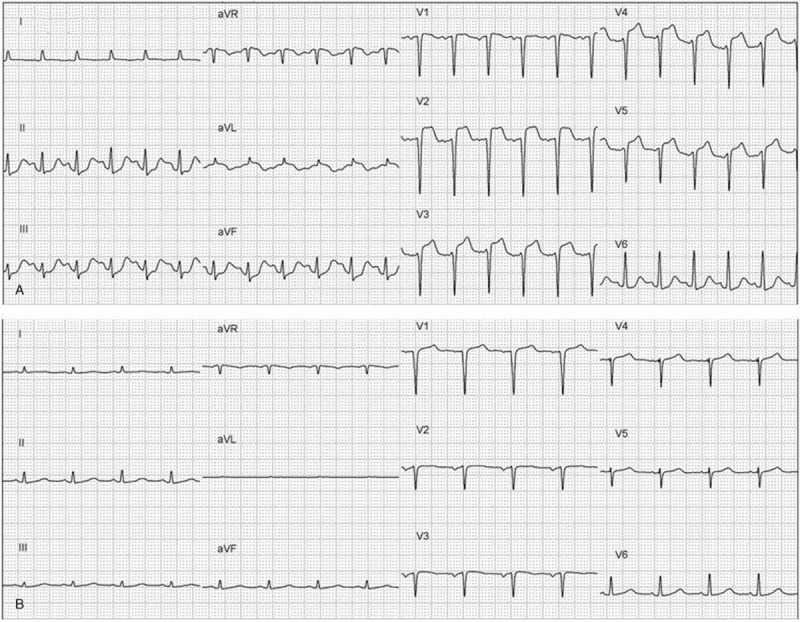
(A) Electrocardiography after intracranial hemorrhage showed ST elevation over V2-V5 and ST depression in lead II, III, aVF. (B) After craniotomy and subdural hematoma removal, electrocardiogram revealed ST segment resolution.
3. Discussion
Acute coronary syndrome is a rare complication in IE, account for only 3% in this population. The mechanism is mostly attributed to obstructive lesion, such as coronary embolism, obstruction of the coronary ostia by large vegetation, or coronary artery compression due to abscess or pseudoaneurysms formation.[7] Yeoh et al reported that coronary artery septic embolism resulting in cardioembolic myocardial infarction is a rare complication of bacterial IE, representing only <1% of complications related to IE.[1] Rischin et al presented a 42-year-old female with multi-embolic STEMI secondary to aortic valve endocarditis.[2] Singh et al reported a 70-year-old male with aortic valve endocarditis and persistent bacteremia developed acute inferior wall STEMI due to septic embolism and the patient expired even under aggressive medical and interventional management.[3] Regmi et al also showed a case of unusual presentation of IE as STEMI secondary to coronary embolization from mitral valve endocarditis.[5] However, there has been no reported case discussing about IE complicated with nonobstructive STEMI.
In our patient, ICH was developed after 21 days of antibiotic treatment for IE. Because this patient did not use any antiplatelet or anticoagulation drugs before and during hospitalization, the most possible mechanism of ICH in this patient was related to septic embolism with hemorrhagic transformation. ECG changes are common in patients with cerebrovascular diseases, particularly in subarachnoid hemorrhage; however, typical ST segment elevation in ICH or SDH is very rare.[8] The exact mechanism is still unclear, but it may be caused by releasing of catecholamines and stimulation of central autonomic center, which resulted in cardiac dysfunction.[9] To our knowledge, our case should be the 1st case of IE complicated with nonobstructive STEMI related to septic embolism with ICH. Although the mortality is extremely high in this situation, our case survived after brain operation and further mitral valve replacement.
4. Conclusion
Although IE complicated with STEMI is a rare complication and most cases are related to coronary embolism or obstructive lesions, our case reminds physicians that nonobstructive STEMI is still an extremely rare but possible complication of IE, and septic embolism related ICH should be carefully surveyed in this rare patient group.
Author contributions
Conceptualization: Po-Chao Hsu.
Data curation: Wen-Hsien Lee, Chun-Yuan Chu.
Formal analysis: Ho-Ming Su.
Investigation: Tsung-Hsien Lin.
Resources: Hsueh-Yei Yen, Wen-Chol Voon.
Validation: Wen-Ter Lai, Sheng-Hsiung Sheu, Po-Chao Hsu.
Writing – original draft: Yi-Hsueh Liu.
Writing – review & editing: Po-Chao Hsu.
Yi-Hsueh Liu orcid: 0000-0001-6915-3679.
Footnotes
Abbreviations: CT = computed tomography, ECG = electrocardiography, ICH = intracranial hemorrhage, IE = infective endocarditis, SDH = subdural hemorrhage, STEMI = ST elevation myocardial infarction.
The authors have no funding and conflicts of interest to disclose.
References
- [1].Yeoh J, Sun T, Hobbs M, et al. An uncommon complication of infective bacterial endocarditis. Heart Lung Circ 2012;21:811–4. [DOI] [PubMed] [Google Scholar]
- [2].Rischin AP, Carrillo P, Layland J. Multi-embolic ST-elevation myocardial infarction secondary to aortic valve endocarditis. Heart Lung Circ 2015;24:e1–3. [DOI] [PubMed] [Google Scholar]
- [3].Singh M, Mishra A, Kaluski E. Acute ST-elevation myocardial infarction due to septic embolism: a case report and review of management options. Catheter Cardiovasc Interv 2015;85:E166–71. [DOI] [PubMed] [Google Scholar]
- [4].Winkler J, Chaudhry SP, Stockwell PH. Gemella endocarditis presenting as an ST-segment-elevation myocardial infarction. Tex Heart Inst J 2016;43:258–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Regmi N, Pandey S, Neupane S. ST-elevation myocardial infarction: an unusual presentation of infective endocarditis. J Cardiovasc Echogr 2017;27:99–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Joliat GR, Halkic N, Pantet O, et al. Ischemic stroke and ST-elevation myocardial infarction revealing infective endocarditis. Eur Rev Med Pharmacol Sci 2017;21:4640–1. [PubMed] [Google Scholar]
- [7].Manzano MC, Vilacosta I, San Roman JA, et al. Acute coronary syndrome in infective endocarditis [in Spanish]. Rev Esp Cardiol 2007;60:24–31. [PubMed] [Google Scholar]
- [8].Goldstein DS. The electrocardiogram in stroke: relationship to pathophysiological type and comparison with prior tracings. Stroke 1979;10:253–9. [DOI] [PubMed] [Google Scholar]
- [9].Heo WJ, Kang JH, Jeong WS, et al. Subarachnoid hemorrhage misdiagnosed as an acute ST elevation myocardial infarction. Korean Circ J 2012;42:216–9. [DOI] [PMC free article] [PubMed] [Google Scholar]


