Abstract
Background:
The aim of this study was to compare the analgesic effect on the lateral and overall knee and early rehabilitation between adductor canal block (ACB) and femoral nerve block (FNB) after total-knee arthroplasty.
Method:
Two hundred patients randomly participated in the study and were divided into the ACB group and FNB group in a randomized manner. All patients received standardized anesthesia and analgesia upon hospitalization. Outcome evaluations included visual analog scale (VAS) scores at rest and during activity, quadriceps strength, range of motion (ROM), total opioid consumption and complication occurrence, sleep interruptions caused by pain, postoperative nausea and vomiting (PONV), and postoperative length of stay (PLOS) before discharge in all groups. In the 90-day postoperative follow-up, we also observed the acute deep periprosthetic joint infection, wound breakdown, readmission, reoperations, inpatient falls, ROM, and patient satisfaction score.
Results:
The lateral knee VAS scores are lower in the FNB group at rest and during activity (2–24 hours postoperatively) compared with those in the ACB group. However, the overall knee VAS score, total opioid consumption and complication occurrence, sleep interruptions caused by pain, and PONV are similar between the FNB and ACB groups. When evaluating early rehabilitation, the quadriceps strength in the ACB group is superior to that in the FNB group 24 hours postoperatively. At 24, 48, and 72 hours postoperatively, ROM in the ACB group is significantly better than that in the FNB group. Furthermore, the ACB group has a shorter PLOS (4.5 ± 0.60 days) than the FNB group (5.3 ± 0.7 days). However, patient satisfaction score, readmission rate, inpatient falls, acute deep periprosthetic joint infection, and wound breakdown are not statistically significantly different between the 2 groups.
Conclusion:
The ACB does not relieve lateral knee pain in the early stage but provides similar analgesic effect and better effectiveness of early rehabilitation compared with FNB in patients undergoing TKA.
Keywords: adductor canal block, analgesic, arthroplasty, femoral nerve block, knee, rehabilitation
1. Introduction
Total-knee arthroplasty (TKA), one of the most common orthopedic operations, is performed in patients with end-stage osteoarthritis and other knee diseases such as rheumatoid arthritis (RA). However, over 60% of patients have suffered severe pain after TKA, which has affected the quality of sleep, appetite, and functional exercise.[1–4] Therefore, postoperative pain management is essential for functional recovery, patients’ return to society, and patient satisfaction after TKA.
So far, postoperative pain control is presented with a large number of methods following TKA, including epidural analgesia, intravenous patient-controlled analgesia (PCA), peripheral nerve blocks, femoral nerve block (FNB), adductor canal block (ACB), and local infiltration analgesia (LIA).[5–10] Compared with epidural or intravenous patient-controlled analgesia, FNB provides superior pain control and shortens hospital stay. However, FNB, causing decreased quadriceps strength, increases the risk of inpatient falls. Its incidence is low (2%), but it is not allowed to occur in the clinical setting.[11–15]
The ACB, a regional analgesic technique, is successfully used for postoperative pain control after knee surgery. In a retrospective cohort study, Manickam et al have demonstrated effectiveness of the ACB plus LIA on early ambulation after TKA compared with LIA alone.[16] Some of the high quality studies have confirmed that ACB and FNB, in TKA, can achieve similar postoperative analgesic effect, but patients with ACB can obtain better early rehabilitation compared with those with FNB.[17] Similarly, in a prospective randomized, controlled trial, 93 patients who underwent TKA were randomized to receive either FNB or ACB, ACB exhibited early relative sparing of quadriceps strength at 6 to 8 hours postanesthesia compared with FNB.[18]
Studies on ACB vs FNB for TKA already exist but are not focused on the analgesic area, and some studies, at the same time, lack research on the impact of postoperative pain on functional recovery, quality of sleep, and postoperative quadriceps strength. The existing large-sample, high-quality, prospective randomized controlled trials were relatively few, which cannot fully prove the existing results that the ACB offered similar effectiveness of early analgesia and promote early rehabilitation compared to FNB in patients undergoing TKA. Simultaneously, an anatomical study had been shown that the distributions of the adductor canal are in the medial and anterior aspects of the knee from the superior pole of the patella to the proximal tibia, and the adductor canal does not contain the motor nerve. However, the distributions of the femoral nerve were in the medial, anterior, and lateral aspects of the knee, and the femoral nerve innervates the quadriceps.[19,20] Considering these factors, the present research seeks to compare the effects of ACB and FNB on the postoperative analgesic area, analgesic effect, and early rehabilitation in patients undergoing TKA.
2. Methods
2.1. Patients and allocation
The study was a double-blind, prospective, randomized, and controlled Trial. It was approved by the Ethics Committee of West China Hospital of Sichuan University and registered with Chictr.org, Identifier ChiCTR-IOR-15005790. Written informed consent was obtained from all patients. The inclusion criterion includes primary unilateral TKA for OA or RA. The exclusion criteria include allergies or intolerance to one of the study drugs, epilepsy, language difficulty, mental illness, dementia, preexisting neuropathy on the operative limb, alcoholism, chronic opioid use (defined as daily or almost daily use of opioids for >3 months), body mass index >35 or <20, age younger than 18 years or older than 80 years, and American Society of Anesthesiologists (ASA) class 4 or 5.
2.2. Standardized anesthesia and analgesia
All patients received a standardized anesthesia and analgesia upon hospitalization. Preoperative oral celecoxib (200 mg, twice a day) was administered 3 days before surgery. On the day of the surgery, all patients were randomly assigned to the ACB and FNB groups (1:1 allocation, parallel trial design) 30 minutes before the surgery using sequentially numbered, opaque-sealed envelopes, based on a computer-generated randomization list created by an independent researcher (anesthetist). The patient and research assistant were blinded to the group assignment, but the anesthesiologist performing the block was aware of the treatment. We referred to and improved the methods described by Jæger et al[17]: In the ACB group, ultrasound-guided ACB (20 mL of 0.5% of ropivacaine with 5 μg/mL epinephrine, via a 22-gauge 2-inch Stimuplex A needle; B Braun Medical Inc, Melsungen Germany) was performed at the mid-thigh level using a high-frequency linear ultrasound transducer (10–12 Hz; SonoSite Turbo; SonoSite Inc, Bothell, WA). Block success was verified by testing for pinprick sensation in the saphenous nerve distribution. Ultrasound-guided FNB (30 mL of 0.33% of ropivacaine with 5 μg/mL epinephrine, via a 22-gauge 2-inch Stimuplex A needle; B Braun Medical Inc) with nerve stimulator confirmation was performed below the inguinal ligament, block success was verified by testing for pinprick sensation in the femoral nerve distribution. During surgery, general anesthesia was induced with sufentanil 0.3 μg/kg, propofol 2 mg/kg, and cisatracurium 1.5 mg/kg, and maintained with 1% to 3% sevoflurane in O2/air, and remifentanil 0.1 μg/kg/min. If systolic blood pressure or heart rate varied by more than 30% of the baseline values (after correction for hypovolemia, if present) intravenous (IV) boluses of nicardipine or ephedrine were administered every 5 minutes until the blood pressure or heart rate improved. Posterior capsule LIA (20 cc of 0.25% of ropivacaine with 5 mg/L epinephrine had been injected in the posterior capsule) had been administered by the experienced orthopedic surgeon at end of the operation. After operation, we used acetaminophen (50 mg, twice a day) and parecoxib (40 mg, twice a day) to control the postoperative pain. Moreover, we administered pethidine hydrochloride (50 mg) to the patients who experienced persistently severe postoperative pain or when their visual analog scale (VAS) at rest was over 4.
After a 1-hour postoperative care in the anesthesia recovery unit, all patients returned to the in-patient unit. It was on the day of the surgery that all patients began walking after the assessment of the physiotherapist. To avoid inpatient falls, a knee brace was used, within postoperative 24 hours, to protect the surgical side of the extremity of all patients. From the day of the surgery until the day of discharge, each patient underwent physical therapy supervised by a physiotherapist 3 times per day.
2.3. Outcome measurements
The primary outcomes included: postoperative pain score of the overall and lateral knee at rest and during activity (45° flexion of the postoperative knee) using VAS score (in the scale of 0 to 10, where 0 = no pain and 10 = worst pain that can be tolerated) score measured at 2, 4, 8, 12, 24, 48, 72 hours postoperatively and upon discharge; quadriceps strength estimated at 2, 4, 8, 12, 24, 48, 72 hours postoperatively, upon discharge, and at 90 days postoperation using an ergographic; and range of motion (ROM) assessed at 2, 4, 8, 12, 24, 48, and 72 hours postoperatively, upon discharge and 90 days postoperation.
Secondary outcomes were as follows: total opioid consumption (pethidine hydrochloride in this study) and complication occurrence was recorded postoperation; sleep interruptions caused by pain in the 1st, 2nd, and 3rd night postoperation; postoperative length of stay (PLOS) and patient satisfaction score evaluated when patient was discharge; and postoperative nausea and vomiting (PONV) recorded when experienced by a certain patient postoperation.
Other outcomes included postoperation urinary retention and inpatient falls recorded before discharge; local anesthetic toxicity or neurologic complications, acute deep periprosthetic joint infection, wound breakdown, readmission, reoperations, and patient satisfaction score recorded in 90-day postoperative follow-up.
2.4. Statistical analysis
All the data were analyzed using SPSS version 21.0 (IBM Inc., Chicago, Illinois). We used the Kolmogorov–Smirnov test to assess whether variable distributions violated the assumption of normality. Data are presented as mean and standard deviation or with medians and 25th to 75th percentiles as appropriate. The normal distributed numerical variable (VAS scores, quadriceps strength, ROM, total opioid consumption, sleep interruptions caused by pain and patient satisfaction scores) was analyzed by Student t test. If the numerical variable has a nonnormal distribution or unequal variance, the Wilcoxon Mann–Whitney U test was used (ASA grade); Pearson Chi-squared test or Fisher exact test was used to analyze the qualitative variable (inpatient falls). The nature of the hypothesis testing was 2-tailed, and a P-value <.05 was considered statistically significant.
3. Results
3.1. Patient characteristic
A total of 321 patients participated in the research, but 121 were excluded by various reasons (Fig. 1). Success rates for the ACB and FNB were 95.37% and 95.33%, respectively. Both 100 patients in the ACB and FNB group completed the study protocol and were analyzed for the outcomes. When admitted to hospital, demographics and perioperative data of the patients were recorded by a nurse who is a blinded observer. The baseline data collected including age, gender, body mass index, knee disease composition, ASA classification, perioperative ROM, duration of the surgery, and preoperative quadriceps strength. The patients were similar with respect to demographics and perioperative data as presented in Table 1.
Figure 1.
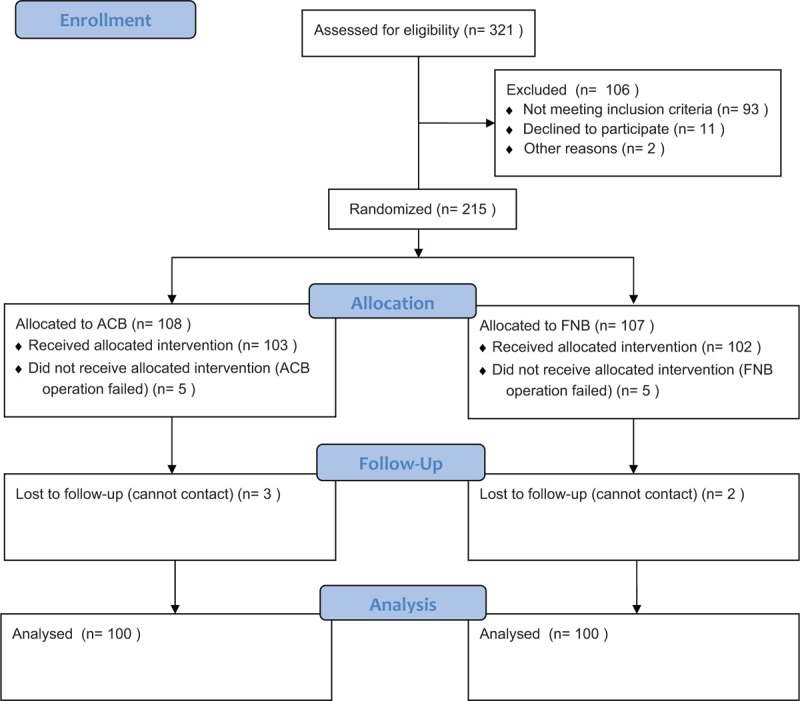
Consort diagram of patients’ randomization, intervention, and analysis.
Table 1.
Demographics and perioperative data.

3.2. Primary outcomes
Primary outcomes were pain management, quadriceps strength, and ROM. The VAS scores (2–24 hours postoperatively), on the lateral of the knee, were lower in the FNB group compared with those in the ACB group at rest and during activity of the knee (rest, 2–12 hours P < .001, 24 hours P = .02; activity, 2–12 hours P < .001, 24 hours P = .03), but there was no statistical significant difference in the VAS scores of both groups 48 and 72 hours postoperatively and upon discharge (rest, P = .13, .12, .40, respectively; activity, P = .15, .13, .30, respectively) (Fig. 2A, B). However, the VAS scores of the overall knee between ACB and FNB groups during all the observation times were not statistically significantly different (Fig. 2C, D). We conducted a strength test and found quadriceps strength for the ACB group to be superior to the FNB group 24 hours postoperatively (2–12 hours P < .001, 24 hours P = .02), but there were not inferior 48, 72 hours postoperatively, upon discharge and at 90 days postoperation (P = .56, .34, .41, .34, respectively) (Fig. 3). Moreover, the ROM were significantly better 24, 48, 72 hours postoperatively in the ACB group than in the FNB group (24, 48, and 72 hours, P < .001) and not inferior upon discharge and at 90 days postoperation (P = .2 and .42, respectively) (Fig. 4).
Figure 2.
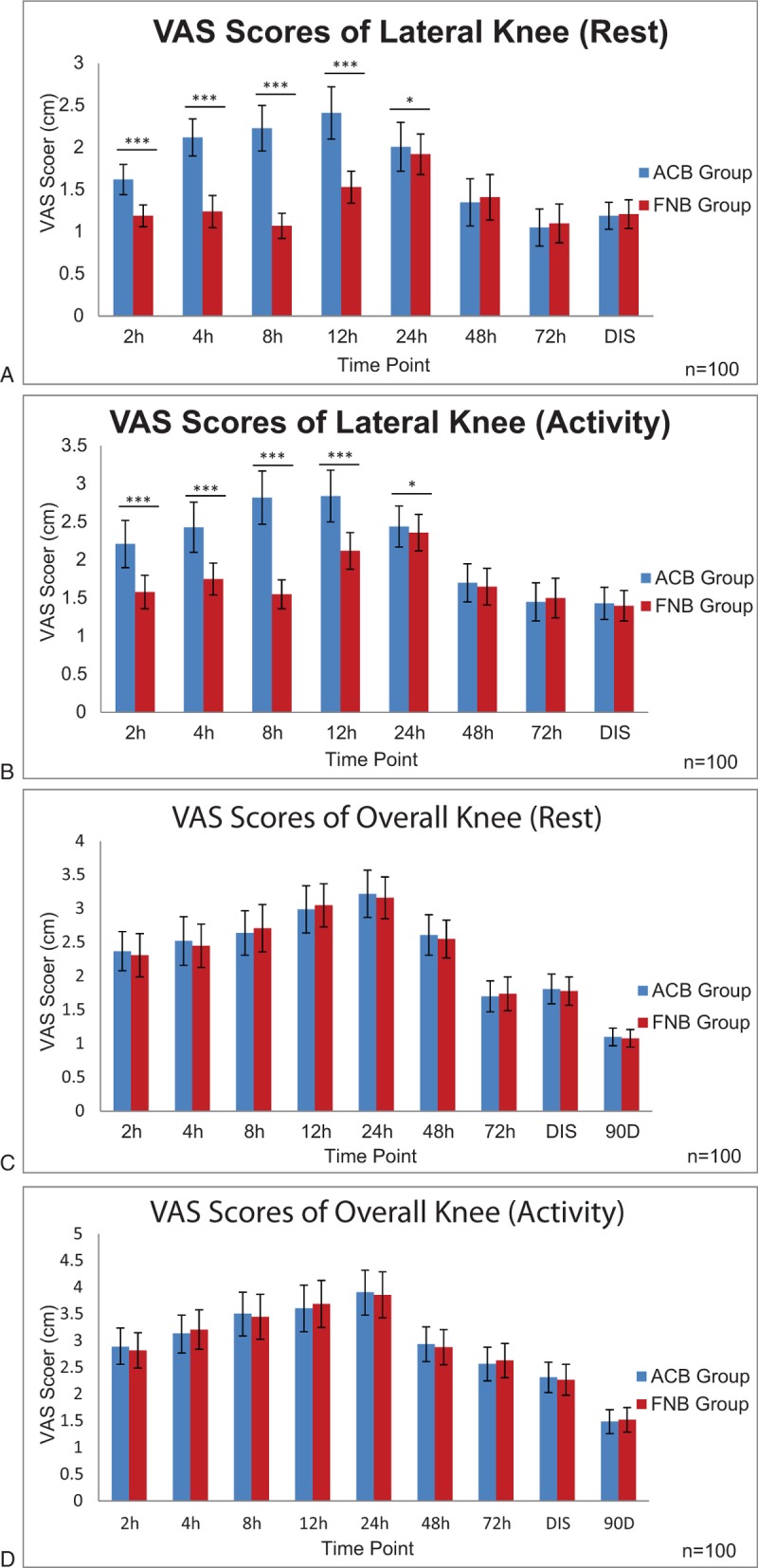
The VAS scores (A) at rest and (B) during activity of lateral knee of adductor canal block ACB and FNB group at different time points postoperation. Statistical significance was assigned at ∗P < .05, ∗∗∗P < .001. VAS scores (C) at rest and (D) during activity of overall knee of ACB and FNB group at different time points postoperation. There was no statistical difference in VAS scores between the 2 groups at all time points. Two-tailed Student t test was used to compare data. ACB = adductor canal block, 90D = 90-day postoperative, DIS = upon discharge, FNB = femoral nerve block, h = hours, VAS scores = visual analog scale scores.
Figure 3.
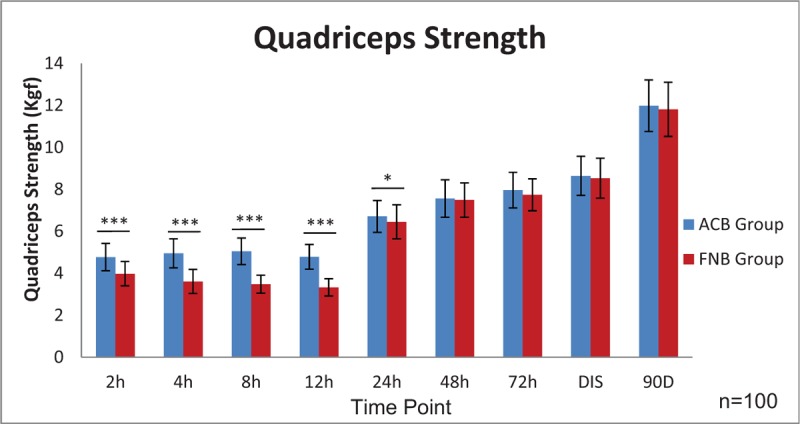
Quadriceps strength of adductor canal block (ACB) and femoral nerve Block (FNB) group at different time-points postoperation. Two-tailed Student t test was used to compare data and statistical significance was assigned at ∗P < .05, ∗∗∗P < .001. 90D = 90 day postoperation, DIS = upon discharge, h = hours, Kgf = kilogram of force.
Figure 4.
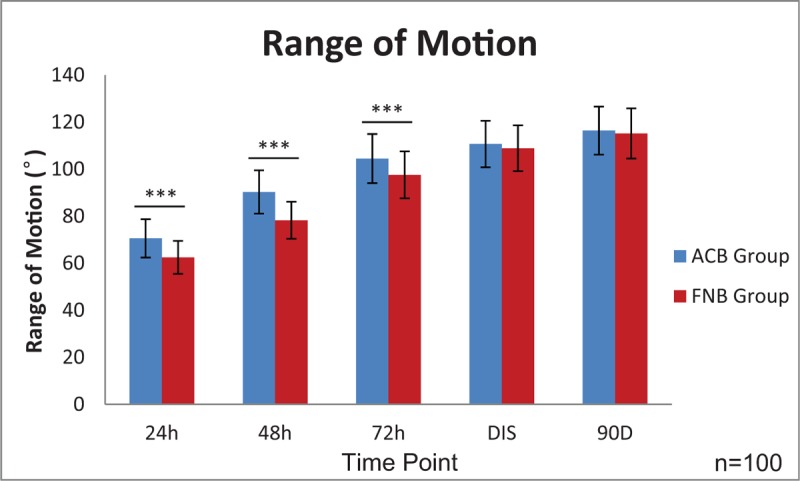
Range of motion of adductor canal block (ACB) and femoral nerve block (FNB) group at different time-point postoperation. Two-tailed Student t test was used to compare data and statistical significance was assigned at ∗∗∗P < .001. 90D = 90-day postoperation, DIS = upon discharge, h = hours.
3.3. Second outcomes
Total opioid consumption not different between the ACB (34.25 ± 22.35) and FNB (32.50 ± 20.95) groups postoperatively (P = .57) (Table 2). There was no significant difference in sleep interruptions caused by pain (the 1st, 2nd, and 3rd night postoperatively) (P = .33, .16, and .11, respectively) between the 2 group's (Table 2). Moreover, the ACB group had shorter postoperative hospital stays compared with the FNB group (P < .001) (Table 2). Fourteen patients (14%, 14/100) in ACB group and 15 patients (15.0%, 15/100) in the FNB group had experienced PONV. The comparison of the 2 groups was not significantly different (P = .84) (Table 2).
Table 2.
Other outcomes.

3.4. Other outcomes
Upon evaluation of the incision drain, urinary retention, readmission, and patient satisfaction score, there was no significant difference between the 2 groups (P = .37, .14, .56, and .24, respectively) (Table 2). There was no acute deep periprosthetic joint infection, reoperations, wound breakdown, in-patient falls, local anesthetic toxicity, or neurologic complications in both groups.
4. Discussion
This is a large-sample trial which evaluated the analgesic effect of the overall knee and lateral knee at rest, activity, and early rehabilitation and compared ACB and FNB in patients undergoing TKA. Our group found that there are significant differences in pain scores on the lateral knee (2–24 hours, postoperatively), but the VAS score of the overall knee was similar in both groups. Moreover, we believe that the difference between ACB and FNB in the analgesic area is the main cause of the above analgesic effect. Some previous studies in patients showed that there was no difference in overall knee pain between the ACB and FNB groups at rest and during activity.[17,21–23] In Jæger's study, they found no difference between ACB and FNB regarding total morphine consumption (P = .94), pain at rest (P = .21), and pain during flexion of the knee (P = .16) after TKA.[17] These results are consistent with our research. However, our results were not consistent with some published studies, which found that the patients with FNB had significantly lower VAS pain scores 6 to 8 hours postanesthesia.[24] We believe that the cause of this result is the use of different multimodal analgesia schemes and a local anesthesia in the 2 trials.
Simultaneously, ACB can significantly reduce the impact on the quadriceps strength 24 hours postoperatively and improve the ROM 72 hours postoperative. In a study of healthy volunteers found that ACB have not impact on the quadriceps strength of volunteer, but FNB will impact it.[25] Research shows that ACB is better in preserving quadriceps muscle strength than FNB in patients undergoing TKA.[22,26] Macrinici et al's studies on total-knee replacement revealed that the ACB group showed better preservation of quadriceps muscle strength and improved ambulation in the first 24 hours.[23] Simultaneously, Grevstad et al's studies on total-knee replacement found that the quadriceps maximum voluntary isometric contraction increased to 193% of the baseline value in the ACB group and decreased to 16% in the FNB group with an estimated difference of 178% (P < .01) after the block.[22] These results are consistent with our research. Similarly, the relevant meta-analysis studies show that ACB provides similar pain control, better ambulation ability, and faster functional recovery after TKA compared with FNB.[27,28] With the lowest effect on quadriceps strength, ACB can promote the rehabilitation of patients. A study reported by Jæger et al compared the analgesic effect and rehabilitation between ACB and FNB and concluded that ACB preserved quadriceps strength and promoted ambulation better compared with FNB.[17]
Our study found that the ACB can provide a similar analgesic effect with FNB, so quadriceps strength becomes the factor which is most likely to promote rehabilitation in patient undergoing TKA. The reason for this phenomenon may be that better quadriceps strength can increase the stability of the joint and so the joint can move more freely. The early ease joint activities can promote transport of intra-articular inflammatory cytokines into the blood, reduce the concentration of inflammatory cytokines, and thus relieve postoperative pain and promote further rehabilitation of patients.
In this trial, total opioid consumption and complication occurrence and sleep interruptions caused by pain are not statistically significantly different between the ACB and FNB groups at all-time-points. The amount of total opioid consumption is significantly less than that in other research which is focused on analgesia after TKA. The explanations as to why ACB and FNB are so effective might be attributed to multimodal analgesia, especially LIA. Numerous studies have demonstrated that LIA can provide good analgesic effect under multimodal analgesia.[29–32] Further, in a similar multimodal analgesia, the amount of total opioid consumption is very close in TKA.[24] In a prospective double-blind, randomized controlled trial, Memtsoudis et al found that the pain score of the ACB group were similar to the FNB group in all time points.[33] In Patterson et al's study, they found that a single-shot ACB provides equally effective analgesia when compared with FNB within the first 24 hours.[34]
Moreover, ACB, in our study, can significantly reduce the PLOS compared with FNB in TKA. The main reason for this difference may be that ACB, compared with FNB, has less impact on quadriceps strength and then promote the recovery of patient's knee joint function. Then, the patients undergoing ACB can meet the discharge criteria earlier than those undergoing FNB.
In addition, we did a 90-day follow-up of our patients. We found that the incision drain, urinary retention, readmission, and patient satisfaction score had no significant difference between ACB and FNB. Moreover, we have not recorded acute deep periprosthetic joint infection, reoperations, wound breakdown, in-patient falls, local anesthetic toxicity, or neurologic complications in both groups.
The strengths of this study were obvious. First, this is a large-sample-size prospective double-blind, randomized controlled trial, evidence of Level I, which is designed and conducted carefully and strictly. Thus, the bias was minimal. Second, this is the 1st trial which evaluated the VAS score of the lateral knee at rest and during activity and compared ACB and FNB in patients undergoing TKA. Third, the outcome measures were observed at high frequency and for a long period which can more fully reflect the studying problem.
Firstly, the main limitation is that the clinical effects and complications of ACB were compared with that of FNB without the control group in the present study. According to the beneficence principle for patients,[35] no control group with placebo was designed in the protocol of the present study. Secondly, although the surgeon and nurses were blinded, the strength of blinding might be weakened because of the distinguished injection area on patients’ thigh. Thirdly, the levels of inflammatory indicators in the joint cavity and circulation were not examined. Our main goal was to compare the effects of 2 different local anesthesia methods on pain and early rehabilitation, but the local anesthesia only blocks the afferent nerve fibers, which we believe does not have a significant effect on the inflammation level of the joint cavity and circulation. Finally, we had to admit that ACB and FNB might theoretically make the risk of infection higher and damage the corresponding nerve. However, in fact, the results of our study showed that the rates of these complications were very low. We do not think these limitations would affect the results tremendously.
5. Conclusion
The ACB, compared to the FNB, allow patients with TKA to achieve similar knee analgesia effect regarding in VAS scores, opioid consumption, and complication occurrences, sleep interruptions caused by pain and gain better effectiveness of early rehabilitation in quadriceps strength, the ROM of knee joint, and PLOS. However, the adductor canal block could not relieve lateral knee pain in the early rehabilitation stage.
Author contributions
Conceptualization: FuXing Pei.
Data curation: Zhen Tan, Pengde Kang, Bin Shen, Jing Yang, Jing Yang.
Formal analysis: FuXing Pei, Bin Shen, Jing Yang.
Funding acquisition: FuXing Pei.
Investigation: Zhen Tan, Jing Yang.
Methodology: Pengde Kang.
Project administration: Pengde Kang, FuXing Pei.
Software: Zhen Tan.
Supervision: Pengde Kang, FuXing Pei, Bin Shen, Jing Yang.
Validation: Pengde Kang, Bin Shen, Jing Yang.
Writing – original draft: Zhen Tan.
Writing – review & editing: Pengde Kang.
Footnotes
Abbreviations: ACB = adductor canal block, ASA = American Society of Anesthesiologists, FNB = femoral nerve block, LIA = local infiltration analgesia, POLS = postoperative length of stay, PONV = postoperative nausea and vomiting, RA = rheumatoid arthritis, ROM = range of motion, TKA = total-knee arthroplasty, VAS score = visual analog scale score.
This work was supported by Health Industry Special Scientific Research Projects of China (No. 201302007).
References
- [1].Parvizi J, Miller AG, Gandhi K. Multimodal pain management after total joint arthroplasty. J Bone Joint Surg Am 2011;93A:1075–84. [DOI] [PubMed] [Google Scholar]
- [2].Vendittoli PA, Makinen P, Drolet P, et al. A multimodal analgesia protocol for total knee arthroplasty - a randomized, controlled study. J Bone Joint Surg Am 2006;88A:282–9. [DOI] [PubMed] [Google Scholar]
- [3].Abdul-Hadi O, Parvizi J, Austin MS, et al. Nonsteroidal anti-inflammatory drugs in orthopaedics. J Bone Joint Surg Am 2009;91A:2020–7. [PubMed] [Google Scholar]
- [4].Husted H, Lunn TH, Troelsen A, et al. Why still in hospital after fast-track hip and knee arthroplasty? Acta Orthop 2011;82:679–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Barrington MJ, Olive D, Low K, et al. Continuous femoral nerve blockade or epidural analgesia after total knee replacement: a prospective randomized controlled trial. Anesth Analg 2005;101:1824–9. [DOI] [PubMed] [Google Scholar]
- [6].Capdevila X, Barthelet Y, Biboulet P, et al. Effects of perioperative analgesic technique on the surgical outcome and duration of rehabilitation after major knee surgery. Anesthesiology 1999;91:8–15. [DOI] [PubMed] [Google Scholar]
- [7].Abdallah FW, Chan VWS, Gandhi R, et al. The analgesic effects of proximal, distal, or no sciatic nerve block on posterior knee pain after total knee arthroplasty a double-blind placebo-controlled randomized trial. Anesthesiology 2014;121:1302–10. [DOI] [PubMed] [Google Scholar]
- [8].Bogoch ER, Henke M, Mackenzie T, et al. Lumbar paravertebral nerve block in the management of pain after total hip and knee arthroplasty - a randomized controlled clinical trial. J Arthroplasty 2002;17:398–401. [DOI] [PubMed] [Google Scholar]
- [9].Kristensen PK, Pfeiffer-Jensen M, Storm JO, et al. Local infiltration analgesia is comparable to femoral nerve block after anterior cruciate ligament reconstruction with hamstring tendon graft: a randomised controlled trial. Knee Surg Sports Traumatol Arthrosc 2014;22:317–23. [DOI] [PubMed] [Google Scholar]
- [10].McMeniman TJ, McMeniman PJ, Myers PT, et al. Femoral nerve block vs fascia iliaca block for total knee arthroplasty postoperative pain control: a prospective, randomized controlled trial. J Arthroplasty 2010;25:1246–9. [DOI] [PubMed] [Google Scholar]
- [11].Sakai N, Inoue T, Kunugiza Y, et al. Continuous femoral versus epidural block for attainment of 120 degrees knee flexion after total knee arthroplasty: a randomized controlled trial. J Arthroplasty 2013;28:807–14. [DOI] [PubMed] [Google Scholar]
- [12].Chan E-Y, Fransen M, Parker DA, et al. Femoral nerve blocks for acute postoperative pain after knee replacement surgery. Cochrane Database Syst Rev 2014;13:CD009941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Pelt CE, Anderson AW, Anderson MB, et al. Postoperative falls after total knee arthroplasty in patients with a femoral nerve catheter: can we reduce the incidence? J Arthroplasty 2014;29:1154–7. [DOI] [PubMed] [Google Scholar]
- [14].Wasserstein D, Farlinger C, Brull R, et al. Advanced age, obesity and continuous femoral nerve blockade are independent risk factors for inpatient falls after primary total knee arthroplasty. J Arthroplasty 2013;28:1121–4. [DOI] [PubMed] [Google Scholar]
- [15].Sharma S, Iorio R, Specht LM, et al. Complications of femoral nerve block for total knee arthroplasty. Clin Orthop Relat Res 2010;468:135–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Manickam B, Perlas A, Duggan E, et al. Feasibility and efficacy of ultrasound-guided block of the saphenous nerve in the adductor canal. Reg Anesth Pain Med 2009;34:578–80. [DOI] [PubMed] [Google Scholar]
- [17].Jæger P, Zaric D, Fomsgaard JS, et al. Adductor canal block versus femoral nerve block for analgesia after total knee arthroplasty: a randomized, double-blind study. Reg Anesth Pain Med 2013;38:526–32. [DOI] [PubMed] [Google Scholar]
- [18].Akkaya T, Ersan O, Ozkan D, et al. Saphenous nerve block is an effective regional technique for post-menisectomy pain. Knee Surg Sports Traumatol Arthrosc 2008;16:855–8. [DOI] [PubMed] [Google Scholar]
- [19].Burckett-St Laurant D, Peng P, Arango LG, et al. The nerves of the adductor canal and the innervation of the knee an anatomic study. Reg Anesth Pain Med 2016;41:321–7. [DOI] [PubMed] [Google Scholar]
- [20].Ishiguro S, Yokochi A, Yoshioka K, et al. Anatomy and clinical implications of ultrasound-guided selective femoral nerve block. Anesth Analg 2012;115:1467–70. [DOI] [PubMed] [Google Scholar]
- [21].Li D, Tan Z, Kang P, et al. Effects of multi-site infiltration analgesia on pain management and early rehabilitation compared with femoral nerve or adductor canal block for patients undergoing total knee arthroplasty: a prospective randomized controlled trial. Int Orthop 2017;41:75–83. [DOI] [PubMed] [Google Scholar]
- [22].Grevstad U, Mathiesen O, Valentiner LS, et al. Effect of adductor canal block versus femoral nerve block on quadriceps strength, mobilization, and pain after total knee arthroplasty: a randomized, blinded study. Reg Anesth Pain Med 2015;40:3–10. [DOI] [PubMed] [Google Scholar]
- [23].Macrinici GI, Murphy C, Christman L, et al. Prospective, double-blind, randomized study to evaluate single-injection adductor canal nerve block versus femoral nerve block postoperative functional outcomes after total knee arthroplasty. Reg Anesth Pain Med 2017;42:10–6. [DOI] [PubMed] [Google Scholar]
- [24].Kim DH, Lin Y, Goytizolo EA, et al. Adductor canal block versus femoral nerve block for total knee arthroplasty. Anesthesiology 2014;120:540–50. [DOI] [PubMed] [Google Scholar]
- [25].Jæger P, Nielsen ZJK, Henningsen MH, et al. Adductor canal block versus femoral nerve block and quadriceps strength: a randomized, double-blind, placebo-controlled, crossover study in healthy volunteers. Anesthesiology 2013;118:409–15. [DOI] [PubMed] [Google Scholar]
- [26].Elkassabany NM, Antosh S, Ahmed M, et al. The risk of falls after total knee arthroplasty with the use of a femoral nerve block versus an adductor canal block: a double-blinded randomized controlled study. Anesth Analg 2016;122:1696–703. [DOI] [PubMed] [Google Scholar]
- [27].Wang D, Yang Y, Li Q, et al. Adductor canal block versus femoral nerve block for total knee arthroplasty: a meta-analysis of randomized controlled trials. Sci Rep 2017;7:40721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Gao F, Ma J, Sun W, et al. Adductor canal block versus femoral nerve block for analgesia after total knee arthroplasty: a systematic review and meta-analysis. Clin J Pain 2017;33:356–68. [DOI] [PubMed] [Google Scholar]
- [29].Ikeuchi M, Kamimoto Y, Izumi M, et al. Local infusion analgesia using intra-articular double lumen catheter after total knee arthroplasty: a double blinded randomized control study. Knee Surg Sports Traumatol Arthrosc 2013;21:2680–4. [DOI] [PubMed] [Google Scholar]
- [30].Moghtadaei M, Farahini H, Faiz SH-R, et al. Pain management for total knee arthroplasty: single-injection femoral nerve block versus local infiltration analgesia. Iran Red Crescent Med J 2014;16: e13247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Binici Bedir E, Kurtulmus T, Basyigit S, et al. A comparison of epidural analgesia and local infiltration analgesia methods in pain control following total knee arthroplasty. Acta Orthop Traumatol Turc 2014;48:73–9. [DOI] [PubMed] [Google Scholar]
- [32].Essving P, Axelsson K, Kjellberg J, et al. Reduced morphine consumption and pain intensity with local infiltration analgesia (LIA) following total knee arthroplasty: a randomized double-blind study involving 48 patients. Acta Orthop 2010;81:354–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Memtsoudis SG, Yoo D, Stundner O, et al. Subsartorial adductor canal vs femoral nerve block for analgesia after total knee replacement. Int Orthop 2015;39:673–80. [DOI] [PubMed] [Google Scholar]
- [34].Patterson ME, Bland KS, Thomas LC, et al. The adductor canal block provides effective analgesia similar to a femoral nerve block in patients undergoing total knee arthroplasty - a retrospective study. J Clin Anesth 2015;27:39–44. [DOI] [PubMed] [Google Scholar]
- [35].Report of the National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research: deliberations and conclusions. Hastings Cent Rep 1975;5:41–5. [PubMed] [Google Scholar]


