Abstract
Objectives
Mastery beliefs are known to contribute to healthy aging. However, it is an open question whether individual mastery–health associations impact the health of close long-term partners.
Method
We applied actor–partner interdependence models to 4-wave, 6-year longitudinal dyadic data from married and cohabitating partners in the Health and Retirement Study (N = 1,981 partners; age at baseline: M = 67 years, SD = 8.93, range 50−94 years).
Results
Higher individual mastery beliefs were associated with better individual physical health and health behaviors. Higher mastery beliefs were associated with subsequent increases in light physical activity. Having a partner with higher levels of mastery was uniquely associated with fewer functional limitations, better self-rated health, and more physical activity. Actor × Partner interaction effects for functional limitations indicated multiplicative associations of actor and partner mastery with health. Of note, mastery–health associations for individuals and their partners were invariant across age, gender, education, employment status, perceived stress over one’s own and partner’s health, and cognition.
Discussion
Findings suggest that partner mastery beliefs matter for the health (behaviors) of older adults. We discuss possible mechanisms underlying partner interrelations in mastery and health, their age invariance, and consider implications arising from our results.
Keywords: Dyads, Health, Health and Retirement Study (HRS), Mastery, Partners
Life span research has long acknowledged the relevance of mastery beliefs for successful aging (Bandura, 1997; Heckhausen & Schulz, 1995). Empirical research has demonstrated that mastery is positively associated with various health outcomes (Lachman, 2006; Rodin, 1986), including cardiovascular health (Roepke & Grant, 2011), physical functioning (Caplan & Schooler, 2003), and reduced mortality hazards (Surtees et al., 2010). These studies focused on associations at the individual level. It is an open question, whether and how mastery beliefs and health are related at the couple level. Individual functioning and development are profoundly shaped by the social contexts people live in (Bronfenbrenner, 1986). Spouses and long-term partners are known to constitute one such context because partners share a long history of idiosyncratic experiences and jointly deal with many of the same opportunities and challenges (Lang, 2001). In the current report, we extend previous research on associations between mastery and health in individuals to also examine links within couples. We also explore whether and how such associations at both individual and partner levels differ by age, gender, education, employment status, perceived stress over one’s own and one’s partners health, and cognition (Hoppmann & Gerstorf, 2016).
Associations of Mastery With Health and Health Behavior at Individual Levels
Mastery beliefs, perceptions of control, and personal agency all refer to beliefs about one’s capability to attain desired outcomes (Bandura, 1997; Skinner, 1996). We refer to mastery as people’s beliefs about their ability to influence and change life circumstances. Perceptions of mastery are a particularly important factor for successful aging (Lachman, Neupert, & Agrigoroaei, 2011). Specifically, mastery has been shown to be associated with the adoption and maintenance of health-related behaviors such as exercising regularly (Infurna & Gerstorf, 2014; Roepke & Grant, 2011), which in turn contributes to better health and maintenance over time (Lachman & Firth, 2004; Rodin, 1986; Sargent-Cox, Butterworth, & Anstey, 2014). Consistent with these theoretical perspectives, research suggests that mastery is associated with numerous health outcomes, including a lower risk for cardiovascular disease (Surtees et al., 2010), better functional capacity (Seeman, Unger, McAvay, & Mendes de Leon, 1999), fewer physical illnesses (Wurm, Tesch-Römer, & Tomasik, 2007), and longevity (Infurna, Ram, & Gerstorf, 2013).
Associations Between Mastery and Health and Health Behaviors at the Partner Level
Romantic relationships are a special social context because partners typically share significant portions of the life span with one another—they live in the same environment and have a stake in each other’s health because unresolved problems (e.g., in the health domain) often have ramifications for the lives of both partners (Berg & Upchurch, 2007). Longitudinal research on spousal health trajectories has shown that spouses and partners play an essential role in shaping each other’s health over years and decades (Khan, Stephens, Franks, Rook, & Salem, 2013; Watson, Beer, & Montez, 2014). One contributing factor may be that partners influence each other’s health behaviors (Ayotte, Margrett, & Patrick, 2013). A healthy spouse might increase the likelihood that their partner engages in healthy behaviors (e.g., fruit and vegetable consumption and physical activity). Jackson, Steptoe, and Wardle (2015) showed that the likelihood of remaining physically active was elevated if one’s spouse also maintained an active lifestyle. Similarly, using longitudinal data, Li, Cardinal, and Acock (2013) demonstrated that levels of physical activity were similar and coordinated between partners over time. However, little is known about how personal resources might contribute to these between-spousal associations in health. Individuals with higher levels of mastery may be expected to be more diligent about health and health behaviors—both for themselves and their partner. Based on the literature, we expect that higher mastery beliefs in one person are associated not only with his/her own health and health behavior but also the health and health behavior of his/her partner. Additionally, we test the interaction between partners’ mastery beliefs. For example, it could be that having a high mastery partner can improve health and compensate for an individual’s own low mastery. Having a low mastery partner, on the other hand, may increase the health vulnerability of a low mastery older adult.
The Present Study
In the present study, we examine dyadic associations of mastery beliefs with level and change in health and health behavior among older partners. To do so, we apply multilevel models to 6-year longitudinal data from 1,981 married and cohabitating partners in the Health and Retirement Study (HRS), a large-scale nationally representative sample in the United States (age at baseline: M = 67 years, SD = 8.93). We make use of three indicators of health status: (a) number of chronic health conditions involving persistent moderate-to-severe physical illnesses, (b) number of functional limitations in instrumental activities of daily living, and (c) self-rated health status. Our indicator of health behavior was the frequency of engaging in different types of physical activity (vigorous, moderate, and light).
Our first objective is to corroborate theoretical perspectives and earlier empirical reports that—at the individual level—mastery beliefs are associated with better health and health behavior. Our second objective is to move the study of mastery–health associations to the dyadic level and examine whether and how mastery beliefs are associated with health and health behavior of the partner. Acknowledging known correlates of mastery and health (Lachman, 2006; Mirowsky, 1995), our models control for individual age, gender, education, employment status, perceived stress over one’s own and one’s partners health, and cognitive functioning. To illustrate, being older, being a woman, unemployment, and having a lower level of education have each been associated with lower mastery and poor health (Lachman & Weaver, 1998). For example, being highly educated and employed may provide people with access to resources (e.g., health care and economic resources) and may influence social norms, which in turn contribute to mastery beliefs, healthy behavior, and health prevention (Ross & Mirowsky, 2002). It is also known that perceptions of one’s health are intertwined with her/his partner’s physical health trajectories (Li et al., 2013). It thus appears reasonable to assume that being stressed by one’s health problems and those of one’s partner also undermine people’s perception of mastery. Finally, levels of cognitive functioning are long known to be closely linked with mastery beliefs, be it as precursor or a consequence (see Lachman’s integrative model; Lachman, 2006). For example, more frequent and severe cognitive declines may reduce the opportunities people may have to exert mastery through processes of strategy production and selection (Dunlosky & Hertzog, 1998).
Method
Sample and Procedure
The HRS is a biennial longitudinal study of a nationally representative probability sample of Americans over the age of 50 (Sonnega et al., 2014). HRS samples by household and interviews both partners in a household if present. In 2006, the HRS introduced an enhanced face-to-face interview for a random 50% of the eligible households. After the interview, participants were given a self-administered psychosocial questionnaire to complete and return by mail (for further details, see Smith et al., 2013). In the current study, we use health data collected in 2006, 2008, 2010, and 2012; mastery data were collected in 2006; sociodemographic covariates were obtained from a cross-wave tracker file.
We selected data from heterosexual cohabiting partners in which both partners completed measures of mastery and health in 2006 (N = 3,962; i.e., 1,981 partners). The partners in this study differed from the remaining HRS participants on several variables of interest: they had higher levels of mastery (d = 0.07); were younger (d = 0.10); had fewer chronic health conditions (d = 0.03); reported fewer limitations in physical functioning (d = 0.14); perceived their health as better (d = 0.13); and engaged in more light (d = 0.12), moderate (d = 0.12), and vigorous (d = 0.06) physical activities. We also compared individuals who only contributed data at Time 1 to individuals who had two or more waves of data. The latter had higher levels of mastery (d = 0.36); were younger (d = 0.90); had fewer chronic health conditions (d = 0.28); reported fewer limitations in physical functioning (d = 0.32); perceived their health as better (d = 0.51); and engaged in more light (d = 0.76), moderate (d = 0.41), and vigorous (d = 0.35) physical activities. As a consequence, our findings may not necessarily generalize to less positively selected population strata.
Measures
Mastery was assessed using 5 items from Pearlin and Schooler’s Mastery Scale (1978; e.g., “I can do just about anything I really set my mind to do.”) that ask participants about their perceived ability to influence life circumstances. Responses were provided on a 6-point scale (1 = strongly disagree; 6 = strongly agree; Cronbach’s α = 0.89). Higher scores indicate higher levels of mastery.
Health and health behavior
We use three different aspects of health and one indicator of health behavior. First, chronic health conditions were assessed by the number of self-reported physical comorbidity across eight physician-diagnosed major chronic illnesses including (1) high blood pressure; (2) diabetes; (3) cancer or any malignant tumor (excluding minor skin cancer); (4) lung disease; (5) coronary heart disease including heart attacks, angina, and congestive heart failure; (6) emotional, nervous, or psychiatric problems; (7) arthritis or rheumatism; and (8) stroke. Global scores on self-reported disease have been shown to be a more reliable indicator of health than self-reports of single illnesses (Katz, Chang, Sangha, Fossel, & Bates, 1996).
Second, limitations of physical functioning were a summed measure of 10 instrumental activities of daily life (see Gerstorf, Hoppmann, Kadlec, & McArdle, 2009). Participants reported whether they experienced difficulty using the phone, managing money, taking medications, shopping for groceries, preparing hot meals, walking several blocks, climbing one flight of stairs, lifting or carrying 10 lbs of weight, picking up a dime, and pushing or pulling large objects. Participants answered items (e.g., “Because of a health problem do you have any difficulty …?”) using a 2-point scale (1 = yes; 0 = no). Analyses are based on a sum score with higher scores indicating more limitations.
Third, self-rated health was assessed using a single item (“Would you say your health is …?”), with participants rating their health on a 5-point Likert-type scale (1 = poor; 5 = excellent). Self-rated health has been shown to be associated with subsequent key health outcomes, including mortality (Idler & Benyamini, 1997).
Finally, health behavior was assessed by asking participants separate questions about how often they engage in vigorous activities (“How often do you take part in sports or activities that are vigorous, such as running or jogging, swimming, cycling, aerobics, or gym workout, tennis, or digging with a space or shovel?”), moderate activities (“How often do you take part in sports or activities that are moderately energetic such as gardening, cleaning the car, walking at a moderate pace, dancing, floor or stretching exercises?”), and light activities (“How often do you take part in sports or activities that are mildly energetic, such as vacuuming, laundry, and home repairs?”). Responses were coded on a 5-point Likert-type scale (1 = every day; 5 = hardly ever or never). We reverse coded responses such that higher scores indicate more physical activity.
Cognitive functioning
As an indicator of cognition, we included episodic memory, as indexed by a sum of performance scores on immediate and delayed free recall tests (Ofstedal et al., 2005). Participants were presented with a list of 10 nouns and asked to recall as many words as possible both immediately after presentation and after a delay of approximately 5min. Scores were calculated as the total sum of words correctly remembered between both tasks (ranging from 0 to 10). Higher scores indicated better performance.
Perceived stress over one’s own and one’s partners health problems
Perceived stress was assessed asking participants two questions about whether or not they or their partner experienced current and ongoing health problems that have lasted 12 months or longer and if so, how upsetting the health problem had been (1 = didn’t happen; 4 = yes, very upsetting).
Sociodemographic covariates
We included age, gender (−1 = men; 1 = women), education (−1 = high school education or less; 1 = at least some college education), and employment status (−1 = not, 1 = yes) as covariates in our models.
Statistical Analyses
We used multilevel modeling for dyadic data analysis to account for the interdependence of individuals within dyads (Kenny, Kashy, & Cook, 2006). We use the term “actor effects” to refer to estimates for each partner (i.e., intrapartner effect), whereas the term “partner effects” refers to estimates for associations between partners (i.e., interpartner effects). These models allow for estimating both associations between one person’s mastery and his/her own health (i.e., actor effects) and associations between her/his partner’s mastery and her/his health (i.e., partner effects) while accounting for the statistical nonindependence of members in a couple. Dyadic models were specified for women (subscript w) and men (subscript m) as,
| (1) |
and
| (2) |
where health (-behavior)ti of person i at time t is a function of a person-specific intercept coefficient, β0i, a person-specific coefficient, β1i, which characterizes change across time, and residual error, eti, which may be correlated within dyad. Between-person differences in intercept (β0i) and slope (β1i) coefficients were modeled as:
| (3) |
| (4) |
and
| (5) |
| (6) |
where γ00 and γ10 indicate level of and changes in health for the typical woman and man the other γ parameters indicate the extent to which differences in levels of and changes in health (behavior) are related to age at T1, education, employment status, perceived stress over one’s own and one’s partners health, cognitive functioning, mastery actor, mastery partner, the interaction between mastery actor and partner, and residual unexplained differences, us, which may be correlated across women, men, and dyads. The γ parameters were assumed to be equal for women and men for the main model, but gender differences in these parameters were also tested.
We used the full information maximum likelihood estimation algorithm that accommodates incomplete data under the data-missing-at-random (MAR) assumption (Little & Rubin, 1987). To accommodate obvious violations of MAR assumptions, our models incorporated a number of attrition-relevant variables: actor age, gender, education, employment status, perceived stress, and several health variables, thereby alleviating problems associated with nonrandom attrition. Statistical analyses were conducted using SPSS (v. 22). The longitudinal dyadic data use heterosexual couples. Thus, we use the distinguishable case for dyadic data analyses in which the intercepts and slopes can be estimated for men and women separately. If no significant gender differences in the actor/partner effects emerge (i.e., the effects are not “distinguishable” between men and women), the effects of men and women are pooled to yield single estimates for actors and partners across gender.
Descriptive statistics and intercorrelations at the baseline assessment are presented in Table 1. At the bivariate level, mastery is associated with actor variables (e.g., among husbands, r = −.11 for chronic health conditions; among wives, r = −.15 for chronic health conditions). Intercorrelations among the four aspects of health included in our study are in the small to moderate range (from r = .32 for light physical activity and self-rated health to r = −.46 for self-rated health and chronic conditions), suggesting that the health and health behavior variables indeed tap into different aspects of health.
Table 1.
Descriptive Statistics and Intercorrelations for Variables in Study at Wave 1
| Intercorrelations | M | SD | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | |||
| 1. Mastery (1–6) | 1 | −0.070** | 0.126** | 0.076** | −0.197** | −0.114** | 0.107** | −0.152** | −0.212** | 0.259** | 0.110** | 0.126** | 0.141** | 4.83 | 1.05 |
| 2. Age (50–95) | −0.077** | 1 | −0.134** | −0.471** | 0.066** | −0.007 | −0.320** | 0.249** | 0.125** | −0.135** | −0.089** | −0.098** | −0.111** | 65.34 | 8.67 |
| 3. Education (−1; 1) | 0.082** | −0.164** | 1 | 0.183** | −0.092** | 0.019 | 0.294** | −0.176** | −0.206** | 0.326** | 0.082** | 0.192** | 0.187** | 45.9a | |
| 4. Employment status (−1; 1) | 0.081** | −0.505** | 0.197** | 1 | −0.144** | 0.006 | 0.244** | −0.229** | −0.212** | 0.223** | 0.051* | 0.072** | 0.039 | 37.5b | |
| 5. Stress over health (1–4) | −0.196** | 0.073** | −0.105** | −0.194** | 1 | 0.206** | −0.095** | 0.409** | 0.441** | −0.546** | −0.126** | −0.196** | −0.176** | 2.06 | 0.99 |
| 6. Stress over partner health (1–4) | −0.074** | −0.029 | −0.005 | −0.005 | 0.293** | 1 | 0.021 | 0.164** | 0.093** | −0.080** | −0.023 | −0.056* | −0.035 | 1.80 | 1.04 |
| 7. Cognitive functioning (0–10) | 0.076** | −0.365** | 0.316** | 0.274** | −0.110** | 0.012 | 1 | −0.160** | −0.202** | 0.268** | 0.103** | 0.134** | 0.107** | 4.87 | 1.91 |
| 8. Chronic health conditions (0–8) | −0.106** | 0.300** | −0.156** | −0.314** | 0.420** | 0.080** | −0.207** | 1 | 0.355** | −0.449** | −0.173** | −0.209** | −0.177** | 1.86 | 1.32 |
| 9. Functional limitations (0–10) | −0.240** | 0.164** | −0.202** | −0.248** | 0.424** | 0.124** | −0.228** | 0.409** | 1 | −0.530** | −0.221** | −0.329** | −0.237** | 0.98 | 1.56 |
| 10. Self-rated health (1–5) | 0.205** | −0.123** | 0.280** | 0.227** | −0.489** | −0.143** | 0.208** | −0.435** | −0.480** | 1 | 0.211** | 0.332** | 0.276** | 3.37 | 1.03 |
| 11. Light physical activity (1–5) | 0.126** | −0.136** | 0.143** | 0.090** | −0.160** | 0.047* | 0.165** | −0.193** | −0.294** | 0.231** | 1 | 0.365** | 0.161** | 3.81 | 0.89 |
| 12. Moderate physical activity (1–5) | 0.104** | −0.068** | 0.144** | 0.087** | −0.189** | −0.022 | 0.094** | −0.206** | −0.385** | 0.288** | 0.429** | 1 | 0.343** | 3.22 | 1.31 |
| 13. Vigorous physical activity (1–5) | 0.055* | −0.119** | 0.119** | 0.124** | −0.162** | −0.038 | 0.109** | −0.205** | −0.236** | 0.270** | 0.235** | 0.335** | 1 | 1.93 | 1.32 |
| M | 4.81 | 68.41 | 49.4a | 40.9b | 1.97 | 1.66 | 4.20 | 1.95 | 0.72 | 3.29 | 3.34 | 3.36 | 2.24 | ||
| SD | 1.09 | 8.93 | 0.94 | 0.96 | 1.78 | 1.41 | 1.46 | 1.06 | 1.14 | 1.23 | 1.40 | ||||
Notes. N = 1,981 partners. Statistics for men presented below the diagonal and those for women above the diagonal.
a% Some college education or higher.
b% Employed.
*p < .05, **p < .01.
Results
Associations of Mastery With Health and Health Behavior at Individual Levels
Results from our multilevel actor–partner interdependence model for each health (behavior) outcome variable are presented in Tables 2 and 3. Over time, the number of chronic health conditions (γ = 0.082) increased over the 6-year period, whereas functional limitations (γ = −0.388) decreased. Light, moderate, and vigorous physical activity increased over time (γ = 0.147, γ = 0.136, γ = 0.089, respectively). Older age and lower education were each associated with poor health and steeper health declines. In particular, older age was associated with more chronic conditions (γ = 0.028), more functional limitations (γ = 0.031) as well as fewer activities at all three levels (light: γ = −0.018; moderate: γ = −0.015; vigorous: γ = −0.017). Women reported more functional limitations (γ = 0.167), but better self-rated health (γ = 0.050), and fewer chronic conditions (γ = – 0.056) as well as more light but less moderate and vigorous activities (light: γ = 0.234; moderate: γ = −0.081; vigorous: γ = −0.142). Higher education was associated with fewer chronic conditions (γ = −0.060), fewer functional limitations (γ = −0.090), higher self-rated health (γ = 0.125) as well as more light and moderate physical activity (light: γ = 0.050, γ = 0.133). Being employed was associated with fewer chronic conditions (γ = −0.149), fewer functional limitations (γ = −0.160), higher self-rated health (γ = 0.070), but not physical activity.
Table 2.
Multilevel Actor–Partner Interdependence Model for Several Physical Health Indicators
| Chronic conditions | Functional limitations | Self-rated health | ||||
|---|---|---|---|---|---|---|
| Estimates (SE) | r | Estimates (SE) | r | Estimates (SE) | r | |
| Fixed effects | ||||||
| Intercept | −0.581** (0.209) | −1.363** (0.250) | 3.988** (0.125) | |||
| Slope | 0.082** (0.025) | 0.18 | −0.388** (0.054) | 0.15 | 0.039 (0.027) | 0.03 |
| Age | 0.028** (0.003) | 0.06 | 0.031** (0.003) | 0.18 | −0.003 (0.002) | 0.10 |
| Gender | −0.056** (0.019) | 0.05 | 0.167** (0.023) | 0.16 | 0.050** (0.011) | 0.17 |
| Education | −0.060** (0.021) | 0.10 | −0.090** (0.025) | 0.06 | 0.125** (0.012) | 0.08 |
| Employment status | −0.149** (0.023) | 0.38 | −0.160** (0.028) | 0.10 | 0.070** (0.014) | 0.50 |
| Stress over health | 0.526** (0.021) | 0.03 | 0.609** (0.026) | 0.38 | −0.432** (0.013) | 0.002 |
| Stress over partners health | 0.040** (0.020) | 0.06 | 0.012 (0.024) | 0.01 | −0.002 (0.012) | 0.16 |
| Cognitive functioning | −0.041** (0.011) | 0.05 | −0.161** (0.014) | 0.20 | 0.067** (0.007) | 0.12 |
| Mastery actor | −0.052** (0.019) | 0.00 | −0.168** (0.023) | 0.13 | 0.085** (0.011) | 0.06 |
| Mastery partner | −0.003 (0.018) | 0.01 | −0.054** (0.022) | 0.04 | 0.041** (0.011) | 0.02 |
| Mastery actor × Partner | −0.004 (0.017) | 0.03 | 0.059** (0.020) | 0.07 | −0.009 (0.010) | 0.08 |
| Slope × Age | 0.000 (0.000) | 0.09 | 0.008** (0.001) | 0.24 | −0.001** (0.000) | 0.04 |
| Slope × Gender | −0.009** (0.002) | 0.001 | 0.003 (0.005) | 0.02 | 0.004 (0.003) | 0.02 |
| Slope × Education | 0.000 (0.002) | 0.01 | −0.006 (0.005) | 0.02 | −0.003 (0.003) | 0.01 |
| Slope × Employment status | −0.001 (0.003) | 0.03 | 0.002 (0.006) | 0.01 | −0.001 (0.003) | 0.10 |
| Slope × Stress over health | 0.005 (0.003) | 0.03 | 0.017** (0.006) | 0.06 | 0.016** (0.003) | 0.03 |
| Slope × Stress over partners health | 0.004 (0.002) | 0.05 | 0.000 (0.005) | 0.001 | −0.005 (0.003) | 0.00 |
| Slope × Memory | −0.004** (0.001) | 0.01 | −0.020** (0.003) | 0.13 | 0.000 (0.002) | 0.02 |
| Slope × Mastery actor | −0.002 (0.002) | 0.01 | −0.001 (0.005) | 0.01 | −0.002 (0.002) | 0.003 |
| Slope × Mastery partner | −0.001 (0.002) | 0.03 | −0.003 (0.005) | 0.01 | 0.000 (0.002) | 0.03 |
| Slope × Master actor × Partner | −0.003 (0.002) | 0.06 | 0.005 (0.004) | 0.03 | −0.003 (0.002) | 0.03 |
| Random effects | ||||||
| Var. intercept male | 1.501** (0.051) | 1.775** (0.073) | 0.469** (0.019) | |||
| Var. intercept female | 1.341** (0.044) | 1.721** (0.067) | 0.387** (0.015) | |||
| Var. slope male | 0.016** (0.001) | 0.046** (0.004) | 0.005** (0.001) | |||
| Var. slope female | 0.013** (0.001) | 0.035** (0.003) | 0.005** (0.001) | |||
| Cov. intercept male, intercept female | 0.242** (0.035) | 0.252** (0.050) | 0.076** (0.013) | |||
| Cov. intercept male, slope male | 0.039** (0.005) | 0.194** (0.013) | 0.016** (0.003) | |||
| Cov. intercept female, slope female | 0.028** (0.004) | 0.149** (0.011) | 0.015** (0.002) | |||
| Cov. intercept male, slope female | 0.009** (0.004) | 0.006 (0.011) | 0.000 (0.003) | |||
| Cov. slope male, intercept female | 0.002 (0.004) | 0.006 (0.011) | −0.004 (0.003) | |||
| Cov. slope male, slope female | 0.001 (0.001) | 0.002 (0.003) | 0.000 (0.001) | |||
| Residual male | 0.104** (0.003) | 0.677** (0.021) | 0.388** (0.010) | |||
| Residual female | 0.081** (0.002) | 0.770** (0.021) | 0.311** (0.007) | |||
| Cov. residual male, female | 0.052** (0.018) | 0.030 (0.022) | 0.052** (0.018) | |||
| Goodness-of-fit indices | ||||||
| AIC | 26,659 | 40,303 | 32,704 | |||
| −2LL | 26,633 | 40,277 | 32,678 | |||
Notes. N = 1,981 partners who provided 7,733 observations. Unstandardized estimates are presented, with SEs in parentheses. Gender: −1 = men, 1 = women. Education: −1 = low education, 1 = high education. Employment status: −1 = not working, 1 = working. Var = variance. Cov = covariance. AIC = Akaike Information Criterion; −2LL = −2 log likelihood, relative model fit statistics.
*p < .05. **p < .01.
Table 3.
Multilevel Actor–Partner Interdependence Model for Several Physical Health Indicators
| Light | Moderate | Vigorous | ||||
|---|---|---|---|---|---|---|
| Estimates (SE) | r | Estimates (SE) | r | Estimates (SE) | r | |
| Fixed effects | ||||||
| Intercept | 4.501** (0.126) | 4.237** (0.165) | 3.402** (0.174) | |||
| Slope | 0.147** (0.034) | 0.08 | 0.136** (0.042) | 0.06 | 0.089** (0.043) | 0.04 |
| Age | −0.018** (0.002) | 0.20 | −0.015** (0.002) | 0.12 | −0.017** (0.002) | 0.13 |
| Gender | 0.234** (0.012) | 0.39 | −0.081** (0.014) | 0.13 | −0.142** (0.015) | 0.21 |
| Education | 0.050** (0.013) | 0.07 | 0.113** (0.016) | 0.12 | 0.104 (0.017) | 0.10 |
| Employment status | −0.011 (0.014) | 0.01 | 0.006 (0.018) | 0.01 | −0.001 (0.019) | 0.001 |
| Stress over health | −0.140** (0.013) | 0.18 | −0.207** (0.017) | 0.21 | −0.191** (0.017) | 0.18 |
| Stress over partners health | 0.034** (0.012) | 0.05 | −0.003 (0.016) | 0.003 | 0.001 (0.016) | 0.001 |
| Cognitive functioning | 0.062** (0.007) | 0.15 | 0.057** (0.009) | 0.10 | 0.032** (0.009) | 0.001 |
| Mastery actor | 0.067** (0.012) | 0.10 | 0.050** (0.015) | 0.06 | 0.059** (0.015) | 0.06 |
| Mastery partner | 0.031** (0.011) | 0.05 | 0.039** (0.014) | 0.05 | 0.032** (0.015) | 0.04 |
| Mastery actor × Partner | 0.001 (0.010) | 0.003 | 0.009 (0.013) | 0.02 | 0.018 (0.014) | 0.03 |
| Slope × Age | −0.003** (0.000) | 0.15 | −0.003** (0.001) | 0.11 | −0.002** (0.001) | 0.05 |
| Slope × Gender | 0.003 (0.003) | 0.02 | 0.004 (0.004) | 0.02 | 0.008 (0.004) | 0.04 |
| Slope × Education | 0.004 (0.003) | 0.02 | 0.000 (0.004) | 0.000 | 0.001 (0.004) | 0.004 |
| Slope × Employment status | 0.003 (0.004) | 0.02 | −0.002 (0.005) | 0.01 | 0.005 (0.005) | 0.02 |
| Slope × Stress over health | −0.008** (0.004) | 0.04 | −0.001 (0.004) | 0.006 | 0.004 (0.005) | 0.02 |
| Slope × Stress over partner health | −0.001 (0.003) | 0.01 | −0.007 (0.004) | 0.03 | −0.003 (0.004) | 0.01 |
| Slope × Memory | 0.007** (0.002) | 0.06 | 0.008** (0.002) | 0.06 | 0.001 (0.002) | 0.01 |
| Slope × Mastery actor | 0.006** (0.003) | 0.03 | −0.008** (0.004) | 0.04 | −0.006 (0.004) | 0.03 |
| Slope × Mastery partner | 0.000 (0.003) | 0.001 | 0.004 (0.004) | 0.02 | 0.003 (0.004) | 0.01 |
| Slope × Master actor × Partner | 0.001 (0.003) | 0.01 | −0.003 (0.003) | 0.02 | −0.002 (0.003) | 0.02 |
| Random effects | ||||||
| Var. intercept male | 0.494** (0.024) | 0.600** (0.028) | 0.760** (0.034) | |||
| Var. intercept female | 0.300** (0.015) | 0.693** (0.031) | 0.717** (0.031) | |||
| Var. slope male | 0.007** (0.002) | 0.011** (0.002) | 0.012** (0.002) | |||
| Var. slope female | 0.005** (0.001) | 0.011** (0.002) | 0.016** (0.002) | |||
| Cov. intercept male, intercept female | 0.053** (0.014) | 0.182** (0.022) | 0.244** (0.024) | |||
| Cov. intercept male, slope male | 0.011 (0.004) | 0.013** (0.005) | −0.011 (0.006) | |||
| Cov. intercept female, slope female | 0.014** (0.003) | 0.008 (0.005) | −0.001 (0.005) | |||
| Cov. intercept male, slope female | −0.008** (0.004) | −0.001 (0.005) | −0.018** (0.006) | |||
| Cov. slope male, intercept female | −0.002 (0.004) | 0.007 (0.006) | −0.005 (0.006) | |||
| Cov. slope male, slope female | 0.001 (0.001) | 0.004** (0.002) | 0.001 (0.002) | |||
| Residual male | 0.743** (0.018) | 0.819** (0.020) | 0.938** (0.023) | |||
| Residual female | 0.507** (0.012) | 0.865** (0.021) | 0.805** (0.019) | |||
| Cov. residual male, female | 0.007** (0.018) | 0.072** (0.018) | 0.081** (0.017) | |||
| Goodness-of-fit indices | ||||||
| AIC | 38,640 | 43,906 | 44,746 | |||
| −2LL | 38,614 | 43,880 | 44,720 | |||
Notes. N = 1,981 partners who provided 7,733 observations. Unstandardized estimates are presented, with SEs in parentheses. Gender: −1 = men, 1 = women. Education: −1 = low education, 1 = high education. Employment status: −1 = not working, 1 = working. Var = variance. Cov = covariance. AIC = Akaike Information Criterion; −2LL = −2 log likelihood, relative model fit statistics.
*p < .05. **p < .01.
Perceiving stress over one’s own health was associated with more chronic conditions (γ = 0.526), more functional limitations (γ = 0.609), lower self-rated health (γ = – 0.432) as well as fewer activities at all three levels (light: γ = −0.140; moderate: γ = −0.207; vigorous: γ = −0.191). Perceiving stress over one’s partners health was associated with more chronic conditions (γ = 0.040), but more light physical activity (γ = 0.034). Better cognitive functioning was associated with fewer chronic conditions (γ = −0.041), fewer functional limitations (γ = −0.161), higher self-rated health (γ = 0.067) as well as more physical activity (light: γ = 0.062; moderate: γ = 0.057; vigorous: γ = 0.032). Over time, being older was associated with increased chronic conditions (γ = 0.082), but surprisingly fewer functional limitation (γ = −0.388). Additionally, women experienced smaller increases in chronic conditions over a 6-year period (γ = −0.009).
Most importantly, actor–level associations of mastery beliefs with health and health behavior emerged. Specifically, higher levels of mastery were associated with fewer chronic conditions (γ = −0.052), fewer functional limitations (γ = −0.168), better self-rated health (γ = 0.085) as well as more physical activity at light (γ = 0.067), moderate (γ = 0.050), and vigorous levels (γ = 0.059). Over time, higher mastery beliefs at baseline assessment were associated with larger increases in light physical activity (γ = 0.006) but decrease in moderate physical activity (γ = −0.008).
Associations of Mastery With Health and Health Behavior at Partner Levels
Tables 2 and 3 also present partner effects that can be interpreted as contributing to health (behavior) over-and-above the actor effects. Having a partner with higher levels of mastery was uniquely associated with fewer functional limitations (γ = −0.054), better self-rated health (γ = 0.041), and more physical activity at light (γ = 0.031), moderate (γ = 0.39), and vigorous level (γ = 0.032). The effects of partner mastery on health outcomes and behavior did not change over time.
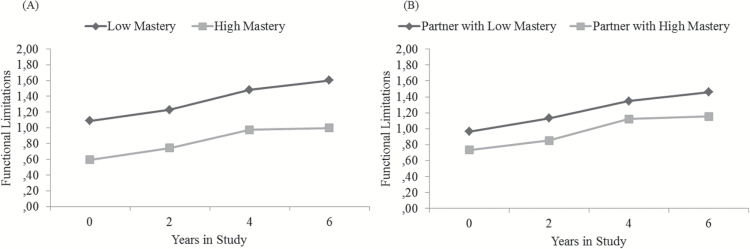
To illustrate the size and direction of effects, Figure 1 shows actor associations (left-hand Panel A) and partner associations (right-hand Panel B) between mastery at baseline and functional limitations over the duration of the study. Panel A shows that relative to participants with low mastery beliefs (−1 SD; dark diamonds), those with high mastery beliefs (+1 SD; gray squares) reported fewer functional limitations consistently across the 6 years. Panel B shows that relative to participants whose partner reported low mastery beliefs (−1 SD; dark diamonds), those with a partner reporting high mastery beliefs (+1 SD; gray squares) reported fewer functional limitations consistently across the waves of the study.
Figure 1.
Actor associations (left-hand Panel A) and partner associations (right-hand Panel B) between mastery at baseline and functional limitations over the duration of the study. Panel A shows that relative to Health and Retirement Study participants who perceived low mastery (−1 SD; dark diamonds), those who perceived high mastery (+1 SD; gray squares) reported fewer functional limitations consistently across four waves of the study. Panel B shows that relative to Health and Retirement Study participants whose partner perceived low mastery (−1 SD; dark diamonds), those who had a partner perceiving high mastery (+1 SD; gray squares) also reported lower functional limitations consistently across the four waves of the study.
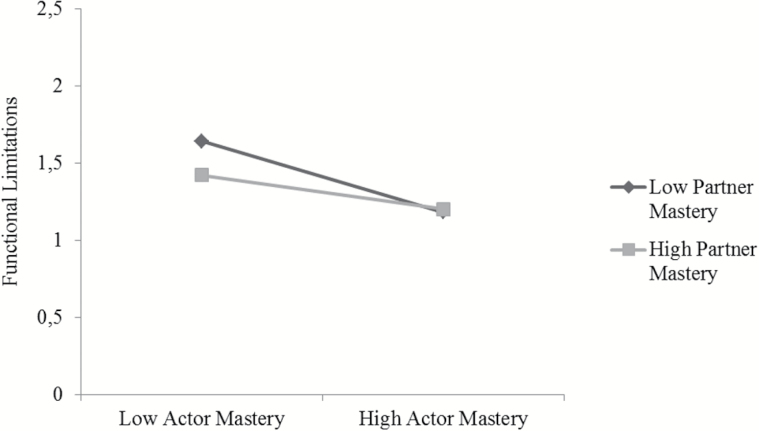
A significant Actor × Partner interaction effect emerged, suggesting a multiplicative association of actor and partner mastery with functional limitations. As illustrated in Figure 2, when actor mastery beliefs were high, the level of partner mastery beliefs was not relevant for functional limitations. However, when actor mastery beliefs are low, the level of partner mastery beliefs indeed mattered, with the combination of low actor mastery beliefs with low partner mastery beliefs being associated with particularly elevated functional limitations.
Figure 2.
Actor × Partner interactions predicting functional limitations. The fewest functional limitations were found among partners in which both members were high in mastery.
In a series of follow-up analyses, we introduced interaction terms for age, gender, employment status, and education with the actor/partner effects. None of these interactions were significant. In a series of additional analyses, we additionally covaried for personality traits of conscientiousness and optimism that had both been linked to health and health behavior in earlier reports (Kim, Chopik, & Smith, 2014; Roberts, Smith, & Edmonds, 2009). Although conscientiousness and optimism were found to be associated with the health variables under study, the partner effects of mastery were substantively identical to those reported in the main text.
Discussion
The major objective of the current study was to examine dyadic associations of mastery with health and health changes among older partners. For individuals, higher mastery beliefs were associated with better physical health and health behaviors and predicted increases in light physical activity. Independent of these actor effects, having a partner with higher levels of mastery was uniquely associated with fewer functional limitations, better self-rated health, and higher levels of physical activities. We also found Actor × Partner interaction effects for functional limitations, indicating evidence for multiplicative associations of actor and partner mastery with health. Of note, all mastery–health (behavior) associations were found to be invariant across age, gender, education, employment status, perceived stress over one’s (and their partner’s) health, and cognitive functioning. Our results reveal that mastery–health (behavior) associations generalize beyond the individual level and emerge within couples, indicating that individual developmental outcomes are intertwined in romantic relationships.
Associations of Mastery With Health and Health Behavior at Individual Levels
Several empirical studies suggest that the health-enhancing nature of mastery is carried from direct and indirect pathways (Caplan & Schooler, 2003). People who perceive themselves as mastering the challenges of their lives well have healthier lifestyles and make better use of their resources so that health limitations can be buffered (Bandura, 2004). In our study, we substantiate this line of research by utilizing data from a heterogeneous and nationwide sample of U.S. couples aged 50 and older. Additionally, we did not focus on one, but rather several indicators of health. We observed that most indicators of health and health behavior were associated with higher levels of mastery. Thus, our results are consistent with proposals about the breadth of mastery–health associations (McAvay, Seeman, & Rodin, 1996). For future inquiry, it would be highly informative to include objective or performance-based measures of physical health and functioning (e.g., grip strength and lung volume) to extend associations between mastery and health beyond self-report data. Acknowledging that mastery beliefs are often modifiable (Sorkin et al., 2014), our findings have implications for the design of interventions aimed at maintaining health into older age.
Associations of Mastery With Health and Health Behavior in Couples
Our findings help to further explicate the health relevance of close others, including why some married people are in better health and face lower mortality hazards compared with unmarried people (Lewis & Butterfield, 2007). Partners might not only motivate each other to engage in health-promoting behavior but also share most of their daily experiences together. Having a partner with high levels of mastery might foster one’s own health insofar as partners feel as though they have some degree of control in promoting their partners’ health and well-being. On the other hand, our results indicate that spouses may increase each other’s risks for poorer health. It is thus necessary to further investigate the specific role of mastery for health behavior and outcomes in partners’ health.
Our focus had been on physical activity as a key health-enhancing behavior. We note that such health-enhancing behavior differs in the degree to which these are performed together or alone. To illustrate, some physical activities can be performed together (e.g., going for a walk, physical exercise, and dieting), whereas other types of health behavior (e.g., cancer screenings) are usually performed alone. Generalizing from the current findings, we would expect that health behavior typically performed alone would be more pronounced among people with partners high in mastery, but such dyadic associations may be weaker compared with health behavior that is typically performed together (see Ayotte, Margrett, & Patrick, 2013). We note, however, that such speculation would need to be tested empirically with the appropriate data. Future research should also investigate the role of partner mastery for health-compromising behavior (e.g., smoking and alcohol abuse) that might also undermine one’s overall health status, for which there is some evidence (Mudde, Kok, & Strecher, 1995). For example, we would expect that health-compromising behavior such as excessive drinking would be lower among people with partners high in mastery (Falba & Sindelar, 2008).
The current findings can also be placed into the context of the literature on external social control (Lewis & Butterfield, 2007). Health-related social control refers to interpersonal interactions that involve influencing and constraining the health behaviors of another person through strategies like verbal persuasion and social pressure. There is mixed evidence as to whether social control is beneficial for health (Stephens et al., 2010; Westmaas, Wild, & Ferrence, 2002). That mastery more or less uniformly relates to better health (behavior) at both the individual and couple level suggests that mastery beliefs may be distinct from external social control (Lachman, Neupert, & Agrigoroaei, 2011). Additionally, mastery was measured in our study as an individual characteristic, whereas social control measures target the dyadic component of influencing another person’s behavior (e.g., asking whether the person thinks his or her partner checks that the person has actually done what he or she was supposed to do). It is therefore conceivable that mastery functions both as an intrapersonal and interpersonal resource. To illustrate, individuals high in mastery might motivate their partner by being role models for good health instead of exercising control over their partner’s behavior.
We note that marriage can operate as either a protective or risk factor for health (DeLongis, Capreol, Holtzman, O’Brien, & Campbell, 2004). It would thus be highly informative if future research were to disentangle whether preserved mastery beliefs in one partner serve as a protective factor against health (behavior) decline in the other partner, whether compromised mastery beliefs in one partner act as a risk factor for health (behavior) declines in the other partner, or whether both mechanisms are operating at the same time (Burkert, Scholz, Gralla, Roigas, & Knoll, 2011).
Limitations and Outlook
We note several limitations of our study. First, most data were based on self-reports. Even though self-report measures of health have been shown to be reliable (Katz et al., 1996), it is also known that reference group comparisons and systematically different standards of health bias self-report measures (Dowd & Todd, 2011). Consequently, it would be informative to make use of more objective measures of physical health (behavior), including documented clinical medical diagnoses, biomarkers of health, and accelerometer-based activity levels. In addition, this research would benefit from the inclusion of fine-grained indicators of physical activity (e.g., duration, total energy expenditure, or mode) as to differentiate specific types of activity that benefit the most from mastery. Similarly, with episodic memory, we only included a single indicator for cognitive functioning in our analyses; other, more elaborate cognitive measures may provide better indication of cognitive performance. It is an open question whether indicators of cognitive functioning that typically evince earlier and steeper forms of deterioration (perceptual speed; Gerstorf, Ram, Lindenberger, & Smith, 2013) would account for a larger share of the variance in mastery–health (behavior) associations. We also acknowledge that our selection of indicators was restricted by the measures available from the HRS assessment protocol. It would have been highly informative to examine further dyadic factors that may shape health (behavior) in older partners, such as dieting and prevention (e.g., cancer screenings).
Second, the structure of the data set only allowed us to examine how mastery beliefs assessed at a given point in time are associated with health (behavior) over time rather than how dyadic changes in mastery are coordinated with changes in health (behavior) over time. Drawing from studies at the individual level, Infurna et al. (2013), for example, reported that both higher levels of and more positive changes in mastery were associated with longevity, independent of sociodemographic correlates. It would be intriguing to examine whether and how such associations generalize to the partner level. One could expect that both change mechanisms are operating at the same time. It would also be intriguing to examine whether or not change–change associations would be different for husbands and wives. To illustrate, a diabetes diagnosis received by one partner could plausibly result in declining mastery of both partners over time because changes in lifestyle and social roles might be initiated. This in turn might be associated with declines in health (behavior) in both individuals. Similarly, with the current study, we cannot draw firm inferences about temporal ordering and causality in how mastery relates to health and health behavior in older partners. Our main goal was to describe how mastery of one person predicts health and health behavior in their partner. Acknowledging the multidirectionality of development (Baltes, Lindenberger, & Staudinger, 2006), health behavior may operate as an antecedent condition for, as well as a consequence of, mastery beliefs.
Third, results indicated a decline in functional limitations. The surprising direction of this effect may be attributable to the numerous interactions included in our models. This is a common issue when higher order interactions implicating those terms are included (Ludlow & Klein, 2014). Excluding these interactions from the model produced estimates for the main effect of time that were intuitive (on average, health and health behavior decline over time and chronic conditions and functional limitations increase over time), suggesting that these surprising results are of little substance.
Finally, our partner sample and particularly those who provided longitudinal change information were a positive selection of the population drawn from. Our findings may thus not necessarily generalize to less positively selected population strata. For example, it is possible that different associations emerge at both individual and dyadic levels among certain at-risk subpopulations (e.g., weaker dyadic associations among couples in which one partner has transitioned into a nursing home).
Conclusions
Taken together, our analyses of dyadic data from the HRS indicate that mastery is not only associated with better health and health behavior at the individual level but also between partners, suggesting that individual developmental outcomes are intertwined in close relationships. Interestingly, these associations were found to be invariant across age, gender, perceived stress over one’s own and one’s partner health, cognitive functioning, and socioeconomic population strata. More mechanism-oriented research is needed to pave the way for a better understanding the underlying pathways.
Funding
J.D. was funded by the International Max Planck Research School on the Life Course (http://www.imprs-life.mpg.de/). The Health and Retirement Study is sponsored by National Institute on Aging (NIA) grant NIA U01AG009740 and conducted by the University of Michigan. Contribution of J.S. to this paper was supported in part by this grant. C.H. gratefully acknowledges the support of the Michael Smith Foundation for Health Research and the Canada Research Chairs program.
References
- Ayotte B. J. Margrett J. A., & Patrick J. H (2013). Dyadic analysis of self-efficacy and perceived support: The relationship of individual and spousal characteristics with physical activity among middle-aged and young-older adults. Psychology & Aging, 28, 555–563. doi:10.1037/a0032454 [DOI] [PubMed] [Google Scholar]
- Baltes P. B. Lindenberger U., & Staudinger U. M (2006). Life span theory in developmental psychology. In Damon W., Lerner R. M. (Eds.), Handbook of child psychology: Vol. 1. Theoretical models of human development (pp. 569–664). New York, NY: Wiley. [Google Scholar]
- Bandura A. (1997). Self-efficacy: The exercise of control. New York, NY: Freeman. [Google Scholar]
- Bandura A. (2004). Health promotion by social cognitive means. Health Education & Behavior, 31, 143–164. doi:10.1177/1090198104263660 [DOI] [PubMed] [Google Scholar]
- Berg C. A., Upchurch R. (2007). A developmental-contextual model of couples coping with chronic illness across the adult life span. Psychological Bulletin, 133, 920–954. doi:10.1037/0033-2909.133.6.920 [DOI] [PubMed] [Google Scholar]
- Bronfenbrenner U. (1986). Recent advances in research on the ecology of human development. In Silbereisen R. K., Eyferth K., Rudinger G. (Hrsg.), Development as Action in Context. Berlin-Heidelberg, Germany: Springer. [Google Scholar]
- Burkert S. Scholz U. Gralla O. Roigas J., & Knoll N (2011). Dyadic planning of health-behavior change after prostatectomy: A randomized-controlled planning intervention. Social Science & Medicine, 73, 783–792. doi:10.1016/j.socscimed.2011.06.016 [DOI] [PubMed] [Google Scholar]
- Caplan L. J., Schooler C. (2003). The roles of fatalism, self-confidence, and intellectual resources in the disablement process in older adults. Psychology and Aging, 18, 551–561. doi:10.1037/0882-7974.18.3.551 [DOI] [PubMed] [Google Scholar]
- DeLongis A. Capreol M. Holtzman S. O’Brien T., & Campbell J (2004). Social support and social strain among husbands and wives: A multilevel analysis. Journal of Family Psychology, 18, 470–479. doi:10.1037/0893-3200.18.3.470 [DOI] [PubMed] [Google Scholar]
- Dowd J. B., & Todd M (2011). Does self-reported health bias the measurement of health inequalities in U.S. adults? Evidence using anchoring vignettes from the Health and Retirement Study. The Journals of Gerontology: Series B: Psychological Sciences and Social Sciences, 66, 478–489. doi:10.1093/geronb/gbr050 [DOI] [PubMed] [Google Scholar]
- Dunlosky J., Hertzog C. (1998). Aging and deficits in associative memory: What is the role of strategy production?Psychology and Aging, 13, 597–607. doi:10.1037/0882-974.13.4.597 [DOI] [PubMed] [Google Scholar]
- Falba T. A., Sindelar J. L. (2008). Spousal concordance in health behavior change. Health Services Research, 43, 96–116. doi:10.1111/j.1475-6773.2007.00754.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerstorf D. Hoppmann C. A. Kadlec K. M., & McArdle J. J (2009). Memory and depressive symptoms are dynamically linked among married couples: Longitudinal evidence from the AHEAD Study. Developmental Psychology, 45, 1595–1610. doi:10.1037/a0016346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerstorf D. Ram N. Lindenberger U., & Smith J (2013). Age and time-to-death trajectories of change in indicators of cognitive, sensory, physical, health, social, and self-related functions. Developmental Psychology, 49, 1805–1821. doi:10.1037/a0031340 [DOI] [PubMed] [Google Scholar]
- Heckhausen J., & Schulz R (1995). A life-span theory of control. Psychological Review, 102, 284–304. doi:10.1037/0033-295x.102.2.284 [DOI] [PubMed] [Google Scholar]
- Hoppmann C. A., & Gerstorf D (2016). Social interrelations in aging: The sample case of married couples. In Schaie K. W., Willis S. L. (Eds.), Handbook of the Psychology of Aging (8th ed., pp. 263–277). San Diego, CA: Elsevier. doi:10.1016/B978-0-12-411469-2.00014-5 [Google Scholar]
- Idler E. L., & Benyamini Y (1997). Self-rated health and mortality: A review of twenty-seven community studies. Journal of Health and Social Behavior, 38, 21–37. doi:10.2307/2955359 [PubMed] [Google Scholar]
- Infurna F. J., & Gerstorf D (2014). Perceived control relates to better functional health and lower cardio-metabolic risk: The mediating role of physical activity. Health Psychology, 33, 85–94. doi:10.1037/a0030208. [DOI] [PubMed] [Google Scholar]
- Infurna F. J. Ram N., & Gerstorf D (2013). Level and change in perceived control predict 19-year mortality: Findings from the Americans’ Changing Lives Study. Developmental Psychology, 49, 1833–47. doi:10.1037/a0031041 [DOI] [PubMed] [Google Scholar]
- Jackson S. E. Steptoe A., & Wardle J (2015). The influence of partner’s behavior on health behavior change: The English Longitudinal Study of Ageing. JAMA Internal Medicine, 175, 385–392. doi:10.1001/jamainternmed.2014.7554 [DOI] [PubMed] [Google Scholar]
- Katz J. N. Chang L. C. Sangha O. Fossel A.H., & Bates D. W (1996). Can comorbidity be measured by questionnaire rather than medical record review?Medical Care, 34, 73–84. doi:10.1097/00005650-199601000-00006 [DOI] [PubMed] [Google Scholar]
- Khan C. M. Stephens M. A. P. Franks M. M. Rook K. S., & Salem J. K (2013). Influences of spousal support and control on diabetes management through physical activity. Health Psychology, 32, 739–747. doi:10.1037/a0028609 [DOI] [PubMed] [Google Scholar]
- Kenny D. A., Kashy D., Cook W. L. (2006). Dyadic data analysis. New York, NY: Guilford Press. [Google Scholar]
- Kim E. S. Chopik W. J., & Smith (2014). Are people healthier if their partners are more optimistic? The dyadic effect of optimism on health among older adults. Journal of Psychosomatic Research, 76, 447–453. doi:10.1016/j.jpsychores.2014.03.104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lachman M. E. (2006). Perceived control over aging-related declines: Adaptive beliefs and behaviors. Current Directions in Psychological Science, 15, 282–286. doi:0.1111/j.1467-8721.2006.00453.x [Google Scholar]
- Lachman M. E., & Firth K.M (2004). The adaptive value of feeling in control during midlife. In Brim O. G. Ryff C. D., & Kessler R. (Eds.), How healthy are we?: A national study of well-being at midlife (pp. 320–349). Chicago, IL: University of Chicago Press. [Google Scholar]
- Lachman M. E. Neupert S. D., & Agrigoroaei S (2011). The relevance of control beliefs for health and aging. Handbook of the Psychology of Aging, 7, 175–190. doi:10.1016/B978-0-12-380882-0.00011-5 [Google Scholar]
- Lachman M. E., & Weaver S. L (1998). The sense of control as a moderator of social class differences in health and well-being. Journal of Personality and Social Psychology, 74, 763–773. doi:10.1037/0022-3514.74.3.763 [DOI] [PubMed] [Google Scholar]
- Lang F. R. (2001). Regulation of social relationships in later adulthood. Journal of Gerontology: Series B: Psychological Sciences and Social Sciences, 56, 321–326. doi:10.1093/geronb/56.6.P321 [DOI] [PubMed] [Google Scholar]
- Lewis M. A., & Butterfield R. M (2007). Social control in marital relationships: Effect of one’s partner on health behaviors. Journal of Applied Social Psychology, 37, 298–319. doi:10.1111/j.0021-9029.2007.00161.x [Google Scholar]
- Li K.-K. Cardinal B. J., & Acock A. C (2013). Concordance of physical activity trajectories among middle-aged and older married couples: Impact of diseases and functional difficulties. Journals of Gerontology: Series B: Psychological Sciences and Social Sciences, 68, 794–806, doi:10.1093/geronb/gbt068 [DOI] [PubMed] [Google Scholar]
- Little R. J. A., & Rubin D. B (1987). Statistical analysis with missing data. New York, NY: Wiley. [Google Scholar]
- Ludlow L. H., & Klein K (2014). Suppressor variables: The difference between “is” versus “acting as”.Journal of Statistics Education, 22, 1–28. http://www.amstat.org/publications/jse/v22n2/ludlow.pdf. [Google Scholar]
- McAvay G. J. Seeman T. E., & Rodin J (1996). A longitudinal study of change in domain-specific self-efficacy among older adults. Journals of Gerontology: Series B: Psychological Sciences and Social Sciences, 51, 243–253. doi:10.1093/geronb/51B.5.P243 [DOI] [PubMed] [Google Scholar]
- Mirowsky J. (1995). Age and the sense of control. Social Psychology Quarterly, 58, 31–43. doi:10.2307/2787141 [Google Scholar]
- Mudde A. N. Kok G. J., & Strecher V. J (1995). Self-efficacy as a predictor for the cessation of smoking: Methodological issues and implications for smoking cessation programs. Psychology and Health, 10, 353–367. doi:10.1080/08870449508401956 [Google Scholar]
- Ofstedal M. B. Fisher G. G., & Herzog A. R (2005). Documentation of cognitive functioning measures in the Health and Retirement Study (HRS/AHEAD Documentation Report DR-006). Ann Arbor: University of Michigan. [Google Scholar]
- Pearlin L. I., & Schooler C (1978). The structure of coping. Journal of Health and Social Behavior, 19, 2–21. doi:10.2307/2136319 [PubMed] [Google Scholar]
- Roberts B. W. Smith J. Jackson J. J., & Edmonds G (2009). Compensatory conscientiousness and health in older couples. Psychological Science, 20, 553–559. doi:10.1111/j.1467-9280.2009.02339.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodin J. (1986). Aging and health: Effects of the sense of control. Science, 233, 1271–1276. doi:10.1126/science.3749877 [DOI] [PubMed] [Google Scholar]
- Roepke S. K., & Grant I (2011). Toward a more complete understanding of the effects of personal mastery on cardiometabolic health. Health Psychology, 30, 615–32. doi:0.1037/a0023480 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross C. E., & Mirowsky J (2002). Age and the gender gap in the sense of personal control. Social Psychology Quarterly, 65,125–145. doi:10.2307/3090097 [Google Scholar]
- Sargent-Cox K. A. Butterworth P., & Anstey K. J (2014). Role of physical activity in the relationship between mastery and functional health. The Gerontologist, 55, 120–131. doi:10.1093/geront/gnu042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seeman T. E. Unger J. B. McAvay G., & Mendes de Leon C. F (1999). Self-efficacy beliefs and perceived declines in functional ability: MacArthur Studies of Successful Aging. Journal of Gerontology Series B: Psychological Sciences and Social Sciences, 54, 214–222. doi:10.1093/geronb/54B.4.P214 [DOI] [PubMed] [Google Scholar]
- Skinner E. A. (1996). A guide to constructs of control. Journal of Personality and Social Psychology, 71, 549–570. doi:10.1037/0022-3514.71.3.549 [DOI] [PubMed] [Google Scholar]
- Smith J. Fisher G. Ryan L. Clarke P. House J., & Weir D (2013). Psychosocial and lifestyle questionnaire: 2006–2010. Ann Arbor: Institute for Social Research, University of Michigan. [Google Scholar]
- Sonnega A., Faul J. D., Ofstedal M. B., Langa K. M., Phillips J. W., Weir D. R. (2014). Cohort profile: the Health and Retirement Study (HRS). International Journal of Epidemiology, 43, 576–585. doi:10.1093/ije/dyu067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sorkin D. H. Mavandadi S. Rook K. S. Biegler K. A. Kilgore D. Dow E., & Ngo-Metzger Q (2014). Dyadic collaboration in shared health behavior change: The effects of a randomized trial to test a lifestyle intervention for high-risk Latinas. Health Psychology, 33, 566–575. doi:10.1037/hea0000063 [DOI] [PubMed] [Google Scholar]
- Stephens M. A. Rook K. S. Franks M. M. Khan C., & Iida M (2010). Spouses use of social control to improve diabetic patients’ dietary adherence. Families, Systems, & Health, 28, 199–208. doi:10.1037/a0020513 [DOI] [PubMed] [Google Scholar]
- Surtees P. G., Wainwright N. W. J., Luben R., Wareham N. J., Bingham S. A., Khaw K.-T. (2010). Mastery is associated with cardiovascular disease mortality in men and women at apparently low risk. Health Psychology, 29, 412–420. doi:10.1037/a0019432 [DOI] [PubMed] [Google Scholar]
- Watson D. Beer A., & Montez E (2014). The role of active assortment in spousal similarity. Journal of Personality, 82, 116–129. doi:10.1111/jopy.12039 [DOI] [PubMed] [Google Scholar]
- Westmaas J. L. Wild T. C., & Ferrence R (2002). Effects of gender in social control of smoking cessation. Health Psychology, 21, 368–376. doi:10.1037/0278-6133.21.4.368 [DOI] [PubMed] [Google Scholar]
- Wurm S. Tesch-Römer C., & Tomasik M. J (2007). Longitudinal findings on aging-related cognitions, control beliefs, and health in later life. Journals of Gerontology. Series B, Psychological Sciences and Social Sciences, 62, 156–164. doi:10.1093/geronb/62.3.P156 [DOI] [PubMed] [Google Scholar]