Abstract
Objectives.
To estimate and compare disability-free life expectancy (DFLE) and current age patterns of disability onset and recovery from disability between the United States and countries in Latin America and the Caribbean.
Method.
Disability is measured using the activities of daily living scale. Data come from longitudinal surveys of older adult populations in Costa Rica, Mexico, Puerto Rico, and the United States. Age patterns of transitions in and out of disability are modeled with a discrete-time logistic hazard model, and a microsimulation approach is used to estimate DFLE.
Results.
Overall life expectancy for women aged 65 is 20.11 years in Costa Rica, 19.2 years in Mexico, 20.4 years in Puerto Rico, and 20.5 years in the United States. For men, these figures are 19.0 years in Costa Rica, 18.4 years in Mexico, 18.1 years in Puerto Rico, and 18.1 years in the United States. Proportion of remaining life spent free of disability for women at age 65 is comparable between Mexico, Puerto Rico, and the United States, with Costa Rica trailing slightly. Male estimates of DFLE are similar across the four populations.
Discussion.
Though the older adult population of Latin America and the Caribbean lived many years exposed to poor epidemiological and public health conditions, their functional health in later life is comparable with the older adult population of the United States.
Keywords: Aging, Disability, Disability-free life expectancy, Latin America, Microsimulation, Multistate modeling
Population aging in Latin America and the Caribbean (LAC) will not proceed along known paths already followed by more developed countries (Palloni & McEniry 2007). In particular, the pace by which the age composition of countries in LAC will shift is nearly unprecedented. Fertility rates have dropped to near or below replacement level in almost every country in Latin America, and life expectancy (LE) at age 60 has nearly doubled in most countries in LAC since 1950 (Palloni, Pinto-Aguirre, & Pelaez, 2002). A typical country in LAC will reach a population with 15% of individuals older than 60 years in less than half the time that this shift took in the United States (Kinsella & Velkoff, 2001; Palloni et al., 2002). The care of this aging population is one of the largest challenges faced by the countries in LAC. However, rigorous research on how these additional years are spent is lacking. This population is growing faster and living longer than ever before, but what portion of this additional life is spent with disability? How do the countrywide levels of disability and rates of chronic noncommunicable diseases (NCDs) compare across the region, and to more developed contexts such as the United States? The answers to these questions will affect social welfare and have substantial repercussions for national health systems, retirement and disability patterns, and the demand for long-term care for the aging in both institutional and family settings (Cotlear, 2011).
The primary aim of this article is to estimate and compare disability-free life expectancy (DFLE) between the United States and countries in LAC and to gain insight into current age patterns of disability onset and recovery from disability in these populations. I center on understanding the lived experience with disability among the aging population as measured by the activities of daily living (ADL) scale. Specifically, I estimate the rates of transitions between life without disability, disabled life, and death in these populations, and use these parameters to estimate the DFLE of individuals in the Costa Rica, Mexico, Puerto Rico, and the United States. Together, these measures characterize processes of disability in the growing older adult population of LAC and can provide important insights into how current disability conditions in these populations may affect future demands from health care systems, pension programs, and social services.
Background
The four contexts compared in this study (three countries—the United States, Costa Rica, and Mexico—and one territory, Puerto Rico) comprise a range of differing economic and demographic conditions, health care systems, and pension systems. Each of the four contexts studied here have similar LE at age 60, though levels of Gross Domestic Product (GDP) per capita, human development index, and health expenditure per capita vary dramatically (Table 1).
Table 1.
Economic and Health Conditions
| Costa Rica | Mexico | Puerto Rico | United States | |
|---|---|---|---|---|
| GDP per capita 2011 (current U.S. $) | 9,386 | 9,749 | 27,678 | 51,749 |
| Health expenditure per capita, 2011 (current U.S. $) | 943 | 620 | — | 8,608 |
| LE at birth, men | 77 | 74 | 74 | 76 |
| LE at birth, women | 81 | 79 | 82 | 81 |
| LE at age 60, men | 21 | 20 | 20 | 20 |
| LE at age 60, women | 24 | 22 | 25 | 24 |
| Total fertility rate 2011 | 1.8 | 2.2 | 1.7 | 1.9 |
| Population, 2011 | 4,737,680 | 119,361,233 | 3,694,093 | 311,587,816 |
| Human Development Index | 62 | 61 | 52 | 3 |
Note. Sources: World Bank World Development Indicators 2013, UN Population Division World Population Prospects 2006 and 2012, UN Development Programme 2013 Human Development Report. LE = life expectancy.
Mexico
The population aged 65+ in Mexico is one of the most rapidly growing in the world. Though this population currently comprises 9.4% of the total population, it is projected to more than double in the next 25 years (U.S. Census Bureau, 2014). LE currently stands at 79 years for women and 74 years for men (Cotlear, 2011). Mexico has closely followed the classical epidemiological transition (Omran, 1977), with a marked decline in deaths from infectious disease since the 1980s and an increase in deaths from chronic and degenerative diseases—from 58% of deaths in 1990 to 75% of deaths in 2005 (Pan-American Health Organization, 2007; Stevens et al., 2008). Mexico’s total fertility rate is slightly above replacement level, but it has dropped rapidly since the mid 1980s (The World Bank, 2014). Although health conditions have improved, availability of medical care lags behind many other upper-middle income countries. Mexico has some of the lowest rates of availability of health care resources in LAC, particularly in hospital beds and physicians per thousand people (The World Bank, 2014). Many older adults did not participate in the formal labor market in their early life, and only about half are covered by Mexican Institute for Social Security (Instituto Mexicano del Seguro Social [IMSS]) health care services (Aguila et al., 2011). This population either forgoes health insurance or relies on public health programs such as Popular Health Insurance (Seguro Popular de Salud [SPS]), where they may incur substantial out-of-pocket expenditures for health care (Aguila et al., 2011).
Costa Rica
Costa Rica, located on the Central American isthmus, is often cited as a model for other middle-income countries. Though it differs little from most other countries in LAC in terms of GDP per capita, it has achieved a level of LE, access to public health services and sanitation, environmental protection, and social security coverage among the highest in the Americas (Rosero-Bixby, 2008). Costa Rica underwent a very rapid demographic transition—LE rose from around the mid 40s in the 1930s to around 70 by 1970, and infant mortality dropped continuously during these years before rapidly declining in the 1970s (Rosero-Bixby, 1990). LE at birth and at age 60 are comparable or even higher than values for the United States. The population is still rather young—about 7% of Costa Ricans currently older than 65 years, though this will rapidly grow to more than 22% by 2040 (U.S. Census Bureau, 2014). Costa Rica has attained these impressive health and development metrics with a surprisingly low level of health expenditure per capita—only $943 per year in 2011, about 11% of the U.S.’ spending (The World Bank, 2014). The Costa Rican Department of Social Insurance (Caja Costarricense de Seguro Social [CCSS]) was established in 1941, and universalization of health care coverage in 1973 consolidated the control of medical facilities to the CCSS. The Costa Rican health system is characterized by a focus on primary care and preventive medicine, a decentralization of health services, and emphasis on training and capacity-building in rural clinics (Eriksson, Mohs, & Eriksson, 1990). The public health insurance system covers about 88% of the population (Saenz, Bermudez, & Acosta, 2010), and the government provides no-cost insurance for the destitute population (Rosero-Bixby, 2004).
Puerto Rico
Puerto Rico is a commonwealth of the United States, located in the Caribbean. The population is already fairly old compared with other LAC contexts due to both demographic aging and high rates of out-migration to the U.S. mainland among the younger population, but the older population is projected to continue growing in coming years. More than 16% of the population is currently older than 65 years, and by 2040, this population is estimated to be about 27.4% of the island’s total population (U.S. Census Bureau, 2014). Rates of GDP per capita sit below the United States but substantially above Costa Rica and Mexico. As U.S. citizens, Puerto Ricans pay Medicare insurance and thus are covered by the Medicare insurance system after the age of 65. Though health insurance coverage is high, preventative care is often poor—only 14% of the diabetic population has received a deep eye test, only 16% are monitored for nephropathy, and 82% have poor control of their blood sugar. Only around half of the female population at risk had received a mammography or Pap smear (Colón, 2005).
United States
The United States is one of the highest income countries in the world, with a fully modern health care system and a completed epidemiological transition. About 14% of the population is currently aged 65 and older, a figure which will rise to about 21% by 2040. GDP per capita and health expenditure per capita rank among the highest in the world and the United States also ranks high on the number of hospital beds and doctors per 1,000 individuals (The World Bank, 2014). The United States had essentially completed its epidemiological transition by the 1920s (Omran, 1977), meaning that the vast majority of the current 65+ population was not exposed to high rates of communicable disease in early life. At the age of 65, individuals are eligible for Medicare, a federal health insurance program, and are also eligible for pension payments from Social Security. Even though access to care is high, the United States still has persistently lower LE outcomes than many other similarly wealthy nations (Ho & Preston, 2010).
Differences in adult health across populations are driven primarily by two complex and interrelated sources of variation. The first of these are childhood or early-life sources, including fetal environment, childhood nutritional and epidemiological environment, and rates of infant and child mortality during early life. Cohorts reaching the ages 65+ in Latin America were exposed to a vastly different set of early-life conditions when compared with the 65+ population in the United States—these cohorts experienced much higher rates of disease and episodic malnutrition both in utero and in early life, both of which are associated with increased risks of NCD, adult mortality, and late-life disability (Ben-Shlomo & Kuh, 2002; Huang, Soldo, & Elo, 2011, McEniry, 2013). A number of LAC-focused studies (Monteverde, Noronha, & Palloni, 2009; Palloni, McEniry, Wong, & Pelaez, 2006) suggest that the higher disease burden and episodic malnutrition experienced by LAC’s aging population during early life may contribute to successive cohorts at higher risk of disability and chronic disease. However, there is also the possibility that differential selection effects may lead to fairly healthy cohorts of 65+ individuals in LAC. The current cohorts of older adults in LAC may be a selective group—that is, they could represent only the “hardiest” survivors of cohorts exposed to high child and infant mortality (Gerst-Emerson, Wong, Michaels-Obregon, & Palloni, 2015), and may thus have a lower burden of disabling conditions.
The second set of factors driving cross-national differences in adult disability is adult or late-life sources such as exposure to advanced medical technology and care for NCDs, declining physical activity, and exposure to lifestyle behaviors such as smoking and consumption of high-calorie convenience foods. As described earlier, the older population in most of LAC has spent substantially less time exposed to these factors than the older population in the United States. How this exposure affects the health of LAC’s older adult population is somewhat unclear—recent access to modern medical technology should result in improving health outcomes, but access to high-quality care is not as widespread in LAC as in the United States. Economic development and urbanization may also lead to an increase in unhealthy behaviors such as a sedentary lifestyle and obesity in LAC, but older cohorts in these countries have had a substantially shorter exposure to these conditions than older cohorts in the United States.
Although a great deal of study of DFLE and the aging process has been conducted in the United States and other developed contexts, research on aging and disabilities is lacking in lower and middle-income countries. This gap in the literature is due in part to the unavailability of high-quality data, and in particular longitudinal data, on aging populations in much of the developing world (Ebrahim et al., 2013). Existing research into health expectancies (HEs) in LAC has largely relied on cross-sectional data or used the limited longitudinal follow-up data collected by some countries following the cross-sectional Study of Health, Well-Being, and Aging in Latin America and the Caribbean (SABE), where the long time periods between waves of data collection (5+ years) may result in substantially biased estimates when used to estimate current status data (Gill, Allore, Hardy, Holford, & Han, 2005; Wolf & Gill, 2009). Even with these data constraints, a small but growing body of literature is emerging on aging and disability in LAC. Research from Mexico shows that individuals with diabetes experience a much diminished LE (10 years of reduced LE at age 50) and a high burden of self-care limitations (Andrade, 2010). Recent work has also found that Hispanic migrants in the United States experience a protracted period of disability in older age, even as they expect to live more total years than White or non-Hispanic Black populations (Hayward, Hummer, Chiu, Gonzalez-Gonzalez, & Wong, 2014). In contrast, a recent article by Gerst-Emerson and colleagues (2015) found that Mexican adults aged 50+ experienced fewer transitions into disability compared with non-Hispanic Whites in the United States and were more likely to recover from disability.
I focus on DFLE as an easily interpretable metric for comparing population-level disability in a cross-national context. DFLE distinguishes between years that are free of limitations on activities and years with activity limitations and provides a more nuanced view of population-level disability than simple LE. DFLE combines mortality and morbidity into a single measure, providing a convenient and easily interpretable metric for measuring population-level health (Minicuci et al., 2004).
Although informative comparisons of health care systems, economic development, and epidemiological histories across these four contexts are possible at the macro level, little existing research has compared processes of disability in the aging population between LAC and the United States. This article compares the DFLE of the older adult population between the very different contexts of the United States and the three Latin American countries under study—Mexico, Puerto Rico, and Costa Rica. The primary goal of this research is to understand the current outcomes of the complex interplay between early-life and late-life influences on health and to gain insight into present and possible future trends in disability in these populations.
Method
Data
Data from my analysis come from four sources: The Costa Rican Longevity and Healthy Aging Study (CRELES), collected in 2005, 2007, and 2009 (Rosero-Bixby, Fernández, & Dow, 2013); the Mexican Health and Aging Survey (MHAS) collected in 2001 and 2003 (Mexican Health and Aging Study, 2001 & 2003); the Puerto Rican Elderly: Health Conditions (PREHCO) survey collected in 2002–2003 and 2006–2007 (Palloni, Luisa Davila, & Sanchez-Ayendez, 2013); and the United States’ Health and Retirement Survey (HRS) from 2004, 2006, 2008, and 2010 (RAND Center for the Study of Aging, 2014). Data instruments and collection procedures from CRELES and MHAS are largely based on HRS methodologies (McEniry, Moen, & McDermott, 2013), and PREHCO asks a large suite of highly comparable questions on ADL activities, demographics, chronic conditions, and interactions with the health care system. In each country, my sample consists of all available noninstitutionalized primary respondents aged 65 and older with data on ADL limitation.
I conceptualize disability within the framework of the disablement process (Kasper & Freedman, 2014; Verbrugge & Jette, 1994), wherein disability is defined as a gap between an individual’s capacities (physical, sensory, or cognitive) and the demands of a given activity in that individual’s particular environment. As such, disability is not a purely health-based measure, but is influenced by environment and accommodation. I investigate patterns of self-reported disability by using the ADL scale to create two distinct states of physical health: active individuals with no reported limitations on ADL activities and ADL disabled individuals with one or more limitations on ADL activities. I parameterize ADL disability as difficulty on any of the following five activities: bathing, eating, getting in/out of bed, toileting, and walking across a room. Where necessary, proxy responses on ADL limitation are used for data from HRS, CRELES, and MHAS. Direct questions on ADLs were not asked of proxy respondents in PREHCO—proxy respondents were asked whether the target respondent was capable of staying home alone without problems, a very similar measure of ability to self-care. Individuals judged by the proxy respondent as not capable of staying home alone without problems are counted as ADL disabled.
Analytic Strategy
Initially, I compare rates of disability, chronic conditions, and sociodemographic variables across these four contexts to gain a baseline understanding of health conditions. I then use a multistate life table (MSLT) to translate the longitudinal data from each country into estimates of DFLE and LE with ADL limitations. This estimation method is based on an adapted version of the Stochastic Population Analysis for Complex Events program (Cai et al., 2010; Payne, Mkandawire, & Kohler, 2013). This method relies on weighted data from nationally representative sample surveys to estimate MSLT functions such as total LE, DFLE, and disabled LE at the population level. Specifically, to calculate MSLT functions such as healthy and ADL-limited HEs, I use microsimulation to create synthetic cohorts of 100,000 65-, 75-, and 85-year-old individuals with the same initial gender and ADL limitation distributions as the study populations. I then “age” these individuals forward year by year using age- and gender-specific mortality rates and probabilities of transitioning in and out of disability estimated from the data. This process is then repeated at each age until death. The resulting synthetic cohort is analyzed to estimate DFLE and other life course health indicators. The process is essentially the microsimulation equivalent of projecting the initial synthetic cohort population P, disaggregated by age, sex, and disability status, using Pt = Q · Pi, where Q is a projection matrix Q containing all age- and gender-specific disability transition rates and mortality rates (Schoen, 1988).
Sample attrition varied somewhat between the four data sources. For the eligible sample of respondents, attrition was 13.3% between the two waves of PREHCO, 4.3% between the two waves of MHAS, about 8% between each wave of CRELES, and about 4% between each wave of HRS. Prior to the microsimulation described earlier, I conducted multiple imputation of missing data by chained equations (van Buuren, Boshuizen, & Knook, 1999). The multiple imputation models included the full set of ADL questions, age, and all demographic and health information from Table 2. For each sample, 10 data sets with imputed ADL disability and mortality outcomes for attrittors were generated. In the microsimulation approach, DFLE estimates are not a deterministic function of the transition probabilities, and instead, these result from the interplay between disability status, gender, and age as individuals move year by year through the simulation. Thus, confidence intervals (CIs) from the transition calculations are not directly applicable to the DFLE estimates. CIs for DFLE, which reflect both the uncertainty of the estimated parameters and the uncertainty from the microsimulation, were created by re-estimating the analysis sequence (estimating state-dependent transition probabilities from each multiply imputed data set and applying them to a representative 100,000-person cohort using microsimulation) using 200 bootstrap resamples. The results from these resamples are then aggregated across the 10 multiply imputed data sets, resulting in 2,000 parameter estimates. The final point estimates presented are the median of the distribution of these 2,000 bootstrapped parameters, with CIs defined as the central 95% of the resulting distribution. All analyses are completed using sample weights normed to the respective national population.
Table 2.
Baseline Sample Characteristics
| Costa Rica—CRELES Wave 1 (2005) | Mexico—MHAS Wave 1 (2001) | Puerto Rico—PREHCO Wave 1 (2002) | United States—HRS Wave 7 (2004) | |||||
|---|---|---|---|---|---|---|---|---|
| Prop. | 95% CI | Prop. | 95% CI | Prop. | 95% CI | Prop. | 95% CI | |
| Age (years) | ||||||||
| 65–74 | 0.60 | (0.58–0.62) | 0.59 | (0.56–0.62) | 0.60 | (0.58–0.63) | 0.52 | (0.51–0.54) |
| 75–84 | 0.31 | (0.29–0.33) | 0.29 | (0.27–0.32) | 0.31 | (0.28–0.33) | 0.37 | (0.36–0.38) |
| 85+ | 0.09 | (0.09–0.1) | 0.12 | (0.09–0.15) | 0.09 | (0.08–0.1) | 0.11 | (0.1–0.11) |
| Sex | ||||||||
| Female | 0.53 | (0.51–0.56) | 0.54 | (0.51–0.57) | 0.57 | (0.54–0.59) | 0.57 | (0.56–0.58) |
| Marital status | ||||||||
| Married/cohabiting | 0.55 | (0.53–0.57) | 0.39 | (0.36–0.42) | 0.47 | (0.44–0.49) | 0.57 | (0.56–0.58) |
| Visited doctor in past 12 months | 0.91 | (0.89–0.92) | 0.64 | (0.61–0.67) | 0.88 | (0.87–0.9) | — | |
| Visited doctor in past 24 months | — | — | — | — | 0.95 | (0.95–0.96) | ||
| Ever a smokera | 0.42 | (0.4–0.44) | 0.45 | (0.42–0.48) | 0.34 | (0.31–0.36) | 0.57 | (0.56–0.58) |
| Disability | ||||||||
| Difficulty on 1+ ADLs | 0.16 | (0.14–0.17) | 0.16 | (0.13–0.18) | 0.14 | (0.12–0.16) | 0.17 | (0.16–0.18) |
| NCDs | ||||||||
| Hypertension | 0.50 | (0.48–0.52) | 0.42 | (0.39–0.45) | 0.59 | (0.57–0.62) | 0.59 | (0.58–0.6) |
| Stroke | 0.05 | (0.04–0.06) | 0.04 | (0.03–0.05) | 0.06 | (0.04–0.07) | 0.10 | (0.1–0.11) |
| Cancer | 0.07 | (0.05–0.08) | 0.02 | (0.01–0.02) | 0.07 | (0.05–0.08) | 0.18 | (0.17–0.19) |
| Heart attack/MIb | 0.05 | (0.04–0.06) | 0.04 | (0.03–0.05) | 0.11 | (0.1–0.13) | 0.30 | (0.3–0.31) |
| Diabetes | 0.21 | (0.19–0.22) | 0.17 | (0.14–0.19) | 0.28 | (0.25–0.3) | 0.19 | (0.18–0.19) |
| Arthritis | 0.16 | (0.14–0.18) | 0.26 | (0.24–0.29) | 0.50 | (0.47–0.52) | 0.65 | (0.64–0.66) |
| BMI | ||||||||
| <20 | 0.07 | (0.05–0.08) | 0.08 | (0.06–0.1) | 0.07 | (0.06–0.08) | 0.07 | (0.07–0.08) |
| 20–30 | 0.69 | (0.67–0.72) | 0.76 | (0.73–0.79) | 0.68 | (0.65–0.7) | 0.71 | (0.7–0.72) |
| 30+ | 0.24 | (0.22–0.26) | 0.15 | (0.13–0.18) | 0.25 | (0.23–0.28) | 0.21 | (0.2–0.22) |
| Education | ||||||||
| 0–6 | 0.82 | (0.8–0.84) | 0.89 | (0.86–0.91) | 0.47 | (0.44–0.5) | 0.05 | (0.05–0.06) |
| 7–11 | 0.08 | (0.07–0.09) | 0.08 | (0.06–0.1) | 0.21 | (0.19–0.23) | 0.22 | (0.21–0.23) |
| 12+ | 0.10 | (0.08–0.11) | 0.04 | (0.03–0.05) | 0.32 | (0.3–0.34) | 0.73 | (0.72–0.73) |
| Income | ||||||||
| Public pensionc | 0.63 | (0.61–0.65) | 0.14 | (0.12–0.17) | 0.98 | (0.98–0.99) | 0.99 | (0.99–0.99) |
| Health insurance | ||||||||
| Public | 0.96 | (0.95–0.97) | 0.50 | (0.47–0.53) | 0.84 | (0.82–0.86) | 0.98 | (0.97–0.98) |
| Private | 0.02 | (0.01–0.03) | 0.03 | (0.02–0.04) | 0.14 | (0.12–0.16) | 0.01 | (0.01–0.02) |
| None | 0.02 | (0.02–0.03) | 0.47 | (0.44–0.5) | 0.02 | (0.01–0.02) | 0.01 | (0.01–0.01) |
| Total sample size | 2,480 | 3,530 | 2,880 | 10,492 | ||||
| Proportion proxy respondents | 0.16 | 0.12 | 0.09 | 0.08 | ||||
Notes. All presented results use national-level sample weights.
aIncludes all individuals who report having smoked more than 100 cigarettes in their lifetime.
bU.S. sample (HRS) also includes wider range of heart conditions; this figure is not directly comparable across samples.
cIn Mexico, this category includes individuals receiving pensions from IMSS, ISSSTE, other public pensions, or U.S. Social Security. In Puerto Rico and the United States, it is comprised of those receiving Social Security. In Costa Rica, it includes all individuals receiving Social Security or government pensions.
ADL = activities of daily living; BMI = body mass index; CI = confidence interval; CRELES = Costa Rican Longevity and Healthy Aging Study; HRS = Health and Retirement Survey; MI = myocardial infarction; MHAS = Mexican Health and Aging Survey; NCD = noncommunicable disease; PREHCO = Puerto Rican Elderly: Health Conditions; prop. = proportion.
To estimate the conditional probabilities of experiencing a transition between the three modeled states (active, ADL disabled, and deceased), I generate data sets in person-year format, assuming that transitions between disability states occur midway between observations. I then model the annual transition probabilities as a function of age and gender, using a multinomial logistic discrete-time hazard model of the form
| (1) |
where pij (Age, t) is the transition probability from current state i (with i = active or ADL disabled) to state j (with j = active, ADL disabled, or deceased) over the interval from time t − 1 to t, β0ij is the intercept, β1ij is the coefficient for Age, β2ij is the coefficient for Age2, and β3ij is the coefficient for Female. An analysis model including an Age * Female interaction was also tested, but the coefficients were not significant at α = .05 and the DFLE and transition probability results were minimally changed; it was thus removed in favor of the simpler model. Transition probability estimates were obtained using PROC SURVEYLOGISTIC in SAS v9.4, accounting for survey weights and sample design.
Results
Sample Characteristics
Table 2 presents the baseline sociodemographic and health characteristics of the four samples. All presented results use national-level sample weights to represent the aging population of the countries under study. Basic sample demographics are somewhat different between the four samples—the United States 65+ population skews older than in Mexico, Puerto Rico, or Costa Rica. Individuals in the United States, Puerto Rico, and Costa Rica were substantially more likely to have visited a doctor in the past year (or, in the U.S. case, past 2 years) than individuals in Mexico at baseline. Almost 60% of the U.S. sample reported having smoked over the course of their lifetime, compared with 45% of Mexican adults older than 65 years, 42% of Costa Rican adults older than 65 years, and 34% of Puerto Rican adults older than 65 years. Rates of doctor-diagnosed NCDs vary somewhat between countries. Hypertension is common across the four samples, though somewhat higher in the United States and Puerto Rico. Diagnosis of cancer, stroke, and arthritis is also more common in the United States, though this could be due to variation in medical practices or frequency of doctor’s visits (particularly in the case of Mexico). Almost 30% of Puerto Rican adults older than 65 years have been diagnosed with diabetes, compared with about 20% for the other countries. In the case of heart attack, the U.S. sample categorized multiple heart conditions together, which likely leads to the substantially higher reported rate.
Older adults in Mexico and Costa Rica, and to a lesser extent those in Puerto Rico, had substantially fewer years of formal education than individuals in the United States. Older adults in the United States and Puerto Rico almost universally receive Social Security, whereas only 63% of Costa Ricans and 14% of Mexicans received a pension from the government at the first wave of data collection. Likewise, most individuals in the United States and Puerto Rico are eligible for health insurance through Medicare, and almost all older individuals in Costa Rica receive health care from the CCSS. In Mexico, a much smaller proportion of individuals receive publically provided health insurance, and more than 47% of individuals older than 65 years in the 2001 MHAS sample reported having no insurance. The proportion of individuals requiring the assistance of a proxy varied somewhat across the four samples, from a high of 16% in CRELES to a low of 8% in HRS.
Multistate Transition Probabilities
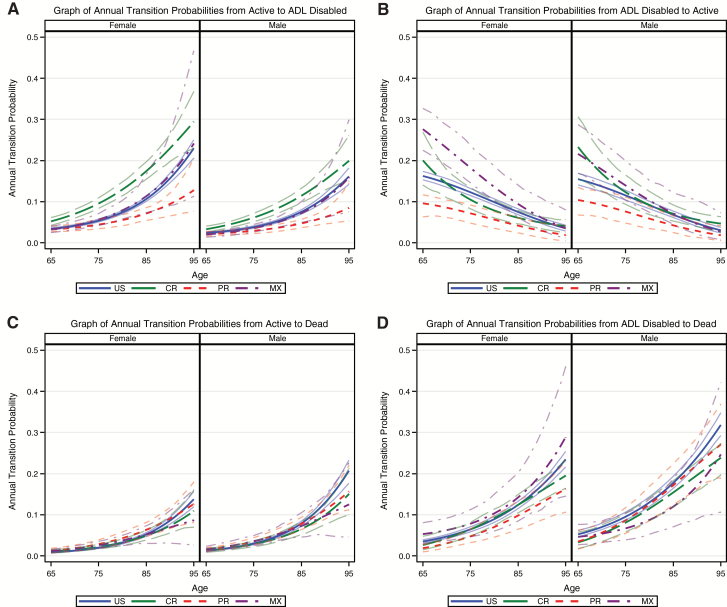
To gain insight into the dynamics of old-age disability in these four populations, I model the underlying age- and gender-specific annual transition probabilities between disability states. Figure 1 illustrates the annual transition probabilities between active life, ADL disabled life, and death by sex, along with the 95% CIs (represented as the thin lines) based on bootstrap resampling. At older ages, particularly above age 85, CIs around the point estimates grow quite large for Mexico, Puerto Rico, and Costa Rica, primarily as a result of limited sample sizes at these advanced ages. Transition probabilities from active life to ADL disability (Panel A) rise sharply with age, though there are substantial differences in the patterns across populations. Annual probability of disability onset doubles from age 65 to age 85 among both men and women in the United States, Costa Rica, and Mexico, but it increases only by 1.5 times in Puerto Rican men and women. This decreased rate may result from differences between data sources—the gap between waves of data collection in PREHCO was 3–4 years rather than 2 years (as in HRS, CRELES, and MHAS), which likely results in fewer observed transitions. This may result in somewhat downwardly biased estimates of DFLE from the PREHCO data compared with the other populations. In addition, Supplementary Table 1 displays the regression coefficients estimated from Equation 1 for each country and transition. As would be expected, given the variation observed in Figure 1, there is some significant variation in coefficients across countries, though directions of the coefficients for most transitions are similar across countries.
Figure 1.
Annual transition probabilities between disability states in CRELES (CR), MHAS (MX), PREHCO (PR), and HRS (US) data. Panel (A) displays the annual transition probabilities from active life to activities of daily living (ADL) disability, panel (B) displays transition probabilities from ADL disability to active life, panel (C) displays transition probabilities from active life to death, and panel (D) displays transition probabilities from ADL disability to death. CRELES = Costa Rican Longevity and Healthy Aging Study; HRS = Health and Retirement Survey; MHAS = Mexican Health and Aging Survey; PREHCO = Puerto Rican Elderly: Health Conditions.
Annual probabilities of becoming ADL disabled are higher for women, following a widely established pattern in contexts where disability transitions have been studied (Crimmins, Kim, & Sole-Auro, 2011; Oksuzyan et al., 2010). Rates of recovery from ADL disability (Panel B) drop substantially with increasing age. By about 85 years of age, disabled individuals are more likely to die within the next year than to recover to disability-free life. Some variation between countries exists in these transition rates—probabilities of recovery are high in Mexico and low in Puerto Rico, but with increasing age these cross-national differences diminish.
Mortality rates from active life (Panel C) and ADL disabled life (Panel D) provide evidence that disability has a strong association with mortality. Throughout later life, individuals with ADL disability have a higher mortality rate, and mortality rate estimates from disabled life are largely quite similar across countries. Point estimates for mortality from active status are higher for men than for women at almost ages, though this difference is often within the CI.
Life and DFLEs
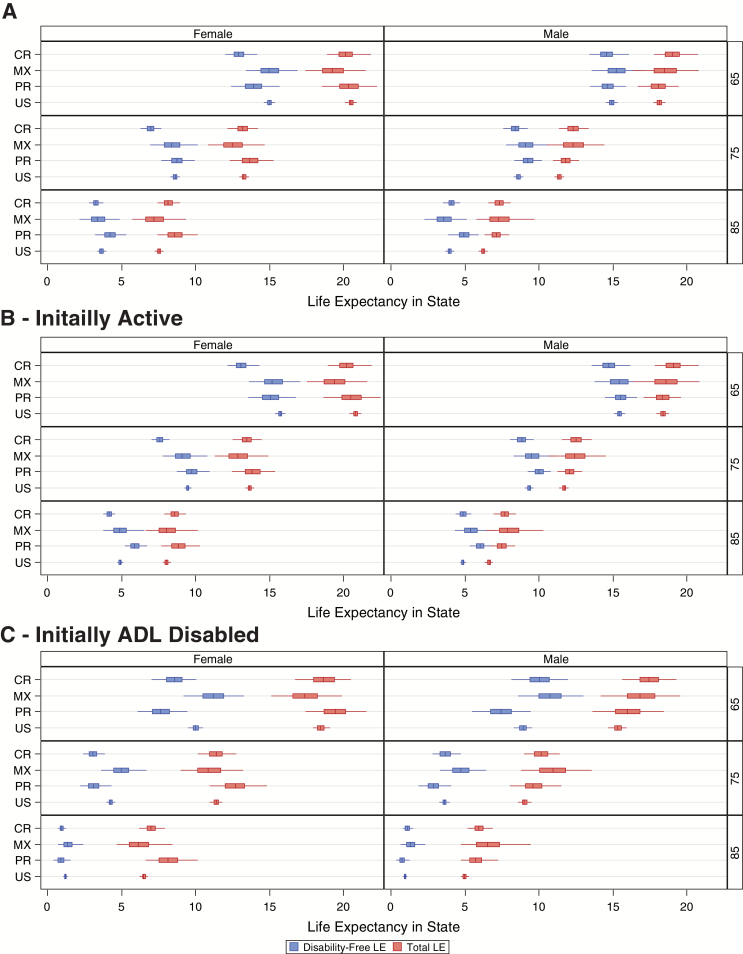
Moving from the transition probabilities in Figure 1 to the corresponding life and DFLEs, Figure 2 translates the age- and sex-specific annual probabilities of transition between disability states into years lived with ADL limitation. In Figure 2, lines represent the central 95% of the distribution of bootstrapped outcomes, and the boxes span the first to third quartile of the outcome distribution with a vertical line at the median. In addition to revealing remaining total LE for the aging population, the microsimulation-based MSLT approach estimates the duration of remaining life expected to be spent disability free with CIs determined through bootstrap replication. Supplementary Table 2 provides the estimated life and HEs across these four populations, and Supplementary Table 3 provides estimated life and DFLEs using listwise deletion rather than multiple imputation to account for missing data. Supplementary Table 4 tests an alternative parameterization of disability using difficulty on 2+ ADLs as a threshold; cross-national differences at ages 65 and 75 are again minimal in this parameterization, though due to small sample sizes, DFLE for those aged 85 could not be estimated in all countries.
Figure 2.
Estimated total and disability-free life expectancy. This figure shows a comparison between the years an average individual will spend in remaining disability free and total life at ages 65, 75, and 85 by country. Lines represent the central 95% of the distribution of bootstrapped outcomes, and boxes span the first to third quartile of the outcome distribution with a vertical line at the median. Panel (A) presents the disability-free life expectancy (DFLE) and life expectancies of all individuals at ages 65, 75, and 85. Panels (B) and (C) present the DFLE and life expectancies of individuals who were initially active (B) and activities of daily living disabled (C) at ages 65, 75, and 85.
Figure 2A displays the total and DFLE estimates for the full sample, regardless of initial disability status. Remaining total LE at age 65 is about 20 years for women in each of the four countries, making the total LE about 85 years (these figures are about 18.5 years and 83.5 years for men). However, there is some country-to-country variation in expected longevity. Mexican womens’ LE lags behind those of the United States by about 1 year at age 65. Men have overall similar LEs across populations, with a few minor variations. A comparison of LEs from multiple life tables (Supplementary Figure 1) shows that the MSLT-based LE estimates from microdata may contain some upward bias in LE compared with estimates from national vital statistics, though these differences are generally not substantial and within the 95% CI.
Moving to DFLEs, women aged 65 and 75 in Costa Rica expect to live about 1.5 fewer disability-free years than their counterparts in the United States. A 65-year-old women in Puerto Rico expects to live about 1 fewer year with ADL disability compared with her counterpart in the United States, though these differences subside at later ages. For men, there are no substantial differences in DFLE across the four populations, though Costa Rican men expect to live about 1 year longer than U.S. men at age 65. Proportion of remaining life spent free of ADL limitations is fairly stable across the four populations, a surprising finding given the variation in income, health infrastructure and expenditure, and health indicators between these four contexts. Women in Costa Rica expect to live slightly less of their remaining life disability free at ages 65, 75, and 85 when compared with women in the United States, but few other differences approach significance. Overall, men expect to spend about 10% more of their remaining life free of ADL disability at all ages when compared with women.
Though the unconditional life and DFLEs in Figure 2A provide an informative overview of the later-life disability conditions in each population, delving deeper into the LEs conditional on entry state (i.e., conditional on being healthy or ADL limited at age 65, 75, or 85) provides a more detailed picture of late-life disability patterns. Conditional DFLE estimates for those initially healthy (Figure 2B) and initially ADL limited (Figure 2C) provide strong evidence that initial disability status is strongly related to total LE and DFLE in later life. A healthy women at ages 65, 75, and 85 will expect to live, on average, about 2 additional years compared with 65-, 75-, and 85-year-old women with ADL limitations and will spend a substantially smaller proportion of her remaining life with no ADL limitations. The gap between initially healthy and initially limited individuals is largest in Puerto Rico and Costa Rica, resulting from the low transition rates from ADL limitation to healthy life (observed in Figure 1). These findings are of similar magnitude for men—men with no ADL limitations at ages 65, 75, and 85 live substantially longer lives than men with ADL limitations at these ages. Individuals with ADL limitations at age 85 expect to live almost their entire remaining life with ADL limitations.
Supplementary Figure 2 provides the smoothed age-specific proportions in ADL-limited life in each population, as well as the proportions from the microsimulation-generated synthetic cohorts based on each population. The proportion disabled at each age in each sample (solid lines) is quite similar across countries, though the proportion disabled appears somewhat lower at older ages in Puerto Rico. The simulated data match closely with observed proportions in each sample, suggesting that the proportion disabled by age in these populations has been fairly stable by cohort and period in recent decades.
Discussion
The purpose of this article is to estimate and compare current levels of DFLE between the United States and countries in LAC and to gain insight into future disability trends in these populations. I use a microsimulation-based MSLT to analyze both the levels of disability by age and the dynamics of disability in later life. This investigation provides a wealth of information about the life course experience with disability in these aging populations, utilizing high-quality longitudinal data to observe and model patterns of transitions between disability-free and ADL disabled life. I compare the processes of functional limitation in three LAC populations with the United States, estimating the prevalence of functional limitations and the transition rates between different disability states. Rates of transition into disability statuses differ substantially across the life course—rates of recovery from ADL disability decline very rapidly with age, and across populations, individuals aged 85 and older are more likely to die within the next year than to recover to disability-free life. Women in Costa Rica, Puerto Rico, Mexico, and the United States expect to live about 20 additional years at age 65, and men expect to live about 18 additional years. Though the total LE for 65-year-old men and women in Costa Rica, Puerto Rico, and the United States is similar, women in Costa Rica expect to spend slightly more of their remaining life with ADL disability. Across the four populations, women, on average, will live a higher proportion of their remaining life subject to disability compared with men.
The 65+ populations in Costa Rica, Mexico, and Puerto Rico were exposed to a vastly different set of epidemiological, nutritional, economic, and public health conditions than the 65+ population in the United States, but these four populations are at near parity in terms of DFLE. This is a surprising finding and one that is not easy to interpret. Late-life health results from a complex interplay between early- and late-life sources, and there are likely counterbalancing effects occurring in these populations that lead to these overall similarities. In Costa Rica, Mexico, and Puerto Rico, high early-life mortality selection of weaker individuals has likely lead to smaller, but healthier, cohorts of older individuals. In the United States, the proportion of individuals surviving to older ages is likely much higher, but these individuals have experienced higher rates of smoking and other poor health behaviors.
Though at present these forces are leading to similar levels of DFLE across these populations, the future trends of disability in LAC are still very much in question. Successive generations entering into later life have spent less and less time subject to poor epidemiological conditions in childhood and young adulthood, suggesting that disability conditions among LAC’s older adult population may indeed improve in coming decades. However, in the thinking of Palloni and Souza (2013), the rapid technological shifts in health care and public health programs in LAC in the 1930s–1950s led to reduced mortality selection and higher survival rates of individuals who were exposed to a heavy burden of disease and nutritional deficits in early life. In this study, the youngest individuals from MHAS were born in 1936, in CRELES this figure is 1940, and in PREHCO this figure is 1937. Thus, only the very youngest individuals in my analyses were exposed to these technological advances in early life. Data from continuing rounds of MHAS and CRELES will be key to measuring and understanding whether a stagnation or reversal in LE and DFLE is happening in LAC.
Though the similarities in overall DFLE are remarkable, patterns of transitions between disability states vary fairly substantially across countries. At present, these transition rate differences appear to be balancing each other leading to overall similarities in DFLE. However, late-life health trends in successive cohorts may shift in the coming years (due to the cohort differences in mortality selection and health behaviors discussed earlier), which could lead to changes in transition rate patterns and a divergence in DFLE. Further research into the factors influencing country-specific transition rates is needed to gain insight into the future trends in DFLE in LAC.
In evaluating the results from this MSLT estimation, several limitations need to be considered. Individuals who experience a health transition between waves of data collection in the four surveys used are assumed to experience only a single transition during the period between surveys, which likely misses shorter-term transitions between health statuses. The MSLT modeling approach is limited in incorporating time-varying covariates, thus my analyses could not simultaneously model ADL disability and the underlying health conditions, which may have resulted in these limitations. In common with other life table based measures, health expectancy estimates assume stationary transition rates over time, and thus will not match the lived experience of any single cohort. My current analyses follow a first-order Markov chain and are thus not state duration dependent—that is, transition probabilities are not adjusted by duration of stay in a given state. The HRS-style ADL questions utilized in this study do result in some ambiguity about whether the instrument is measuring underlying or residual disability (Freedman, 2000). Even though the questions asked were exactly the same across the four studied populations (aside from questionnaire translation), respondent interpretation may have varied across setting. Further research is needed to determine how strongly results from Mexico, Costa Rica, and Puerto Rico generalize to other similar contexts in Latin America.
The DFLE estimates presented here are based directly on individual-level reporting of ADL disability from nationally representative panel surveys. This approach to calculating population-level health represents an approach that is substantially different than most other metrics of population health, such as those of the Global Burden of Disease (GBD) reports (Salomon et al., 2012; Vos et al., 2012). The DFLE results in this article are a direct metric of the burden of disability experienced by individuals in these populations. This direct measurement of later-life health conditions contrasts with GBD’s sequela-based estimates, where national-level burdens of individual diseases are summed up to estimate the total disability burden of a population.
Combined, these results suggest that at present, the growing older adult populations in Costa Rica, Puerto Rico, and Mexico are not experiencing a substantially higher burden of disability than the disability experienced by those in the United States. This parity in levels of disability is particularly important given that the older adult populations of Costa Rica, Mexico, and Puerto Rico lived many years exposed to poor childhood conditions and a very different epidemiological context than prevails in these countries today. Though these four populations are reaching similar levels of overall DFLE, they may be taking very different paths to this outcome. These analyses present a first step toward understanding how early-life and late-life conditions have affected current patterns of disability and DFLE in LAC and how these countries compare with more developed contexts.
Funding
This work was supported by the National Science Foundation Graduate Research Fellowship (DGE-0822). The views expressed are those of the author alone.
Supplementary Material
Acknowledgments
An earlier version of this article was presented at the annual meeting of the Population Association of America, Boston, MA, May 1–3, 2014. The author thanks the Editor and three anonymous reviewers for their very helpful comments on the manuscript and Michel Guillot, Hans-Peter Kohler, and Paul Allison for their advice and patience. C.F. Payne designed the study, carried out the analyses, generated the figures and tables, and wrote the manuscript.
References
- Aguila E. Diaz C. Manqing Fu M. Kapteyn A., & Pierson A (2011). Living longer in Mexico: Income security and health. Santa Monica, CA: RAND Corporation. [PMC free article] [PubMed] [Google Scholar]
- Andrade E. C. D. (2010). Measuring the impact of diabetes on life expectancy and disability-free life expectancy among older adults in Mexico. The Journals of Gerontology, Series B: Social Sciences, 65, 381. doi:10.1093/geronb/gbp119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ben-Shlomo Y., Kuh D. (2002). A life course approach to chronic disease epidemiology: conceptual models, empirical challenges and interdisciplinary perspectives. International Journal of Epidemiology, 31, 285–293. doi:10.1093/ije/31.2.285 [PubMed] [Google Scholar]
- Cai L. Hayward M. D. Saito Y. Lubitz J. Hagedorn A., & Crimmins E (2010). Estimation of multi-state life table functions and their variability from complex survey data using the SPACE Program. Demographic Research, 22, 129–157. doi:10.4054/DemRes.2010.22.6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colón J. L. S.,& Comision Para Evaluar El Sistema De Salud Del Estado Libre Asociado de Puerto Rico. (2005). Evaluacion Del Sistema De Salud De Puerto Rico, San Juan, Puerto Rico. [Google Scholar]
- Cotlear D. (2011). Population aging: Is Latin America ready? Washington, DC: The World Bank. [Google Scholar]
- Crimmins E. M. Kim J. K., & Sole-Auro A (2011). Gender differences in health: Results from SHARE ELSA and HRS. European Journal of Public Health, 21, 81–91. doi:10.1093/eurpub/ckq022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ebrahim S., Pearce N., Smeeth L., Casas J. P., Jaffar S., Piot P. (2013). Tackling non-communicable diseases in low- and middle-income countries: Is the evidence from high-income countries all we need?PLoS Medicine, 10, e1001377. doi:10.1371/journal.pmed.1001377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eriksson C. Mohs E., & Eriksson B (1990). Assessment of health policy in Costa Rica—Some preliminary remarks. Scandinavian Journal of Social Medicine, 46, 82–91. [PubMed] [Google Scholar]
- Freedman V. A. (2000). Implications of asking “ambiguous” difficulty questions: An analysis of the second wave of the asset and health dynamics of the oldest old study. The Journals of Gerontology, Series B: Social Sciences, 55, S288–S297. [DOI] [PubMed] [Google Scholar]
- Gerst-Emerson K. Wong R. Michaels-Obregon A., & Palloni A (2015). Cross-national differences in disability among elders: Transitions in disability in Mexico and the United States. The Journals of Gerontology, Series B: Social Sciences, 70, 759–768. doi:10.1093/geronb/gbu185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gill T. M. Allore H. Hardy S. E. Holford T. R., & Han L (2005). Estimates of active and disabled life expectancy based on different assessment intervals. The Journals of Gerontology, Series A: Biological Sciences and Medical Sciences, 60, 1013–1016. [DOI] [PubMed] [Google Scholar]
- Hayward M. D. Hummer R. A. Chiu C. Gonzalez-Gonzalez C., & Wong R (2014). Does the Hispanic paradox in US adult mortality extend to disability?Population Research and Policy Review, 33, 81–96. doi:10.1007/s11113-013-9312-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ho J. Y., & Preston S. H (2010). US mortality in an international context: Age variations. Population and Development Review, 36, 749–773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang C., Soldo B. J., Elo I. T. (2011). Do early-life conditions predict functional health status in adulthood? The case of Mexico. Social Science & Medicine, 72, 100–107. doi:10.1016/j.socscimed.2010.09.040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kasper J. D., Freedman V. A. (2014). Findings from the 1st round of the National Health and Aging Trends Study (NHATS): Introduction to a special issue. The Journals of Gerontology, Series B: Social Sciences, 69, S1–S7. doi:10.1093/geronb/gbu125 [DOI] [PubMed] [Google Scholar]
- Kinsella K., & Velkoff V (2001). An aging world: 2001. Washington, DC: U.S. Census Bureau. [Google Scholar]
- McEniry M. Moen S., & McDermott J (2013). Methods report on the compilation of the RELATE cross national data set on older adults from 20 low, middle and high income countries. Ann Arbor, MI: ICPSR. [Google Scholar]
- McEniry M. (2013). Early-life conditions and older adult health in low- and middle-income countries: A review. Journal of Developmental Origins of Health and Disease, 4, 10–29. doi:10.1017/S2040174412000499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- MHAS Mexican Health and Aging Study(2001) and (2003). Data files and documentation: Mexican health and aging study Retrieved from www.MHASweb.org on July 22, 2014.
- Minicuci N. Noale M. Pluijm S. M. F. Zunzunegui M. V. Blumstein T. Deeg D. J. H. Bardage C., & Jylha M (2004). Disability-free life expectancy: A cross-national comparison of six longitudinal studies on aging. The CLESA project. European Journal of Ageing, 1, 37–44. doi:10.1007/s10433-004-0002-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monteverde M. Noronha K., & Palloni A (2009). Effect of early conditions on disability among the elderly in Latin America and the Caribbean. Population Studies, 63, 21–35. doi:10.1080/00324720802621583 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oksuzyan A., Crimmins E., Saito Y., O’Rand A., Vaupel J. W., Christensen K. (2010). Cross-national comparison of sex differences in health and mortality in Denmark, Japan and the US. European Journal of Epidemiology, 25, 471–480. doi:10.1007/s10654-010-9460-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Omran A. R. (1977). A century of epidemiological transition in the United States. Preventative Medicine, 6, 30–51. [DOI] [PubMed] [Google Scholar]
- Palloni A. McEniry M. Wong R., & Pelaez M (2006). The tide to come—Elderly health in Latin America and the Caribbean. Journal of Aging and Health, 18, 180–206. doi:10.1177/0898264305285664 [DOI] [PubMed] [Google Scholar]
- Palloni A. Pinto-Aguirre G., & Pelaez M (2002). Demographic and health conditions of ageing in Latin America and the Caribbean. International Journal of Epidemiology, 31, 762–771. doi:10.1093/ije/31.4.762 [DOI] [PubMed] [Google Scholar]
- Palloni A. Luisa Davila A., & Sanchez-Ayendez M (2013). Puerto Rican elderly: Health Conditions (PREHCO) Project, 2002–2003, 2006–2007. Inter-University Consortium for Political and Social Research (ICPSR). [Google Scholar]
- Palloni A., & McEniry M (2007). Aging and health status of elderly in Latin America and the Caribbean: Preliminary findings. Journal of Cross Cultural Gerontology, 22, 263–285. doi:10.1007/s10823-006-9001-7 [DOI] [PubMed] [Google Scholar]
- Palloni A., & Souza L (2013). The fragility of the future and the tug of the past: Longevity in Latin America and the Caribbean. Demographic Research, 29, 543–577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pan-American Health Organization. Health in the Americas Retrieved from http://www.paho.org/HIA/homeing.html on June 4, 2014.
- Payne C. F. Mkandawire J., & Kohler H (2013). Disability transitions and health expectancies among adults 45 years and older in Malawi: A cohort-based model. PLoS Medicine, 10, e1001435. doi:10.1371/journal.pmed.1001435 [DOI] [PMC free article] [PubMed] [Google Scholar]
- RAND Center for the Study of Aging. (2014). RAND HRS Data, Version N., Santa Monica, CA. [Google Scholar]
- Rosero-Bixby L. (2008). The exceptionally high life expectancy of Costa Rican nonagenarians. Demography, 45, 673–691. doi:10.1353/dem.0.0011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosero-Bixby L. (2004). Spatial access to health care in Costa Rica and its equity: A GIS-based study. Social Science & Medicine, 58, 1271–1284. doi:10.1016/S0277-9536(03)00322-8 [DOI] [PubMed] [Google Scholar]
- Rosero-Bixby L. (1990). Socioeconomic development, health interventions and mortality decline in Costa Rica. Scandinavian Journal of Social Medicine Supplementum, 46, 33–42. [PubMed] [Google Scholar]
- Rosero-Bixby L. Fernández X., & Dow W. H (2013). CRELES: Costa Rican Longevity and Healthy Aging Study, 2005 (Costa Rica Estudio de Longevidad y Envejecimiento Saludable), Inter-University Consortium for Political and Social Research (ICPSR). [Google Scholar]
- Saenz M. d. R., Bermudez J. L., Acosta M. (2010). Universal coverage in a middle income country: Costa Rica. World Health Report, WHO, Geneva, Switzerland. [Google Scholar]
- Salomon J. A., Wang H., Freeman M. K., Vos T., Flaxman A. D., Lopez A. D., Murray C. J. L. (2012). Healthy life expectancy for 187 countries, 1990–2010: A systematic analysis for the Global Burden Disease Study 2010. Lancet, 380, 2144–2162. doi:10.1016/S0140-6736(12)61690-0 [DOI] [PubMed] [Google Scholar]
- Schoen R. (1988). Modeling multigroup populations. New York, NY: Plenum Press. [Google Scholar]
- Stevens G. Dias R. H. Thomas K. J. A. Rivera J. A. Carvalho N. Barquera S. Hill K., & Ezzati M (2008). Characterizing the epidemiological transition in Mexico: National and subnational burden of diseases, injuries, and risk factors. PLoS Medicine, 5, 900–910. doi:10.1371/journal.pmed.0050125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- The World Bank. (2014). World development indicators Retrieved from http://data.worldbank.org/data-catalog/world-development-indicators on June 28, 2014
- U.S. Census Bureau. (2014). International data base Retrieved from http://www.census.gov/population/international/data/idb/informationGateway.php on June 10, 2014
- van Buuren S., Boshuizen H. C., Knook D. L. (1999). Multiple imputation of missing blood pressure covariates in survival analysis. Statistics in Medicine, 18, 681–694. [DOI] [PubMed] [Google Scholar]
- Verbrugge L. M., Jette A.M. (1994). The disablement process. Social Science & Medicine, 38, 1–14. [DOI] [PubMed] [Google Scholar]
- Vos T., Flaxman A. D., Naghavi M., Lozano R., Michaud C., Ezzati M., Shibuya K., Salomon J. A; the Global Burden of Disease Team. (2012). Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet, 380, 2163–2196. doi:10.1016/S0140-6736(12)61729-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolf D., & Gill T (2009). Modeling transition rates using panel current-status data: How serious is the bias?Demography, 46, 371–386. doi:10.1353/dem.0.0057 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.