Abstract
Introduction
To estimate the prevalence of use of different sources of contraceptive supplies in Britain and its variation by key demographic and behavioural characteristics.
Methods
Cross-sectional probability sample survey of women and men aged 16–74 years, resident in Britain, interviewed between 2010 and 2012. Analyses reported here were of 4571 women and 3142 men aged 16–44 years who reported having vaginal sex in the past year. Those relying exclusively on sterilisation (including hysterectomy) were excluded. Sources of contraceptive supplies were categorised as: general practice, community clinic, retail and other. Prevalence of use of these sources was estimated, and associated factors examined.
Results
Some 87.0% of women and 73.8% of men accessed at least one source of contraceptive supplies in the previous year. Most women (59.1%) used general practice and most men (54.6%) used retail outlets. Community clinics were less commonly used, by 23.0% of women and 21.3% of men, but these users were younger and at greater sexual health risk. These associations were also observed among the 27.3% of women and 30.6% of men who used more than one source category (general practice, community clinic or retail) for contraceptive supplies.
Conclusions
People in Britain use a variety of sources to obtain contraceptive supplies and some sources are more commonly used by those more vulnerable to poorer sexual health. Our findings suggest that national policy changes to increase access to contraceptive methods have had an effect on the diversity of services used.
Keywords: prevalence, user characteristics, contraceptive service use, family planning, natsal-3
Key message points.
General practice continues to be the most commonly used source by women for contraceptive supplies. It is therefore important that relevant practitioner skills and willingness to provide all methods be maintained in this setting.
Integrated sexual and reproductive health clinics and wider contraceptive provision in community settings, such as in schools and colleges, have helped reach those who have not accessed more traditional services in the past.
A strong case can be made for the provision of high-quality services in different settings and with different styles of service delivery to ensure that women and men have access to contraception that meets their needs.
Introduction
Contraceptive supplies have been available free of charge to all wishing to prevent pregnancy from the National Health Service (NHS) in Britain since the early 1970s. Open-access contraceptive services are provided in general practice, family planning clinics (FPCs) and young people’s services. The availability of a range of contraceptive sources and services including retail outlets helps ensure that the needs of different users are met.
The first decade of the 21st century saw several changes in the delivery of contraceptive services in Britain, largely in response to national strategies to improve sexual and reproductive health.1–4 Guidance relating to long-acting reversible contraceptives (LARC) from the National Institute of Health and Care Excellence extended their availability to general practice.5 Recommendations have been made for availability of contraception in schools and other educational settings to improve access for young people,6 and the trend towards integration of FPCs and genitourinary medicine (GUM) services has increased the likelihood that those attending for the treatment of sexually transmitted infection (STI) leave the service with contraception.7 8 During the same period, the provision of over-the-counter emergency contraception has increased.9 10
Of interest is the extent to which these changes may be reflected in patterns of contraceptive service use. In this article, we analyse data from the third National Survey of Sexual Attitudes and Lifestyles (Natsal-3) to estimate the prevalence of use of different sources of contraceptive supplies in Britain and its variation by key demographic and behavioural characteristics. In doing so, we update similar information from the second survey (Natsal-2).11
Methods
Data were analysed from Natsal-3, a multistage, clustered and stratified probability sample survey of 15 162 British residents aged 16–74 years interviewed between September 2010 and August 2012. Participants were interviewed in their homes using a combination of face-to-face computer-assisted personal interview (CAPI) and computer-assisted self-interview (CASI) for more sensitive questions. The sampling frame was the Postcode Address File. The response rate was 57.7% and the cooperation rate, for all the eligible addresses contacted, was 65.8%. Full details of the methods used in Natsal-3 and the characteristics of the complete sample are reported elsewhere.12–14
Measures
Participants were asked in the CAPI which methods of contraception they or together with a partner had used in the past year. Those reporting use of any method(s) were asked to identify which sources of supply they had used from a card showing all available options with the following question: “Have you got contraception from any of these sources in the last year?”.15 Sources listed were grouped into four categories: general practice (doctor or nurse), community clinic (sexual health (GUM) clinic, family planning/contraceptive/reproductive health clinic, youth services or school/college/university), retail (pharmacy/chemist, website, petrol station/supermarket/other shop, vending machine or mail order) and other (emergency department at hospital, antenatal clinic, private doctor or other). Sociodemographic characteristics used in this analysis included age, ethnic group, and educational attainment. Area of residence was categorised as rural or urban and area-related socioeconomic status was measured using the Index of Multiple Deprivation (IMD).16 IMD is a multi-dimensional measure of area (neighbourhood)-level deprivation based on the participants’ postcode. Sexual health and lifestyle indicators included current relationship status, parity, STI diagnosis and pregnancy, including planning status (ie, ambivalent/unplanned, planned, trying or not pregnant).
Statistical analyses
Women and men aged 16–44 years were included if they reported having (i) had vaginal intercourse in the past year, and (ii) not exclusively relied on either female or male sterilisation (including hysterectomy) for contraception. We used Stata (version 13.1) for complex survey analysis to incorporate weighting, clustering and stratification of the Natsal-3 data.13 We calculated the percentage of participants (with 95% confidence intervals) who had obtained contraception in the past year from each source and used the chi-square statistic to determine whether there were statistically significant variation in the reporting of these sources by sociodemographic characteristics and by lifestyle and sexual health variables. Participants were not asked from which sources they obtain specific contraceptive methods, and so we were unable to link method with source used. However, since use of LARC methods was likely to have been of longer duration, we included sole use of LARC (intrauterine contraceptives and implants) as an independent variable. Injectables were not included in the LARC category due to their lower continuation rates. Proportional Venn diagrams were used to represent the extent of overlap in use of different sources among those who had obtained contraceptive supplies.
Results
Some 4571 women and 3142 men were eligible for inclusion in the analysis; 87.0% of women and 73.8% of men obtained contraception from at least one source in the past year (table 1).
Table 1.
Use of sources to obtain contraceptives in the past year among women and men aged 16–44 years who had had vaginal sex in the past year
| Source of contraceptive supplies | Women | Men |
| Denominators (unweighted, weighted) | 4571, 3088 | 3142, 3182 |
| % (95% CI) | % (95% CI) | |
| General practice* | 59.1 (57.2 to 61.0) | 15.3 (13.6 to 17.0) |
| Community clinic | 23.0 (21.6 to 24.5) | 21.3 (19.6 to 23.0) |
| GUM clinic | 8.5 (7.6 to 9.5) | 10.8 (9.6 to 12.1) |
| Family planning clinic | 14.4 (13.2 to 15.7) | 6.8 (5.8 to 8.1) |
| Youth advisory clinic | 1.1 (0.8 to 1.6) | 2.1 (1.7 to 2.7) |
| School/college/university | 2.4 (1.9 to 3.0) | 6.4 (5.4 to 7.5) |
| Retail | 28.6 (26.9 to 30.3) | 54.6 (52.3 to 56.8) |
| Pharmacy/chemist | 21.3 (19.8 to 22.9) | 35.0 (32.8 to 37.2) |
| Internet website | 0.7 (0.5 to 1.2) | 3.1 (2.4 to 4.0) |
| Petrol station/supermarket | 10.3 (9.2 to 11.5) | 24.8 (23.0 to 26.7) |
| Vending machine | 0.7 (0.5 to 1.1) | 9.4 (8.2 to 10.7) |
| Mail order | 0.2 (0.1 to 0.4) | 0.7 (0.4 to 1.2) |
| Other | 2.9 (2.4 to 3.6) | 2.9 (2.3 to 3.6) |
| Emergency department at hospital | 0.30 (0.2 to 0.5) | 0.2 (0.1 to 0.5) |
| NHS antenatal clinic | 0.90 (0.7 to 1.3) | 1.0 (0.7 to 1.5) |
| Private doctor | 1.3 (0.9 to 1.7) | 1.0 (0.7 to 1.4) |
| Other | 0.5 (0.3 to 0.8) | 0.8 (0.5 to 1.3) |
| Contraception not obtained in the last year | 13.0 (11.6 to 14.4) | 26.2 (24.2 to 28.3) |
| Number of sources used† | ||
| 0 | 13.0 (11.6 to 14.4) | 26.2 (24.2 to 28.3) |
| 1 | 59.8 (57.9 to 61.6) | 43.3 (41.0 to 45.5) |
| 2 | 21.0 (19.6 to 22.5) | 20.6 (18.9 to 22.4) |
| 3+ | 6.2 (5.5 to 7.1) | 10.0 (8.8 to 11.3) |
*General practice includes doctor, nurse and general practice surgery.
†Any source rather than source category.
GUM, genitourinary medicine; NHS, National Health Service.
Prevalence of use of different sources of contraception
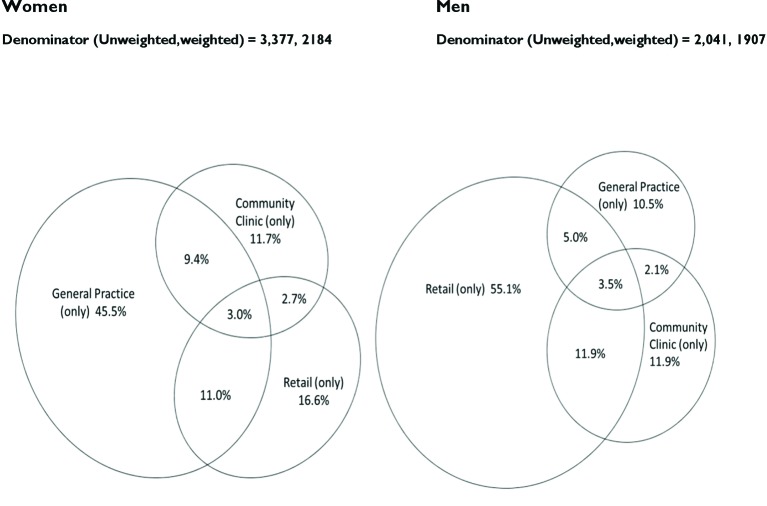
The source of contraceptive supplies used by the largest proportion of women (59.1%) was general practice. 28.6% obtained supplies from retail outlets, the majority being pharmacies. 23% of women obtained supplies from community services, predominantly FPCs (14.4%) but 8.5% obtained supplies from GUM services (table 1). 27.3% of women had used more than one source. Women most commonly reported use of both general practice and retail sources (11.0%) (figure 1).
Figure 1.
Extent of overlap in the type(s) of source used to obtain contraceptives in the past year among women and men aged 16–44 years who reported vaginal sex in the past year and obtaining contraceptives. These diagrams apply only to those who obtained contraception in the previous year and so the percentages differ from those presented in the tables, where the denominator includes those who had not.
The source of contraceptive supplies used by the largest proportion of men (54.6%) was retail outlets (table 1). Among retail suppliers, pharmacies were most commonly used by more than one-third of men, but petrol stations and supermarkets were used by one in four (24.8%) and vending machines by nearly one in ten (9.4%). Just over one-fifth (21.3%) of men used community clinics, of which GUM services were more commonly used than other community services. 15.3% of men reported contraception used by them being from general practice. 30.6% of men used more than one source of contraception, with the greatest overlap in use being community clinics and retail (11.9%) (figure 1).
Use of contraceptive sources by characteristics of participants
General practice
Marked age differences among women were seen in the use of general practice for contraceptive supplies (table 2). Roughly two-thirds of women in their 20s had obtained contraception from this source in the past year, compared with half of 16–17-year-olds and 35–44-year-olds. Statistically significant differences were also seen by other demographic variables. Women living in rural districts, those in cohabiting or ‘steady’ relationships as opposed to those who were single or married, and childless women compared with mothers, all more commonly used general practice for contraceptive supplies. Half of LARC users obtained supplies from general practice. Women with minimum educational qualifications, or none, more commonly used this source compared with those who were more highly qualified. The most marked difference, however, was seen by ethnic group. Compared with women identifying as ‘white’, considerably lower proportions of women in black and minority ethnic groups obtained contraception from general practice. Variation in use of general practice by health behaviour was not statistically significant among women.
Table 2.
Prevalence of source(s) used to obtain contraceptive supplies in the past year among women aged 16–44 years who had had vaginal sex in the past year by sociodemographic and behavioural characteristics*
| Sociodemographic and behavioural characteristics | General practice | Community clinics | Retail | More than one | None | |
| Denominators (unweighted, weighted) |
% (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) | |
| All | 4571, 3088 | 59.1 (57.2 to 61.0) | 23.0 (21.6 to 24.5) | 28.6 (26.9 to 30.3) | 27.3 (25.7 to 28.9) | 13.0 (11.6 to 14.4) |
| Age group (years) | p<0.0001 | p<0.0001 | p=0.0255 | p<0.0001 | p<0.0001 | |
| 16–17 | 242, 118 | 50.3 (43.5 to 57.0) | 53.7 (46.8 to 60.5) | 23.9 (18.4 to 30.4) | 43.5 (36.8 to 50.5) | 11.5 (7.7 to 16.9) |
| 18–19 | 345, 182 | 59.7 (53.9 to 65.3) | 45.2 (39.4 to 51.1) | 21.4 (17.2 to 26.4) | 36.2 (30.8 to 42.0) | 7.2 (4.5 to 11.4) |
| 20–24 | 865, 504 | 67.3 (63.6 to 70.7) | 36.5 (32.8 to 40.3) | 29.4 (26.1 to 33.0) | 40.9 (37.3 to 44.5) | 6.1 (4.5 to 8.2) |
| 25–29 | 1042, 522 | 66.0 (62.5 to 69.3) | 19.7 (17.3 to 22.3) | 30.2 (27.1 to 33.5) | 27.7 (24.8 to 30.7) | 8.8 (7.0 to 11.0) |
| 30–34 | 725, 464 | 60.0 (55.8 to 64.0) | 17.1 (14.3 to 20.2) | 31.0 (27.3 to 35.0) | 24.4 (21.2 to 28.0) | 13.4 (10.8 to 16.7) |
| 35–44 | 629, 758 | 49.6 (45.5 to 53.8) | 9.9 (7.6 to 12.7) | 27.8 (24.4 to 31.5) | 15.0 (12.4 to 18.0) | 21.7 (18.4 to 25.4) |
| Ethnic group† | p<0.0001 | p=0.0002 | p=0.0263 | p=0.0687 | p=0.1049 | |
| White | 3410, 2223 | 61.4 (59.3 to 63.4) | 22.2 (20.7 to 23.7) | 28.3 (26.6 to 30.1) | 27.4 (25.8 to 29.1) | 12.3 (10.9 to 13.8) |
| Black | 120, 92 | 38.7 (28.9 to 49.4) | 40.2 (30.2 to 51.0) | 23.2 (16.0 to 32.6) | 26.1 (18.5 to 35.5) | 16.0 (9.2 to 26.5) |
| Black: African | 64, 51 | 46.7 (32.6 to 61.3) | 32.7 (21.0 to 47.0) | 21.2 (12.1 to 34.5) | 23.9 (14.3 to 37.2) | 17.8 (8.5 to 33.7) |
| Black: Caribbean | 41, 28 | 29.2 (16.0 to 47.1) | 57.9 (38.8 to 75.0) | 30.2 (16.0 to 49.7) | 41.8 (25.1 to 60.7) | 9.9 (3.3 to 26.5) |
| Asian | 160, 126 | 39.3 (30.9 to 48.3) | 18.5 (12.3 to 26.9) | 39.3 (31.1 to 48.2) | 19.2 (13.4 to 26.9) | 16.8 (11.2 to 24.3) |
| Mixed/other | 163, 113 | 49.3 (40.2 to 58.5) | 31.5 (23.7 to 40.6) | 24.7 (17.7 to 33.3) | 30.7 (23.0 to 39.5) | 19.3 (12.2 to 29.2) |
| Academic qualificationsठ| p=0.0474 | p=0.0251 | p<0.0001 | p<0.0001 | p=0.3574 | |
| No academic qualifications | 270, 162 | 63.1 (56.3 to 69.5) | 27.2 (21.2 to 34.3) | 14.8 (10.6 to 20.3) | 21.5 (16.5 to 27.6) | 9.8 (6.6 to 14.5) |
| Academic qualifications typically gained at age 16 years | 1225, 791 | 62.7 (59.2 to 66.0) | 20.0 (17.6 to 22.6) | 24.1 (21.4 to 27.0) | 22.8 (20.3 to 25.4) | 12.1 (9.9 to 14.6) |
| Studying for/attained further academic qualifications | 2150, 1463 | 57.8 (55.3 to 60.3) | 23.7 (21.8 to 25.8) | 32.8 (30.5 to 35.3) | 30.8 (28.7 to 33.0) | 13.2 (11.4 to 15.1) |
| Quintiles of Index of Multiple Deprivation | p=0.7373 | p<0.0001 | p=0.8767 | p=0.3140 | p=0.1343 | |
| 1–2 (lower deprivation) | 1354, 950 | 59.6 (56.5 to 62.6) | 18.5 (16.4 to 20.9) | 28.9 (26.3 to 31.7) | 26.0 (23.6 to 28.5) | 14.7 (12.6 to 17.2) |
| 3 | 780, 528 | 59.9 (55.8 to 64.0) | 24.1 (21.1 to 27.4) | 29.0 (25.5 to 32.8) | 26.7 (23.3 to 30.5) | 11.7 (9.0 to 15.1) |
| 4–5 (higher deprivation) | 1714, 1070 | 58.2 (55.2 to 61.2) | 26.5 (24.1 to 29.0) | 28.0 (25.5 to 30.7) | 28.7 (26.2 to 31.2) | 12.0 (10.1 to 14.1) |
| Area type¶ | p=0.0010 | p<0.0001 | p=0.8584 | p=0.0386 | p=0.3058 | |
| Urban | 3162, 2082 | 57.6 (55.5 to 59.8) | 24.6 (23.0 to 26.3) | 28.5 (26.6 to 30.4) | 28.1 (26.3 to 29.9) | 13.3 (11.8 to 14.9) |
| Rural | 686, 465 | 65.7 (61.5 to 69.7) | 15.8 (13.1 to 19.1) | 28.9 (25.2 to 32.9) | 23.6 (20.2 to 27.4) | 11.4 (8.7 to 14.9) |
| Relationship status | p<0.0001 | p<0.0001 | p=0.4251 | p<0.0001 | p<0.0001 | |
| Married/civil partnership | 1044, 924 | 52.5 (49.1 to 55.8) | 11.1 (9.1 to 13.5) | 29.8 (26.8 to 33.1) | 18.0 (15.5 to 20.8) | 18.7 (16.0 to 21.6) |
| Living with partner | 899, 621 | 65.2 (61.5 to 68.7) | 21.1 (18.4 to 24.1) | 27.3 (24.2 to 30.6) | 27.1 (24.2 to 30.3) | 10.8 (8.4 to 13.7) |
| In a steady relationship | 993, 515 | 65.5 (62.0 to 68.8) | 36.3 (33.0 to 39.8) | 29.7 (26.4 to 33.2) | 38.8 (35.4 to 42.4) | 6.7 (5.0 to 8.9) |
| Single, never married | 902, 482 | 57.1 (53.4 to 60.7) | 34.1 (30.5 to 37.9) | 26.6 (23.3 to 30.2) | 32.9 (29.4 to 36.5) | 11.7 (9.4 to 14.4) |
| Opposite-sex partners, past year | p=0.4996 | p<0.0001 | p=0.1243 | p<0.0001 | p<0.0001 | |
| 1 | 2889, 2023 | 59.0 (56.7 to 61.1) | 18.8 (17.3 to 20.4) | 28.0 (26.1 to 30.0) | 23.7 (22.1 to 25.5) | 14.4 (12.9 to 16.2) |
| 2+ | 937, 510 | 60.4 (56.8 to 63.9) | 39.7 (36.0 to 43.5) | 31.0 (27.6 to 34.7) | 41.7 (38.2 to 45.4) | 6.8 (5.2 to 8.8) |
| Any STI diagnosis (excluding thrush) (past year) | p=0.9270 | p<0.0001 | p=0.4544 | p<0.0001 | p=0.0038 | |
| No | 3729, 2482 | 59.1 (57.2 to 61.1) | 22.2 (20.8 to 23.6) | 28.7 (27.0 to 30.5) | 26.8 (25.2 to 28.4) | 13.2 (11.8 to 14.6) |
| Yes | 94, 49 | 59.7 (46.2 to 71.9) | 65.4 (52.7 to 76.2) | 24.3 (15.0 to 37.0) | 56.8 (46.0 to 67.0) | 3.7 (1.5 to 9.0) |
| Pregnancy in past year | p=0.4000 | p<0.0001 | p=0.3186 | p=0.0002 | p=0.0004 | |
| Pregnancy: unplanned/ambivalent | 306, 178 | 59.8 (53.0 to 66.3) | 32.3 (26.6 to 38.5) | 28.4 (22.5 to 35.1) | 32.0 (26.4 to 38.1) | 6.1 (3.7 to 9.9) |
| Pregnancy: planned | 293, 188 | 60.5 (54.1 to 66.6) | 13.9 (10.2 to 18.8) | 24.6 (19.7 to 30.3) | 20.5 (16.0 to 25.9) | 17.2 (12.6 to 23.1) |
| Trying to get pregnant | 176, 125 | 53.3 (44.3 to 62.1) | 16.6 (11.3 to 23.7) | 20.0 (14.1 to 27.5) | 15.2 (10.5 to 21.6) | 20.8 (14.0 to 29.6) |
| No pregnancy | 1551, 1100 | 56.2 (53.2 to 59.2) | 17.4 (15.4 to 19.7) | 26.3 (23.8 to 28.9) | 21.0 (18.8 to 23.3) | 16.2 (14.1 to 18.7) |
| Number of children | p=0.0081 | p<0.0001 | p=0.0007 | p<0.0001 | p<0.0001 | |
| 0 | 1936, 1210 | 62.0 (59.5 to 64.5) | 29.8 (27.6 to 32.1) | 31.9 (29.5 to 34.4) | 35.3 (32.9 to 37.7) | 9.3 (7.8 to 11.1) |
| 1 | 783, 459 | 58.0 (54.0 to 62.0) | 19.6 (16.7 to 22.8) | 26.0 (22.6 to 29.7) | 22.4 (19.3 to 25.8) | 13.4 (10.7 to 16.8) |
| 2+ | 1119, 874 | 55.6 (52.1 to 59.1) | 15.3 (13.1 to 17.9) | 25.3 (22.4 to 28.3) | 18.7 (16.4 to 21.3) | 17.8 (15.2 to 20.7) |
| Used LARC only (past year) | 509, 374 | 48.0 (42.6 to 53.4) | 23.4 (19.5 to 27.7) | 2.0 (1.2 to 3.5) | 7.4 (5.5 to 10.0) | 30.8 (26.1 to 36.0) |
*P-values indicate differences within exposure category (ie, source of contraceptive supplies). Row percentages are presented; the categories are not mutually exclusive and add up to more than 100%.
†P-value presented corresponds to the categories: White, Black, Asian, Mixed/Other.
‡Participants aged ≥17 years.
§English General Certificate of Secondary Education or equivalent.
¶Urban is defined as areas with a population of >=10 000 people.
LARC, long-acting reversible contraception; STI, sexually transmitted infection.
Among men, the proportions reporting general practice as a source of contraception in the past year were statistically significantly higher among those living with a partner, fathers and those reporting only one sexual partner during the period (table 3).
Table 3.
Prevalence of source(s) used to obtain contraceptive supplies in the past year among men aged 16–44 years who had had vaginal sex in the past year by sociodemographic and behavioural characteristics*
| Sociodemographic and behavioural characteristics | General practice | Community clinics | Retail | More than one | None | |
| Denominators (unweighted, weighted) |
% (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) | |
| All | 3142, 3182 | 15.3 (13.6 to 17.0) | 21.3 (19.6 to 23.1) | 54.6 (52.3 to 56.8) | 30.6 (28.57 to 32.67) | 26.2 (24.2 to 28.3) |
| Age group (years) | p=0.2423 | p<0.0001 | p=0.0001 | p<0.0001 | p<0.0001 | |
| 16–17 | 195, 116 | 14.3 (9.8 to 20.4) | 58.9 (51.1 to 66.2) | 48.0 (40.4 to 55.8) | 41.2 (34.0 to 48.8) | 7.6 (4.3 to 13.0) |
| 18–19 | 287, 194 | 17.6 (13.2 to 23.0) | 53.0 (46.2 to 59.6) | 56.9 (49.9 to 63.6) | 46.7 (39.8 to 53.7) | 10.2 (6.9 to 14.8) |
| 20–24 | 671, 537 | 15.7 (12.7 to 19.3) | 37.3 33.4 to 41.4) | 63.1 (59.0 to 67.0) | 46.0 (41.9 to 50.2) | 16.0 (13.2 to 19.3) |
| 25–29 | 650, 514 | 12.9 (10.4 to 15.9) | 18.9 (15.6 to 22.6) | 57.1 (52.8 to 61.2) | 30.1 (26.1 to 34.4) | 25.7 (22.2 to 29.4) |
| 30–34 | 452, 476 | 18.2 (14.6 to 22.5) | 10.8 (7.9 to 14.6) | 55.6 (50.6 to 60.6) | 26.5 (22.3 to 31.2) | 28.3 (23.9 to 33.1) |
| 35–44 | 452, 802 | 14.3 (11.0 to 18.3) | 5.2 (3.5 to 7.8) | 47.0 (42.1 to 52.0) | 17.6 (14.1 to 21.8) | 38.6 (33.8 to 43.6) |
| Ethnic group† | p=0.5357 | p=0.0431 | p=0.0658 | p=0.2708 | p=0.0052 | |
| White | 2384, 2256 | 14.9 (13.3 to 16.7) | 21.0 (19.3 to 22.8) | 53.4 (51.0 to 55.7) | 30.7 (28.6 to 32.9) | 27.6 (25.4 to 29.9) |
| Black | 89, 97 | 21.2 (13.1 to 32.5) | 28.6 (18.8 to 40.9) | 67.0 (54.7 to 77.4) | 40.1 (28.7 to 52.8) | 12.1 (6.5 to 21.4) |
| Black: African | 51, 56 | 18.2 (8.9 to 33.6) | 26.0 (14.1 to 43.0) | 69.6 (52.4 to 82.7) | 41.5 (26.9 to 57.9) | 8.1 (3.2 to 19.3) |
| Black: Caribbean | 30, 33 | 22.4 (9.1 to 45.4) | 24.4 (12.0 to 43.3) | 56.7 (34.6 to 76.4) | 31.3 (15.7 to 52.7) | 22.0 (9.3 to 43.7) |
| Asian | 119, 170 | 16.4 (10.1 to 25.6) | 15.4 (9.2 to 24.7) | 63.4 (52.4 to 73.2) | 23.1 (15.6 to 32.7) | 16.5 (9.8 to 26.5) |
| Mixed/Other | 119, 120 | 17.2 (10.6 to 26.6) | 32.1 (23.6 to 42.1) | 58.7 (47.5 to 68.9) | 33.9 (25.3 to 43.8) | 21.9 (13.2 to 34.2) |
| Academic qualifications ठ| p=0.1968 | p=0.0265 | p<0.0001 | p=0.0001 | p<0.0001 | |
| No academic qualifications | 205, 209 | 19.5 (13.8 to 26.7) | 20.7 (15.1 to 27.7) | 40.8 (33.1 to 49.0) | 26.9 (20.3 to 34.7) | 33.7 (26.0 to 42.4) |
| Academic qualifications typically gained at age 16 years | 915, 888 | 15.6 (13.1 to 18.5) | 17.6 (15.1 to 20.5) | 48.5 (44.8 to 52.3) | 25.2 (22.2 to 28.4) | 33.0 (29.4 to 36.9) |
| Studying for/attained further academic qualifications | 1432, 1408 | 14.0 (11.9 to 16.3) | 22.8 (20.4 to 25.4) | 61.6 (58.6 to 64.5) | 34.5 (31.6 to 37.4) | 21.3 (18.8 to 24.0) |
| Quintiles of Index of Multiple Deprivation | p=0.0461 | p=0.0866 | p=0.8472 | p=0.2125 | p=0.1546 | |
| 1–2 (lower deprivation) | 1017, 1005 | 13.0 (10.7 to 15.8) | 19.7 (17.2 to 22.6) | 55.4 (51.8 to 59.0) | 30.5 (27.4 to 33.8) | 28.0 (24.8 to 31.5) |
| 3 | 529, 535 | 14.5 (11.5 to 18.1) | 19.6 (16.3 to 23.5) | 54.2 (49.3 to 59.0) | 27.3 (23.2 to 31.9) | 27.5 (22.9 to 32.6) |
| 4–5 (higher deprivation) | 1161, 1098 | 17.7 (15.1 to 20.6) | 23.5 (20.9 to 26.2) | 54.0 (50.4 to 57.5) | 32.2 (29.1 to 35.5) | 23.8 (20.9 to 27.0) |
| Area type¶ | p=0.3805 | p=0.8600 | p=0.002 | p=0.217 | p=0.002 | |
| Urban | 2201, 2166 | 14.9 (13.1 to 16.9) | 21.3 (19.5 to 23.3) | 56.1 (53.6 to 58.6) | 31.1 (28.8 to 33.5) | 24.6 (22.5 to 26.9) |
| Rural | 506, 472 | 16.7 (13.4 to 20.7) | 21.0 (17.4 to 25.0) | 47.5 (42.7 to 52.3) | 28.1 (24.2 to 32.4) | 33.2 (28.2 to 38.6) |
| Relationship status | p=0.0001 | p<0.0001 | p<0.0001 | p<0.0001 | p<0.0001 | |
| Married/civil partnership | 617, 887 | 19.1 (15.9 to 22.8) | 7.6 (5.7 to 10.2) | 47.0 (42.6 to 51.4) | 17.9 (14.8 to 21.5) | 34.7 (30.5 to 39.0) |
| Living with partner | 570, 604 | 17.3 (14.1 to 21.0) | 14.1 (11.4 to 17.3) | 44.0 (39.4 to 48.7) | 25.2 (21.5 to 29.3) | 37.9 (33.4 to 42.6) |
| In a steady relationship | 698, 525 | 10.9 (8.6 to 13.6) | 34.9 (30.8 to 39.1) | 61.6 (57.4 to 65.6) | 41.7 (37.3 to 46.1) | 18.4 (15.3 to 21.9) |
| Single, never married | 816, 617 | 11.6 (9.1 to 14.7) | 36.2 (32.5 to 40.0) | 70.0 (66.5 to 73.4) | 44.6 (40.7 to 48.6) | 9.1 (7.0 to 11.6) |
| Opposite-sex partners, past year | p=0.0289 | p<0.0001 | p<0.0001 | p<0.0001 | p<0.0001 | |
| 1 | 1802, 1913 | 16.3 (14.4 to 18.5) | 15.4 (13.7 to 17.3) | 50.2 (47.5 to 52.9) | 25.6 (23.3 to 28.0) | 31.5 (29.0 to 34.2) |
| 2+ | 882, 702 | 12.5 (10.2 to 15.4) | 37.3 (33.6 to 41.1) | 66.3 (62.7 to 69.8) | 44.0 (40.1 to 47.9) | 11.9 (9.5 to 14.6) |
| Any STI diagnosis (excluding thrush) (past year) | p=0.6319 | p<0.0001 | p=0.5533 | p=0.0342 | p=0.1018 | |
| No | 2617, 2552 | 15.1 (13.5 to 16.9) | 20.6 (18.9 to 22.3) | 54.7 (52.4 to 56.9) | 30.3 (28.2 to 32.4) | 26.5 (24.4 to 28.7) |
| Yes | 57, 47 | 18.0 (8.5 to 34.1) | 57.4 (42.6 to 71.1) | 50.2 (35.7 to 64.7) | 45.2 (31.1 to 60.1) | 15.5 (7.5 to 29.5) |
| Number of children | p=0.0268 | p<0.0001 | p<0.0001 | p<0.0001 | p<0.0001 | |
| 0 | 1893, 1614 | 13.5 (11.7 to 15.6) | 27.8 (25.6 to 30.1) | 61.3 (58.7 to 63.8) | 36.8 (34.3 to 39.4) | 19.4 (17.4 to 21.6) |
| 1 | 382, 416 | 17.3 (13.3 to 22.1) | 11.6 (8.7 to 15.3) | 43.2 (37.6 to 48.9) | 18.7 (14.9 to 23.2) | 35.9 (30.4 to 41.8) |
| 2+ | 429, 605 | 18.6 (14.9 to 22.9) | 10.5 (7.8 to 13.9) | 44.6 (39.4 to 49.9) | 22.3 (18.2 to 27.0) | 37.4 (32.3 to 42.8) |
| Partner used LARC only (past year) | 177, 193 | 20.4 (14.1 to 28.5) | 7.5 (4.4 to 12.6) | 9.1 (5.4 to 15.0) | 5.2 (2.6 to 10.0) | 64.2 (55.6 to 71.9) |
*P-values indicate differences within exposure category (ie, source of contraceptive supplies). Row percentages are presented; the categories are not mutually exclusive and add up to more than 100%.
†P-value presented corresponds to the categories: White, Black, Asian, Mixed/Other.
‡Participants aged ≥17 years.
§English General Certificate of Secondary Education or equivalent.
¶Urban is defined as areas with a population of >=10 000 people.
LARC, long-acting reversible contraception; STI, sexually transmitted infection.
Community clinics
Marked age differences were also seen in the use of community clinics for contraception. There was a strong and consistent age gradient with over half of 16–17-year-old women sourcing contraception from community clinics compared with fewer than 10% of those aged 35–44 years. Other variation by demographic characteristic tended to reverse that found in relation to general practice. Community clinics were more commonly used by women living in urban areas, women in black and ethnic minority groups, those not co-habiting with a partner, and childless women. Variation was also seen by demographic characteristics, which were not significantly associated with use of general practice. Notable among these was area-related deprivation; women living in poorer areas more commonly sought contraceptive supplies from community clinics compared with those living in more affluent areas. Statistically significant associations between sourcing contraception from community clinics and sexual health-related variables were found which were also not seen for general practice. Use of community clinics was statistically higher among women diagnosed with an STI, those with more than one partner, and those who had an unplanned pregnancy in the past year.
Among men, the age gradient in use of community clinics was even more marked than among women; 58.9% of 16–19-year-olds had used community clinics in the past year, compared with 5.2% of 35–44-year-olds. Statistically significant differences in use were seen by all the sexual health variables.
Retail outlets
Among women, few strong or consistent differences in use of retail outlets were seen by demographic characteristics, and none by sexual health variables. A strong gradient was seen by academic achievement with almost one-third of women studying for or having attained post-16 qualifications reporting use, compared with barely 15% of those with minimum educational qualifications or none. Other significant associations were observed in relation to parity and ethnicity, with women without children (31.9%) and Asian women (39.3%) most commonly reporting use of retail outlets.
More variation by demographic characteristic was observed among men. Statistically significant differences were seen by age, educational level, area of residence, relationship status and parity. Use was highest among men aged 20–24 years, those with the highest educational qualifications, those living in urban areas, those who were neither married nor cohabiting, and those without children.
Use of more than one source of contraception
Age differences were seen in the use of more than one source of contraceptive supplies. More than one-third of women aged under 25 years had used two or more sources in the past year. Statistically significant associations were also seen between multiple use and higher educational level, being unmarried, having more than one sexual partner in the past year, having been diagnosed with an STI, having experienced unplanned pregnancy, and being childless.
A broadly similar pattern was observed among men. Statistically significant associations were seen between use of more than one source and being under 25, being unmarried, having two or more partners in the past year, an STI diagnosis in the past year and not having children.
Use of no source of contraception
Some 13% of sexually active women reported having used no source of contraceptive supplies in the past year, although their partner may have done so. Age was associated with non-use, being most common among women in the 35–44 years age group. Not having used a source of contraception was significantly less common among women who were unmarried, childless, who had had an unplanned pregnancy during the past year, who had more than one sexual partner and who had been diagnosed with an STI. The proportion was highest among LARC users, rising to 30.8%.
Among men, prevalence of non-use was also higher in older age groups. Not having used a source of contraceptive supplies was significantly less common among unmarried men, those without children, those living in urban areas, and those identifying as Black Caribbean. It was also lower among men reporting more than one sexual partner and among those diagnosed with an STI in the past year.
Discussion
These data, from a large population-based national survey, provide information on patterns of service use for contraception among women and men in Britain. They show high proportions accessing a source of contraceptive supplies in the past year, nearly 90% of women and almost three-quarters of men. The majority of women, six in ten, use general practice and roughly the same proportion of men use retail suppliers. Little more than one in five women and men access contraception from community clinics, but those who do are younger and at greater risk of poor sexual health. Similar characteristics are seen for the sizeable minority who used more than one source in the past year.
A strength of this study is that it provides data from a large representative community sample rather than, as is more often the case, from attenders at health services.17–19 We were able to examine use of contraceptive sources by a wider range of factors than is usual, including not only sociodemographic characteristics but indicators of sexual and reproductive health status. Caution is needed in interpreting some findings due to the small numbers in some categories (eg, ethnic group). We also need to bear in mind that, in identifying the source of contraception used during the past year, we cannot be sure that participants were not referring to access by their partner and this is perhaps more likely to apply in the case of men. Nor were we able to establish which contraceptive methods were obtained from which sources, and participants may have interpreted ‘source’ as their main provider or all services involved in obtaining a contraceptive method. For example, contraceptive pill/oral contraceptives users may get their prescription from a general practitioner (GP) but may have to pick up their supplies from a pharmacy. Finally, we were unable to establish whether user preference for method determines choice of source, or vice versa. While most contraception is used for the prevention of pregnancy, other benefits such as management of acne or STI protection may also affect choice of source to obtain methods. The source from which women and men obtain a contraceptive method will depend on a number of variables, including which service is able to provide it. Condoms are rarely available free of charge from general practice in Britain; hormonal methods (emergency contraception excepted) are not available from retail outlets; and methods such as withdrawal and periodic abstinence require no contact with a provider.
Although direct comparisons with data from Natsal-2, conducted between 1999 and 2001, are not possible because of slight differences in question wording (Natsal-2 asked about use of sources of contraceptive advice or supplies while Natsal-3 asked only about supplies), we can nevertheless identify some shifts in patterns of use between the two surveys.10 A marked increase can be seen in use of any source of contraceptive supplies by the whole population aged 16–44 years, but especially among younger men. Two-thirds of men aged under 20 had accessed no source of contraception (for either advice or supplies) in 2000 but a decade later nine in ten reported accessing a service for supplies. Prevalence of sources of contraception is still ranked in the same order as was seen in Natsal-2. General practice remains the source used by the majority of women, the proportion of women using this source is virtually unchanged between the surveys (59.2% in Natsal-2). By contrast, although still accessed by smaller proportions, use of community clinics by both women and men increased between 2000 and 2010, as did use of retail outlets. In Natsal-2, 15.0% of women and 7.7% of men reported use of community clinics in the last year and 22.5% and 42.7%, respectively, reported use of retail. Commensurate with these changes, reported use of more than one source of contraception was higher in Natsal-3 than in Natsal-2, especially among men.
If these data represent true trends and not simply changes to question wording, they may reflect recent changes in public health policy and practice. The increase in the use of any source of contraception by men may follow from the now broader range of services available, including school- and college-based services. It may also be associated with a shift in focus from traditionally organised, women-centred family planning services towards integrated sexual and reproductive health services likely to have broader appeal in which staff may be better able to discuss contraception with young men attending for STI-related reasons.7 8 The increase in use of community clinics, which is consistent with increases in attendance observed using routinely collected clinic data,20 is likely to be welcomed by commissioners and providers in Britain as validating the considerable efforts made at the start of the 21st century to reach their target clientele. Their higher prevalence of use among the young, those living in more deprived areas, and those at greater sexual health risk is consistent with the growth in the number of dedicated young people’s services, increased accessibility, extended opening hours and capacity to provide drop-in services. The trend towards greater use of retail services by women may reflect greater availability of over-the-counter emergency contraception. The high proportion of LARC users reporting use of no service, almost a third, is likely to be attributable to the growing number of women using LARC methods which require few visits to services.
This said, general practice is still the mainstay of contraceptive provision in Britain, at least among women. Healthcare professionals in this setting provide services to more women who are single, multi-partnered and living in more deprived areas with contraception than do those in community clinics. General practice supplies twice as many women with LARC methods than community clinics, which may reflect financial incentives to increase LARC uptake introduced in general practice.21 It follows that staff in general practice are still vitally important as a source of contraceptive supplies and need to maintain their skills and willingness to provide all methods. This is especially so in rural areas where community clinics are less commonly situated, a fact consistent with evidence in our data of lower rates of their use outside cities and towns. However, while there has been some evidence that LARC provision has been increasing in general practice, these methods may not be available in many practices requiring referral to more specialist services.17 22
We cannot tell whether the increase in use of multiple sources in general, and in particular among young people, is attributable to users ‘shopping around’ to find out which service best suits their needs, whether the mix of contraceptive methods they use requires use of different services or whether young people are more likely to be referred between different services compared with those in older age groups. These issues may require further investigation. Data from Natsal-3 on actual and preferred use of sources of contraceptive supplies showed that one-third of those aged under 25 years reported not having accessed their preferred source and this discordance was associated with use of less effective contraception and markers of poor sexual and reproductive health.23
These data on variation in the use of different sources by users’ characteristics will be of interest to those planning, purchasing and providing services. They may also provide evidence supporting the retention and expansion of community-based services. In England, local authorities are responsible for ensuring the availability of "confidential, open access services for STIs and contraception as well as reasonable access to all methods of contraception".24 This includes costs of the contraceptive methods or prescriptions and specialist sexual health services. Additional services provided in general practice, such as contraceptive advice and medical examinations of those seeking advice (excluding the fitting of any contraceptive devices), are commissioned by NHS England under the GP contract. Concerns have been raised that the move to the commissioning of enhanced contraceptive services to local authorities will lead to greater centralisation of services and fewer services providing more specialist care and facilities.25 Although access to contraception has widened over the last decade, there remains yet more potential for expanding services in community pharmacies and via the internet, such as by the provision of oral contraceptives.26–28 The increase in the choice of sources for contraceptive supplies and greater choice of contraceptive methods available from these sources have coincided with a decline in teenage pregnancy.29 30 A strong case can be made for continuing to provide high-quality services in different settings and with different styles of service delivery.
Acknowledgments
Natsal-3 is a collaboration between University College London, the London School of Hygiene and Tropical Medicine, NatCen Social Research, Public Health England, and the University of Manchester.
Footnotes
Contributors: RSF led on the writing of the paper. RG and KJ conducted the statistical analysis. All other authors (KW, AG, JD, CHM, MP, AMJ, WM) commented on drafts of the paper and were involved in the planning and conduct of the study.
Funding: Natsal-3 was supported by grants from the Medical Research Council (G0701757)and the Wellcome Trust (084840), with contributions from the Economic and Social Research Council and Department of Health.
Competing interests: AG receives an honorarium from HRPharma. None of the other authors report conflicting interests.
Ethics approval: The Natsal-3 study was approved by the Oxfordshire Research Ethics Committee (Reference: 09/H0604/27).
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Social Exclusion Unit. Teenage pregnancy. London: Stationery Office, 1999. http://dera.ioe.ac.uk/15086/1/teenage-pregnancy.pdf (accessed 08 Jun 2016). [Google Scholar]
- 2. The Scottish Executive Health Department. Respect and responsibility. Strategy and action plan for improving sexual health, 2005. http://www.gov.scot/Resource/Doc/35596/0012575.pdf (accessed 08 Jun 2016).
- 3. Welsh Assembly Government. Sexual health and wellbeing: action plan for Wales 2010-15, 2010. http://www.shnwales.org.uk/Documents/485/Strategy_%28English%29.pdf (accessed 08 Jun 2016).
- 4. Department of Health. The National Strategy for Sexual Health and HIV, 2001. http://webarchive.nationalarchives.gov.uk/20130107105354/http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/@dh/@en/documents/digitalasset/dh_4058945.pdf (accessed 08 Jun 2016).
- 5. National Collaborating Centre for Women’s and Children’s Health. Long-acting reversible contraception (NICE Guideline). London, UK: RCOG Press, 2005. [Google Scholar]
- 6. National Institute for Health and Excellence. Contraceptive services for under 25s: NICE, 2014. https://www.nice.org.uk/guidance/ph51 (accessed 24 Aug 2016). [Google Scholar]
- 7. Griffiths C, Gerressu M, French RS. One-Stop Shop Evaluation Team. Are one-stop shops acceptable? Community perspectives on one-stop shop models of sexual health service provision in the UK. Sex Transm Infect 2008;84:395–9. 10.1136/sti.2008.030833 [DOI] [PubMed] [Google Scholar]
- 8. French RS, Mercer CH, Robinson AJ, et al. Addressing sexual health needs: a comparison of a one-stop shop with separate genitourinary medicine and family planning services. J Fam Plann Reprod Health Care 2010;36:202–9. 10.1783/147118910793048502 [DOI] [PubMed] [Google Scholar]
- 9. Marston C, Meltzer H, Majeed A. Impact on contraceptive practice of making emergency hormonal contraception available over the counter in Great Britain: repeated cross sectional surveys. BMJ 2005;331:271 10.1136/bmj.38519.440266.8F [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Glasier A, Manners R, Loudon JC, et al. Community pharmacists providing emergency contraception give little advice about future contraceptive use: a mystery shopper study. Contraception 2010;82:538–42. 10.1016/j.contraception.2010.05.008 [DOI] [PubMed] [Google Scholar]
- 11. French RS, Mercer CH, Johnson AM, et al. Use of contraceptive services in Britain: findings from the second National Survey of Sexual Attitudes and Lifestyles (Natsal-2). J Fam Plann Reprod Health Care 2009;35:9–14. 10.1783/147118909787072360 [DOI] [PubMed] [Google Scholar]
- 12. Erens B, Phelps A, Clifton S, et al. Methodology of the third British National Survey of Sexual Attitudes and Lifestyles (Natsal-3). Sex Transm Infect 2014;90:84–9. 10.1136/sextrans-2013-051359 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Erens B, Phelps A, Clifton S, et al. The third National Survey of Sexual Attitudes and Lifestyles (Natsal-3): technical report. http://www.natsal.ac.uk/natsal-3/methodology.aspx (accessed 08 Jun 2016).
- 14. Mercer CH, Tanton C, Prah P, et al. Changes in sexual attitudes and lifestyles in Britain through the life course and over time: findings from the National Surveys of Sexual Attitudes and Lifestyles (Natsal). Lancet 2013;382:1781–94. 10.1016/S0140-6736(13)62035-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. The National Survey of Sexual Attitudes and Lifestyles Questionnaire. Revised for Natsal 3. http://www.natsal.ac.uk/media/2078/b1-capi-and-casi-questionnaire.pdf (accessed 07 Jun 2017).
- 16. Payne RA, Abel GA. UK indices of multiple deprivation-a way to make comparisons across constituent countries easier. Health Stat Q 2012;53:22–37. [Google Scholar]
- 17. Cea-Soriano L, García Rodríguez LA, Machlitt A, et al. Use of prescription contraceptive methods in the UK general population: a primary care study. BJOG 2014;121:53–61. 10.1111/1471-0528.12465 [DOI] [PubMed] [Google Scholar]
- 18. Cea Soriano L, Wallander MA, Andersson S, et al. Use of long-acting reversible contraceptives in the UK from 2004 to 2010: analysis using the health improvement network database. Eur J Contracept Reprod Health Care 2014;19:439–47. 10.3109/13625187.2014.948613 [DOI] [PubMed] [Google Scholar]
- 19. Reddy A, Watson M, Hannaford P, et al. Provision of hormonal and long-acting reversible contraceptive services by general practices in Scotland, UK (2004-2009). J Fam Plann Reprod Health Care 2014;40:23–9. 10.1136/jfprhc-2012-100477 [DOI] [PubMed] [Google Scholar]
- 20. Health and Social Care Information Centre. NHS contraceptive services: England Community Contraceptive Clinics. Statistics for 2013-14. England: NHS Contraceptive Services, 2014. [Google Scholar]
- 21. Arrowsmith ME, Majeed A, Lee JT, et al. Impact of pay for performance on prescribing of long-acting reversible contraception in primary care: an interrupted time series study. PLoS One 2014;9:e92205 10.1371/journal.pone.0092205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Ma R, Brown E. An evaluation of commissioning arrangements for intrauterine and subdermal contraception services from general practitioners in London, UK. J Fam Plann Reprod Health Care 2015;41:54–9. 10.1136/jfprhc-2013-100831 [DOI] [PubMed] [Google Scholar]
- 23. Geary RS, Tommes C, Jones K, et al. Actual and preferred sources of contraception among young people in Britain: findings from the third National Survey of Sexual Attitudes and Lifestyles (Natsal-3). BMJ Open 2016;6:e011966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Public Health England. MEDFASH Making it work. A guide to whole system commissioning for sexual health, reproductive health and HIV. 2014. https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/408357/Making_it_work_revised_March_2015.pdf (accessed 11 May 2017).
- 25. Advisory Group for Contraception. Commissioning high quality contraceptive services: a guide for commissioning groups, 2014. http://theagc.org.uk/wp-content/uploads/2013/08/Commissioning-high-quality-contraceptive-services-A-guide-for-clinical-commissioning-groups-%E2%80%93-February-2014.pdf (accessed 08 Jun 2016).
- 26. Parsons J, Adams C, Aziz N, et al. Evaluation of a community pharmacy delivered oral contraception service. J Fam Plann Reprod Health Care 2013;39:97–101. 10.1136/jfprhc-2012-100304 [DOI] [PubMed] [Google Scholar]
- 27. Michie L, Cameron ST, Glasier A, et al. Pharmacy-based interventions for initiating effective contraception following the use of emergency contraception: a pilot study. Contraception 2014;90:447–53. 10.1016/j.contraception.2014.05.004 [DOI] [PubMed] [Google Scholar]
- 28. Gawron LM, Turok DK. Pills on the World Wide Web: reducing barriers through technology. Am J Obstet Gynecol 2015;213:500.e1–4. 10.1016/j.ajog.2015.06.002 [DOI] [PubMed] [Google Scholar]
- 29. Office for National Statistics. Live births in England and Wales by characteristics of mother 1: 2013, 2014. http://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/livebirths/bulletins/livebirthsinenglandandwalesbycharacteristicsofmother1/2014-10-16 (accessed 08 Jun 2016).
- 30. Wellings K, Palmer MJ, Geary RS, et al. Changes in conceptions in women younger than 18 years and the circumstances of young mothers in England in 2000-12: an observational study. Lancet 2016;388:586–95. 10.1016/S0140-6736(16)30449-4 [DOI] [PMC free article] [PubMed] [Google Scholar]