Abstract
Angiogenesis plays a pivotal role in normal ovarian physiology as well as in the progression of ovarian cancer through ascites formation and metastatic spread. Bevacizumab (Avastin®, Genentech; South San Francisco, CA, USA), a humanized anti-vascular endothelial growth factor (VEGF) monoclonal antibody, is the most widely studied anti-angiogenesis agent both across tumor types and specifically in epithelial ovarian cancer. In 2005, single-agent bevacizumab at 15 mg/kg (IV) every 3 weeks was first reported to be active in a case of recurrent high-grade serous ovarian cancer after failing 11th line cytotoxic treatment. Since then, many case series, phase II and phase III trials have confirmed these results leading to regulatory approval in most countries including the US Food and Drug Administration in 2014. Guidelines now give clear recommendations as to when and how bevacizumab should be integrated into the ovarian cancer treatment paradigm. Other anti-VEGF agents such as the VEGF receptor (VEGFR) tyrosine kinase inhibitors have not shown increased activity or reduced toxicity relative to bevacizumab. However, anti-angiogenics other than anti-VEGF/VEGFR agents such as those targeting Angiopoietin-1 and -2 are in development as well as novel combinations with vascular disrupting agents (VDAs), PARP inhibitors and immune checkpoint inhibitors. Clearly, the benefits of anti-angiogenic agents such as bevacizumab must be carefully weighed against the cost and associated toxicities. Although almost all patients with ovarian cancer will receive an anti-angiogenic compound, cures are not increased. Predictive biomarkers are an urgent unmet need.
Keywords: bevacizumab, fosbretabulin, nintedanib, pazopanib, cediranib, trebananib
bevacizumab: the first active targeted agent in ovarian cancer
Since the 1990s, a combination of a platinum and taxane has been standard in treating newly diagnosed peritoneal, fallopian tube, and ovarian cancer, collectively known as epithelial ovarian cancer (EOC) [1]. Most would agree that, variations in chemotherapy dosing, scheduling, and the route of administration have only made modest improvements in frontline management. In the recurrent setting, only topotecan [2], pegylated liposomal doxorubicin (PLD) [3], and trabectedin [4] in platinum-resistant disease and combination gemcitabline/carboplatin in sensitive disease have gained regulatory approval in most countries but again, only with marginal improvements. Until 2014, the US Food and Drug Administration (FDA) had not approved any targeted therapies in EOC, making it the most lethal cancer in American and European women without an available targeted intervention. However, on 14 November 2014, the US FDA approved bevacizumab for the treatment of platinum-resistant EOC [5]. Bevacizumab is the first active targeted therapy in EOC and the current publication will highlight its mechanism of action, development, as well as mechanisms of resistance and novel combinations. Other therapies that target angiogenesis will also be reviewed.
Angiogenesis plays a fundamental role in normal ovarian physiology as well as in the pathogenesis of ovarian cancer, promoting tumor growth and progression through ascites formation and metastatic spread. Vascular endothelial growth factor (VEGF) and VEGF receptor (VEGFR) are expressed on ovarian cancer cells, and increased VEGF expression has been associated with the development of malignant ascites and tumor progression [6]. Bevacizumab (Avastin®, Genentech, South San Francisco, CA, USA), a humanized anti-VEGF monoclonal antibody, is the most widely studied anti-angiogenesis agent both across tumor types and specifically in EOC. Preclinical data suggest that prolonged administration of bevacizumab as maintenance therapy after cisplatin-based chemotherapy prolongs survival by inhibiting or delaying disease recurrence in a murine ovarian cancer model [7].
In March 2005, single-agent bevacizumab at 15 mg/kg (IV) every 3 weeks was first reported to be active in a case of recurrent high-grade serous ovarian cancer after failing 11th line cytotoxic chemotherapy and radiation. An objective durable response lasting more than 5 months was documented [8]. Since then, many case series [9] and phase II trials have confirmed these results. Gynecologic Oncology Group (GOG) protocol 170-D prospectively studied single-agent bevacizumab at this dose and schedule among 62 women with recurrent ovarian cancer. Thirteen patients (21.0%) had documented responses (2 complete, 11 partial; median response duration, 10 months), and 25 (40.3%) survived progression-free for at least 6 months. The median progression-free survival (PFS) and overall survival (OS) were 4.7 and 17 months, respectively. Prior platinum sensitivity, age, number of prior chemotherapeutic regimens, or performance status were not predictive of clinical activity [10].
positive randomized phase III trials
Most recently, four randomized phase III trials have been carried out adding bevacizumab to either frontline chemotherapy (GOG protocol 218 [11] or ICON7 [12]) or to chemotherapy in ‘platinum-resistant’ (AURELIA Trial [13]) or ‘platinum-sensitive’ (OCEANS Trial [14]) recurrent EOC. Although all four studies met their primary end points of prolonging PFS (Table 1), only two suggested an improvement in OS among predefined subgroups in exploratory analyses. In ICON7, among patients at high risk for progression (FIGO stage IV disease or FIGO stage III disease and >1.0 cm of residual disease after debulking surgery), the benefit of adding bevacizumab was greatest. The estimated median PFS was 10.5 months with standard therapy, when compared with 15.9 months with bevacizumab {hazard ratio (HR) for progression or death in the bevacizumab group = 0.68 [95% confidence interval (CI) 0.55–0.85]; P < 0.001}. The final analysis of OS of these 502 poor prognosis patients showed that 332 (66%) had died (174 in the standard chemotherapy group and 158 in the bevacizumab group), with a significant difference among women who received bevacizumab plus chemotherapy compared with those who received chemotherapy alone [restricted mean survival time 34.5 months (95% CI 32.0–37.0) with standard chemotherapy versus 39.3 months (37.0–41.7) with bevacizumab; log-rank P = 0.03] [15]. In GOG protocol 218, a larger and placebo-controlled study of bevacizumab at twice the dose (15 mg/kg), the median OS for FIGO stage IV subjects was increased from 32.8 months in arm 1 (placebo containing arm) to 40.6 months in arm 3 with the addition of bevacizumab plus maintenance [HR = 0.72 (95% CI 0.53–0.97)] [16]. The consistency in the data across these trials suggests that those with bulky disease may be the ideal candidates for frontline bevacizumab, although this hypothesis requires prospective validation.
Table 1.
Phase III trials of bevacizumab in epithelial ovarian cancer
| Study | Setting | n | Treatment arm | PFS (median, months) | PFS, HR (95%CI) | OS (median, months) | OS, HR (95% CI) |
|---|---|---|---|---|---|---|---|
| GOG-218 [11] | Frontline and maintenance | 1873 | I: paclitaxel + carboplatin + placebo; placebo maintenance | 10.3 | – | 39.3 | – |
| II: paclitaxel + carboplatin + bevacizumab; placebo maintenance | 11.2 | 0.91 (0.8–1.04) | 38.7 | 1.036 (0.83–1.3) | |||
| III: paclitaxel + carboplatin + bevacizumab; bevacizumab maintenance | 14.1 | 0.72 (0.63–0.82) | 39.7 | 0.92 (0.73–1.15) | |||
| ICON7 [12, 15] | Frontline and maintenance | 1528 | I: paclitaxel + carboplatin | 17.5 | – | 58.6 | – |
| II: paclitaxel + carboplatin + bevacizumab; bevacizumab maintenance | 19.98 | 0.93 (0.83–1.05) | 58.0 | 0.99 (0.85–1.14) | |||
| AURELIA [13] | Recurrent, platinum-resistant | 361 | I: chemotherapy (paclitaxel-weekly, topotecan-daily 5× or weekly, PLD) | 3.4 | – | 13.3 | – |
| II: chemotherapy + bevacizumab | 6.7 | 0.48 (0.38–0.6) | 16.6 | 0.85 (0.66–1.08) | |||
| OCEANS [14] | Recurrent, platinum-sensitive | 484 | I: gemcitabine + carboplatin + placebo (combination and maintenance) | 8.4 | – | 35.2 | – |
| II: gemcitabine + carboplatin + bevacizumab (combination and maintenance) | 12.4 | 0.48 (0.39–0.61) | 33.3 | 1.027 (0.79–1.33) | |||
| GOG-213 [17] | Recurrent, platinum-sensitive | 674 | I: paclitaxel + carboplatin | 10.4 | – | 37.3 | – |
| II: paclitaxel + carboplatin + bevacizumab; bevacizumab maintenance | 13.8 | 0.61 (0.52–0.72) | 42.2 | 0.83 (0.68–1.005) |
PFS, progression-free survival; OS, overall survival; HR, hazard ratios.
aEstimated from publication.
Unfortunately, there has been concern about toxicity, especially bowel perforation [11], renal dysfunction, and hypertension [12]. In addition, the expense and cost-effectiveness of bevacizumab has created much controversy [13]. Furthermore, biomarkers and imaging have not consistently been predictive of response [14–16] and patient-reported outcomes (PRO) have not shown improvements in quality of life with the addition of bevacizumab [17]. Importantly, both AURELIA and ICON7 were not placebo-controlled trials, creating a potential bias in evaluating both PRO and PFS. OCEANS had no PROs at all.
A fifth randomized phase III trial has been presented. Peer-review publication is imminent. GOG protocol 213 is a randomized open label phase III trial of carboplatin and paclitaxel with or without 15 mg/kg of bevacizumab every 3 weeks followed by maintenance [17]. The primary end point was OS. Although there was an improvement in PFS [adjusted HR = 0.61 (95% CI 0.52–0.72); P < 0.0001, median 10.4 and 13.4 months], the 674 patient study barely missed statistical significance for OS [adjusted HR = 0.829 (95% CI 0.683–1.005); P = 0.056]. Many believe that the 5-month improvement from 37.3 to 42.2 months associated with bevacizumab in GOG protocol 213 is clinically important despite the fact that the two-sided P-value barely missed being <0.05. GOG protocol 213 stands in strong contrast to the OCEANS trial, also a study in platinum-sensitive relapsed EOC, where there was no hint of an OS signal. Could this simply be related to the chemotherapy backbone suggesting that carboplatin plus paclitaxel is better than carboplatin plus gemcitabine as a companion for bevacizumab? Obviously, this requires prospective validation, but the AGO-OVAR 2.21/ENGOT-ov18 trial compares carboplatin plus gemcitabine with bevacizumab to carboplatin plus PLD with bevacizumab (ClinicalTrials.gov Identifier: NCT01837251). So, this critical question of the optimal chemotherapy backbone in combination with bevacizumab will likely go unanswered. The ICON 6 study [18] discussed below further supports carboplatin plus paclitaxel as the best chemotherapy backbone in platinum-sensitive recurrent disease.
regulatory approvals, guidelines, and adding value to care
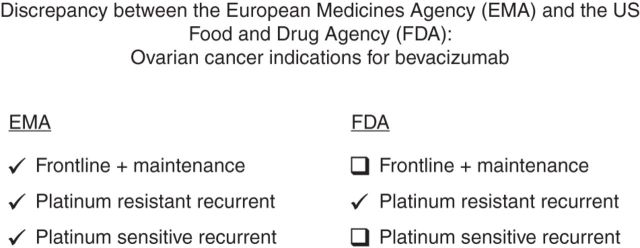
As a result of the four positive randomized trials adding bevacizumab to chemotherapy in EOC, bevacizumab has gained regulatory approval by the European Medicines Agency (EMA) with the first approval being based on GOG protocol 218 in 2011 and subsequent approvals following in platinum-sensitive and then platinum-resistant recurrent EOC [19]. Like the FDA, the latter is limited to second and third lines only (Figure 1). Although the frontline EMA approval of bevacizumab includes the treatment of advanced (FIGO stages IIIB, IIIC, and IV) EOC for a maximum of 15 months at 15 mg/kg of body weight given once every 3 weeks, the recommendation by the European Society of Medical Oncology (ESMO) is based on the ‘high risk population’ in ICON 7 [20]. In these patients with advanced EOC and poor prognostic features, such as stage IV or suboptimal debulking, bevacizumab treatment duration is for 1 year at 7.5 mg/kg every 3 weeks. This is similar to the usage in the UK as per the Cancer Drug Fund [21]. The optimal duration of frontline bevacizumab, 12, 15 months or even longer, 30 months, is undergoing prospective evaluation (ClinicalTrials.gov Identifier: NCT01462890).
Figure 1.
Discrepancy between the European Medicines Agency (EMA) and the US Food and Drug Agency (FDA): ovarian cancer indications for bevacizumab.
Bevacizumab is a level 2A recommendation by the National Comprehensive Cancer Network (NCCN) both as a single agent in platinum-sensitive or -resistant disease (as per GOG protocol 170-D) and with chemotherapy in platinum-resistant recurrent cancer (as per AURELIA). It is a level 2B in platinum-sensitive relapsed cancer (as per OCEANS) and level 3 in frontline (as per ICON-7 and GOG protocol 218) [22].
There is a move away from incremental cost-effectiveness ratios (ICERs) [23] to a more ‘value’-based assessments in defining clinical benefit in oncology [24]. Recently, ESMO published the ESMO Magnitude of Clinical Benefit Scale (ESMO-MCBS) to stratify the magnitude of clinical benefit that can be anticipated from anti-cancer therapies [25]. This tool uses a ‘rational, structured, and consistent approach’ that addresses the critical public policy issue of value in cancer care, helping to frame the appropriate use of limited public and personal resources to deliver cost-effective and affordable cancer care. According to their recommendations, non-curative therapies rated as 4 and 5 should be highlighted for accelerated assessment of value and cost-effectiveness. Using the ESMO-MCBS scale, AURELIA, OCEANS, GOG protocol 218, and the high-risk ICON7 population achieved ratings of 4, 3, 3, and 1, respectively.
toxicity and adverse events
Clearly, the benefits of anti-VEGF therapy such as bevacizumab must be carefully weighed against the associated toxicity and attributable adverse events (AEs) seen in clinical trials. Bevacizumab carries three ‘boxed warnings’ [26]: gastrointestinal (GI) perforation [27], surgery and wound-healing complications, and hemorrhage. Additional serious and sometimes fatal AEs with increased incidence in the bevacizumab-treated arm versus control in clinical trials include: GI fistulae, non-GI fistulae, arterial thromboembolic events, proteinuria [28], venous thromboembolism, hypertension, and posterior reversible encephalopathy syndrome. Even pain, hoarseness, and marrow suppression have also been documented. The FDA ‘Label’ says to ‘Avoid use in patients with ovarian cancer who have evidence of recto-sigmoid involvement by pelvic examination or bowel involvement on CT scan or clinical symptoms of bowel obstruction’. Across all tumor types, bevacizumab was discontinued in 8.4%–21% of patients because of adverse reactions [26].
mechanisms of resistance and biomarkers
Given the cost, potential for toxicity, and finding that only a subset of patients will benefit from these drugs, a better understanding of the mechanisms of bevacizumab resistance and identification of predictive biomarkers is critical. The exact mechanisms of adaptive escape from anti-angiogenesis therapy and resistance to VEGF are unknown but may be related to activation or up-regulation of alternative pro-angiogenic pathways within the tumor [Angiopoietin 1 (Ang 1), Delta-like ligand 4/Notch, and microRNAs], immune response such as recruitment of pro-angiogenic monocytes from the bone marrow, induction of hypoxia, or increased pericyte coverage of the tumor vasculature [6]. In addition, there appears to be an immune molecular subgroup of ovarian cancer that has repressed angiogenesis-related gene expression. This subgroup has improved survival, but the addition of bevacizumab to chemotherapy appeared to significantly reduce PFS and OS compared with chemotherapy alone. These data suggest that patient stratification to identify who will benefit from drugs such as bevacizumab should be considered [29].
Several other candidate biomarkers have been proposed such as plasma protein levels, circulating endothelial cells, and cell-free DNA, but none have been validated [30]. In ICON7, the combined values of circulating Ang1 and Tie2 (tunica internal endothelial cell kinase 2) concentrations predicted improved PFS in bevacizumab-treated patients in a training set. Using median concentrations as cutoffs, high Ang1/low Tie2 values were associated with significantly improved PFS for bevacizumab-treated patients in both datasets (median, 23.0 versus 16.2 months; P = 0.003). The prognostic indices derived from the training set also distinguished high and low probability for progression in the validation set (P = 0.008), generating similar values for HR (0.21 versus 0.27) between treatment and control arms for patients with high Ang1 and low Tie2 values. These findings need to be validated in larger trials due to the limitation of sample size in this study [31]. The most intriguing predictive biomarker is imaging [32]. GOG protocol 262/ACRIN 6695 evaluated CT perfusion as an early biomarker of treatment efficacy in advanced ovarian cancer. There was a significant association between changes in tumor blood flow within 4 weeks of initiating therapy with bevacizumab and 6-month PFS and time to progression [33]. The identification of the mechanisms of resistance to bevacizumab and predictive biomarkers remain an urgent unmet medical need in treating EOC.
novel combinations
One strategy to overcome resistance to bevacizumab as well as enhancing its activity is to combine it with other targeted therapies, although this is potentially limited by adding additional toxicities and cost. However, novel rationale combinations hold great promise in enhancing the efficacy of bevacizumab.
fosbretabulin
Newer anti-angiogenesis as well as agents like VDAs that target existing blood vessels are in development and combine well with bevacizumab. In contrast to anti-angiogenesis agents that target VEGF/VEGFR and angiopoietin, VDAs target existing tumor vascular rather than preventing neovascularization. Tumor vessels can be selectively targeted by VDAs because the newly formed endothelial cells associated with cancer progression lack smooth muscle and pericyte coverage thereby relying more on intracellular tubulin to maintain their flat tube-like shape in vessel walls. VDAs that inhibit cancer-associated endothelial cell tubulin cause the affected endothelial cells to ‘round up’, thereby obstructing tumor-associated blood vessel lumens. This causes vessel collapse and obstruction. Finally, non-tumor-associated blood vessels are relatively resistant to VDAs not only because of increased amounts of endothelial cell smooth muscle but also because of increased endothelial pericyte coverage allowing them to maintain their shape when exposed to VDAs.
Interestingly, cells on the periphery of solid tumors are also relatively insensitive to VDA-induced vascular shutdown. This resistant peripheral rim of tumor cells contributes to tumor regeneration, metastasis, and ongoing progression after VDA exposure. The induced hypoxic environment also induces an intense VEGF milieu in the peripheral microenvironment. Conceptually, combining VDAs with anti-angiogenesis compounds such as bevacizumab might overcome this ‘regrowth’ phenomenon.
Combretastatin A4 (CA4) is a VDA originally isolated from the African bush willow (Combretum caffrum). Fosbretabulin is a water-soluble prodrug of cis-combretastatin A4 (cis-CA4) otherwise known as combretastatin A4 mono-tri-phosphate (abbreviated in the literature as CA4P). Fosbretabulin is a small molecule that acts as a potent and reversible tubulin depolymerizing agent. Preclinical models have shown that fosbretabulin results in massive acute vascular collapse as early as 2 h after administration with recovery as soon as 24 h providing further rationale for combining it with bevacizumab. In a phase I study of the combination of fosbretabulin plus bevacizumab, the dose-limiting toxicity appeared to be hypertension with the maximum tolerated dose of fosbretabulin being 63 mg/m2 every other week. Importantly, this study showed dynamic contrast-enhanced diffusion-weighted MRI evidence of profound vascular changes associated with fosbretabulin administration which were only sustained following bevacizumab [34]. In a recent randomized phase II study in recurrent ovarian cancer [35], the combination of bevacizumab plus fosbretabulin improved PFS compared with bevacizumab alone [HR = 0.685 (90% CI 0.47–1.00)]. The proportion responding to bevacizumab was 28.2% (90% CI 16.7–42.3%) among 39 patients with measurable disease and 35.7% (90% CI 23.5–49.5%) among 42 patients treated with the combination. Phase III trials of this novel non-cytotoxic chemotherapy combination of bevacizumab with fosbretabulin are in development.
poly (ADP-ribose) polymerase inhibitors
Preclinical studies suggest that anti-angiogenics and poly (ADP-ribose) polymerase (PARP) inhibitors are synergistic likely owing to impaired homologous recombination under tumor hypoxia. Additionally, they can be combined at full doses, which is unusual for two clinically active agents [36]. A recently reported randomized, open label, phase II trial compared the activity of olaparib (oral PARP inhibitor) alone with combined cediranib [an oral potent inhibitor of VEGF receptor tyrosine kinases (TKI)] and olaparib in recurrent platinum-sensitive high-grade serous EOC [37]. The median PFS was 9.0 months for olaparib and 17.7 months for cediranib plus olaparib [HR = 2.9 (95% CI 1.5–5.6); P = 0.001]. There were 2 complete responses and 21 partial responses in subjects on olaparib [56% objective response rate (ORR)] and 3 complete responses and 33 partial responses in patients on cediranib plus olaparib (84% ORR, P = 0.008). Less treatment effect between the two arms was seen among patients carrying a BRCA mutation. The overall rate of grade 3/4 toxicity was higher for patients on cediranib plus olaparib (70%) than on olaparib (7%). Differentially occurring toxicities included fatigue (27% cediranib plus olaparib versus 7% olaparib), diarrhea (23% versus 0%), and hypertension (39% versus 0%) [22]. This combination also deserves phase III study, but toxicity might be problematic. Adding olaparib to bevacizumab in frontline maintenance is also being studied in the PAOLA-1 phase III randomized clinical trial (ClinicalTrials.gov Identifier: NCT02477644).
immune check point inhibitors
Immunotherapy is perhaps the most robust area of clinical discovery at the current time in EOC. Programed death-1 (PD-1), a co-inhibitory immune signal receptor expressed in T cells, binds to PD-1 ligand (PD-L1) and regulates antitumor immunity. Early phase II data show promising efficacy of anti-PD-1 and anti-PDL-1 in EOC. Preclinical and early phase clinical trial data also provide the rationale for the addition of the anti-PD-L1 or PD-1 agents to PLD and bevacizumab [38]. In addition to being a mutagenic cytotoxic, doxorubicin is known to exert its antitumor effects in part through interferon signaling [39]. VEGF blockade may increase T-cell trafficking to tumors, increase antitumor populations of T cells (CD8+ and CD4+ central memory), and decrease pro-tumor immune populations (myeloid-derived suppressor cells and regulatory T cells) [40]. There is also evidence that tumor-associated macrophages are recruited to the microenvironment leading to angiogenesis escape and this would be another reason to combine these agents. Therefore, randomized trials of combinations of anti-angiogenics and immune checkpoint inhibitors are imminent.
other agents that target the VEGF/VEGFR pathway
Compounds targeting receptor tyrosine kinsases have shown promise in early phase trials, with several advancing to phase III clinical trials in EOC. These differ from bevacizumab in that they engage multiple targets. Although appealing, broader target engagement may be associated with additional toxicity compared with agents such as bevacizumab that only targets VEGF. Additionally, TKIs are generally administered orally lending in increased convenience but are associated with inconsistent bioavailability and inflexibility in dosing (Table 2).
Table 2.
Targets of tyrosine kinase inhibitors studied in phase III clinical trials in epithelial ovarian cancer
| Agent | Route of administration | Targets |
|---|---|---|
| Nintedanib | Oral | VEGFR, FGFR, and PDGFR |
| Pazopanib | Oral | VEGFR, PDGFR, FGFR, c-Kit, and c-Fms |
| Cediranib | Oral | VEGFR |
VEGFR, vascular endothelial growth factor receptor; FGFR, fibroblast growth factor receptor; PDGFR, platelet-derived growth factor receptor.
nintedanib
Nintedanib is a TKI that inhibits VEGFR, FGFR, and PDGFR. OVAR-12 was a phase III trial evaluating nintedanib in combination with carboplatin and paclitaxel followed by nintedanib maintenance in the up-front setting [41]. PFS was significantly improved with the addition of nintedanib [median = 17.2 months (95% CI 16.6–19.9) versus 16.6 months (13.9–19.1); HR = 0.84 (95% CI 0.72–0.98); P = 0.024]. Curiously, the PFS seemed to be most improved among patients in the low-risk group with small residual tumors after surgery. Serious AEs were reported in 376 (42%) of 902 patients in the nintedanib group and 155 (34%) of 450 in the placebo group. The most common AEs were GI [diarrhea: nintedanib group 191 (21%) of 902 grade 3 and 3 (<1%) grade 4 versus placebo group 9 (2%) of 450 grade 3 only].
pazopanib
Pazopanib is a TKI that inhibits VEGFR, PDGFR, c-Kit, and minimally c-fms. OVAR-16, a phase III trial evaluating pazopanib maintenance after first-line chemotherapy in patients with stage II–IV ovarian cancer, demonstrated a significant improvement in PFS [HR = 0.77 (95% CI 0.64–0.91); P = 0.0021; median, 17.9 versus 12.3 months, respectively] [42]. Interim survival analysis based on events in 35.6% of the population did not show any significant difference. Grade 3 or 4 AEs of hypertension (30.8%), neutropenia (9.9%), liver-related toxicity (9.4%), diarrhea (8.2%), fatigue (2.7%), thrombocytopenia (2.5%), and palmar-plantar erythrodysesthesia (1.9%) were significantly higher in the pazopanib arm. Treatment discontinuation related to AEs was higher among patients treated with pazopanib (33.3%) compared with placebo (5.6%) (Table 3).
Table 3.
Phase III studies of anti-angiogenic agents targeting receptor tyrosine kinases in epithelial ovarian cancer
| Study | Targeting agent | Setting | n | Treatment arm | PFS (median, months) | PFS, HR (95%CI) | OS (median, months) | OS, HR (95% CI) |
|---|---|---|---|---|---|---|---|---|
| OVAR12 [41] | Nintedanib | Frontline and maintenance | 1366 | I: paclitaxel + carboplatin + placebo; placebo maintenance | 16.6 | 0.84 (0.72–0.98) | Not stated | – |
| II: paclitaxel + carboplatin + nintedanib; nintedanib maintenance | 17.3 | 0.84 (0.72–0.98) | Not stated | – | ||||
| OVAR16 [42] | Pazopanib | Maintenance | 940 | I: placebo | 12.3 | – | 49a | – |
| II: pazopanib | 17.9 | 0.77 (0.64–0.91) | Not reached | 1.08 (0.87–1.33) | ||||
| ICON6 [18] | Cediranib | Recurrent, platinum-sensitive | 486 | I: chemotherapy (paclitaxel or gemcitabine combination) or single-agent carboplatin + placebo; placebo maintenance | 8.7 | – | 20.3 | – |
| II: chemotherapy + cediranib; placebo maintenance | 10.1 | 0.67 (0.53–0.87) | Not stated | – | ||||
| III: chemotherapy + cediranib; cediranib maintenance | 11.1 | 0.57 (0.44–0.74) | 26.3 | 0.70 (0.51–0.99) |
PFS, Progression-Free Survival; OS, Overall Survival; HR, Hazard Ratios; aestimated from publication.
The treatment effect of maintenance pazopanib in East Asian patients seemed to differ from that in non-Asian patients. In study-specific and pooled analyses, none of the potential factors analyzed could satisfactorily explain the different efficacy results of pazopanib in East Asian patients [43].
cediranib
Cediranib is a potent TKI that inhibits VEGFR and has show activity in both phase II [44] and phase III [18] studies. ICON6 was a randomized, double-blind, three-arm phase III trial of cediranib in patients with platinum-sensitive recurrent ovarian cancer. Data presented at the 2013 ESMO annual meeting indicated a significant improvement in PFS in the cediranib maintenance arm relative to control [12.5 versus 9.4 months; HR= 0.57 (95% CI 0.45–0.74), P = 0.00001]. Additionally, a 2.7-month improvement in OS was identified in the cediranib plus platinum-based chemotherapy followed by maintenance cediranib arm. Although cediranib led to an increased OS, there is no evidence to suggest it is more active than other anti-angiogenesis agents. Post-progression therapy informs post-progression survival and is probably not uniform due to emerging therapies and practice patterns in different countries. ICON6 is the first trial to demonstrate a suggested improvement in both PFS and OS using an oral VEGFR tyrosine kinase inhibitor in ovarian cancer. The most common cediranib-related AEs included diarrhea, nausea, and fatigue.
non-VEGF/VEGFR targets of angiogenesis
trebananib
The Ang-Tie pathway is of particular interest due to its critical role in blood vessel formation. Angiopoietin-1 (Ang1) and -2 (Ang2) interact with the Tie2 receptor, which is expressed on endothelial cells, to mediate vascular remodeling in a signaling pathway that is distinct from the VEGF axis. Ang1 promotes vessel stabilization by increasing endothelial junctions and pericyte coverage; Ang2 blocks Ang1's blood vessel stabilizing action, increasing angiogenesis and vascularity in tumors. Trebananib (formerly known as AMG 386; Amgen Inc.) is a peptide-Fc fusion protein (or peptibody) that acts by binding both Ang 1 and Ang2, thus preventing their interaction with the Tie2 receptor. Trebananib has shown anti-angiogenesis activity in preclinical models of ovarian cancer, single-agent activity in relapsed ovarian cancer in phase I study as well as prolongation of PFS in randomized phase II and III trials in recurrent EOC [45]. In contrast to anti-VEGF/VEGRF agents, trebananib has not been associated with an increase in typical class-related anti-VEGF/VEGFR toxicities. Its most significant toxicity has been reported to be edema [46]. The results of Trebananib in Ovarian Cancer-1 (TRINOVA-1), a 919 subject randomized placebo-controlled phase III trial investigating the addition of trebananib to single-agent weekly paclitaxel in relapsed EOC, showed a PFS improvement of 52% (Cox's model HR = 0.66; 95% CI 0.56–0.76; P < 0.001) from a median of 5.4 (95% CI 4.3–5.5) to 7.2 months (95% CI 5.8–7.4). Other randomized studies of trebananib ovarian cancer are ongoing.
conclusions
Almost all patients with EOC will receive an anti-angiogenic compound. However, the ability to identify those most likely to benefit is lacking and these interventions remain expensive with the benefits only being modest. Cures are not increased. Additionally, they are associated with significant toxicity with oral TKIs being even more toxic than bevacizumab. However, there is reason for optimism as combinations, biosimilars, and predictive biomarkers emerge.
funding
RLC is supported in part by the Ann Rife Cox Chair in Gynecology, the Judy Reis (Al Pisani) Ovarian Cancer Research Fund, and grants CPRIT RP120214 and P50CA083639.
disclosure
BJM discloses that his institution has received research grants from Lilly, Genentech, and Janssen/Johnson & Johnson. He also discloses that he has received honoraria for speaker bureaus from Roche/Genentech and AstraZeneca. Additionally, BJM has been a consultant for Roche/Genentech, AstraZeneca, and Amgen. RLC discloses research grants from Roche/Genentech, Janssen/Johnson& Johnson, Clovis, AstraZeneca, Novartis, Array, and Esperance. LEM declares no conflicts of interest.
acknowledgements
The authors would like to thank Daniele Sumner, BA for her assistance with administrative support. The authors are solely responsible for the preparation and content of the manuscript.
references
- 1. Coleman RL, Monk BJ, Sood AK, Herzog TJ. Latest research and treatment of advanced-stage epithelial ovarian cancer. Nat Rev Clin Oncol 2013; 10: 211–224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. ten Bokkel Huinink W, Lane SR, Ross GA. International Topotecan Study Group. Long-term survival in a phase III, randomised study of topotecan versus paclitaxel in advanced epithelial ovarian carcinoma. Ann Oncol 2004; 15: 100–103. [DOI] [PubMed] [Google Scholar]
- 3. Gordon AN, Tonda M, Sun S, Rackoff W. Doxil Study 30-49 Investigators. Long-term survival advantage for women treated with pegylated liposomal doxorubicin compared with topotecan in a phase 3 randomized study of recurrent and refractory epithelial ovarian cancer. Gynecol Oncol 2004; 95: 1–8. [DOI] [PubMed] [Google Scholar]
- 4. Monk BJ, Herzog TJ, Kaye SB et al. Trabectedin plus pegylated liposomal doxorubicin in recurrent ovarian cancer. J Clin Oncol 2010; 28(19): 3107–3114. [DOI] [PubMed] [Google Scholar]
- 5. US Food and Drug Administration. Bevacizumab solution in combination with paclitaxel. http://www.fda.gov/Drugs/InformationOnDrugs/ApprovedDrugs/ucm423159.htm (20 November 2015, date last accessed).
- 6. Graybill W, Sood AK, Monk BJ, Coleman RL. State of the science: emerging therapeutic strategies for targeting angiogenesis in ovarian cancer. Gynecol Oncol 2015; 138: 223–226. [DOI] [PubMed] [Google Scholar]
- 7. Mabuchi S, Terai Y, Morishige K et al. Maintenance treatment with bevacizumab prolongs survival in an in vivo ovarian cancer model. Clin Cancer Res 2008; 14: 7781–7789. [DOI] [PubMed] [Google Scholar]
- 8. Monk BJ, Choi DC, Pugmire G, Burger RA. Activity of bevacizumab (rhuMAB VEGF) in advanced refractory epithelial ovarian cancer. Gynecol Oncol 2005; 96: 902–905. [DOI] [PubMed] [Google Scholar]
- 9. Monk BJ, Han E, Josephs-Cowan CA et al. Salvage bevacizumab (rhuMAB VEGF)-based therapy after multiple prior cytotoxic regimens in advanced refractory epithelial ovarian cancer. Gynecol Oncol 2006; 102: 140–144. [DOI] [PubMed] [Google Scholar]
- 10. Burger RA, Sill MW, Monk BJ et al. Phase II trial of bevacizumab in persistent or recurrent epithelial ovarian cancer or primary peritoneal cancer: a Gynecologic Oncology Group Study. J Clin Oncol 2007; 25: 5165–5171. [DOI] [PubMed] [Google Scholar]
- 11. Burger RA, Brady MF, Bookman MA et al. Gynecologic Oncology Group. Incorporation of bevacizumab in the primary treatment of ovarian cancer. N Engl J Med 2011; 365: 2473–2483. [DOI] [PubMed] [Google Scholar]
- 12. Perren TJ, Swart AM, Pfisterer J et al. ICON7 Investigators. A phase 3 trial of bevacizumab in ovarian cancer. N Engl J Med 2011; 365: 2484–2496. [DOI] [PubMed] [Google Scholar]
- 13. Pujade-Lauraine E, Hilpert F, Weber B et al. AURELIA: a randomized phase III trial evaluating bevacizumab (BEV) plus chemotherapy (CT) for platinum (PT)-resistant recurrent ovarian cancer (OC). J Clin Oncol 2012; 30(suppl): abstr LBA5002. [Google Scholar]
- 14. Aghajanian C, Blank SV, Goff BA et al. OCEANS: a randomized, double-blind, placebo-controlled phase III trial of chemotherapy with or without bevacizumab in patients with platinum-sensitive recurrent epithelial ovarian, primary peritoneal, or fallopian tube cancer. J Clin Oncol 2012; 30: 2039–2045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Oza AM, Cook AD, Pfisterer J et al. ICON7 Trial Investigators. Standard chemotherapy with or without bevacizumab for women with newly diagnosed ovarian cancer (ICON7): overall survival results of a phase 3 randomised trial. Lancet Oncol 2015; 16: 928–936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Randall LM, Burger RA, Nguyen H et al. Outcome differences in patients with stage IV epithelial ovarian, primary peritoneal and fallopian tube cancers treated with and without bevacizumab. In 44th Annual Meeting of the Society of Gynecologic Oncology, Los Angeles, CA, 2013. [Google Scholar]
- 17. Coleman RL, Brady MF, Herzog TJ et al. A Phase III randomized controlled clinical trial of carboplatin and paclitaxel alone or in combination with bevacizumab followed by bevacizumab and secondary cytoreductive surgery in platinum-sensitive, recurrent ovarian, peritoneal primary and fallopian tube cancer (Gynecologic Oncology Group 213). In 46th Annual Meeting of the Society of Gynecologic Oncology, Chicago, IL, 2015. [Google Scholar]
- 18. Ledermann JA, Perren TJ, Raja FA et al. Randomised double-blind phase III trial of cediranib (AZD 2171) in relapsed platinum sensitive ovarian cancer: results of the ICON6 trial. Eur J Cancer 2013; 49: (suppl 3):abstr LBA10. [Google Scholar]
- 19. European Medicines Agency. Science Medicines Health. Avastin http://www.ema.europa.eu/ema/index.jsp?curl=pages/medicines/human/medicines/000582/human_med_000663.jsp&mid=WC0b01ac058001d124 (20 November 2015, date last accessed).
- 20. Ledermann JA, Raja FA, Fotopoulou C et al. Newly diagnosed and relapsed epithelial ovarian carcinoma: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 2013; 24(Suppl 6): vi24–vi32. [DOI] [PubMed] [Google Scholar]
- 21. NHS England. Cancer Drug Fund decision summaries. https://www.england.nhs.uk/ourwork/cancer/cdf/cdf-drug-sum/ (20 November 2015, date last accessed).
- 22. National Comprehensive Cancer Network. http://www.nccn.org (21 November 2015, date last accessed).
- 23. Cohn DE, Kim KH, Resnick KE et al. At what cost does a potential survival advantage of bevacizumab make sense for the primary treatment of ovarian cancer? A cost-effectiveness analysis. J Clin Oncol 2011; 29: 1247–1251. [DOI] [PubMed] [Google Scholar]
- 24. Young RC. Value-based cancer care. N Engl J Med 2015; 373: 2593–2595. [DOI] [PubMed] [Google Scholar]
- 25. Cherny NI, Sullivan R, Dafni U et al. A standardised, generic, validated approach to stratify the magnitude of clinical benefit that can be anticipated from anti-cancer therapies: the European Society for Medical Oncology Magnitude of Clinical Benefit Scale (ESMO-MCBS). Ann Oncol 2015; 26: 1547–1573. [DOI] [PubMed] [Google Scholar]
- 26. Genentech, Inc. Avastin®, Bevacizumab, Clinically meaningful activity in 6 distinct tumor types. http://www.avastin-hcp.com (23 November 2015, date last accessed).
- 27. Han ES, Monk BJ. What is the risk of bowel perforation associated with bevacizumab therapy in ovarian cancer? Gynecol Oncol 2007; 105: 3–6. [DOI] [PubMed] [Google Scholar]
- 28. Hayman SR, Leung N, Grande JP, Garovic VD. VEGF inhibition, hypertension, and renal toxicity. Curr Oncol Rep 2012; 14: 285–294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Gourley C, McCavigan A, Perren T et al. Molecular subgroup of high-grade serous ovarian cancer (HGSOC) as a predictor of outcome following bevacizumab. J Clin Oncol 2014; 32:5s(suppl): abstr 5502. [Google Scholar]
- 30. Han ES, Burger RA, Darcy KM et al. Predictive and prognostic angiogenic markers in a gynecologic oncology group phase II trial of bevacizumab in recurrent and persistent ovarian or peritoneal cancer. Gynecol Oncol 2010; 119: 484–490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Backen A, Renehan AG, Clamp AR et al. The combination of circulating Ang1 and Tie2 levels predicts progression-free survival advantage in bevacizumab-treated patients with ovarian cancer. Clin Cancer Res 2014; 20: 4549–4558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Chase DM, Sill MW, Monk BJ et al. Changes in tumor blood flow as measured by dynamic contrast-enhanced magnetic resonance imaging (DCE-MRI) may predict activity of single agent bevacizumab in recurrent epithelial ovarian (EOC) and primary peritoneal cancer (PPC) patients: an exploratory analysis of a Gynecologic Oncology Group Phase II study. Gynecol Oncol 2012; 126: 375–380. [DOI] [PubMed] [Google Scholar]
- 33. Lee TY, Ng CS, Zhang Z et al. CT perfusion as an early biomarker of treatment efficacy in advanced ovarian cancer: an ECOG-ACRIN and NRG GOG study. J Clin Oncol 2015; 33(suppl):abstr 5522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Nathan P, Zweifel M, Padhani AR et al. Phase I trial of combretastatin A4 phosphate (CA4P) in combination with bevacizumab in patients with advanced cancer. Clin Cancer Res 2012; 18: 3428–3439. [DOI] [PubMed] [Google Scholar]
- 35. Monk B, Sill M, Walker J et al. Randomized Phase 2 evaluation of bevacizumab versus bevacizumab/fosbretabulin in recurrent ovarian, tubal or peritoneal carcinoma: a Gynecologic Oncology Group Study. In 15th Biennial Meeting of the International Gynecologic Cancer Society, Melbourne, Australia, November2014. [Google Scholar]
- 36. Dean E, Middleton MR, Pwint T et al. Phase I study to assess the safety and tolerability of olaparib in combination with bevacizumab in patients with advanced solid tumours. Br J Cancer 2012; 106: 468–474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Liu JF, Barry WT, Birrer M et al. Combination cediranib and olaparib versus olaparib alone for women with recurrent platinum-sensitive ovarian cancer: a randomised phase 2 study. Lancet Oncol 2014; 15: 1207–1214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. De Felice F, Marchetti C, Palaia I et al. Immunotherapy of ovarian cancer: the role of checkpoint inhibitors. J Immunol Res 2015; 2015: 191832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Sistigu A, Yamazaki T, Vacchelli E et al. Cancer cell-autonomous contribution of type I interferon signaling to the efficacy of chemotherapy. Nat Med 2014; 20: 1301–1309. [DOI] [PubMed] [Google Scholar]
- 40. Kusmartsev S, Eruslanov E, Kübler H et al. Oxidative stress regulates expression of VEGFR1 in myeloid cells: link to tumor-induced immune suppression in renal cell carcinoma. J Immunol 2008; 181: 346–353. [DOI] [PubMed] [Google Scholar]
- 41. Bois AD, Kristensen G, Ray-Coquard I et al. AGO Study Group led Gynecologic Cancer Intergroup (GCIG)/European Network of Gynaecologic Oncology Trials Groups (ENGOT) Intergroup Consortium. Standard first-line chemotherapy with or without nintedanib for advanced ovarian cancer (AGO-OVAR 12): a randomised, double-blind, placebo-controlled phase 3 trial. Lancet Oncol 2015(Epub ahead of print), pii: S1470-2045(15)00366-6. [DOI] [PubMed] [Google Scholar]
- 42. du Bois A, Floquet A, Kim JW, Rau J et al. Incorporation of pazopanib in maintenance therapy of ovarian cancer. Clin Oncol 2014; 32: 3374–3382. [DOI] [PubMed] [Google Scholar]
- 43. Kim JW, Mahner S, Wu LY et al. Pazopanib maintenance therapy in east Asian women with advanced epithelial ovarian cancer: results from AGO-OVAR16 and an East Asian Study. Int J Gynecol Cancer 2015(Epub ahead of print). [DOI] [PubMed] [Google Scholar]
- 44. Hirte H, Lheureux S, Fleming GF et al. A phase 2 study of cediranib in recurrent or persistent ovarian, peritoneal or fallopian tube cancer: a trial of the Princess Margaret, Chicago and California Phase II Consortia. Gynecol Oncol 2015; 138: 55–61. [DOI] [PubMed] [Google Scholar]
- 45. Monk BJ, Poveda A, Vergote I et al. Anti-angiopoietin therapy with trebananib for recurrent ovarian cancer (TRINOVA-1): a randomised, multicentre, double-blind, placebo-controlled phase 3 trial. Lancet Oncol 2014; 15: 799–808. [DOI] [PubMed] [Google Scholar]
- 46. Monk BJ, Lambrechts S, Minion L et al. Incidence and management of edema associated with trebananib (AMG 386). Gynecol Oncol 2013; 130: 636–641. [DOI] [PubMed] [Google Scholar]