Abstract.
Early names for leptospirosis often indicate occupational or environmental exposure. Leptospirosis is hard to identify in the tropical setting because of co-circulating diseases. This is not the case in the temperate setting, such as Europe, where the few historical differential diagnoses were malaria, typhoid, and viral hepatitis. Leptospirosis presumably caused community epidemics in Europe before 1900 and military epidemiologists carefully documented outbreaks in “constrained settings.” Achille Kelsch (1841–1911) synthesized available military data and epidemiological perspectives to define “epidemic jaundice” as a nosological continuum, caused by an infectious agent found in muds and water. He viewed Weil’s disease as being only one form of that now well-identified disease continuum. The causative pathogen and epidemiological determinants were identified years later. The role of soils and muds as intermediate reservoirs, as suggested by Kelsch, deserves further investigation.
Leptospirosis is a complex disease caused by a spirochete. The clinical entity1 and causative infectious agent of leptospirosis were identified at the turn of the previous century, but these had long been circulating and identified in a classic case of “disease emergence,” descriptions being rather an “unveiling” and the structuration of a disease entity.
Although infections and outbreaks were well described, identifying a disease complex or entity is challenging when many names are used. Many of those names, however, bore the notion of behavior, occupation, or seasonality: “rat-catcher yellows”; “cane-cutter’s disease”; “pea-picker’s disease”; “harvest fever”; “rice/paddy field jaundice”; “maladie des éboueurs” (sewage workers’ disease); or “schlammfieber” (“slime fever”).2,3
Leptospirosis is difficult to identify in the tropical setting, where many other diseases with similar initial presentation co-circulate: dengue; Hepatitis A; yellow fever; schistosomiasis (Bilharzia); or blackwater fever (malaria).4 Before becoming a neglected tropical disease, however, leptospirosis was a public health concern in now-developed countries. The French Royal Society of Medicine received 80 communications on “bilious epidemics” in France from 1782 to 1784 alone, many of which may have been leptospirosis outbreaks.5 In the absence of endemic yellow fever in Europe, the principal differential diagnoses in leptospirosis outbreaks were malaria, typhoid, and viral hepatitis A. Clinicians, however, knew the febrile cycles associated with malaria well and routinely used the bark of cinchona, including in febrile jaundice cases.6 Typhoid was similarly lethal in the pre-antibiotic age but rarely associated with jaundice.7 The issue of viral hepatitis is more complex, but this was a widespread, benign childhood disease before public hygiene improved, with most infections remaining symptom-free.8 At the end of the 20th century, anti-hepatitis A virus seroprevalence remained high in European populations, with antibody prevalence of approximately 50% around age the of 20 in Spain and around age 40 in the Czech Republic.9 The prevalence of protective antibodies in young adults was likely much higher in the 19th century when most French inmates or soldiers described in the following paragraphs, would have been born and raised on farms or in urban slums. Moreover, oliguria is rarely documented in nonfulminant type A hepatitis.10
In temperate settings, leptospires may have caused a devastating outbreak among Patuxet (Plimouth) Indians in New England in the early 17th C3,11 or in Minorca in 1745.12 Ozanam (1773–1837) mentioned community outbreaks of “epidemic jaundice” in Berlin in 1699 and 1702, in Hungary in 1703 and 1705, in Rome in 1709, and in now-Belgium and the Netherlands in 1719.5,13 Most of the well-documented epidemiological records available on what may be considered to be leptospirosis in Europe, however, were documented by military doctors.
These forefathers of clinical epidemiology were struck by the brutal character of “epidemic jaundice” outbreaks even among healthy adults; they described environmental or occupational exposures leading to jaundice, which bore similarities to “typhoid” or “typhus” but was less lethal and not always febrile.
Sir John Pringle (1707–1782) relates the account of “epidemic jaundice” among British troops in Flanders in 1743.14 Outbreaks and their dynamics were described in Europe, for example, in now-German troops besieging Paris, causing 799 cases among 33,380 Bavarian troops stationed around Paris, in February–May 1870 with an estimated attack rate of 2.4%.5 Many other such epidemics were described elsewhere in Europe and no doubt detailed in other languages.15 But the best-described epidemics—in French medical literature at least—occurred in closed settings with documented denominators.16
E. Fritsch dit Lang (1833–1877) described epidemics among French garrisons in 1859, during the second Italian independence war against Austria. Outbreaks in garrisons in Pavia and Civitavecchia near Rome occurred among 71/1,022 troops (6.9% attack rate and no deaths) and 47 cases including 21 severe (four deaths) among stationed troops, respectively.5,6,16 The latter outbreak was associated with soldiers’ bathing in waters contaminated by sewage, one of the first mentions of a telluric origin.15
In Gaillon, France, Carville cited by Lavéran documented in 1859, a 5-month prison outbreak of 47 cases of “severe epidemic jaundice” (“ictère grave épidémique”), associating frisson, headache, extreme fatigue, oliguria in some, abdominal tenderness, and vomiting. After 6.5 days on average, the presentation progressed to jaundice, vomiting, epistaxis, hematemesis or petechiae, albuminuria, and caused 11 (23.4%) deaths.16,17
Two well-documented outbreaks with thorough clinical descriptions occurred in garrisons in and around Paris in 1865: One in May in Saint-Cloud18,19 and the other in July–August at Caserne Lourcine, in Paris.17 These epidemics were at the time attributed to drinking or exposure to biocontaminated water from uncleansed or rat-infested reservoirs. Others in Arras, France, documented “epidemic jaundice” cases in 1864, 1865, and 1867 associated in time and space with the cleansing of water reservoirs and muds.15,16
ACHILLE KELSCH’S OVERVIEW OF MILITARY DATA AND EPIDEMIOLOGICAL PERSPECTIVE
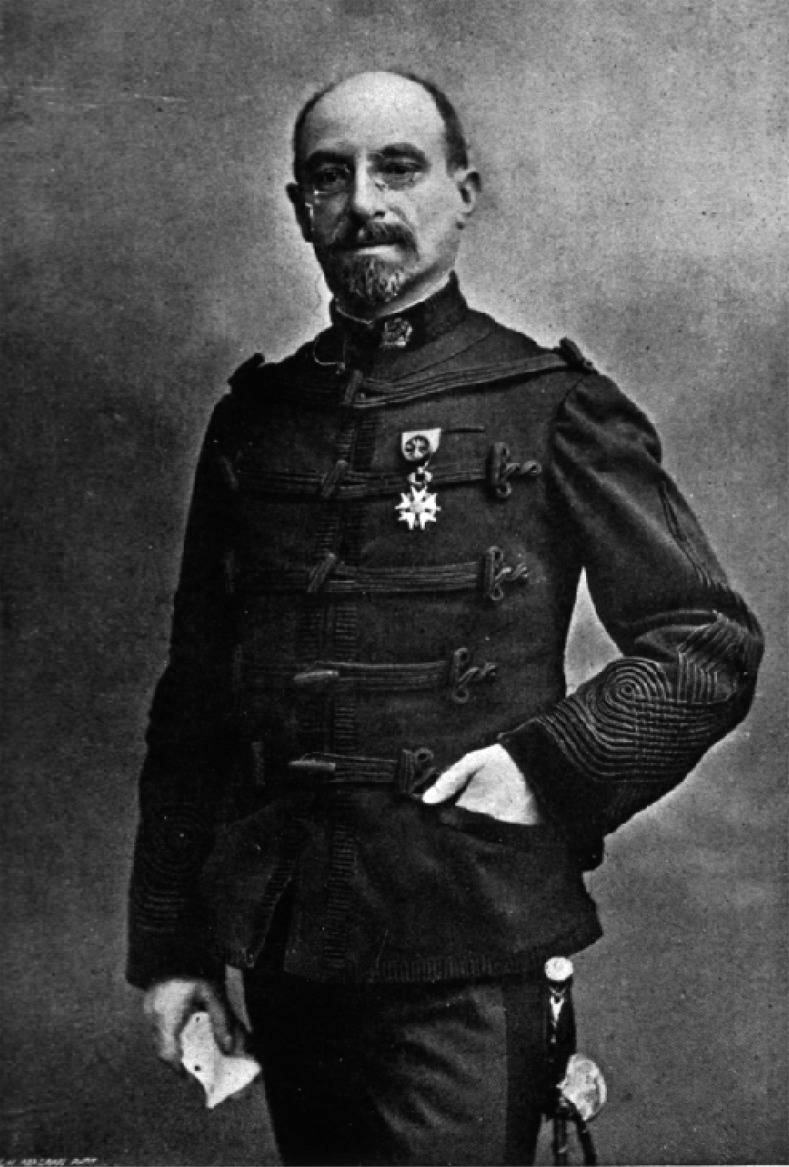
Louis Félix Achille Kelsch (1841–1911) (Figure 1) was a French military doctor and epidemiologist. A contemporary of Louis Pasteur, he was well aware of the microbial theory but resisted the notion that microbes were the sole agents of disease, his view being that these were necessary but not sufficient to cause disease, anticipating individual vulnerability and host–pathogen response.20
Figure 1.
L. F. A. Kelsch (source: U.S. National Library of Medicine Digital Collections available at https://collections.nlm.nih.gov/catalog/nlm:nlmuid-101420156-img).
Kelsch who became a professor at Val-de-Grâce—Paris’s military teaching hospital—wrote a reference textbook on diseases in the army, with a focus on “essential jaundice” (“ictère essentiel”).16,21 In the authors’ opinion, this provides one of the best and most comprehensive views of what was later identified as leptospirosis.
With first-hand field experience in Algeria in 1878, he later built on his own and many others’ knowledge5 to clinically delineate the leptospiral disease paradigm. Kelsch also noted the seasonality and the “circumscribed nature of disease,”15 thereby not ascribing outbreaks of “catarrhal jaundice” solely to seasonal factors. The following are the authors’ translation of Kelsch’s conclusions from French13:
“The two jaundices are associated: Simple jaundice is reported in severe jaundice epidemics, and vice versa; Sporadic cases of the latter sometimes occur during epidemics of ‘catarrhal jaundice’; The latter, by some attenuation of its traits, such as muscle pains, prostration, epistaxis, often reminds one of the presentation of the former; Severe jaundice has its benign forms, and simple jaundice is often marked by severe presentations […]16 The [geographically] circumscribed nature of the disease bears undoubtable witness to the [geographical] limitation of its cause,”21
Kelsch concluded:
“1) That sporadic or epidemic ‘catarrhal jaundice’ is a specific, infectious disease; 2) That the infectious agent develops outside of the body; 3) That the foci in which it generates are ponds, muds, soils rich in organic matter of animal or vegetal origin, and the waters in which these substances are in suspension; 4) That, these infectious foci being common to malaria and dothienenteria [typhoid], this explains concurrent epidemics of jaundice and intermittent fever [malaria] or typhoid which are sometimes reported.”21,22
Like L. Landouzy (1845–1917) in 1883,23,24 Adolph Weil published his detailed clinical report on what is now termed Weil’s disease in 1886, considering it to be an abortive form of “typhus” perhaps because of climatic factors.1 In his 1894 re-edition Kelsch writes:
“We do not yet know the pathogenic agent of epidemic jaundice […]. But although we remain ignorant of the essential cause, epidemiology enables us to at least delineate its origin and the conditions which underlie its development […]. In summary, the analysis of observations published to date brings us to conclude that neither clinical experience, etiology, nor anatomical pathology allow us to see Weil’s symptomatic complex as a single and undivided affliction by essence.”21
The pathogenic agent of leptospirosis was some years later identified, thanks to work by Nobel prize winners Inada and Ido25 and Wolbach,26 among others.27 The link with rats was quickly established by Ido et al.28 and Mikinosuke Miyajima (1872–1944), who in 1915 identified Spirochaeta. icterohaemorrhagiae in Fukuoka (Kyūshū, Japan) houses and coal mines, and rural rats, with suggested prophylactic measures.29 Noguchi was the first to study the survival of leptospires in various media, including soils.30 We now know that infection by pathogenic leptospires is mostly pauci- or asymptomatic and can cause a very wide range of symptoms,31 confirming “Weil’s disease” to be only one of multiple possible presentations of leptospirosis.
The role of rats and domestic animals in the epidemiology of leptospirosis is now well established. Work is currently being performed, notably at the Institut Pasteur in New Caledonia, on the diversity and persistence of Leptospira in soils, strongly supporting the intermediate, telluric reservoir of leptospirosis.32,33
As suggested by Kelsch 130 years ago in a prefiguration of Hill’s criteria34 and supported by our present knowledge on host–pathogen interactions in leptospirosis,35 the role of contaminated soils and muds as intermediate reservoir deserves to be further explored and better understood.
Acknowledgments:
The American Society of Tropical Medicine and Hygiene (ASTMH) assisted with publication expenses.
REFERENCES
- 1.Weil A, 1886. Über eine Eigenthümliche mit Milztumor, Icterus und Nephritis Einhergehende Acute Infectionskrankheit Available at: https://archive.org/stream/b2811906x/b2811906x_djvu.txt. Accessed July 3, 2018.
- 2.Faine S, Adler B, Bolin C, Perolat P, 1999. Leptospira and Leptospirosis, 2nd edition. Melbourne, Australia: MediSci. [Google Scholar]
- 3.Conover MR, Vail RM, 2015. Leptospirosis. In: Human Diseases from Wildlife. Boca Raton, FL: CRC Press, Taylor & Francis Group, 175–189. [Google Scholar]
- 4.Hem S, et al. 2016. Estimating the burden of leptospirosis among febrile subjects aged below 20 years in Kampong Cham communities, Cambodia, 2007–2009. PLoS One 11: e0151555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Seguin MPEM, 1889. Considérations Générales sur les Épidémies D’ictère Catarrhal, à Propos d’une Série de Cas Observés Dans les Troupes Casernées à Lorient en 1889 Thèze, Rochefort-sur-Mer. Available at: https://gallica.bnf.fr/ark:/12148/bpt6k5684130c. Accessed July 3, 2018.
- 6.Fritsch-Lang E, 1861. Épidémie d’Ictère Compliqué de Purpura Observée à Civita-Vecchia en Janvier 1859. Thèse, Faculté de Médecine, Université de Strasbourg.
- 7.Ogilvie G, 1901. Jaundice in typhoid fever. BMJ 1: 75–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hadler SC, Webster HM, Erben JJ, Swanson JE, Maynard JE, 1980. Hepatitis a in day-care centers. N Engl J Med 302: 1222–1227. [DOI] [PubMed] [Google Scholar]
- 9.Jacobsen KH, Koopman JS, 2004. Declining hepatitis A seroprevalence: a global review and analysis. Epidemiol Infect 132: 1005–1022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Geltner D, Naot Y, Zimhoni O, Gorbach S, Bar-Khayim Y, 1992. Acute oliguric renal failure complicating type A nonfulminant viral hepatitis. A case presentation and review of the literature. J Clin Gastroenterol 14: 160–162. [DOI] [PubMed] [Google Scholar]
- 11.Marr JS, Cathey JT, 2010. New hypothesis for cause of epidemic among native Americans, New England, 1616–1619. Emerg Infect Dis 16: 281–286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dawson B, Hume WE, Bedson SP, 1917. Infective jaundice. BMJ 2: 345–354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ozanam JAF, 1835. Histoire Médicale Générale et Particulière Des Maladies Épidémiques, Contagieuses et Épizotiques Qui Ont Régné en Europe Depuis les Temps les plus Reculés, et Notamment Depuis Le XIVe Siècle Jusqu’à Nos Jours. T1/Par J.-A.-F. Ozanam,…; 1835. Available at: https://gallica.bnf.fr/ark:/12148/bpt6k441472f. Accessed July 3, 2018.
- 14.Pringle J, Rush B, 1812. Chapter III–A general account of the diseases of the British troops, during the campaign in Germany in the year 1743; and the ensuing winter in Flanders. In: Observations on the Diseases of the Army Philadelphia, PA: Anthony Finley; Fry and Kammerer, printers. Available at: http://archive.org/details/2567047R.nlm.nih.gov. Accessed July 4, 2018.
- 15.Longuet R, 1886. L’origine tellurique de l’ictère catarrhal. Union Médicale J Intérêts Sci Prat Moraux Prof Corps Méd 1886 42: 433–438. [Google Scholar]
- 16.Marvaud A, 1894. Chapitre XIV—Les ictères. In: Les Maladies du Soldat : Étude Etiologique, Epidémiologique, Clinique et Prophylactique Paris, France: Félix Alcan, 886. Available at: https://archive.org/stream/b21927170#page/n7/mode/2up. Accessed July 3, 2018.
- 17.Laveran A, 1875. Traité des Maladies et Épidémies des Armées Paris, France: Masson. Available at: http://archive.org/details/b21356117. Accessed July 3, 2018.
- 18.Worms D, 1865. Relation de la maladie qui a régné pendant le mois de Mai 1865 sur les troupes casernées à Saint-Cloud (2). Gaz Hebd Médecine Chir 2: 533–535. [Google Scholar]
- 19.Worms D, 1865. Relation sur la maladie ictérique, qui a régné pendant le mois de mai 1865 sur les troupes casernées à Saint-Cloud (1). Gaz Hebd Médecine Chir 2: 524. [Google Scholar]
- 20.Osborne M, 1992. French military epidemiology and the limits of the laboratory: The case of Louis-Félix-Achille Kelsch. Cunningham A, Williams P, eds. The Laboratory Revolution in Medicine. Cambridge, England: Cambridge University Press, 189–208. Available at: https://www.academia.edu/12586319/_French_military_epidemiology_and_the_limits_of_the_laboratory_The_case_of_Louis-F%C3%A9lix-Achille_Kelsch_. Accessed July 4, 2018. [Google Scholar]
- 21.Kelsch A, 1894. De l’ictère essentiel. In: Traité des Maladies Épidémiques : Étiologie et Pathogénie des Maladies Infectieuses. Paris, France: Octave Doin, 178–198. Available at: https://archive.org/details/b21985091_0001. Accessed July 3, 2018. [Google Scholar]
- 22.Deschamps E, 1886. De la nature de l’ictère catarrhal, par M. Kelsch. Union Médicale J Intérêts Sci Prat Moraux Prof Corps Méd 1886: 453. [Google Scholar]
- 23.Mathieu A, 1886. Typhus hépatique bénin, rechute, guérison. Rev Médecine 6: 633–639. [Google Scholar]
- 24.Landouzy L, 1883. Typhus hépatique. Gaz Hôp Civ Mil 1883: 913–914. [Google Scholar]
- 25.Inada R, Ido Y, Hoki R, Kaneko R, Ito H, 1916. The etiology, mode of infection, and specific therapy of Weil’s disease (spirochaetosis icterohaemorrhagica). J Exp Med 23: 377–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wolbach SB, Binger CAL, 1914. Notes on a filterable spirochete from fresh water. Spirocheta biflexa (new species). J Med Res 30: 23–26.1. [PMC free article] [PubMed] [Google Scholar]
- 27.Stimson AM, 1907. Note on an organism found in yellow-fever tissue. Public Health Rep 1896-1970 22: 541–541. [Google Scholar]
- 28.Ido Y, Hoki R, Ito H, Wani H, 1917. The rat as a carrier of spirochæta icterohæmorrhagiæ, the causative agent of Weil’s disease (spirochætosis icterohæmorrhagica). J Exp Med 26: 341–353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ido Y, Hoki R, Ito H, Wani H, 1916. The prophylaxis of Weil’s disease (spirochætosis icterohæmorrhagica). J Exp Med 24: 471–483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Noguchi H, 1918. The survival of leptospira (spirochaeta) icterohaemorrhagiae in nature; observations concerning microchemical reactions and intermediary hosts. J Exp Med 27: 609–625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Felzemburgh RDM, et al. 2014. Prospective study of leptospirosis transmission in an urban slum community: role of poor environment in repeated exposures to the Leptospira agent. PLoS Negl Trop Dis 8: e2927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Thibeaux R, Girault D, Bierque E, Soupé-Gilbert M-E, Rettinger A, Douyère A, Meyer M, Iraola G, Picardeau M, Goarant C, 2018. Biodiversity of environmental leptospira: improving identification and revisiting the diagnosis. Front Microbiol 9: 816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Thibeaux R, Iraola G, Ferrés I, Bierque E, Girault D, Soupé-Gilbert ME, Picardeau M, Goarant C, 2018. Deciphering the unexplored Leptospira diversity from soils uncovers genomic evolution to virulence. Microbial Genomics 4: 000144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hill AB, 1965. The environment and disease: association or causation? Proc R Soc Med 58: 295–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mikulski M, et al. 2015. Severity markers in severe leptospirosis: a cohort study. Eur J Clin Microbiol Infect Dis 34: 687–695. [DOI] [PubMed] [Google Scholar]