Abstract
Background
Insomnia is one of the main symptoms of sleep disorders. Previous studies have suggested that alcohol intake is associated with several adverse health outcomes. The association between alcohol consumption and insomnia has been addressed in several studies with different results. However, whether gender may modify the association between alcohol consumption and insomnia is not clear. This study will focus on gender differences in the relationship between alcohol consumption and insomnia.
Methods
The final study includes 8081 subjects aged between 18 and 65 years from the Jidong cohort. The data on alcohol consumption is collected by questionnaires, and insomnia problems are assessed using the entire 8-item Athens Insomnia Scale (AIS-8). Logistic analysis is used to evaluate the association between alcohol consumption and insomnia.
Results
Among the 8081 participants in this study, 2618 (32.4%) are alcohol drinkers, including 2424 males and 194 females. The prevalence of insomnia is 9.6% in the male and 10.6% in the female. The adjusted odds ratios (ORs) with 95% confidence interval (CI) of mild-to-moderate drinkers and heavy drinkers for insomnia are 1.27 (1.02–1.58) and 1.02 (0.79–1.32), respectively. Heavy alcohol consumption is significantly correlated with insomnia in the female, after controlling for potential confounding factors (OR: 2.11, 95% CI: 1.28–3.49, p for interaction = 0.002).
Conclusion
A significant association between alcohol consumption and insomnia is found in females, but not in males from the northern Chinese population.
Introduction
Alcohol consumption has created various global public health problems. There are now nearly two billion alcohol drinkers around the world [1]. The WHO global status on alcohol and health reports that more than half of the population aged 15 years and older in China are alcohol consumers [2]. Alcohol consumption is associated with a variety of psychiatric disorders, especially depression and sleep disorders [3, 4]. Insomnia is one of the main symptoms of sleep-related disturbances, which is considered to be a common clinical condition characterized by difficulty in initiating or maintaining sleep. The prevalence of insomnia is ranging from 6% to 33% in the general population [5].
Previous studies have attempted to identify the possible modifiable factors which could potentially help people to sleep. Alcohol is used as a hypnotic to help those with insomnia to fall asleep [6]. The currently available data also suggest that sleep effects actually appear to be associated with the reinforcement effects of ethanol as a hypnotic for insomniacs [7–9]. However, some laboratory studies have reported that alcohol quickly loses its effectiveness as a hypnotic while retaining its sleep disturbing properties after following chronic consumption [10, 11]. Notably, the gender difference may alter the association between alcohol use and insomnia, and it has been extensively studied in some researches [12, 13]. For example, a study based on Brazilian subjects showed that subjective sleep disturbance was prevalent in all women (100%) and most of men (88.9%) after drinking. On the one hand, men are more likely to carry the endogenous vulnerabilities and exogenous risks that increase their sleep problems due to alcohol dependence. On the other hand, women might be more susceptible to the effects of alcohol consumption than men because of the higher blood alcohol concentrations after drinking equivalent doses of alcohol per kilogram of body weight [14, 15]. This study hereby hypothesizes that the relationship between alcohol consumption and insomnia differs from gender to gender. Therefore, the aim of this study is to investigate whether gender differences will modify the association between alcohol consumption and insomnia in the northern Chinese population.
Materials and methods
Study design and population
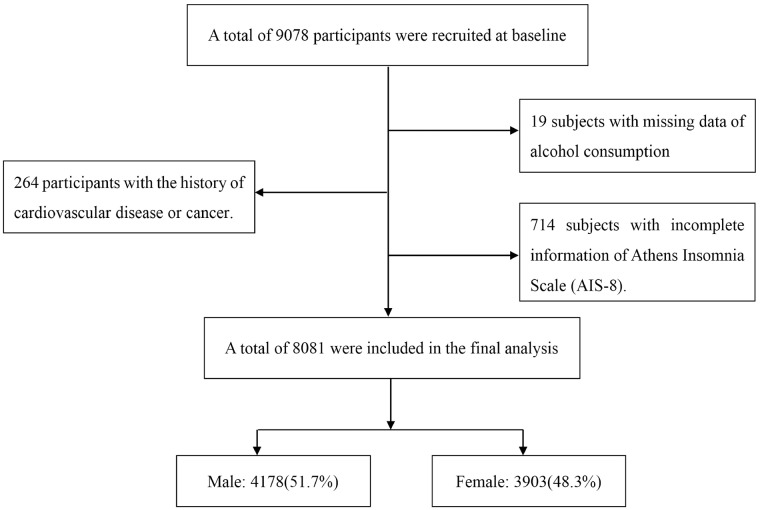
We used data from Jidong cohort, which was a community-based cohort for prospective researches on Chinese adults. Jidong community is located in Tangshan, which is a large and modern industrial city in the central section of the Bohai Rim in HeBei Province, of northern China [16]. From July 2013 to August 2014, a total of 9078 residents aged ≥ 18 years in Jidong community were recruited to participate in the study. Inclusion and exclusion criteria have been demonstrated in previous publication [17, 18]. In brief, all candidates who successfully replied to a standardized questionnaire were selected. 19 subjects with missing data on alcohol consumption, 714 subjects with incomplete information of Athens Insomnia Scale (AIS-8), and 264 subjects with a history of cardiovascular disease (such as atrial fibrillation, heart failure, myocardial infarction and so on) or cancer were all excluded. Finally, 8081 participants were included in this study.
The study was performed according to guidelines from the Helsinki Declaration. Ethical approvals were obtained from the Ethics Committee of Jidong Oil- field, Inc. Medical Centers. All participants signed informed consent.
Measurement of alcohol consumption
Data on alcohol consumption were collected using questionnaires [17, 19, 20]. The questionnaires gathered information on the drinking frequency and the average amount of alcohol consumed per day. Participants were also asked to report the number of standard drinks. The total alcohol intake was calculated in grams by multiplying drinking frequency per day, the average amount of alcohol consumed and the volume of alcohol contained (the volume of ethanol is 12.5% in wine, 5% in beer and 45% in liquor). In this study, 15g of ethanol was taken as a standard serving [21]. On the basis of the number of standard servings, participants were classified into three categories: none (never drank or drank in the past), mild-to-moderate (women ≤1.0 servings/day; men ≤2.0 servings/day) and heavy (women >1.0 servings/day; men > 2.0 servings/day) [22].
Assessment of insomnia
The entire 8-item Athens Insomnia Scale (AIS-8) is a self-assessment psychometric instrument based on the Tenth Revision (ICD-10) diagnostic criteria, which has been developed as a tool to evaluate the severity of insomnia. In addition, AIS-8 is not only used to measure the intensity of sleep difficulty reliably, but also to assist in establishing the diagnosis of insomnia, and thus it has become an invaluable tool in sleep research and clinical practice. In this study, the AIS-8 was created into a questionnaire including 8 items. The first 5 items were used to assess the difficulty with sleep induction, awakenings during the night, early morning awakening, total sleep time, and the overall quality of sleep. While another 3 items were used to evaluated the consequences of insomnia on the following day, including sense of well-being, functioning, and sleepiness during daytime [23]. The entire 8-items AIS had a total score ranging from 0 to 24, with each item rating from 0 to 3. Participants with 0 score corresponded to “no problem at all”, and those with 3 scores corresponded to “very serious problem”. Subjects with AIS scores ≥6 were recognized as insomnia victims [24].
Assessment of covariates
Data on demographic (age, sex, marital status, education level, income, physical activity and smoking status) and clinical characteristics (body mass index (BMI), hypertension, diabetes and insomnia) were collected via questionnaires. The levels of education were classified into three categories: primary school and below, middle and high school, college and above. The physical activities of participants were divided into three categories according to the following three kinds of circumstances: (1) inactive, nearly none; (2) moderately active, 1–149 min/ week of moderate intensity or 1–74 min/week of vigorous intensity; or (3) active, ≥150 min/week of moderate intensity or ≥75 min/week of vigorous intensity [25]. The smoking status were classified as never (<100 cigarettes in the entire life), past or current smoker. After measuring body weight (kg) and height (cm) for each subject on the day of tests, the BMI was calculated as body weight (kg) divided by the square of height (m) [26]. Simultaneously, hypertension was defined as a self-reported history of hypertension, including the use of antihypertensive medication, systolic blood pressure ≥140 mm Hg or diastolic blood pressure ≥90 mm Hg [26, 27]. The definition of diabetes mellitus was fasting blood glucose ≥7.0 mmol/L, current treatment with insulin/oral hypoglycemic agents or a history of diabetes mellitus [28].
All biochemical variables were measured at the central laboratory at Jidong Oilfield Hospital, including total cholesterol (TC was measured using the endpoint test method), triglyceride (TG was measured using the GPO method), high-density lipoprotein cholesterol and low-density lipoprotein cholesterol (HDL-C and LDL-C levels were measured using the direct test method) [17].
Statistical analysis
Statistical analysis was performed with SAS software, version 9.4 (SAS Institute, Cary, North Carolina, USA). Normal distribution of continuous variables was tested using the Kolmogorov-Smirnov test. The continuous data underlying normal distribution were presented as mean values (standard deviation, SD) and compared via T-test or ANOVA analysis; While non-normal distribution variables were presented as median values (interquartile range, IQR) and compared using corresponding nonparametric methods. Categorical variables were presented as counts and percentages, and compared using chi-squared tests or the Fisher’s exact test, when appropriate. Logistic regression analyses were performed to assess the association between alcohol consumption and insomnia by calculating the odds ratios (ORs) and 95% confidence interval (95% CI), with the adjustments for age, sex, income, BMI, education level, smoking status, physical activity, hypertension, diabetes, TC, TG, HDL-C and LDL-C. Furthermore, this study not only evaluated the relationship between alcohol consumption and insomnia among all participants, but also stratified the data by gender and age.
All statistical analyses were 2-sided and the P-value <0.05 was considered statistically significant.
Results
Baseline characteristics
Fig 1 shows the flow chart of this study. Totally, 9078 residents were selected, among which 8081 of them were recruited in the present study. The baseline characteristics of alcohol consumption are shown in Table 1. Among 8081 eligible subjects, 2618 (32.4%) are alcohol drinkers (mild-to-moderate drinkers: 59.1%; heavy drinkers: 40.9%), including 2424 (92.6%) males and 194 (7.4%) females. Alcohol consumers have a relatively higher income and education level than non-drinkers, with 52.8% (1381/2618) current smokers. In addition, mild-to-moderate and heavy alcohol drinkers also have a higher prevalence of hypertension than non-drinkers (44.5% vs 31.1% and 45.5% vs 31.1%, respectively).
Fig 1. Flow chart of subjects with different exclusion criteria in this study.
Table 1. Baseline characteristics of total alcohol consumption.
| Characteristic | Total (N = 8081) |
Alcohol consumption | P-value | ||
|---|---|---|---|---|---|
| None (n = 5463) |
Mild-to-Moderate (n = 1546) |
Heavy (n = 1072) |
|||
| Age, year | 42.1±13.0 | 42.8±13.3 | 41.5±12.5 | 39.7±11.5 | <0.01 |
| Male, n (%) | 4178 (51.7) | 1754 (32.1) | 1446 (93.5) | 978 (91.2) | <0.01 |
| Married, n (%) | 7511 (93.0) | 5104 (93.4) | 1426 (92.2) | 981 (91.5) | 0.04 |
| BMI (SD), kg/m2 | 24.5±3.7 | 24.1±3.7 | 25.5±3.5 | 25.5±3.6 | <0.01 |
| Income | <0.01 | ||||
| ≤3000, n (%) | 3066 (37.9) | 2211 (40.5) | 560 (36.2) | 295 (27.5) | |
| 3000–5000,n (%) | 4400 (54.5) | 2914 (53.3) | 829 (53.6) | 657 (61.3) | |
| >5000, n (%) | 615 (7.6) | 338 (6.2) | 157 (10.2) | 120 (11.2) | |
| Education level | <0.01 | ||||
| Primary school and below, n (%) | 296 (3.7) | 241 (4.4) | 34 (2.2) | 21 (2.0) | |
| Middle and high school, n (%) | 2824 (34.9) | 2038 (37.3) | 500 (32.3) | 286 (26.7) | |
| College and above, n (%) | 4961 (61.4) | 3184 (58.3) | 1012 (65.5) | 765 (71.4) | |
| Physical activity | <0.01 | ||||
| Inactive, n (%) | 3118 (38.6) | 2186 (40.0) | 559 (36.2) | 373 (34.8) | |
| Moderately active, n (%) | 769 (9.5) | 481 (8.8) | 171 (11.1) | 117 (10.9) | |
| Active, n (%) | 4194 (51.9) | 2796 (51.2) | 816 (52.8) | 582 (54.3) | |
| Smoking status | <0.01 | ||||
| Never, n (%) | 5734 (71.0) | 4663 (85.4) | 626 (40.5) | 445 (41.5) | |
| Current, n (%) | 2068 (25.6) | 687 (12.6) | 817 (52.9) | 564 (52.6) | |
| Past, n (%) | 279 (3.4) | 113 (2.1) | 103 (6.7) | 63 (5.9) | |
| Diabetes, n (%) | 524 (6.5) | 344 (6.3) | 106 (6.9) | 74 (6.9) | 0.61 |
| Hypertension, n (%) | 2881 (35.7) | 1700 (31.1) | 704 (45.5) | 477 (44.5) | <0.01 |
| TG (SD), mmol/L | 1.6±1.3 | 1.4±1.1 | 2.0±1.8 | 1.9±1.5 | <0.01 |
| TC (SD), mmol/L | 4.5±0.9 | 4.4±0.9 | 4.5±0.9 | 4.5±0.9 | <0.01 |
| HDL-C (SD), mmol/L | 1.2±0.3 | 1.2±0.3 | 1.1±0.3 | 1.1±0.2 | <0.01 |
| LDL-C (SD), mmol/L | 2.5±0.6 | 2.5±0.6 | 2.5±0.6 | 2.6±0.6 | <0.01 |
| Insomnia, n (%) | 1028 (12.7) | 757 (13.9) | 176 (11.4) | 95 (8.9) | <0.01 |
Values are expressed as mean value ± SD, median value (IQR), or percentage. TG = Triglyceride; TC = Total Cholesterol; HDL-C = High-density lipoprotein cholesterol; LDL-C = Low-density lipoprotein cholesterol; SD = standard deviation.
Prevalence of insomnia
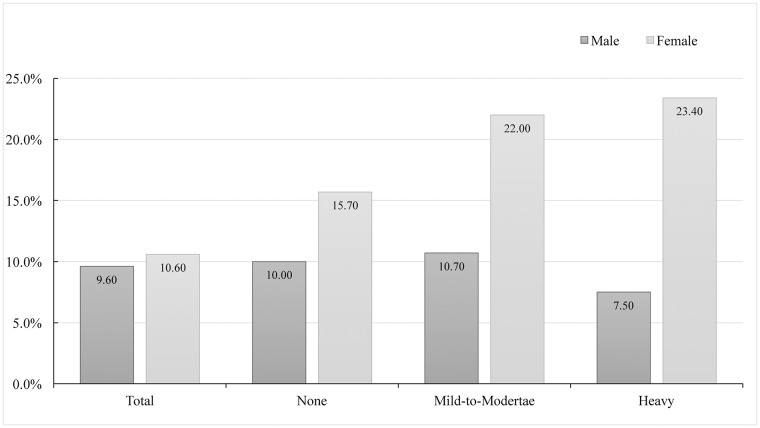
The prevalence of insomnia among non-drinkers, mild-to-moderate drinkers and heavy drinkers are shown in Fig 2. The prevalence of insomnia is 12.7% among the whole participants, and it is higher in females (16.0%) than in males (9.6%). Among the males, the prevalence of insomnia is 10.0% in non-drinkers, 10.7% in mild-to-moderate drinkers and 7.5% in heavy drinkers. Whereas among females, the prevalence of insomnia increases along with the increase of alcohol intake, which is 15.7% in none group, 22.0% in mild-to-moderate group and 23.4% in heavy group.
Fig 2. The prevalence of insomnia between males and females according to alcohol consumption.
Association between alcohol consumption and insomnia
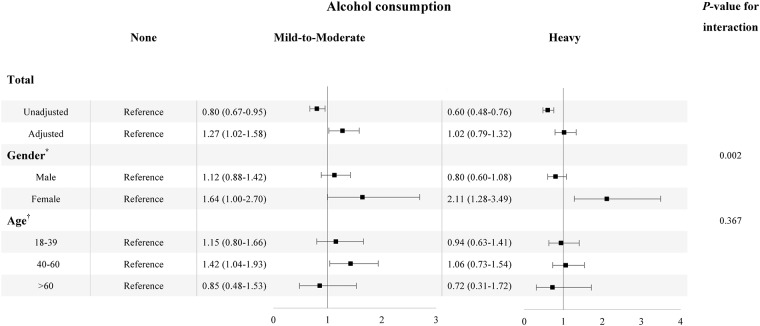
Fig 3 demonstrates the association between insomnia and alcohol consumption in the whole participants, and stratifies by age and gender. After adjusting for age, gender, BMI, income, education level, physical activities, smoking status, hypertension, diabetes, TC, TG, HDL-C and LDL-C, the association between mild-to-moderate alcohol consumption and insomnia is statistically significant (OR:1.27, 95% CI:1.02–1.58). The P value for interaction about gender difference in the association between alcohol consumption and insomnia is statistically significant (P inter = 0.002). Thus, a positive correlation between heavy alcohol consumption and insomnia is found in the female (OR:2.11, 95% CI:1.28–3.49), but not in the male (OR:0.80, 95% CI:0.60–1.08). Stratified by age, the mild-to-moderate alcohol consumption is associated with insomnia among participants aged above 45 years (OR:1.44, 95% CI:1.07–1.92), though the interaction is not statistical significance (P inter = 0.367).
Fig 3. Odds radio with 95% CI of alcohol consumption on insomnia in total, different gender and age categories.
For the total subjects, we presented the association without the introduction of the confounding factors, and we also presented the association controlling for age, gender, BMI, income, education level, physical activities, smoking status, hypertension, diabetes mellitus, TC, TG, HDL-C and LDL. In the stratification analysis, all the covariates were controlled.
Discussion
This large community-based study shows that alcohol consumption is significantly associated with insomnia in females, but not in males. Additionally, it is the first attempt to demonstrated a diverse relationship on gender between alcohol consumption and insomnia in the northern Chinese population.
Several previous studies suggested that there was a relationship between alcohol consumption and insomnia. Consistent with our findings, some studies have found that alcohol consumption might be a risk factor for sleep disorders in general population [29, 30]. Hartwell et al demonstrated a robust association between alcoholism severity and sleep disorders determined by the Pittsburgh Sleep Quality Index (PSQI), and concluded that the problem of alcohol severity might be a predictive signal of sleep disorders [31]. In a 10-year prospective study (N = 2602), Janson and the colleagues found that some subsequent insomnia symptoms were associated with alcohol dependence (moderate-to-severe alcohol consumption disorder), with insomnia assessed by CAGE questionnaire [32]. Similarly, two studies performed in men showed that alcohol use could prevent subjects initiating sleep or make them hard of falling asleep [33, 34]. In addition, some literature also reported that the relationship between alcohol and sleep appeared to be dose related, stating that alcohol consumption might have stimulant effects when it was absorbed at low to moderate dose, and have sedative effects at higher dose and during alcohol elimination [35]. A study found that there was a positive relationship between mild-to-moderate doses alcohol consumption and insomnia in this large gender-based sample population, which was inconsistent with those previous detections. Different results about the relationship between alcohol consumption and insomnia might occur due to several possible reasons: (1) The lack of standard definitions and measurements for both alcohol consumption and insomnia; (2) The different population distribution and sample sizes were not taken into account; (3) There were differences in alcohol pharmacokinetics between men and women.
In the present study, the major finding is that alcohol consumption is associated with insomnia in females, but not in males. Female heavy drinkers have a significantly higher risk of suffering from insomnia than their counterpart males. A lot of evidences have shown an apparent difference in alcohol consumption between males and females [13, 36]. As we all know, the gender gap in alcohol drinking is one of the universal gender differences in human social behavior, which also reflects a different effect on drinking men and women in different drinking cultures. In China, alcohol consumption was generally not discouraged for women, while it was widely accepted in men in the traditional Chinese culture [37]. There were also some obvious differences in the numbers of drinkers and the frequency of alcohol consumption among men and women [8, 38]. The gender difference in the relationship between alcohol consumption and insomnia might be ascribed to alcohol pharmacokinetics. A study based on 93 healthy adults (females: 59; males: 34) found that alcohol objectively disrupted sleep continuity more in the female than in the male only at equally high peak breath alcohol concentrations (BrAC) throughout the entire night [39]. Compared to men, women were likely to suffer more psycho-social and mental impairments due to alcohol intake. Accordingly, the reasons for this result are multifactorial and multilevel, which suggest for further consideration of gender differences in the future research. In addition, we have found that mild-to-moderate alcohol consumption is associated with insomnia in participants aged above 45 years, though the interaction is not statistically significant, which indicates that alcohol intake might be a risk for older individuals. Inconsistent with our finding, a study based on a large proportion of alcoholics detected that only older age was associated with improvements in sleep disturbances during early alcohol recovery [40]. The possible reasons for these different conclusions might be ethnic or gender differences.
Furthermore, some previous studies examined the biological, psychological and social risk factors for the association between alcohol consumption and insomnia, though only few of them explained the mechanisms in the correlation of alcohol use and sleep disorders. Based on limited literature and research results, we have presented several possible mechanisms of the association between alcohol consumption and insomnia for females. On the one hand, the prevalence of mental and psychological illness was higher in females than that in males, especially depression and anxiety. Alcohol intake could stimulate the physiological sensitivity of women, which might help explain the high prevalence of insomnia among women [41]. In addition, since alcohol had a stimulating effect on nervous system, alcohol might motivate the female brain to make them excited, while damaging their neurons, and making them hard of initiating sleep [42]. On the other hand, the primary insomnia was associated with menstrual-related changes in the female, and these menstrual-related changes might affect subjective and objective sleep disorders, especially in the late luteal phase [43, 44]. This evidence has shown that estrogen plays an important regulatory role for female insomnia. Alcohol consumption might have an effect on female estrogen hormone that also led to insomnia.
There are several limitations in this study. Firstly, this study is a cross-sectional study, making it unable to explore the causal effect between insomnia and alcohol consumption. Secondly, the Athens Insomnia Scale (AIS-8) is not used for clinical diagnosis of insomnia, even though it is a widely used epidemiological tool for insomnia assessment. Thirdly, the study is based on the self-reported data and absence of objective measures against insomnia such as polysomnography (PSG) or actigraphy, and the biological markers of alcohol consumption or breath alcohol tests are absent.
Conclusion
This study suggests that alcohol consumption is associated with insomnia in females, but not in males. To a certain extent, alcohol consumption may prevent females from initiating asleep.
Supporting information
(DOCX)
Acknowledgments
We thankfully appreciate all the participants and their relatives in the study. We also thank to the members of the survey teams from the Jidong community.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This study is support by grants from the National Natural Science Foundation of China (No. 81202279); (No. 81473057) and the National Social Science Foundation of China (17BGL184).
References
- 1.Reynolds K, Lewis B, Nolen JD, Kinney GL, Sathya B, He J. Alcohol consumption and risk of stroke: a meta-analysis. Jama. 2003;289(5):579–88. Epub 2003/02/13. . [DOI] [PubMed] [Google Scholar]
- 2.Gowing LR, Ali RL, Allsop S, Marsden J, Turf EE, West R, et al. Global statistics on addictive behaviours: 2014 status report. Addiction (Abingdon, England). 2015;110(6):904–19. Epub 2015/05/13. 10.1111/add.12899 . [DOI] [PubMed] [Google Scholar]
- 3.Chaudhary NS, Kampman KM, Kranzler HR, Grandner MA, Debbarma S, Chakravorty S. Insomnia in alcohol dependent subjects is associated with greater psychosocial problem severity. Addictive behaviors. 2015;50:165–72. Epub 2015/07/08. 10.1016/j.addbeh.2015.06.021 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Li L, Wu C, Gan Y, Qu X, Lu Z. Insomnia and the risk of depression: a meta-analysis of prospective cohort studies. BMC psychiatry. 2016;16(1):375 Epub 2016/11/07. 10.1186/s12888-016-1075-3 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Buysse DJ. Insomnia. Jama. 2013;309(7):706–16. Epub 2013/02/21. 10.1001/jama.2013.193 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Roehrs T, Papineau K, Rosenthal L, Roth T. Ethanol as a hypnotic in insomniacs: self administration and effects on sleep and mood. Neuropsychopharmacology: official publication of the American College of Neuropsychopharmacology. 1999;20(3):279–86. Epub 1999/03/04. 10.1016/s0893-133x(98)00068-2 . [DOI] [PubMed] [Google Scholar]
- 7.Stein MD, Friedmann PD. Disturbed sleep and its relationship to alcohol use. Substance abuse. 2005;26(1):1–13. Epub 2006/02/24. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Johnson EO, Roehrs T, Roth T, Breslau N. Epidemiology of alcohol and medication as aids to sleep in early adulthood. Sleep. 1998;21(2):178–86. Epub 1998/07/04. . [DOI] [PubMed] [Google Scholar]
- 9.Ancoli-Israel S, Roth T. Characteristics of insomnia in the United States: results of the 1991 National Sleep Foundation Survey. I. Sleep. 1999;22 Suppl 2:S347–53. Epub 1999/07/08. . [PubMed] [Google Scholar]
- 10.Singareddy R, Vgontzas AN, Fernandez-Mendoza J, Liao D, Calhoun S, Shaffer ML, et al. Risk factors for incident chronic insomnia: a general population prospective study. Sleep medicine. 2012;13(4):346–53. Epub 2012/03/20. 10.1016/j.sleep.2011.10.033 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brower KJ, Hall JM. Effects of age and alcoholism on sleep: a controlled study. Journal of studies on alcohol. 2001;62(3):335–43. Epub 2001/06/21. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Li RH, Wing YK, Ho SC, Fong SY. Gender differences in insomnia—a study in the Hong Kong Chinese population. Journal of psychosomatic research. 2002;53(1):601–9. Epub 2002/07/20. . [DOI] [PubMed] [Google Scholar]
- 13.Reyner LA, Horne JA, Reyner A. Gender- and age-related differences in sleep determined by home-recorded sleep logs and actimetry from 400 adults. Sleep. 1995;18(2):127–34. Epub 1995/02/01. . [PubMed] [Google Scholar]
- 14.Nolen-Hoeksema S. Gender differences in risk factors and consequences for alcohol use and problems. Clinical psychology review. 2004;24(8):981–1010. Epub 2004/11/10. . [DOI] [PubMed] [Google Scholar]
- 15.Lin YY, Chen HC, Lai WS, Wu LW, Wang CH, Lee JC, et al. Gender Differences in the Association between Moderate Alcohol Consumption and Hearing Threshold Shifts. Scientific reports. 2017;7(1):2201 Epub 2017/05/21. 10.1038/s41598-017-02426-4 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Song Q, Liu X, Wang A, Wang Y, Zhou Y, Zhou W, et al. Associations between non-traditional lipid measures and risk for type 2 diabetes mellitus in a Chinese community population: a cross-sectional study. Lipids in health and disease. 2016;15:70 Epub 2016/04/06. 10.1186/s12944-016-0239-y . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wang Y, Ge S, Yan Y, Wang A, Zhao Z, Yu X, et al. China suboptimal health cohort study: rationale, design and baseline characteristics. Journal of translational medicine. 2016;14(1):291 Epub 2016/10/16. 10.1186/s12967-016-1046-y . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gao X, Zhou Y, Guo YC, Chen Q, Lei XY, Hu HP. Association between Elevated Resting Heart Rate and Metabolic Syndrome in a Community-Based Population. Chinese medical journal. 2018;131(8):1003–4. Epub 2018/04/18. 10.4103/0366-6999.229885 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Li Z, Bai Y, Guo X, Zheng L, Sun Y, Roselle AM. Alcohol consumption and cardiovascular diseases in rural China. International journal of cardiology. 2016;215:257–62. Epub 2016/04/30. 10.1016/j.ijcard.2016.04.095 . [DOI] [PubMed] [Google Scholar]
- 20.Morioka H, Itani O, Kaneita Y, Ikeda M, Kondo S, Yamamoto R, et al. Associations between sleep disturbance and alcohol drinking: A large-scale epidemiological study of adolescents in Japan. Alcohol (Fayetteville, NY). 2013;47(8):619–28. Epub 2013/11/06. 10.1016/j.alcohol.2013.09.041 . [DOI] [PubMed] [Google Scholar]
- 21.Huang S, Li J, Shearer GC, Lichtenstein AH, Zheng X, Wu Y, et al. Longitudinal study of alcohol consumption and HDL concentrations: a community-based study. The American journal of clinical nutrition. 2017;105(4):905–12. Epub 2017/03/03. 10.3945/ajcn.116.144832 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.McGuire S. U.S. Department of Agriculture and U.S. Department of Health and Human Services, Dietary Guidelines for Americans, 2010. 7th Edition, Washington, DC: U.S. Government Printing Office, January 2011. Advances in nutrition (Bethesda, Md). 2011;2(3):293–4. Epub 2012/02/15. 10.3945/an.111.000430 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Soldatos CR, Dikeos DG, Paparrigopoulos TJ. Athens Insomnia Scale: validation of an instrument based on ICD-10 criteria. Journal of psychosomatic research. 2000;48(6):555–60. Epub 2000/10/18. . [DOI] [PubMed] [Google Scholar]
- 24.Soldatos CR, Dikeos DG, Paparrigopoulos TJ. The diagnostic validity of the Athens Insomnia Scale. Journal of psychosomatic research. 2003;55(3):263–7. Epub 2003/08/23. . [DOI] [PubMed] [Google Scholar]
- 25.Wu R, Hou F, Wang X, Zhou Y, Sun K, Wang Y, et al. Nonalcoholic Fatty Liver Disease and Coronary Artery Calcification in a Northern Chinese Population: a Cross Sectional Study. Scientific reports. 2017;7(1):9933 Epub 2017/09/01. 10.1038/s41598-017-09851-5 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hao Z, Zhang Y, Li Y, Zhao J, Zhou Y, Qiu J, et al. The Association between Ideal Cardiovascular Health Metrics and Extracranial Carotid Artery Stenosis in a Northern Chinese Population: A Cross-Sectional Study. Scientific reports. 2016;6:31720 Epub 2016/08/31. 10.1038/srep31720 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. Jama. 2003;289(19):2560–72. Epub 2003/05/16. 10.1001/jama.289.19.2560 . [DOI] [PubMed] [Google Scholar]
- 28.Pearson TA, Palaniappan LP, Artinian NT, Carnethon MR, Criqui MH, Daniels SR, et al. American Heart Association Guide for Improving Cardiovascular Health at the Community Level, 2013 update: a scientific statement for public health practitioners, healthcare providers, and health policy makers. Circulation. 2013;127(16):1730–53. Epub 2013/03/23. 10.1161/CIR.0b013e31828f8a94 . [DOI] [PubMed] [Google Scholar]
- 29.Kuppermann M, Lubeck DP, Mazonson PD, Patrick DL, Stewart AL, Buesching DP, et al. Sleep problems and their correlates in a working population. Journal of general internal medicine. 1995;10(1):25–32. Epub 1995/01/01. . [DOI] [PubMed] [Google Scholar]
- 30.Ford DE, Kamerow DB. Epidemiologic study of sleep disturbances and psychiatric disorders. An opportunity for prevention? Jama. 1989;262(11):1479–84. Epub 1989/09/15. . [DOI] [PubMed] [Google Scholar]
- 31.Hartwell EE, Bujarski S, Glasner-Edwards S, Ray LA. The Association of Alcohol Severity and Sleep Quality in Problem Drinkers. Alcohol and alcoholism (Oxford, Oxfordshire). 2015;50(5):536–41. Epub 2015/05/29. 10.1093/alcalc/agv046 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Janson C, Lindberg E, Gislason T, Elmasry A, Boman G. Insomnia in men-a 10-year prospective population based study. Sleep. 2001;24(4):425–30. Epub 2001/06/14. . [DOI] [PubMed] [Google Scholar]
- 33.Harma M, Tenkanen L, Sjoblom T, Alikoski T, Heinsalmi P. Combined effects of shift work and life-style on the prevalence of insomnia, sleep deprivation and daytime sleepiness. Scandinavian journal of work, environment & health. 1998;24(4):300–7. Epub 1998/10/01. . [DOI] [PubMed] [Google Scholar]
- 34.Fabsitz RR, Sholinsky P, Goldberg J. Correlates of sleep problems among men: the Vietnam Era Twin Registry. Journal of sleep research. 1997;6(1):50–6. Epub 1997/03/01. . [DOI] [PubMed] [Google Scholar]
- 35.Roehrs T, Roth T. Sleep, sleepiness, sleep disorders and alcohol use and abuse. Sleep medicine reviews. 2001;5(4):287–97. Epub 2003/01/18. 10.1053/smrv.2001.0162 . [DOI] [PubMed] [Google Scholar]
- 36.Mumenthaler MS, Taylor JL, O’Hara R, Yesavage JA. Gender differences in moderate drinking effects. Alcohol research & health: the journal of the National Institute on Alcohol Abuse and Alcoholism. 1999;23(1):55–64. Epub 2000/07/13. . [PMC free article] [PubMed] [Google Scholar]
- 37.Cochrane J, Chen H, Conigrave KM, Hao W. Alcohol use in China. Alcohol and alcoholism (Oxford, Oxfordshire). 2003;38(6):537–42. Epub 2003/11/25. . [DOI] [PubMed] [Google Scholar]
- 38.Kaneita Y, Uchiyama M, Takemura S, Yokoyama E, Miyake T, Harano S, et al. Use of alcohol and hypnotic medication as aids to sleep among the Japanese general population. Sleep medicine. 2007;8(7–8):723–32. Epub 2007/05/22. 10.1016/j.sleep.2006.10.009 . [DOI] [PubMed] [Google Scholar]
- 39.Arnedt JT, Rohsenow DJ, Almeida AB, Hunt SK, Gokhale M, Gottlieb DJ, et al. Sleep following alcohol intoxication in healthy, young adults: effects of sex and family history of alcoholism. Alcoholism, clinical and experimental research. 2011;35(5):870–8. Epub 2011/02/18. 10.1111/j.1530-0277.2010.01417.x . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kolla BP, Schneekloth T, Biernacka J, Mansukhani M, Geske J, Karpyak V, Hall-Flavin D, et al. The course of sleep disturbances in early alcohol recovery: an observational cohort study. (1521–0391 (Electronic)). [DOI] [PubMed] [Google Scholar]
- 41.Lindberg E, Janson C, Gislason T, Bjornsson E, Hetta J, Boman G. Sleep disturbances in a young adult population: can gender differences be explained by differences in psychological status? Sleep. 1997;20(6):381–7. Epub 1997/06/01. . [DOI] [PubMed] [Google Scholar]
- 42.de Wit H, Metz J, Wagner N, Cooper M. Behavioral and subjective effects of ethanol: relationship to cerebral metabolism using PET. Alcoholism, clinical and experimental research. 1990;14(3):482–9. Epub 1990/06/01. . [DOI] [PubMed] [Google Scholar]
- 43.Manber R, Armitage R. Sex, steroids, and sleep: a review. Sleep. 1999;22(5):540–55. Epub 1999/08/18. . [PubMed] [Google Scholar]
- 44.Steiger A, von Bardeleben U, Wiedemann K, Holsboer F. Sleep EEG and nocturnal secretion of testosterone and cortisol in patients with major endogenous depression during acute phase and after remission. Journal of psychiatric research. 1991;25(4):169–77. Epub 1991/01/01. . [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.