Abstract
Background
Despite the increasing number of studies evaluating patient reported outcome measures (PROs), there is no clearness regarding which restorative treatment offers major benefits based on the pediatric patient perspective.
Aim
To compare different restorative techniques in pediatric dentistry regarding patient-reported outcomes.
Design
Literature searching was carried out on prospective studies indexed in PubMed, Scopus and OpenGrey. A Mixed Treatment Comparisons (MTC) meta-analysis was undertaken considering the results from reviewed studies. Anxiety, pain and quality of life were extracted as mean with standard deviation, percentage of pain, and mean difference of scores with standard deviation, respectively. For direct comparisons, data were combined using a random-effect model. Heterogeneity was assessed with the I2 statistic. For indirect comparisons, fixed and random effects were chosen through comparison of competing models based on the Deviance Information Criteria (DIC). The expected efficacy ranking based on the posterior probabilities of all treatment rankings was also calculated.
Results
An initial search resulted in 4,322 articles, of which 17 were finally selected. Due to unavailability of data, only pain, anxiety and oral health related quality of life (OHRQoL) were statistically analyzed. The difference in means (95% CI) of anxiety between treatments using only hand instruments with or without chemomechanical agents were -5.35 (-6.42 to -4.20) and -5.79 (-7.77 to -3.79) respectively when compared to conventional treatment using rotary instruments and/or local anesthesia. Regarding pain, there was a trend for treatments without rotary instruments and local anesthesia to be less frequently reported as painful. No statistical difference was found intragroup nor among treatments for OHRQoL.
Conclusions
Anxiety and pain are directly related with more invasive restorative treatments. On the other hand, quality of life is not improved regardless of the restorative technique used. Further well-designed prospective studies regarding PROs in children are still necessary.
Introduction
Patient-reported outcome (PRO) is an assessment of health status reported by the patients themselves instead of being interpreted by an observer[1]. Although physical, physiological and biomechanical data may be measured through medical examination, there is some information that can only be obtained from the patient, such as symptoms, feelings and disease’s impact[2]. The utilization of PRO in health care is an emerging metric that is becoming increasingly important[3–5]. It is considered an essential component in the provision of health care and ensures patient’s voice and his engagement in medical decision-making[6]. In the field of pediatric dentistry, this takes a major role because negative dental experiences during childhood and adolescence reverberate in adulthood, presenting a long-term effect[7].
As restorative care is a fundamental part of the comprehensive oral health treatment of children[8], it has been more extensively studied regarding PROs. The traditional clinical parameters to assess restorative treatments, such as marginal integrity and wear surface of restorations, secondary caries, and pulp inflammation[9], have been complemented by patient-based outcomes as quality of life[10,11], anxiety[12–13], children and parental perception[14] and pain[14–18].
Recent studies have been focusing on patient-based outcomes measured not only by psychometric scales[19–21] but also physiological rates or under the health professional perspective[19]. However, the published data presents conflicting results and inconclusive findings, with no clearness regarding which restorative treatment offers major benefits based on the patient perspective. In this context, the aim of this systematic review is to compare different restorative techniques in pediatric dentistry regarding patient-reported outcomes.
Material and methods
This systematic review was reported according to PRISMA guidelines[22] as detailed in Supporting Information section. A review protocol was recorded at PROSPERO database under the registration number CRD42017056285.
Literature search
The literature search on MEDLINE (PubMed), Scopus and OpenGrey was performed until February 2018. A search strategy was developed for MEDLINE (PubMed) and then suited to the other two databases (Table 1). Three groups of words combined with the boolean term ‘OR’ were created, including key words for primary teeth, restorative treatment and patient-based outcome. The three groups were combined with the boolean term ‘AND’. Both Text Word and Mesh Terms were used. Hand searching was performed on reference lists of full-text read articles and no languages restrictions were applied.
Table 1. Search strategy developed for MEDLINE via PubMed.
| #1 | (child*) or (children) or (pediatric) or (paediatric) or (infant*) or (minor*) or (deciduous tooth) or (deciduous teeth) or (primary tooth) or (primary teeth) or (primary dentition) or (baby tooth) or (baby teeth) or (primary molar*) or (adolescent*) or (adolescent) or (deciduous tooth) or (deciduous teeth) or (deciduous dentition) or (primary tooth) or (primary teeth) |
| #2 | (restorative treatment*) or (dental restoration*) or (dental filling*) or (atraumatic restorative treatment, dental) or (atraumatic restorative treatment) or (amalgam) or (resin composite) or (composite resin) or (composite restoration*) or (compomer) or (glass ionomer cement) or (permanent dental restoration*) or (permanent dental filling) |
| #3 | (pain) or (discomfort) or (anxiety) or (quality of life) or (fear) or (patient based outcome) or (patient centered outcome) or (patient satisfaction) or (dental fear) or (dental phobia) or (odontophobia) or (panic) or (acceptability) or (tooth appearance) or (oral health related to quality of life) |
| #4 | #1 AND #2 AND #3 |
* Truncating search terms: it finds terms that begin with the word’s root
Selection criteria
Eligible studies in this systematic review included prospective studies assessing dental restorative treatment in the primary dentition. The lack of a comparison group and patient-reported outcomes as well as studies performed in groups with specific conditions different from normality and studies in which primary and permanent dentition data were not analyzed separately were excluded. As patient-reported outcomes we consider all assessments that are reported by the patient according to the CONSORT PRO Extension[1]. In addition, the proxy-reported outcome Oral Health Related Quality of Life (OHRQoL) was also appraised.
Review methods
Titles and abstracts were screened independently by two reviewers (N.M.L and T.K.T.). If the study met the inclusion criteria or if there were insufficient data available, full-text articles were obtained for further assessment by the same reviewers. Cohen Kappa test was performed to ensure their inter-rater reliability before both phases using 10% of the search sample. Disagreements were discussed with an expert (D.P.R.) to reach consensus.
Data extraction and processing
Relevant data were collected using a structured data extraction form. Author, publication year, country, study location and design were extracted to describe the studies. Sample size, age of participants, group of teeth treated and sample size according to the treatment were collected to characterize the sample. Regarding the results, operator, outcome, evaluation criteria, time of evaluation and main findings were extracted. Authors of included studies were contacted to provide additional data when needed.
The treatments compared among the studies were categorized in six groups according to the characteristics described: I- Restorative treatment using rotary instruments and local anesthesia (BUR+LA); II- Restorative treatment using rotary instruments (BUR); III- Restorative treatment using hand instruments and adhesive material (HI); IV- Restorative treatment using chemomechanical agents (CHM); V- Hall Technique (HT); VI- Ultraconservative restorative treatment (UCT).
Studies’ quality was assessed by two reviewers (N.M.L and T.K.T) independently. The Cochrane Collaboration Tool was used to appraise all studies included. Each study was evaluated as low, high or unclear risk of bias according to the randomization, allocation concealment, blinding, completeness of outcome data, selective outcome reporting, and other potential bias. Authors were contacted via e-mail for missing or unclear information. Disagreements between the reviewers were solved by consensus.
Publication bias would be assessed if more than 10 studies were identified, since power is low otherwise [23].
Statistical analysis
The three outcomes quantitatively evaluated in the meta-analysis were considered as continuous variables and treated according to the measures available in each article. Mean with standard deviation, percentage of pain, and mean difference of scores with standard deviation were extracted to evaluate anxiety, pain and quality of life respectively. The coefficients reported in the meta-analysis were difference in means with 95% confidence interval (95%CI) for anxiety and quality of life and risk relative (RR) with 95%CI for pain.
The effects of each treatment for dental caries in primary teeth on patient-reported outcomes were analyzed using a Mixed Treatment Comparisons (MTC) meta-analysis. The MTC combines direct and indirect comparisons across a range of competing interventions by including multiple distinct pairwise data. It also allows the calculation of treatment ranking probabilities regarding their efficacy[24]. As MTC is based on Bayesian hierarchical framework, the estimates were obtained by Markov-Chain Monte Carlo simulations. All analysis was performed in the R statistical software using the GeMTC package version 0.8 and the rJAGSpackage to estimate the models.
For direct comparisons, data were combined using a random-effect model. Heterogeneity was assessed with the I2 statistic when more than one study compared the same treatments regarding the same outcome.
For indirect comparisons, the choice between fixed and random effects was made through the comparison of competing models based on the Deviance Information Criteria (DIC). For each model, goodness-of-fit to data was evaluated using residual deviance[25]. Vague prior distributions were used for all models. The expect ranking of efficacy for all treatments based on the posterior probabilities of all treatment rankings[26] was also calculated. Node split analysis for inconsistency was not performed because most part of the treatments did not present direct comparisons.
Results
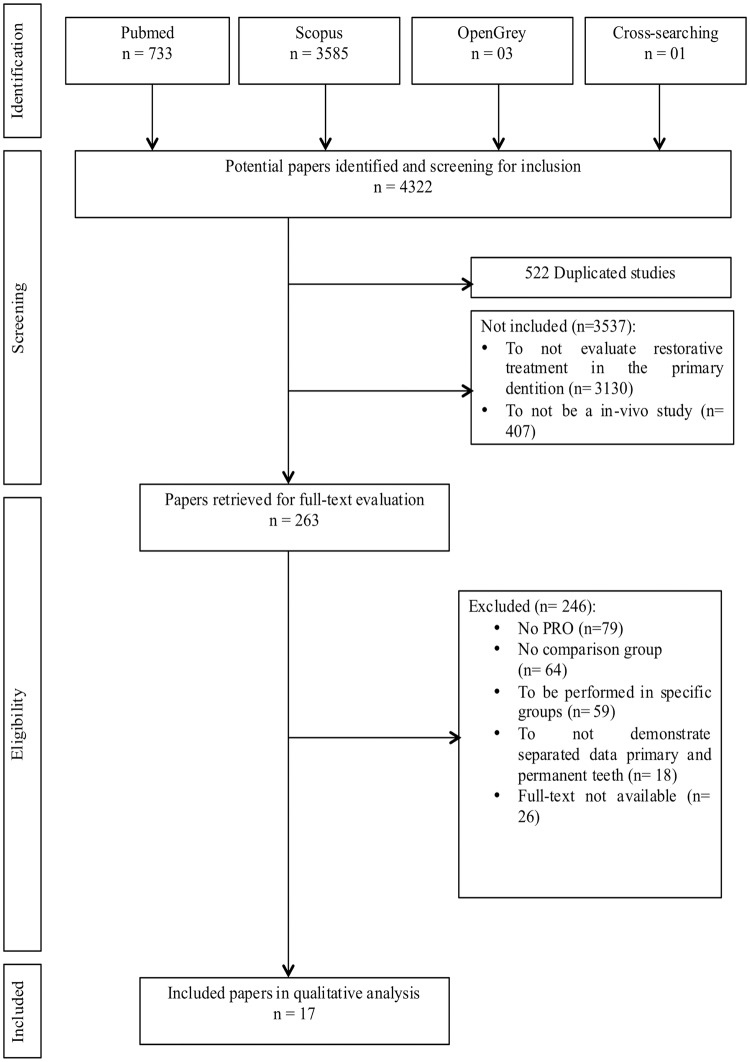
In total, 4,322 studies were identified through the search strategy of which 3,800 were non-duplicated. The inter-rater reliability was 0.79 for abstract inclusion and 1.0 for full-text exclusion. After screening titles and abstracts, 263 papers were retrieved for full-text evaluation. The main reason for excluding studies was the absence of patient-reported outcome measures (n = 79). A final number of 17 papers met the eligibility criteria (Fig 1). From those, eight different patient-reported outcomes were identified as following: pain (n = 7), discomfort (n = 2), treatment preference (n = 1), anxiety (n = 6), quality of life related to oral health (n = 2), satisfaction (n = 3), willingness to receive the treatment again (n = 1) and appearance (n = 1). Some papers reported more than one outcome (Table 2).
Fig 1. Flowchart of studies selection.
Table 2. Main characteristics of data from included studies.
| Author/ Year and Country |
Designesign | Location | n (patient) |
Age (years) | Teeth | N in according to the treatment | Operator | Outcome | Evaluation criteria | Moment of evaluation | Findings |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Louw et al. [15] 2002 (South Africa) |
RCT† Parallel Groups |
Clinic | 401 | 6–9 | Primary teeth | ART*: 175 ART* w/ bur: 117 ART* & ART* w/ bur: 109 |
Dentists | Pain | Question: Did you feel pain when the tooth was being fixed? | 10 days after treatment |
% Pain ART*: 19 ART* w/ bur: 15 ART* & ART* w/ bur: 22 |
| Bochove et al. [27] 2006 (Suriname) |
RCT† Parallel Groups |
Clinic | 300 | 6–7 | Primary molars (Proximal cavity) |
Bur–n/m ART* –n/m Bur w/ LA§ –n/m ART* w/ LA§- n/m |
Final year dental student and dentist | Discomfort | Venham Picture Test | Immediately after treatment | No numerical results available |
| Innes et al. [28] 2007 (Scotland) |
RCT† Split mouth |
Clinic | 132 | 3–10 | Primary molar | Bur w/ LA§: 132 Hall Technique: 132 |
General clinicians | Child Preference | Question | After completion of both treatments |
% Most preferred Children: 72% Hall Technique |
| Mickenautsch et al. [12] 2007 (South Africa) |
RCT† Parallel Groups |
Clinic | 143 | 8.9 (Mean) 10.3 (Mean) |
Primary teeth | ART*: 59 Bur w/ LA§- 84 |
Dental operators | Anxiety | Children’s Fear Survey Schedule | Immediately after treatment |
Mean Score (SEπ) A: 24.4 (1.2) B: 14.8 (1.7) |
| Topaloglu-Ak et al. [13] 2007 (A) (Turkey) |
RCT† Parallel Groups |
Clinic | 518 | 6–7 | Primary molar (Proximal cavity) |
Bur: 64 ART*: 96 |
Dentists | Anxiety | Venham Picture Test | Immediately after treatment |
Mean (SDˆ) Bur: 1.0 (1.6) ART*: 1.0 (1.7) |
| Topaloglu-Ak et al. [13] 2007 (B) (Turkey) |
RCT† Parallel Groups |
Clinic | 518 | 6–7 | Primary molar (Proximal cavity) |
ART*: 158 ART* w/ Cariosolv: 150 |
Dentists | Anxiety | Venham Picture Test | Immediately after treatment |
Mean (SDˆ) ART*: 1.7 (1.9) ART* w/ Cariosolv: 1.3 (1.7) |
| Abreu et al. [16] 2009 (Brazil) |
RCT† Parallel Groups |
Clinic | 40 | 4–7 | Primary molars | ART*: 20 Bur w/ LA§: 20 |
Not mentioned | Pain | Wong-Baker Facial Scale | Immediately after treatment |
% Pain ART*: 7 Bur w/ LA§: 25 |
| Aguilar et al. [17] 2012 (Peru) |
RCT† Split mouth |
Clinic | 30 | 5 | Primary molars (Occlusal cavity) |
ART* w/ Papacarie: 30 Bur w/ LA§: 30 |
General clinician | Pain | Wong-Baker Facial Scale (Yes/No) |
Immediately after treatment |
% Pain ART* w/ Papacarie: 3.33 Bur w/ LA§: 53.33 |
| Luz et al. [18] 2012 (Brazil) |
RCT† Parallel Groups |
Clinic | 30 | 4–7 | Primary molars (Proximal cavity) |
ART*: 15 Bur w/ LA§: 15 |
Not mentioned | Satisfaction Pain Willing to receive the treatment again |
Facial Image Scale (FIS) Yes/No Question: Would you be prepared to receive the same type of treatment again? |
Immediately after treatment | ART*: 50% Satisfied, 42.9% Pain, 37.5% Willing Bur w/ LA§ 2% Satisfied, 62.5% Pain, 71.4% Willing |
| Leal et al. [10] 2013 (Brazil) |
RCT† Parallel Groups |
Clinic | 277 | 6–7 | Primary molars | Bur: 55 ART*: 47 UCTΔ: 58 |
Paedodontists | Quality of life related to oral health | B-ECOHIS | Baseline and follow-up (1 year) |
Difference in mean B-ECOHIS scores (SEπ) Bur: -0.04 (0.11) ART*: 0.01 (0.11) UCTΔ: -0.10 (0.11) |
| Mustafa et al. [29] 2013 (United Kingdom) |
Prospective PROM study | Clinic | 125 | 5–17 | Primary teeth | Preformed Crown w/ LA§: 10 Bur w/ LA: 16 |
Not mentioned | Pain | FPS-R (5-7yrs) VAS (7-18yrs) |
2, 4, 6 Hours after treatment |
% Pain (Highest score) Crown: 40 Bur w/ LA§: 38 |
| Santamaria et al. [14] 2014 (Germany) |
RCT† Parallel Groups |
Clinic | 169 | 3–8 | Primary molars (Proximal cavity) |
Bur w/ LA§: 65 Hall Technique: 52 NRCT+ w/ bur: 52 |
Paedodontists Post-graduate paediatric students |
Pain | Visual analogue pain scale | Immediately after treatment |
% Pain Bur w/ LA§: 42 Hall Technique: 81 NRCT: 88 |
| Arrow et al. [11] 2016 (Australia) |
RCT† Parallel Groups |
Clinic | 254 | 3.8 (Mean) | Primary teeth | ART* w/ Bur: 127 Bur w/ LA§: 127 |
Dental therapists | Quality of life related to oral health | ECOHIS | Baseline and follow up (6–12 months) |
Mean (SDˆ) ART* w/ Bur: 2.00 (0.92) Bur w/ LA§: 1.28 (0.63) |
| Arrow et al. [30] 2017 (Australia) |
RCT† Parallel Groups |
Clinic | 254 | > 6 | Primary teeth | ART*: 127 Bur w/LA: 127 |
Dental therapists (ART) Dentists (Bur) |
Anxiety | Facial Image Scale (FIS) | Baseline and follow up (12 months) |
% Anxiety improvement ART*: 26 Bur: 26 |
| Maciel et al. [31] 2016 (Brazil) |
Mixed-method study | Clinic or Schools | 1045 | 4–8 | Primary molars | Hall technique: 234 ART*: 408 Amalgam: 198 Composite resin: 205 |
Dentists | Satisfaction (Quantitative data) |
Face scale with 5 possible answers (Quantitative data) Content analysis (Qualitative data) |
Immediately after treatment |
Satisfaction (%): Hall technique: 95.3 ART*: 94.9 Amalgam: 97.5 Composite resin: 99 |
| Lakshmi et al. [32] 2018 (India) |
RCT† | School | 30 | 5–8 | Primary molar | ART*: 15 Hall Technique: 15 |
Not mentioned | Satisfaction Discomfort Appearance |
Yes/No Wong-Baker Facial Scale Positive/Negative |
After treatment |
%Satisfied: ART* 86.67 versus HT+ 66.67 Mean Discomfort (SDˆ): ART* 1.87 (0.92) versus HT+ 0.53 (0.92) %Positive appearance: ART* 100 versus HT+ 20 |
| Barreto et al. [33] 2017 (Brazil) |
Analytical cross-sectional study | School | 94 | 6–8 | Deciduous molar | ART*: 46 SDF: 48 |
Not mentioned | Anxiety | Facial Image Scale (FIS) | Before, during and after treatment |
No anxiety (% Worse scenario) ART*: 41.3 SDF: 39.8 |
| Tavares et al. [34] 2018 (Brazil) |
RCT† Split mouth |
Clinic | 79 | 5–8 | Primary molars | ART*: 79 Bur: 79 |
Pediatric dentist | Anxiety Pain |
Facial Image Scale (FIS) Wong-Baker Facial Scale |
Before treatment At the end of the restoration |
Median Anxiety (IQR”): ART* 2.0 (1.25) versus Bur 2.0 (1.5) Median Pain (IQR”): ART* 0 (2.0) versus Bur 2.0 (2.0) |
†RCT: Randomized Clinical Trial;
*ART: Atraumatic Restorative Treatment;
§LA: Local Anesthesia;
ΔUCT: Ultraconservative Treatment;
+NRCT: Non-Restorative Caries Treatment;
+HT: Hall Technique;
πSE: Standard Error;
ˆSD: Standard Deviation;
“IRQ: Interquartile range; n/m: not mentioned.
Cells in grey: studies that were not included in the quantitative analysis due to an impossibility to merge and compare the available data.
All studies except three, which was a prospective PRO study, a mixed-method study and an analytical cross-sectional study, were randomized clinical trials (RCT). Treatments were only performed in posterior teeth.
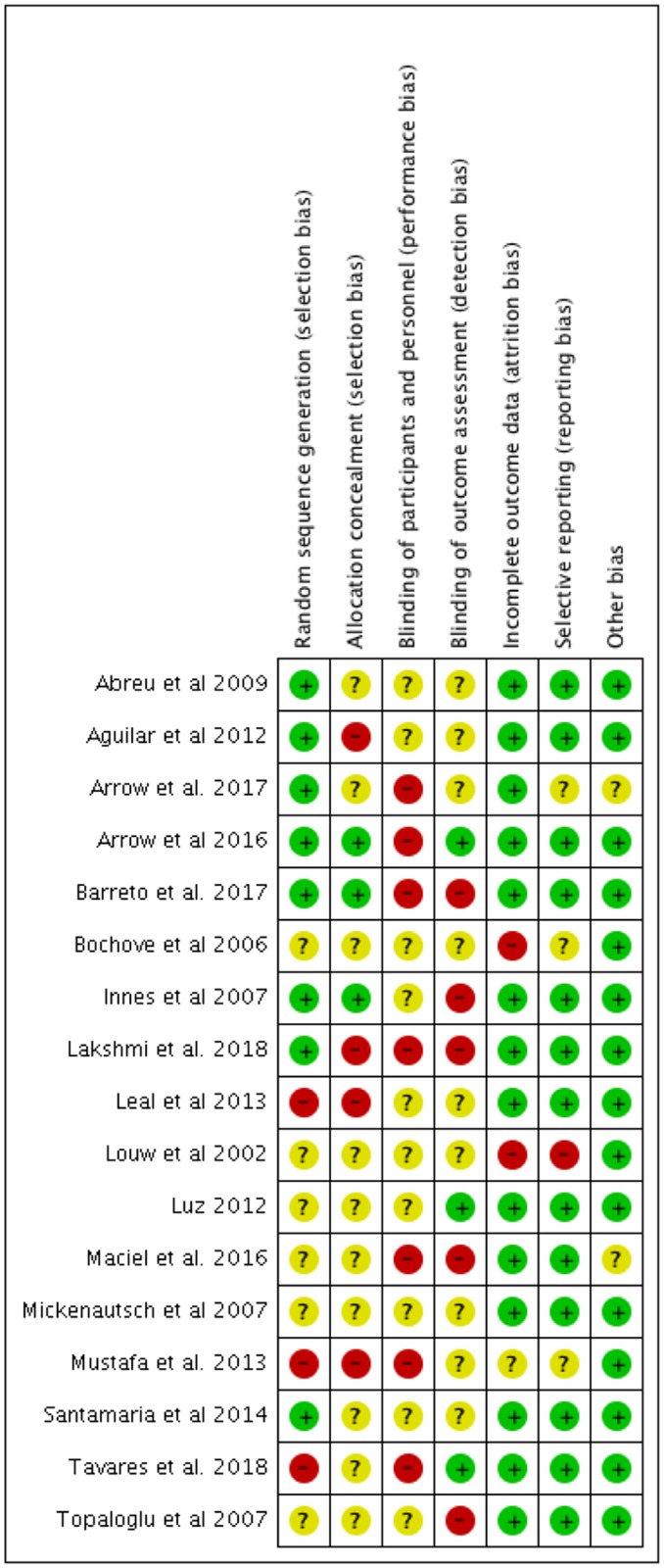
Risk of bias assessment
The assessment of the risk of bias for the included studies is displayed in Fig 2. None of the categories was classified as low risk for all the studies. Most of them did not report enough data regarding allocation concealment and blinding of participants, operators and evaluators. Reporting, attrition and selecting bias were the most frequent available low-risk bias information.
Fig 2. Risk of bias assessment using the Cochrane Collaboration Tool.
Mixed treatment comparisons
Due to the unavailability of data regarding the same outcome, only pain, anxiety and oral health related quality of life were statistically analyzed.
Anxiety
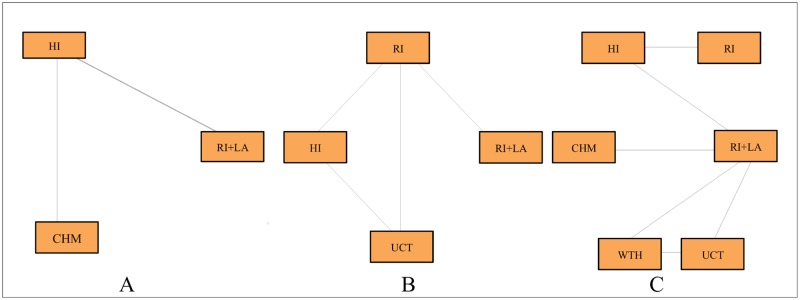
From the six studies assessing anxiety, three of them presented comparable data. The Venham Picture Test was used as the evaluation tool by two studies while the Child’s Fear Survey Schedule, by the remaining one. The treatments compared were restorative treatment using rotary instruments and local anesthesia (BUR+LA), restorative treatment using rotary instruments (BUR), restorative treatment using hand instruments and adhesive materials (HI), and restorative treatment using chemomechanical agents (CHM). The mean and standard deviations were used to perform the MTC meta-analysis. Treatments (BUR+LA) and (BUR) were merged and analyzed as the same group (BUR+LA). Direct comparison was possible between treatments (BUR+LA) and (HI) as well as (HI) and (CHM) as illustrated in Fig 3A. Treatments (BUR+LA) and (CHM) were compared indirectly using a fixed effects model.
Fig 3. Network of the comparisons of restorative treatments in primary teeth.
The width of lines connecting each pair of treatment is proportional to the number of studies regarding anxiety (A), quality of life (B) and pain (C).
The results of the MTC meta-analysis are summarized in Table 3. Regarding anxiety, the indirect comparison identified a significant difference between treatments using rotary instruments with or without local anesthesia (BUR+LA) and chemomechanical agents (CHM). It also indicated a better performance of treatments using hand instruments and adhesive materials (HI) compared to (BUR+LA). The difference between (HI) and (CHM) were not confirmed in this model.
Table 3. Mixed treatment comparison (MTC) model comparing anxiety among treatments.
| Anxiety | Direct comparison * | Indirect comparison ** |
|---|---|---|
| Difference in means (95% CI) | ||
| HI vs. BUR+LA | -1.21 (-3.66 to 1.1) | -5.35 (-6.42 to -4.20) |
| CHM vs. BUR+LA | -- | -5.79 (-7.77 to -3.79) |
| CHM vs. HI | -0.40 (-0.80 to 0.002) | -0.45 (-2.15 to 1.30) |
* Random effects model,—Inverse variance method; DerSimonian-Laird estimator for tau^2; I^2 = 98.7% (97.3%–99.4%).
** Fixed effects model, Model fit: residual deviance; DIC = 19.44. Each chain used 80,000 iterations with a burn-in of 10,000 and a tinning interval of 20.
Negative values represent a decrease in the anxiety levels. Highlighted cells represent contributions from indirect comparisons.
Table 4 presents the ranking of treatments according to their probability of being the best choice. The order of the probability of less-anxiety provoking treatments was restorative treatment using chemomechanical agents (CHM), restorative treatment using hand instruments and adhesive material (HI) and rotary instruments with or without local anesthesia (BUR+LA). The probability of treatment (BUR+LA) be the worse treatment regarding anxiety was approximately 97%.
Table 4. Ranking of efficacy among treatments regarding anxiety.
| Treatments | Position 1 | Position 2 | Position 3 |
|---|---|---|---|
| BUR+LA | 0.00025 | 0.02616 | 0.97358 |
| HI | 0.49933 | 0.57066 | 0.00000 |
| CHM | 0.57041 | 0.40316 | 0.02641 |
Bold values are the highest values in the selected columns.
Oral health related to quality of life
From the two studies evaluating the Oral Health Related to Quality of Life (OHRQoL), both of them used the Early Childhood Oral Health Impact Scale (ECOHIS) questionnaire. The treatments compared were restorative treatment using rotary instruments and local anesthesia (BUR+LA), restorative treatment using rotary instruments (BUR), restorative treatment using hand instruments and adhesive material (HI), and ultraconservative restorative treatment (UCT) as demonstrated in Fig 3B. The mean difference of OHRQoL scores after and before treatment and the standard deviation were used to perform the MTC meta-analysis. Direct comparison was possible between treatments (BUR+LA) and (BUR), (BUR) and (HI), (BUR) and (UCT), and (HI) and (UCT). Treatments (BUR+LA) and (HI) as well as (BUR+LA) and (UCT) were indirectly compared using a fixed effects model.
Regarding the improvement in the OHRQoL, no statistical difference was observed intragroup nor among treatments. The significant difference reported in the studies whose values did not overcome 1 was lost after performing the MTC meta-analysis.
In relation to the ranking probability of OHRQoL improvement (Table 5), treatment (UCT) was ranked in the first position even though no restorative material is used to fill the cavities in this technique. It would be followed by (BUR), (HI) and (BUR+LA). The last one presented approximately 70% of chance to be the least effective.
Table 5. Ranking of efficacy among materials regarding OHRQoL.
| Treatments | Position 1 | Position 2 | Position 3 | Position 4 |
|---|---|---|---|---|
| BUR+LA | 0.2382 | 0.0268 | 0.0341 | 0.7009 |
| BUR | 0.2065 | 0.3723 | 0.3364 | 0.848 |
| HI | 0.1153 | 0.2648 | 0.4522 | 0.1677 |
| UCT | 0.4400 | 0.3361 | 0.1773 | 0.0466 |
Bold values are the highest values in the selected columns.
Pain
From the seven studies assessing pain, six of them presented enough data for a quantitative analysis. Regarding the evaluation criteria, two studies used a yes/no question, two of them applied the Wong-Baker facial scale and two studies used the Visual Analogue Pain Scale. Both scales are 5-point measurements whose results were dichotomized as presence and absence of pain. The treatments compared were restorative treatment using rotary instruments and local anesthesia (BUR+LA), restorative treatment using rotary instruments (BUR), restorative treatment using hand instruments and adhesive material (HI), restorative treatment using chemomechanical agents (CHM), hall technique (HT) and ultraconservative restorative treatment (UCT). The relative risk (RR) was calculated using the percentage of pain reported for each treatment. The direct comparisons are illustrated in Fig 3C. The remaining comparisons were performed indirectly using a fixed effects model. There was only one study per pair of comparison. No statistical difference was found between treatments.
In relation to the ranking probability regarding pain, treatment (CHM) would be ranked as the low painful treatment while treatment (HT) would be the most painful (Table 6). However, the probabilities are low, 58% and 39% respectively.
Table 6. Ranking of efficacy among treatments regarding pain.
| Treatments | Position 1* | Position 2 | Position 3 | Position 4 | Position 5 | Position 6* |
|---|---|---|---|---|---|---|
| BUR+LA | 0.0010 | 0.0257 | 0.0632 | 0.2955 | 0.3365 | 0.2779 |
| BUR | 0.2161 | 0.3185 | 0.2534 | 0.0721 | 0.0571 | 0.0825 |
| HI | 0.1517 | 0.3983 | 0.2920 | 0.0709 | 0.0587 | 0.0281 |
| CHM | 0.5869 | 0.1203 | 0.2214 | 0.0359 | 0.0225 | 0.0129 |
| HT | 0.0171 | 0.0549 | 0.0790 | 0.1848 | 0.2702 | 0.3937 |
| UCT | 0.0270 | 0.0821 | 0.0907 | 0.3405 | 0.2548 | 0.2046 |
Bold values are the highest values in the selected columns.
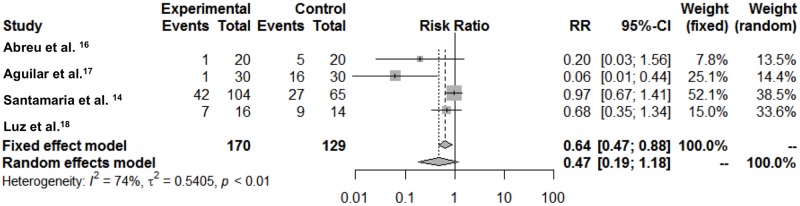
A direct meta-analysis was additionally performed after dichotomizing the groups in treatments using rotary instruments and local anesthesia versus treatment without the use of rotary instruments or local anesthesia (Fig 4). From the 7 studies included in the quantitative analysis, only 4 compared dichotomized groups. High heterogeneity was found (I = 74%, 95%CI 27.6%; 90.7%), thus the random model was considered the best choice. Although no association was found using the random model, it seems to be a trend for treatments without rotary instruments and local anesthesia to be less reported as painful.
Fig 4. Forest plot comparing treatments with versus without rotary instruments and local anesthesia regarding self-reported pain.
Discussion
Despite the historical limited development and utilization of patient-reported outcome (PROs) in clinical dentistry, some important steps have been taken to report data regarding PROs[35]. This evolution seems logic considering that unpleasant dental experiences have a large range of consequences since patient apprehension[36] until dental treatment avoidance[37]. Regarding the young population, children aging 3 years and older are able to effectively communicate emotional and physical experiences despite the clear differences in their developmental skills[38] which enable them to participate in the decision-making process. In this context, it is clear to understand why the sample of all included studies were composed by children from 3 years old and up even though no age-related exclusion criteria were applied. Considering the availability of evidence-based restorative treatment options[39] and the shorter lifetime of the primary dentition, choosing a patient-friendly treatment may be the key for a successful dental management of this population.
Studies have demonstrated that there is a weak to moderate agreement between professional and children regarding some patient-based outcomes, such as pain and anxiety[40–41] and a moderate concordance between parents and children[42]. Hence, clinical observation or parents-reported measures are considered unreliable methods[43–44]. On the other hand, valid and trustworthy information can be obtained from both parents and children when measuring OHRQoL[45]. This justifies the exclusive use of patient-reported studies, excepting those regarding OHRQoL, in this systematic review.
Unfortunately, the increasing number of studies did not imply in strong and conclusive evidence. The risk of bias assessment demonstrated the lack of rigor in the publications reporting patient outcomes measures. In most of the clinical studies, it lacks information about allocation concealment and blinding of outcome assessment, parameters which could greatly influence a self-reported outcome.
The great variability of treatments and measurements regarding the same outcome limited to merger the data. Therefore, it was not possible to fully perform the MTC, since there was no direct and indirect evidence for pairwise comparison of neither outcome. However, the MTC still contributed significantly with the results, as not only increased the possibilities of comparisons among treatments for all three outcomes, but it also detected differences that had not been observed in the direct analysis of anxiety. Children reported significant higher levels of anxiety when treatments using local anesthesia and rotary instruments were performed. This result does not corroborate with a recent systematic review which demonstrated that there is no difference between ART and conventional treatment regarding this outcome[19]. However, this study only performed direct comparisons which is not enough to detect this difference with the current scientific data available.
The higher levels of anxiety related to conventional restorative procedures can be explained by the use of high-speed handpiece with or without needle/anesthesia (BUR+LAR) which are triggering factors often related to adverse emotional reactions in children in the dental office[46]. In this context, less invasive treatments such as ART (HI) can be indicated as first choice treatment because it does not require the use of these devices[47].
Regarding pain, when dichotomizing treatments between those that use or do not use rotary instruments and local anesthesia, a trend in favor of procedures that do not use these devices was found. However, it was observed through the Forest Plot that the studies showing a protective effect have smaller sample sizes. Due to the clinical heterogeneity of pain, it is possible that the protective effect is attenuated in larger studies.
On the other hand, some results regarding both pain and quality of life that had presented statistical difference in the direct analysis lost the significance in the indirect comparisons. This may represent only a statistical effect, since indirect analysis enlarge the confidence interval as a result of the mathematical modeling[24]. However, it may also be related to the impossibility of generalizing the studies’ findings. The few data available are insufficient to come to a conclusion about this divergence.
There is an evident need for high-quality prospective PRO studies in restorative pediatric dentistry. Randomized clinical trials using PRO as primary outcomes after performing an appropriate and powerful sample size calculation could bring important contributions to the current scientific literature. Yet, following a protocol for reporting PRO[1] may improve the quality of data produced. Based on the current evidence, we can conclude that anxiety and pain are directly related with more invasive restorative treatments. On the other hand, quality of life is not improved regardless the type of restorative treatment. Further well-designed prospective studies regarding PROs in children are still necessary.
Supporting information
(DOC)
Acknowledgments
The authors would like to thank the São Paulo Research Foundation—FAPESP (grant #2015/11356–6) and CNPq for financial support. Daniela Prócida Raggio is a recipient of the Research Productivity Scholarship–CNPq (303109/2012-2). We also acknowledge all participants in the postgraduate Paediatric Dentistry Seminar and in the Implementation of Scientific Evidence: Systematic Review and Meta-Analysis course of FOUSP (Faculty of Dentistry, University of São Paulo) for the constructive criticism provided.
Data Availability
All data collection files are available from the Mendeley Data database: http://dx.doi.org/10.17632/47x4scy37y.1.
Funding Statement
São Paulo Research Foundation — FAPESP (grant #2015/11356–6) granted Nathalia de Miranda Ladewig with a PhD scholarship. Daniela Prócida Raggio is a recipient of the Research Productivity Scholarship – CNPq (303109/2012-2).
References
- 1.Calvert M, Blazeby J, Altman DG, Revicki DA, Moher D, Brundage MD et al. Reporting of patient-reported outcomes in randomized trials: the CONSORT PRO extension. JAMA 2013;309(8):814–22. 10.1001/jama.2013.879 [DOI] [PubMed] [Google Scholar]
- 2.Deshpande PR, Rajan S, Sudeepthi BL, Abdul Nazir CP. Patient-reported outcomes: A new era in clinical research. Perspectives in Clinical Research. 2011;2(4):137–144. 10.4103/2229-3485.86879 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cano SJ, Browne JP, Lamping DL. Patient-based measures of outcome in plastic surgery: current approaches and future directions. Br J Plast Surg 2004;57(1):1–11. [DOI] [PubMed] [Google Scholar]
- 4.Cano SJ, Klassen A, Pusic AL. The science behind quality-of-life measurement: a primer for plastic surgeons. Plast Reconstruct Surg 2009;123(3):98e–106e. [DOI] [PubMed] [Google Scholar]
- 5.Fleming PS, Koletsi D, O’Brien K, Tsichlaki A, Pandis N. Are dental researchers asking patient-important questions? A scoping review. J Dent. 2016;49:9–13. 10.1016/j.jdent.2016.04.002 [DOI] [PubMed] [Google Scholar]
- 6.Noonan VK, Lyddiatt A, Ware P, Jaglal SB, Riopelle RJ, Bingham CO 3rd, et al. Montreal Accord on patient-reported outcomes use series-paper 3: patient-reported outcomes can facilitate shared decision-making and guide self-management. J Clin Epidemiol. 2017: S0895-4356(17)30413-4. [DOI] [PubMed] [Google Scholar]
- 7.Thomson WM, Broadbent JM, Locker D, Poulton R. Trajectories of dental anxiety in a birth cohort. Comunity Dent Oral Epidemiol. 2009; 37:209–219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dhar V, Hsu KL, Coll JA, Ginsberg E, Ball BM Chhibber S, et al. Evidence-based update of pediatric dental restoration procedures: dental materials. Journal of Clinical Pediatric Dentistry 2015; 39(4): 303–10. doi: 10.17796/1053-4628-39.4.303 [DOI] [PubMed] [Google Scholar]
- 9.Roeleveld AC, Van Amerongen WE, Mandari GJ. Influence of residual caries and cervical gaps on the survival rate of Class II glass ionomer restorations. Eur. Arch. Paediatr. Dent. 2006; 7(2): 85–91. [DOI] [PubMed] [Google Scholar]
- 10.Leal SC, Bronkhorst EM, Fan M, Frencken JE. Effect of different protocols for treating cavities in primary molars on the quality of life of children in Brazil—1 year follow-up. Int Dent J. 2013;63(6):329–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Arrow P, Klobas E. Child oral health-related quality of life and early childhood caries: a non-inferiority randomized control trial. Aust Dent J. 2016;61(2):227–35. 10.1111/adj.12352 [DOI] [PubMed] [Google Scholar]
- 12.Mickenautsch S, Frencken JE, van’t HM. Atraumatic restorative treatment and dental anxiety in outpatients attending public oral health clinics in South Africa. J Public Health Dent. 2007;67(3):179–84. [DOI] [PubMed] [Google Scholar]
- 13.Topaloglu-Ak A, Eden E, Frencken JE. Perceived dental anxiety among schoolchildren treated through three caries removal approaches. J Appl Oral Sci. 2007;15(3):235–40. 10.1590/S1678-77572007000300015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Santamaria RM, Innes NP, Machiulskiene V, Evans DJ, Alkilzy M, Splieth CH. Acceptability of different caries management methods for primary molars in a RCT. Int J Paediatr Dent. 2015;25(1):9–17. 10.1111/ipd.12097 [DOI] [PubMed] [Google Scholar]
- 15.Louw AJ, Sarvan I, Chikte UM, Honkala E. One-year evaluation of atraumatic restorative treatment and minimum intervention techniques on primary teeth. SADJ. 2002;57(9):366–71. [PubMed] [Google Scholar]
- 16.de Menezes Abreu DM, Leal SC, Frencken JE. Self-report of pain in children treated according to the atraumatic restorative treatment and the conventional restorative treatment—a pilot study. J Clin Pediatr Dent. 2009;34(2):151–5. [DOI] [PubMed] [Google Scholar]
- 17.Aguilar AA, Rios Caro TE, Huamán Saavedra J, França CM, Fernandes KP, Mesquita-Ferrari RA, et al. Atraumatic restorative treatment: a dental alternative well-received by children. Rev Panam Salud Publica. 2012;31(2):148–52. [PubMed] [Google Scholar]
- 18.Luz PB, Barata JS, Meller CR, Slavutsky SMB, de Araujo FB. ART acceptability in children: a randomized clinical trial. Rev Fac Odontol. Porto Alegre. 2012;53(1):27–31. [Google Scholar]
- 19.Simon AK, Bhumika TV, Nair NS. Does atraumatic restorative treatment reduce dental anxiety in children? A systematic review and meta-analysis. Eur J Dent. 2015;9(2):304–9. 10.4103/1305-7456.156841 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hesse D, de Araujo MP, Olegário IC, Innes N, Raggio DP, Bonifácio CC. Atraumatic Restorative Treatment compared to the Hall Technique for occluso-proximal cavities in primary molars: study protocol for a randomized controlled trial. Trials. 2016;17:169 10.1186/s13063-016-1270-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ladewig NM, Sahiara CS, Yoshioka L, Olegário IC, Floriano I, Tedesco TK, et al. Efficacy of conventional treatment with composite resin and atraumatic restorative treatment in posterior primary teeth: study protocol for a randomised controlled trial. BMJ Open. 2017;10:7(7):e015542 10.1136/bmjopen-2016-015542 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JPA, et al. The PRISMA Statement for Reporting Systematic Reviews and Meta-Analyses of Studies That Evaluate Health Care Interventions: Explanation and Elaboration. PLoS Med. 2009;6(7): e1000100 10.1371/journal.pmed.1000100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sterne JA, Gavaghan D, Egger M. Publication and related bias in meta-analysis: power of statistical tests and prevalence in the literature. J Clin Epidemiol. 2000;53(11):1119–29. [DOI] [PubMed] [Google Scholar]
- 24.Jansen JP, Crawford B, Bergman G, Stam W. Bayesian meta-analysis of multiple treatment comparisons: an introduction to mixed treatment comparisons. Value Health. 2008;11(5):956–64. 10.1111/j.1524-4733.2008.00347.x [DOI] [PubMed] [Google Scholar]
- 25.Spiegelhalter DJ, Best NG, Carlin BP, van der Linde A. Bayesian measures of model complexity and fit. J R Stat Soc Ser B (Statistical Methodol). 2002;64:583–639. [Google Scholar]
- 26.Jansen JP, Fleurence R, Devine B, Itzler R, Barrett A, Hawkins N, et al. Interpreting Indirect Treatment Comparisons and Network Meta-Analysis for Health-Care Decision Making: Report of the ISPOR Task Force on Indirect Treatment Comparisons Good Research Practices: Part 1. Value Heal. 2011;14:417–428. [DOI] [PubMed] [Google Scholar]
- 27.van Bochove JA, van Amerongen WE. The influence of restorative treatment approaches and the use of local analgesia, on the children’s discomfort. Eur Arch Paediatr Dent. 2006. March;7(1):11–6. [DOI] [PubMed] [Google Scholar]
- 28.Innes NP, Evans DJ, Stirrups DR. The Hall Technique; a randomized controlled clinical trial of a novel method of managing carious primary molars in general dental practice: acceptability of the technique and outcomes at 23 months. BMC Oral Health. 2007;7:18 10.1186/1472-6831-7-18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mustafa O, Parekh S, Ashley P, Anand P. Post-operative pain and anxiety related to dental procedures in children. Eur J Paediatr Dent. 2013;14(4):289–94. [PubMed] [Google Scholar]
- 30.Arrow P, Klobas E. Minimal intervention dentistry for early childhood caries and child dental anxiety: a randomized controlled trial. Aust Dent J. 2017;62(2):200–207. 10.1111/adj.12492 [DOI] [PubMed] [Google Scholar]
- 31.Maciel R, Salvador D, Azoubel K, Redivivo R, Maciel C, da Franca C, et al. The opinion of children and their parents about four different types of dental restorations in a public health service in Brazil. Eur Arch Paediatr Dent. 2017;18(1):25–29. 10.1007/s40368-016-0262-8 [DOI] [PubMed] [Google Scholar]
- 32.Lakshmi SP, Sahana S, Vasa AAK, Madu GP, Bezawada S, Deepika M. Atraumatic restorative treatment vs. Hall technique for occlusoproximal lesions in primary dentition-an in vivo study. Journal of Clinical and Diagnostic Research 2018;12(2):ZC09–ZC13. [Google Scholar]
- 33.Barreto KA, dos Prazeres LDKT, Lima DSM, Redivivo RMMP, Colares V. Children’s anxiety during dental treatment with minimally invasive approaches: Findings of an analytical cross-sectional study. Brazilian Rsearch in Pediatric Dentistry and Integrated Clinic 2017;17(1):e3146. [Google Scholar]
- 34.Tavares RNM, Zanin L, Flório FM. Pain and anxiety in children receiving atraumatic and conventional restorative dental treatment: a randomized clinical study. Bioscience Journal 2018;34(1):251–259. [Google Scholar]
- 35.Rosen EB, Donoff RB, Riedy CA. U.S. Dental School Deans’ Views on the Value of Patient-Reported Outcome Measures in Dentistry. J Dent Educ. 2016. June;80(6):721–5. . [PubMed] [Google Scholar]
- 36.Banerjee A, Watson TF, Kidd EA. Dentine caries excavation: A review of current clinical techniques. Br Dent J. 2000;188:476–82. [DOI] [PubMed] [Google Scholar]
- 37.Cohen SM, Fiske J, Newton JT. The impact of dental anxiety on daily living. Br Dent J. 2000; 189:385–390. [DOI] [PubMed] [Google Scholar]
- 38.Woolley ME, Bowen GL, Bowen NK. Cognitive pretesting and the developmental validity of child self-report instruments: theory and applications. Res Soc Work Pract. 2004;14:191–200. 10.1177/1049731503257882 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tedesco TK, Calvo AF, Lenzi TL, Hesse D, Guglielmi CA, Camargo LB, et al. ART is an alternative for restoring occlusoproximal cavities in primary teeth—evidence from an updated systematic review and meta-analysis. Int J Paediatr Dent. 2017;27(3):201–209. 10.1111/ipd.12252 [DOI] [PubMed] [Google Scholar]
- 40.Buchanan H, Niven N. Further evidence for the validity of the Facial Image Scale. Inter J of Paediatr Dent. 2003;13:368–369. [DOI] [PubMed] [Google Scholar]
- 41.Barros L, Buchanan H. Correspondence between dentist and child ratings of dental anxiety in Portugal: a preliminary study. Rev Port Estomatol Med Dent Cir Maxilofac. 2011;52:13–15. [Google Scholar]
- 42.Gustafsson A, Arnrup K, Broberg AG, Bodin L, Berggren U. Child dental fear as measured with the Dental Subscale of the Children’s Fear Survey Schedule: the impact of referral status and type of informant (child versus parent). Community Dent Oral Epidemiol. 2010;38(3):256–266. 10.1111/j.1600-0528.2009.00521.x [DOI] [PubMed] [Google Scholar]
- 43.Luoto A, Tolvanen M, Rantavuori K, Pohjola V, Lahti S. Can parents and children evaluate each other’s dental fear? Eur J Oral Sci. 2010;118(3):254–8. 10.1111/j.1600-0722.2010.00727.x [DOI] [PubMed] [Google Scholar]
- 44.Porrit J, Buchanan H, Hall M, Gilchrist F, Marshman Z. Assessing children’s dental anxiety: a systematic review of current measures. Community Den Oral Epidemiol. 2013;41(2):130–42. [DOI] [PubMed] [Google Scholar]
- 45.Barbosa TS, Gavião MB. Oral health-related quality of life in children: part III. Is there agreement between parents in rating their children’s oral health-related quality of life? A systematic review. Int J Dent Hyg. 2008;6(2):108–13. 10.1111/j.1601-5037.2007.00271.x [DOI] [PubMed] [Google Scholar]
- 46.Walsh LJ. Anxiety prevention: implementing the 4 S principle in conservative dentistry. Auxilliary. 2007;17:24–6. [Google Scholar]
- 47.Frencken JE, Pilot T, Songpaisan Y, Phantumvait P. Atraumatic restorative treatment (ART): Rationale, technique, and development. Journal of Public Health Dentistry. 1996; 56(3): 135–140. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOC)
Data Availability Statement
All data collection files are available from the Mendeley Data database: http://dx.doi.org/10.17632/47x4scy37y.1.