Abstract
Background
Vitamin C deficiency is prevalent in adults with heart failure (HF). Little is known about the relationship of dietary vitamin C deficiency with health outcomes in adults with HF.
Objective
To determine the relationships of vitamin C deficiency measured at baseline, with health-related quality of life (HRQOL), and cardiac event-free survival in patients with HF measured 1 year later.
Method
A total of 251 patients with HF completed a 4-day food diary. Dietary vitamin C deficiency was defined as daily intake below the estimated average requirement (EAR) from the Institute of Medicine of 75 mg/day for men and 60 mg/day for women. HRQOL was assessed using the Minnesota Living with Heart Failure Questionnaire at 12 months. Patients were followed for a median of 1 year to determine time to first event of cardiac-related hospitalization or death. Data were analyzed by hierarchical linear and Cox proportional hazards regressions.
Results
One hundred patients (40%) had vitamin C deficiency. Dietary vitamin C deficiency was associated with poorer HRQOL at 12 months (Beta=.16, P=.02) after controlling for demographic and clinical variables. During the follow-up period, 59 patients (24%) had cardiac events. In Cox regression, vitamin C deficiency predicted shorter cardiac event-free survival after adjusting for the same covariates (HR=1.95, 95%CI=1.08–3.51).
Conclusion
Vitamin C deficiency was associated with poorer HRQOL and shorter cardiac event-free survival in patients with HF. The findings suggest that encouraging HF patients to consume a diet rich in fruits/vegetables to prevent vitamin C deficiency may lead to better health outcomes.
Keywords: Dietary vitamin C deficiency, heart failure, quality of life, cardiac event-free survival
Although significant advancements in morbidity and mortality have resulted from improved medical treatment, heart failure (HF) remains a prevalent, morbid, and costly condition with a high early mortality rate.1–6 Currently, 6.5 million Americans have HF.1–3 Even after optimum medical treatment, up to 84% patients with HF remain symptomatic;7, 8 these symptoms are associated with decreased health-related quality of life (HRQOL), as well as frequent hospitalization.9, 10 About half of patients with HF are readmitted within 6 months of hospital discharge for exacerbations of HF.11, 12
Mean serum vitamin C levels are significantly lower in patients with HF compared to those with other chronic conditions13–15 and up to 39% of patients are reported to have a vitamin C dietary deficiency.14 Consequences of low serum vitamin C include increased oxidative stress and decreased physical performance.16 In a large study of community-dwelling older people, low serum vitamin C concentrations were associated with all-cause and cardiac-related mortality.17 Previous studies have shown that higher vitamin C levels are associated with better endothelial cell and immune system function, and lower risk for cardiovascular disease in healthy adults.18–21 In patients with HF, serum vitamin C levels are positively correlated with cardiac function (measured by left ventricular ejection fraction [LVEF]).22 Furthermore, those with dietary vitamin C deficiency (i.e., those who consumed less than 100 mg/day of vitamin C) had about two times the risk of experiencing a cardiac event in a recent prospective study of Korean patients with HF.14
Little is known about the effects of dietary vitamin C deficiency on outcomes important to patients with HF. There are no studies of vitamin C deficiency and HRQOL and the relationship between vitamin C intake and cardiac event-free survival has only been examined in one study of patients with HF in Korea.14 Accordingly, the purpose of this study was to determine the relationship of dietary vitamin C deficiency with HRQOL and cardiac event-free survival in patients with HF. We hypothesized that patients with HF and dietary vitamin C deficiency would have poorer HRQOL and shorter cardiac event-free survival than patients with HF and no deficiency.
Methods
Study Design
This was a secondary data analysis of a longitudinal study in which patients’ sociodemographic (e.g., age, gender, race/ethnicity) and clinical (e.g., comorbidities [diabetes, hypertension], left ventricular ejection fraction [LVEF], New York Heart Association [NYHA], body mass index [BMI], medications) data were collected at baseline by patient interview and medical record review. Dietary vitamin C intake/deficiency, as well as total energy intake and vegetable and fruit food serving size were determined from a 4-day food diary. HRQOL was assessed by patient interview at 12 months by phone. Cardiac events were followed by patient/family interview and hospital medication record review.
Samples and Setting
Detailed eligibility criteria and recruitment methods have been published previously.8 Patients were recruited from clinics associated with three large community hospitals or academic medical centers in 3 Midwestern states. Patients were included if they had a confirmed diagnosis of chronic HF. Patients were excluded if they had a terminal illness or obvious cognitive impairment that precluded provision of informed consent.
Measures
Vitamin C deficiency
Dietary vitamin C intake was defined as the averaged 4 day intake from food diaries (3 weekdays and 1 weekend day), a method that is widely-used to measure nutritional intake and dietary patterns.23 The diets from the 4-day food diary were analyzed using Nutrition Data Systems-R (NDS-R) software (NCC, University of Minnesota).24, 25 The NDS-R is a valid, widely used program to analyze dietary intake to determine nutrient deficiency in multiple patient populations.24, 25 Dietary vitamin C deficiency was defined as daily intake below the estimated average requirement (EAR) of 75 mg/day for men and 60 mg/day for women from the Institute of Medicine.26
Health-related quality of life (HRQOL)
The Minnesota Living with Heart Failure questionnaire (MLHFQ) is a measure of HRQOL that assesses the patient’s perceptions of the influence of HF on physical and emotional aspects of life.27, 28 The 21 items are summed with higher scores indicating worse HRQOL. Researchers have demonstrated evidence for validity (MLHFQ scores were associated with survival) and reliability (Cronbach’s alphas ranging from 0.88 to 0.93), and the instrument has been widely used to measure HRQOL in patients with HF.27–29 In this study, the Cronbach’s alpha was 0.95. The MLHFQ has physical (item # 2–7, 12, and 13) and emotional (item # 17–21) subscales to measure physical and emotional aspects of HRQOL. The Cronbach’s alphas for the subscales in this study were 0.95 and 0.93 respectively.
Cardiac event-free survival
The outcome variable was the composite end-point of time to the first cardiac event, whether it was a cardiac-related hospitalization, or death. Data on cardiac events were collected monthly by patient phone calls, hospital record review, and review of death certificates. We calculated number of days from baseline to the first cardiac event during the follow-up period.
Covariates
Age, gender, race/ethnicity, education, financial status, left ventricular ejection fraction (LVEF), New York Heart Association (NYHA) functional class, body mass index (BMI), comorbidity (diabetes, hypertension), and medication use (angiotensin-converting-enzyme inhibitor [ACEI] and beta-blocker) which might influence health outcomes (HRQOL and cardiac event-free survival) were collected as covariates.8, 30, 31 We also assessed patients’ total energy intake, fruit and vegetable serving size using the 4-day food diary as these might influence dietary vitamin C intake and deficiency.32 Patients’ sociodemographic and clinical characteristics were collected from the medical record and patient interview. Patients’ NYHA functional class was determined by a structured patient interview at baseline.33 Based on patients’ reports of symptoms associated with performing their usual activities, they were assigned to Class I [ordinary activity causes no symptoms] to IV [symptoms occur at rest]).33
Procedure
Permission to conduct the study was obtained from the Institutional Review Board (IRB) at all sites. A trained research nurse visited patients in their home to explain the study and obtain informed, written consent. Patients were provided with digital scales and face-to-face instructions with return demonstrations on how to use digital scales to weigh each food item and record in food diary. Written instructions were given also provided. The patient completed food diaries on 3 weekdays and 1 weekend day prior to baseline measurements according to patent’s schedule (usually Wednesday through Saturday). Patients did not record food diaries during any week that included a holiday or other special occasion. The research nurse contacted patients by phone on Day 1 to remind them to start recording the food diary and to verify accuracy of recording the first meal. The 4-day food diary was reviewed by a registered dietitian to verify portions, food preparation, and complete any missing data during the baseline visit to the Clinical Research Center. Patients’ sociodemographic and clinical data were collected by interview and medical record review at baseline. HRQOL was assessed by patient interview at 12 months by phone. Patients were followed to collect data on cardiac events (cardiac hospitalization or death).
Data Management and Analysis
All data analyses were done using IBM SPSS version 24.0 (Armonk, NY); a significance level of .05 was determined a priori. Data analysis began with a descriptive examination of all variables, including frequency distributions, means, standard deviations, medians, as appropriate to the level of measurement of the variables. Student’s independent t-tests and chi-squares were used to compare differences between dietary vitamin C adequacy and deficiency groups.
We used hierarchical linear regression to examine the relationship between dietary vitamin C deficiency and HRQOL (total scores, as well as scores for physical and emotional subscales) with and without potential confounding covariates: age, gender, LVEF, NYHA functional class, ACEI use, and beta-blocker use, BMI, hypertension, diabetes, and total energy intake. The Kaplan-Meier with log-rank test was used to compare the time to cardiac event-free survival between patients with and without vitamin C deficiency. Hierarchical Cox proportional hazards regression modeling was used to assess the time to first cardiac event between patients with and without vitamin C deficiency and with and without adjusting for same covariates listed above.
Results
Patient Characteristics
The sample included 251 patients with a mean age of 61 years and an average left ventricular ejection fraction of 34.4%. (Table 1–2). The most common HF etiology was ischemic heart disease. The majority of patients were male, Caucasians, and married. About half of the patients had NYHA III/IV. More than one quarter of patients (26%) reported not having enough income to make ends meet.
Table 1.
Demographic and clinical characteristics of participants—frequency (N=251)
| Characteristics | Number (%) |
|---|---|
|
| |
| Female Gender | 83 (33.1%) |
| Race/ethnicity: Caucasian | 185 (73.7%) |
| Marital status | |
| Married/cohabitate | 146 (58.2%) |
| Financial status | |
| Comfortable | 62 (24.7%) |
| Enough to make ends meet | 123 (49%) |
| Not enough to make ends meet | 66 (26.3%) |
| Etiology | |
| Ischemic | 117 (47.6%) |
| Idiopathic | 49 (19.9%) |
| Hypertensive | 36 (14.6%) |
| Other (e.g., alcoholic) | 44 (17.9%) |
| NYHA | |
| Class I/II | 137 (54.8%) |
| Class III/IV | 113 (45.2%) |
| ACE inhibitor use | 167 (68.4%) |
| Beta-blocker use | 221 (88.8%) |
| Hypertension | 173 (69.8%) |
| Diabetes | 89 (35.5%) |
NYHA = New York Heart Association functional classification
Table 2.
Demographic and clinical characteristics of participants—mean (N=251)
| Characteristics | Mean (SD) |
|---|---|
| Age | 61.5 (12.0) |
| Education, years | 13.9 (3.2) |
| LVEF, % | 34.4 (13.1) |
| Body Mass Index | 30.3 (7.0) |
| Total energy intake, kcal/day | 1853.9 (640.6) |
| Total MLHFQ scores | 42.3 (25.2) |
| Physical MLHFQ scores | 18.7 (11.2) |
| Emotional MLHFQ scores | 8.5 (7.4) |
SD, standard deviation.
LVEF = Left Ventricular Ejection Fraction.
MLHFQ score: higher score reflects greater poorer health-related quality of life
Dietary Vitamin C deficiency
The median dietary vitamin C intake was 90 mg/day (± 495 mg), which was higher than the recommended dietary vitamin C intake for both male (75 mg/day) and female adults (60 mg/day). The range of dietary vitamin C intake was from 1.1 to 6199 mg/day. One hundred fifty-one patients (60%) consumed recommended amounts of dietary vitamin C whereas one hundred patients (40%) had dietary vitamin C deficiency. There were no gender nor race/ethnicity differences in dietary vitamin C deficiency.
Dietary Vitamin C Deficiency and Health-related Quality of Life
The mean score for the MLHFQ at 12 months was 42.3 (± 24.5). The mean scores of the physical and emotional aspects of the MLHFQ at 12 months were 18.8 (± 11.1) and 8.4 (± 7.3), respectively. Patients with dietary vitamin C deficiency had higher total MLHFQ scores compared to those with adequate dietary vitamin C intake (49.3 vs. 37.9, t = −3.251, P =0.001), indicating poorer HRQOL in patients with dietary vitamin C deficiency. Specifically, patients with dietary vitamin C deficiency had higher scores in the physical subscale of the MLHFQ than those with adequate dietary vitamin C intake (22.2 vs. 16.5, t = −3.699, P <0.001), indicating more physical symptoms in patients with dietary vitamin C deficiency. There was no difference between groups in the emotional subscale of the MLHFQ (t = −1.267, P=0.21). The hierarchical multiple linear regression model for prediction of total MLHFQ scores is shown in Table 3. Dietary vitamin C deficiency and higher (worse) NYHA functional class were associated with higher total MLHFQ (i.e., poorer HRQOL; F = 4.749, P < 0.001). Similarly, dietary vitamin C deficiency and NYHA functional class predicted worse physical aspect of the MLHFQ (F = 5.175, P < 0.001). Dietary vitamin C deficiency did not predict the emotional aspect of the MLHFQ (P = 0.69).
Table 3.
Hierarchical Multiple Regression: Dietary Vitamin C Deficiency on Health-related Quality of Life in Patients with Heart Failure* (N = 251)
| Variable | Standardized β | Significance |
|---|---|---|
|
| ||
| * Step 1: | ||
| Gender | −.080 | .280 |
| Age | −.151 | .031 |
| Left ventricular ejection fraction (%) | .019 | .798 |
| NYHA | .317 | <.001 |
| ACEI user | −.112 | .107 |
| Beta-blocker user | −.091 | .180 |
| Body Mass Index | .094 | .207 |
| Hypertension | .124 | .075 |
| Diabetes | .034 | .629 |
| Total energy intake (kcal/day) | −.069 | .341 |
| ** Step 2: | ||
| Gender | −.064 | .382 |
| Age | −.127 | .068 |
| Left ventricular ejection fraction (%) | .032 | .655 |
| NYHA | .313 | <.001 |
| ACEI user | −.125 | .069 |
| Beta-blocker user | −.086 | .200 |
| Body Mass Index | .075 | .314 |
| Hypertension | .122 | .074 |
| Diabetes | .045 | .513 |
| Total energy intake (kcal/day) | −.046 | .522 |
| Dietary vitamin C deficiency | .159 | .020 |
ACEI = angiotensin-converting-enzyme inhibitor; NYHA = New York Heart Association
F=4.563, p < .001;
F=4.749, p < .001
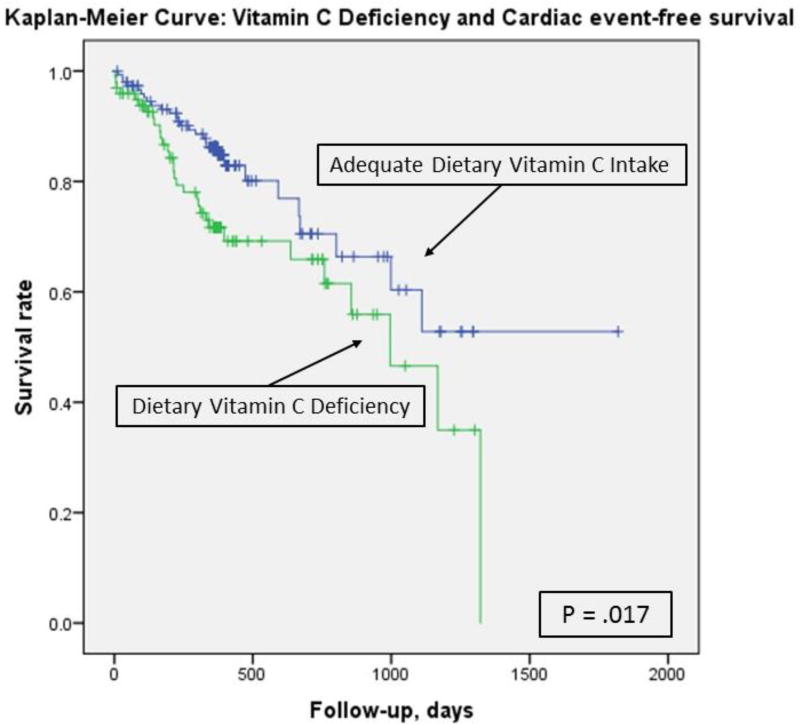
Dietary Vitamin C Deficiency and Cardiac Event-free Survival
There were 59 cardiac events (3 cardiac deaths and 56 cardiac hospitalizations) during the follow-up period, with 31 events in patients with dietary vitamin C deficiency and 28 events in those who had adequate dietary vitamin C intake. Kaplan-Meier plots and log-rank tests demonstrated that cardiac event-free survival was significantly worse in patients who had dietary vitamin C deficiency (P = 0.017; Figure 1). In unadjusted Cox proportional hazard regression, patients with dietary vitamin C deficiency had a shorter cardiac event-free survival compared with those with dietary vitamin C adequacy (HR: 1.85, 95% CI [1.11, 3.09], P = 0.019). When adjusting for age, gender, LVEF, NYHA, ACEI use, beta-blocker use, BMI, hypertension, diabetes, and total energy intake, dietary vitamin C deficiency remained a significant predictor of cardiac event-free survival (HR: 1.95, 95% CI [1.08, 3.51], P = 0.026, Table 4).
Figure 1.
Dietary Vitamin C Deficiency and Cardiac Event-free Survival
Patients with adequate dietary vitamin C intake had better cardiac event-free survival than those with dietary vitamin C deficiency.
Table 4.
Cox Regression: Dietary Vitamin C Deficiency on Cardiac Event-free Survival in Patients with Heart Failure* (N = 251)
| Variable | Hazard ratio | 95% CI | Significance |
|---|---|---|---|
|
| |||
| *Without covariate adjustment | |||
| Dietary vitamin C deficiency | 1.85 | 1.11–3.09 | .019 |
|
| |||
| **With covariate adjustment | |||
| Gender | .489 | .238–1.004 | .051 |
| Age | 1.005 | .98–1.03 | .697 |
| Left ventricular ejection fraction (%) | .991 | .967–1.016 | .487 |
| NYHA | 1.381 | .989–1.929 | .058 |
| ACEI user | 1.022 | .517–2.02 | .950 |
| Beta-blocker user | 1.016 | .4–2.584 | .973 |
| Body Mass Index, % | 1.0 | .954–1.049 | .987 |
| Hypertension | 1.918 | .951–3.872 | .069 |
| Diabetes | .987 | .524–1.859 | .967 |
| Total energy intake (kcal/day) | 1.0 | .999–1.0 | .333 |
| Dietary vitamin C deficiency | 1.95 | 1.083–3.511 | .026 |
CI = confidence interval; ACEI = angiotensin-converting-enzyme inhibitor; NYHA = New York Heart Association
χ2 = 5.688, p = .017;
χ2 = 18.374, p =.073
In the adjusted model with all covariates, none of the covariates were associated with cardiac event-free survival. In each adjusted regression model, all variance inflation factors were < 1.2, suggesting no parameter distortion due to multicollinearity.
Discussion
This is the first study in patients with HF examining the relationship between dietary vitamin C and HRQOL. The findings of this study supported our hypothesis that patients with dietary vitamin C deficiency will have worse HRQOL compared with those with adequate dietary vitamin C intake. In this study, the mean score for the MLHFQ at 12 months was 42.3, which was already much higher than the MLHFQ score of 14 among the healthy older adults,34 indicating poorer HRQOL in patients with HF than healthy older adults. Patients with dietary vitamin C deficiency had higher total MLHFQ scores than those with adequate dietary vitamin C intake (49.3 vs. 37.9). Our result is in line with prior intervention studies that demonstrated vitamin C supplementation improved physical activity level,35 HRQOL, and symptoms of fatigue, insomnia, poor appetite, nausea, and pain in cancer patients.36–38
Our results also showed that dietary vitamin C deficiency was associated with a shorter cardiac event-free survival compared to vitamin C adequacy. The finding is consistent with a similar prospective study in Korean patients with HF.14 Although the research on the effect of vitamin C to reduce cardiac events is mixed, a large body of evidence shows beneficial effects of vitamin C on health outcomes, such as reducing cold incidence in healthy adults;35 alleviating a number of cancer- and chemotherapy-related symptoms (e.g., fatigue, loss of appetite) in cancer patients, enhancing immune system and improving recovery from infectious disease and respiratory infections.36–40 Patients with HF are more likely to have dietary vitamin C deficiency compared to those with other chronic illness.13–15 Because vitamin C is not synthesized, not stored in the body, and is readily excreted in the urine, it must be continuously replaced in the diet and supplements if necessary. In this study, forty percent of the patients with HF had dietary vitamin C deficiency. Our findings on high prevalence of vitamin C deficiency is consistent with the current literature.41 Considering the importance of dietary vitamin C intake in terms of HRQOL and cardiac event-free survival for patients with HF from observational studies (prior and our studies),14 future randomized controlled trials (RCTs) are needed to test if providing more vitamin C supplementation to those HF patients with vitamin C deficiencies improves patients’ HRQOL and impacts cardiac event-free survival.
The mechanism underlying the relationship between dietary vitamin C deficiency, poorer HRQOL, and worse cardiac event-free survival is not known. One possible explanation for this relationship in HF may be lower vitamin C leads to endothelial dysfunction which increases systemic vascular resistance and afterload leading to low cardiac output42 and subsequent HF symptoms (e.g., edema, shortness of air, and fatigue).42, 43 HF symptoms produced by low cardiac output insufficient to support patients’ activities of daily living are potential reasons for decreased HRQOL9, 10 and hospitalizations.44 Prior studies have demonstrated that higher vitamin C levels were associated with improved endothelial function.18–20 There was a significant positive correlation between cardiac function and serum vitamin C level.22 In intervention studies in patients with HF, investigators found that vitamin C supplementation increased serum vitamin C level20 and improved endothelial function.19, 20, 45 Other interventional studies provided evidence that vitamin C supplementation not only improved cardiac function,18, 46, 47 but also reduced oxidative stress20, 48 in patients with HF. Therefore, patients with dietary vitamin C deficiency may be more likely to have endothelial dysfunction, low cardiac output, more HF symptoms, poorer HRQOL, and worse cardiac event-free survival. Consistent with this hypothesis, our study showed that the physical aspect of HRQOL was significantly worse in patients with dietary vitamin C deficiency, providing evidence that patients with dietary vitamin C deficiency had more symptoms of HF (such as shortness of breath, fatigue, less physical strength to move around) that impair patients’ HRQOL. Additional research is needed to confirm this potential mechanism.
Our study has several limitations. First, dietary vitamin C intake was measured at one-time point that might not reflect habitual dietary vitamin C intake. Longitudinal and repeated measurements of dietary vitamin C intake is needed to confirm our findings. Second, dietary vitamin C intake was not confirmed using serum vitamin C concentration. Third, our sample was relatively small, mostly white, male, and married. Therefore, our findings warrant further study to confirm these results in a more diverse sample of patients with HF.
In conclusion, vitamin C deficiency was associated with poor HRQOL and shorter event-free survival. The findings suggest that patients with HF should be encouraged to consume a diet rich in fruits and vegetables to prevent dietary vitamin C deficiency while awaiting confirmation from future RCTs to confirm that vitamin C supplementation actually results in better health outcomes for patients with HF.
Acknowledgments
This study was supported by funding from the National Institute of Nursing Research of the National Institutes of Health under Award Number NR009280 (Lennie, T., PI) and the National Research Foundation of Korea (NRF) Grant by the Korean Government (NRF-2015R1D1A1A01059392) (Song, E. K., PI). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Nursing Research or the National Institutes of Health.
Footnotes
Declaration of Conflicting Interests
None.
Contributor Information
Jia-Rong Wu, University of North Carolina at Chapel Hill, School of Nursing.
Eun Kyeung Song, Department of Nursing, College of Medicine, University of Ulsan, Korea.
Debra K. Moser, University of Kentucky, College of Nursing.
Terry A. Lennie, University of Kentucky, College of Nursing.
References
- 1.Benjamin EJ, Blaha MJ, Chiuve SE, et al. Heart disease and stroke statistics-2017 update: A report from the american heart association. Circulation. 2017;135:e146–e603. doi: 10.1161/CIR.0000000000000485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mozaffarian D, Benjamin EJ, Go AS, et al. Executive summary: Heart disease and stroke statistics-2016 update: A report from the american heart association. Circulation. 2016;133:447–454. doi: 10.1161/CIR.0000000000000366. [DOI] [PubMed] [Google Scholar]
- 3.Mozaffarian D, Benjamin EJ, Go AS, et al. Heart disease and stroke statistics--2015 update: A report from the american heart association. Circulation. 2015;131:e29–322. doi: 10.1161/CIR.0000000000000152. [DOI] [PubMed] [Google Scholar]
- 4.van Jaarsveld CH, Ranchor AV, Kempen GI, et al. Epidemiology of heart failure in a community-based study of subjects aged > or = 57 years: Incidence and long-term survival. European journal of heart failure. 2006;8:23–30. doi: 10.1016/j.ejheart.2005.04.012. [DOI] [PubMed] [Google Scholar]
- 5.Young JB. The global epidemiology of heart failure. Med Clin North Am. 2004;88:1135–1143. ix. doi: 10.1016/j.mcna.2004.06.001. [DOI] [PubMed] [Google Scholar]
- 6.Roger VL, Go AS, Lloyd-Jones DM, et al. Heart disease and stroke statistics--2012 update: A report from the american heart association. Circulation. 2012;125:e2–e220. doi: 10.1161/CIR.0b013e31823ac046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jurgens CY, Moser DK, Armola R, et al. Symptom clusters of heart failure. Research in nursing & health. 2009;32:551–560. doi: 10.1002/nur.20343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lennie TA, Song EK, Wu JR, et al. Three gram sodium intake is associated with longer event-free survival only in patients with advanced heart failure. Journal of cardiac failure. 2011;17:325–330. doi: 10.1016/j.cardfail.2010.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Heo S, Doering LV, Widener J, Moser DK. Predictors and effect of physical symptom status on health-related quality of life in patients with heart failure. Am J Crit Care. 2008;17:124–132. [PubMed] [Google Scholar]
- 10.Zambroski CH, Moser DK, Bhat G, Ziegler C. Impact of symptom prevalence and symptom burden on quality of life in patients with heart failure. European journal of cardiovascular nursing : journal of the Working Group on Cardiovascular Nursing of the European Society of Cardiology. 2005;4:198–206. doi: 10.1016/j.ejcnurse.2005.03.010. [DOI] [PubMed] [Google Scholar]
- 11.Hamner JB, Ellison KJ. Predictors of hospital readmission after discharge in patients with congestive heart failure. Heart & lung : the journal of critical care. 2005;34:231–239. doi: 10.1016/j.hrtlng.2005.01.001. [DOI] [PubMed] [Google Scholar]
- 12.Krumholz HM, Chen YT, Wang Y, et al. Predictors of readmission among elderly survivors of admission with heart failure. American heart journal. 2000;139:72–77. doi: 10.1016/s0002-8703(00)90311-9. [DOI] [PubMed] [Google Scholar]
- 13.Arcand J, Floras V, Ahmed M, et al. Nutritional inadequacies in patients with stable heart failure. Journal of the American Dietetic Association. 2009;109:1909–1913. doi: 10.1016/j.jada.2009.08.011. [DOI] [PubMed] [Google Scholar]
- 14.Song EK, Kang SM. Vitamin c deficiency, high-sensitivity c-reactive protein, and cardiac event-free survival in patients with heart failure. The Journal of cardiovascular nursing. 2016 doi: 10.1097/JCN.0000000000000389. [DOI] [PubMed] [Google Scholar]
- 15.Gorelik O, Almoznino-Sarafian D, Feder I, et al. Dietary intake of various nutrients in older patients with congestive heart failure. Cardiology. 2003;99:177–181. doi: 10.1159/000071246. [DOI] [PubMed] [Google Scholar]
- 16.Paschalis V, Theodorou AA, Kyparos A, et al. Low vitamin c values are linked with decreased physical performance and increased oxidative stress: Reversal by vitamin c supplementation. European journal of nutrition. 2016;55:45–53. doi: 10.1007/s00394-014-0821-x. [DOI] [PubMed] [Google Scholar]
- 17.Fletcher AE, Breeze E, Shetty PS. Antioxidant vitamins and mortality in older persons: Findings from the nutrition add-on study to the medical research council trial of assessment and management of older people in the community. The American journal of clinical nutrition. 2003;78:999–1010. doi: 10.1093/ajcn/78.5.999. [DOI] [PubMed] [Google Scholar]
- 18.Ashor AW, Lara J, Mathers JC, Siervo M. Effect of vitamin c on endothelial function in health and disease: A systematic review and meta-analysis of randomised controlled trials. Atherosclerosis. 2014;235:9–20. doi: 10.1016/j.atherosclerosis.2014.04.004. [DOI] [PubMed] [Google Scholar]
- 19.Ellis GR, Anderson RA, Chirkov YY, et al. Acute effects of vitamin c on platelet responsiveness to nitric oxide donors and endothelial function in patients with chronic heart failure. Journal of cardiovascular pharmacology. 2001;37:564–570. doi: 10.1097/00005344-200105000-00008. [DOI] [PubMed] [Google Scholar]
- 20.Ellis GR, Anderson RA, Lang D, et al. Neutrophil superoxide anion--generating capacity, endothelial function and oxidative stress in chronic heart failure: Effects of short- and long-term vitamin c therapy. Journal of the American College of Cardiology. 2000;36:1474–1482. doi: 10.1016/s0735-1097(00)00916-5. [DOI] [PubMed] [Google Scholar]
- 21.Deruelle F, Baron B. Vitamin c: Is supplementation necessary for optimal health? Journal of alternative and complementary medicine (New York, N.Y.) 2008;14:1291–1298. doi: 10.1089/acm.2008.0165. [DOI] [PubMed] [Google Scholar]
- 22.Demirbag R, Yilmaz R, Erel O, et al. The relationship between potency of oxidative stress and severity of dilated cardiomyopathy. The Canadian journal of cardiology. 2005;21:851–855. [PubMed] [Google Scholar]
- 23.Ortega RM, Perez-Rodrigo C, Lopez-Sobaler AM. Dietary assessment methods: Dietary records. Nutricion hospitalaria. 2015;31(Suppl 3):38–45. doi: 10.3305/nh.2015.31.sup3.8749. [DOI] [PubMed] [Google Scholar]
- 24.Frediani JK, Tukvadze N, Sanikidze E, et al. A culture-specific nutrient intake assessment instrument in patients with pulmonary tuberculosis. Clinical nutrition (Edinburgh, Scotland) 2013;32:1023–1028. doi: 10.1016/j.clnu.2013.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ptomey L, Goetz J, Lee J, Donnelly J, Sullivan D. Diet quality of overweight and obese adults with intellectual and developmental disabilities as measured by the healthy eating index-2005. Journal of developmental and physical disabilities. 2013;25 doi: 10.1007/s10882-013-9339-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Institute of Medicine (US) Subcommittee on Interpretation and Uses of Dietary Reference Intakes; Institute of Medicine (US) Standing Committee on the Scientific Evaluation of Dietary Reference Intakes. DRI Dietary Reference Intakes: Applications in Dietary Assessment. Washington (DC): National Academies Press (US); 2000. Using the Estimated Average Requirement for Nutrient Assessment of Groups. [PubMed] [Google Scholar]
- 27.Moser DK, Yamokoski L, Sun JL, et al. Improvement in health-related quality of life after hospitalization predicts event-free survival in patients with advanced heart failure. J. Card. Fail. 2009;15:763–769. doi: 10.1016/j.cardfail.2009.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rector TS, Tschumperlin LK, Kubo SH, et al. Use of the living with heart failure questionnaire to ascertain patients' perspectives on improvement in quality of life versus risk of drug-induced death. Journal of cardiac failure. 1995;1:201–206. doi: 10.1016/1071-9164(95)90025-x. [DOI] [PubMed] [Google Scholar]
- 29.Wu JR, Lennie TA, Frazier SK, Moser DK. Health-related quality of life, functional status, and cardiac event-free survival in patients with heart failure. The Journal of cardiovascular nursing. 2015 doi: 10.1097/JCN.0000000000000248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zhang JY, Yan LX, Tang JL, et al. Estimating daily salt intake based on 24 h urinary sodium excretion in adults aged 18–69 years in shandong, china. BMJ open. 2014;4:e005089. doi: 10.1136/bmjopen-2014-005089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Xu J, Wang M, Chen Y, et al. Estimation of salt intake by 24-hour urinary sodium excretion: A cross-sectional study in yantai, china. BMC public health. 2014;14:136. doi: 10.1186/1471-2458-14-136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Harris J, Benedict F. A biometric study of basal metabolism in man. Washington DC: Carnegie Institute of Washington; 1919. [Google Scholar]
- 33.Mills RM, Jr, Haught WH. Evaluation of heart failure patients: Objective parameters to assess functional capacity. Clin Cardiol. 1996;19:455–460. doi: 10.1002/clc.4960190603. [DOI] [PubMed] [Google Scholar]
- 34.Heo S, Moser DK, Lennie TA, Zambroski CH, Chung ML. A comparison of health-related quality of life between older adults with heart failure and healthy older adults. Heart & lung : the journal of critical care. 2007;36:16–24. doi: 10.1016/j.hrtlng.2006.06.003. [DOI] [PubMed] [Google Scholar]
- 35.Johnston CS, Barkyoumb GM, Schumacher SS. Vitamin c supplementation slightly improves physical activity levels and reduces cold incidence in men with marginal vitamin c status: A randomized controlled trial. Nutrients. 2014;6:2572–2583. doi: 10.3390/nu6072572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Carr AC, Vissers MC, Cook JS. The effect of intravenous vitamin c on cancer- and chemotherapy-related fatigue and quality of life. Frontiers in oncology. 2014;4:283. doi: 10.3389/fonc.2014.00283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yeom CH, Jung GC, Song KJ. Changes of terminal cancer patients' health-related quality of life after high dose vitamin c administration. Journal of Korean medical science. 2007;22:7–11. doi: 10.3346/jkms.2007.22.1.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Fritz H, Flower G, Weeks L, et al. Intravenous vitamin c and cancer: A systematic review. Integrative cancer therapies. 2014;13:280–300. doi: 10.1177/1534735414534463. [DOI] [PubMed] [Google Scholar]
- 39.Hemila H. Vitamin c supplementation and respiratory infections: A systematic review. Military medicine. 2004;169:920–925. doi: 10.7205/milmed.169.11.920. [DOI] [PubMed] [Google Scholar]
- 40.Hunt C, Chakravorty NK, Annan G, Habibzadeh N, Schorah CJ. The clinical effects of vitamin c supplementation in elderly hospitalised patients with acute respiratory infections. International journal for vitamin and nutrition research. Internationale Zeitschrift fur Vitamin- und Ernahrungsforschung. Journal international de vitaminologie et de nutrition. 1994;64:212–219. [PubMed] [Google Scholar]
- 41.Moore LV, Dodd KW, Thompson FE, et al. Using behavioral risk factor surveillance system data to estimate the percentage of the population meeting us department of agriculture food patterns fruit and vegetable intake recommendations. American journal of epidemiology. 2015;181:979–988. doi: 10.1093/aje/kwu461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sharma R, Davidoff MN. Oxidative stress and endothelial dysfunction in heart failure. Congestive heart failure (Greenwich, Conn.) 2002;8:165–172. doi: 10.1111/j.1527-5299.2002.00714.x. [DOI] [PubMed] [Google Scholar]
- 43.Bauersachs J, Widder JD. Endothelial dysfunction in heart failure. Pharmacological reports : PR. 2008;60:119–126. [PubMed] [Google Scholar]
- 44.Lee KS, Song EK, Lennie TA, et al. Symptom clusters in men and women with heart failure and their impact on cardiac event-free survival. The Journal of cardiovascular nursing. 2010;25:263–272. doi: 10.1097/JCN.0b013e3181cfbb88. [DOI] [PubMed] [Google Scholar]
- 45.Hornig B, Arakawa N, Kohler C, Drexler H. Vitamin c improves endothelial function of conduit arteries in patients with chronic heart failure. Circulation. 1998;97:363–368. doi: 10.1161/01.cir.97.4.363. [DOI] [PubMed] [Google Scholar]
- 46.Ashor AW, Siervo M, Lara J, et al. Effect of vitamin c and vitamin e supplementation on endothelial function: A systematic review and meta-analysis of randomised controlled trials. The British journal of nutrition. 2015;113:1182–1194. doi: 10.1017/S0007114515000227. [DOI] [PubMed] [Google Scholar]
- 47.Witte KK, Nikitin NP, Parker AC, et al. The effect of micronutrient supplementation on quality-of-life and left ventricular function in elderly patients with chronic heart failure. European heart journal. 2005;26:2238–2244. doi: 10.1093/eurheartj/ehi442. [DOI] [PubMed] [Google Scholar]
- 48.Tomiyama H, Watanabe G, Yoshida H, Doba N, Yamashina A. Reduction of oxidative stress augments natriuretic effect of furosemide in moderate heart failure. American heart journal. 2003;145:E2. doi: 10.1067/mhj.2003.42. [DOI] [PubMed] [Google Scholar]