Abstract
Objectives:
Autopsy rates in North American Children’s hospitals have not been recently evaluated. Our objectives were 1) to determine the autopsy rates from patients cared for in pediatric intensive care units (PICUs) during a portion of their hospital stay; 2) to identify patient characteristics associated with autopsies; and 3) to understand the relative role of medical examiner cases.
Design:
Secondary analysis of data prospectively collected from a sample of patients (n=10,078) admitted to PICUs affiliated with the Collaborative Pediatric Critical Care Research Network (CPCCRN) between December 2011 and April 2013.
Setting:
Eight quaternary care PICUs
Patients:
Patients in the primary study were less than 18 years of age, admitted to a PICU and not moribund on PICU admission. Patients included in this analysis were those who died during their hospital stay.
Intervention:
None
Measurements and Main Results:
Socio-demographic, clinical, hospital and PICU data were compared between patients who had autopsies conducted and those who did not and between medical examiner and non-medical examiner autopsies. Of 10,078 patients, 275 died of which 36% (n=100) had an autopsy performed. Patients with cancer who died were less likely to receive autopsies (p=0.005) whereas those who died after trauma or cardiac arrest had autopsies performed more often (p<0.01). Autopsies were more common in patients with greater physiological instability at admission (p<0.001), and those who received more aggressive PICU care. Medical examiner cases comprised nearly half of all autopsies (n=47, 47%), were conducted in patients presenting with greater physiological instability (p<0.001) and more commonly after catastrophic events such as cardiac arrest or trauma (p<0.001).
Conclusions:
In this first multicenter analysis of autopsy rates in children, 36% of deaths had autopsies conducted, of which nearly half were conducted by the medical examiner. Deaths with autopsy are more likely to be previously healthy children that had catastrophic events prior to admission.
Keywords: Pediatric Intensive Care Unit, autopsy, medical examiner, death
Background:
Autopsy rates in adults have steadily declined in the last half century from nearly 50% to less than 20%. [1–4]. This decline has been attributed to advances in diagnostic and imaging techniques that make autopsies less informative, difficulties obtaining consent and loss of interest by clinicians [3]. Approximately 25% of autopsies on adults resulted in a diagnosis that was missed clinically and for up to 10% of cases, the new diagnosis would have resulted in a change in clinical care that may have led to recovery or prolonged survival if it had been known before death [3,5]. In the past, physicians believed that autopsies provide valuable information, should be performed more frequently, and may provide support for grieving families [6].
The most recent North American pediatric autopsy rates from the 1990’s range between 26% and 40% in single center studies [2, 7, 8]. None of the previous reports focused on identifying patient characteristics associated with autopsies. Similar to adult results, single center pediatric studies found discordance between the premorbid and autopsy diagnostic information in 16% to 30% of cases [8–10].
Most pediatric deaths occur either in the pediatric intensive care unit (PICU) or involve patients who had care delivered in the PICU for part of their hospitalization [11]. The objectives of this project were to determine the autopsy rate among patients cared for in the PICU, to identify patient characteristics associated with autopsies, and to understand the current role of medical examiner cases in performing autopsies.
Methods
This study was a secondary analysis of data collected prospectively in a 10,078 patient probability sample of all patients admitted to PICUs in the eight sites in the Eunice Kennedy Shriver National Institute of Child Health and Human Development Collaborative Pediatric Critical Care Research Network (CPCCRN) between December 2011 and April 2013 [12]. Patients in this sample were less than 18 years old and admitted to a medical/surgical or cardiac PICU. Patients were excluded in the primary data set if their vital signs were incompatible with life for at least the first 2 hours after PICU admission. Data were collected at the time of first PICU admission for each of the 10,078 patients. The protocol was approved by the Institutional Review Boards at all participating institutions. This analysis focuses on PICU patients who died during their hospitalization, including children who died during the initial PICU stay, while readmitted to the PICU, or elsewhere in hospital.
Data Collection
Details of data collection have been previously reported [12–13]. Socio-demographic data included sex, age, race, ethnicity, and payer type. Clinical parameters on admission included baseline functional status, underlying conditions (congenital heart disease, acute or chronic cancer), events prior to admission (trauma, cardiac arrest), admission status (elective or emergent), admission source (post-operative, inpatient, referral hospital or emergency department), and primary system of dysfunction on admission (classified as Respiratory, Cardiovascular (Acquired or Congenital), Cancer, Neurologic or Other).Severity of illness was assessed with Pediatric Risk of Mortality (PRISM) scores using laboratory information obtained between 2 hours prior to through 4 hours after PICU admission and vital signs recorded in the first 4 hours post-admission. The PRISM score is a physiology-based score for mortality risk [14– 15].
Functional status on admission (baseline) was assessed with the Functional Status Scale (FSS) using historical information at hospital admission. The FSS is a granular scale for assessing pediatric functional status in six domains including mental, sensory, communication, motor function, feeding and respiratory status [16]. Total FSS scores range from 6 to 30 and are categorized as 6–8 (normal and mild dysfunction), 9–13 (moderate dysfunction), 14–20 (severe dysfunction), and greater than 20 (very severe dysfunction).
Autopsies were categorized as medical examiner autopsy only if they were performed by the medical examiner. If the death was referred to the medical examiner, but autopsy was performed in the tertiary children’s hospital, it was categorized as a non-medical examiner autopsy. PICU and hospital resource use included PICU and hospital length of stay. Mechanical ventilation and/or vasoactive agent infusion were used as indicators of aggressive PICU care while antibiotics and/or steroid administrations were used as indicators of non-aggressive PICU care. Variables related to end-of-life care included the date, time, and location of death; whether the death was a medical examiner case; and whether an autopsy was performed. Location of death was categorized as PICU, general care area, or other hospital location.
Statistical Analysis
Statistical analysis was under the supervision of RH. Binary and categorical data were expressed as absolute numbers and percentages. Continuous data were summarized by medians and interquartile ranges (25–75th percentiles). Statistical analysis used the Wilcoxon rank sum test to compare continuous factors between subgroups, while chi-squared tests or Fisher’s exact tests were used to compare proportions of binary or categorical factors between subgroups. All tests were two-tailed and a probability value less than 0.05 was treated as significant in this exploratory analysis. Statistical analysis was performed in SAS Version 9.4 (SAS Institute, Cary, NC).
Results
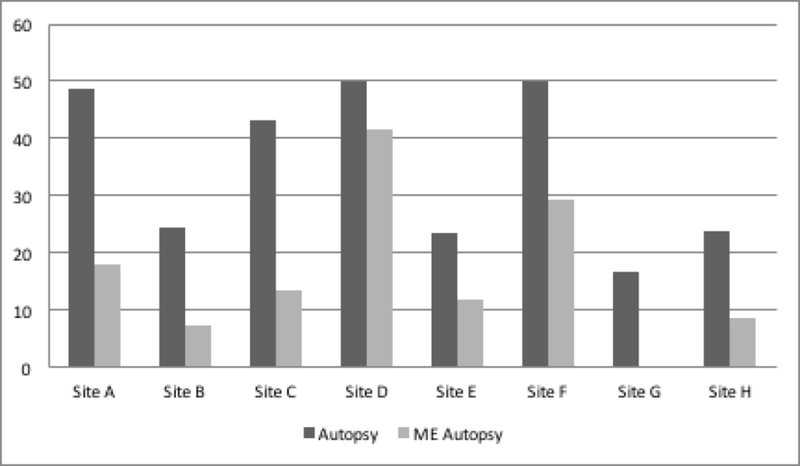
Of the 10,078 patients in the cohort, a total of 275 (2.7%) died during their hospital stay, of whom 100 (36.4%) received an autopsy. Autopsy rates were different by study site (Figure 1, p=0.009 for chi-squared comparison of autopsy rates by sites; also p<0.001 for chi-squared comparison of medical examiner autopsy rates by site). Socio-demographic and baseline characteristics of the patient deaths with and without autopsy are contained in Table 1. Over half the patients (n=142, 51.6%) were male and 44.4% were < 1 year of age. While there was no difference in median age between those who were autopsied and those who were not, autopsy rates were lower in some age categories, such as infants under 14 days of age and children aged over 144 months. The majority of patients (67%) had government insurance; payer type was not associated with autopsy rate. Race and ethnicity were not assessed in this report due to a large number of missing values.
Figure 1:
Proportion of Deaths that were Autopsies and ME autopsies by Site
Table 1:
Socio-Demographic Characteristics of Deaths by Autopsy Performance
| Variable | Deaths with Autopsy (n=100) | Deaths without Autopsy (n=175) | Significance Level |
|---|---|---|---|
| Gender | 0.731 | ||
| Male | 53 (37.3) | 89 (62.7) | |
| Female | 47 (35.3) | 86 (64.7) | |
| Age, median [IQR] | 0.9 [0.3–7.2] | 2.0 [0.2–9.8] | 0.262 |
| Age category (%) | <0.0011 | ||
| 0 to <14 days | 13 (26.5) | 36 (73.5) | |
| 14 days to <1 month | 2 (40.0) | 3 (60.0) | |
| 1 month to <12 months | 36 (52.9) | 32 (47.1) | |
| 12 months to <60 months | 18 (29.5) | 43 (70.5) | |
| 60 months to <144 months | 22 (51.2) | 21 (48.8) | |
| ≥144 months | 9 (18.4) | 40 (81.6) | |
| Payer Type, n (%) | 0.881,3 | ||
| Government | 67 (36.6) | 116 (63.4) | |
| Commercial | 24 (33.3) | 48 (66.7) | |
| Other | 3 (37.5) | 5 (62.5) | |
| Unknown | 6 (50.0) | 6 (50.0) |
Chi-squared
Wilcoxon Rank Sum
Excluding unknowns
IQR: Interquartile range
Admission characteristics of patient deaths with and without autopsies are depicted in Table 2. Baseline functional status, while normal, was worse in children without autopsies than those with autopsies, as seen by the larger interquartile range for non-autopsied children (p=0.046). Congenital heart disease was not significantly associated with autopsies. However, children who died with an underlying condition of cancer were less likely to have an autopsy conducted (p=0.005). Patients who presented to the ICU after trauma or after cardiac arrest were significantly more likely to have an autopsy than others. Elective versus emergent admission status, admission source, and primary system of dysfunction on admission to the PICU were not significantly associated with autopsy status.
Table 2:
Autopsy Performance by Clinical Characteristics of Children who Died
| Variable | Autopsy (n=100) | No Autopsy (n=175) | Significance Level | |
|---|---|---|---|---|
| Baseline Function | ||||
| Baseline FSS, Median [IQR] | 6 [6–8] | 6 [6–10] | 0.0461 | |
| Underlying Conditions | ||||
| Cancer Diagnosis: Present | 5 (14.7) | 29 (85.3) | 0.0052 | |
| Absent | 95 (39.4) | 146 (60.6) | ||
| Congenital Heart Disease: Present | 33 (30.8) | 74 (69.2) | 0.132 | |
| Absent | 67 (39.9) | 101 (60.1) | ||
| Events Prior to Admission | ||||
| Trauma: Yes | 14 (63.6) | 8 (36.4) | 0.0062 | |
| No | 86 (34.0) | 167 (66.0) | ||
| Cardiac Arrest: Yes | 34 (68.0) | 16 (32.0) | <0.0012 | |
| No | 66 (29.3) | 159 (70.7) | ||
| Admission Status | ||||
| Elective (scheduled) | 17 (34.7) | 32 (65.3) | 0.792 | |
| Emergent (unscheduled) | 83 (36.7) | 143 (63.3) | ||
| Admission Source | 0.822 | |||
| Post-Operative, n (%) | 21 (36.2) | 37 (63.8) | ||
| Inpatient, n (%) | 21 (32.8) | 43 (67.2) | ||
| Direct Admission from Referral Hospital, n (%) | 36 (40.0) | 54 (60.0) | ||
| Emergency Department, n (%) | 22 (34.9) | 41 (65.1) | ||
| Primary System of Dysfunction | 0.353 | |||
| Respiratory, n (%) | 22 (27.8) | 57 (72.2) | ||
| Cardiovascular, n (%) | 49 (38.9) | 77 (61.1) | ||
| Cancer, n (%) | 2 (22.2) | 7 (77.8) | ||
| Neurologic, n (%) | 18 (43.9) | 23 (56.1) | ||
| Gastrointestinal, n (%) | 4 (40.0) | 6 (60.0) | ||
| Other, n (%) | 5 (50.0) | 5 (50.0) | ||
| Severity of Illness | ||||
| PRISM Score, median [IQR] | 18 [7 – 27] | 11 [5 – 19] | <0.0011 | |
Wilcoxon Rank Sum
Chi-squared
Fisher’s Exact
FSS: Functional Status Scale; IQR: Interquartile range; GI: Gastrointestinal: PRISM: Pediatric Risk of Mortality
Patients with autopsies had shorter, but more aggressively treated illnesses than patients without autopsies (Tables 2, 3). Patients with autopsies had worse severity of illness (median PRISM scores:18 vs 11, p < 0.001), and a shorter length of stay in the PICU (median 3.2 days vs 6.2 days, p = 0.04) as well as shorter hospital stay (median 4.9 days vs 13.5 days, p = 0.001). PICU therapies including mechanical ventilation and vasoactive infusions were used significantly more often in patients with autopsies (p < 0.01), while less aggressive therapies such as antibiotics and steroids were not. The majority of patients died in the PICU; there was no difference in the proportion of autopsies based on hospital location of death.
Table 3:
PICU and Hospital Resource Use by Autopsy Performance
| Variable | Autopsy (n=100) | No Autopsy (n=175) | Significance Level |
|---|---|---|---|
| PICU LOS, days, Median [IQR] | 3.2 [1.3–13.2] | 6.2 [1.8–15.0] | 0.041 |
| Hospital LOS, days, Median [IQR] | 4.9 [1.6–18.1] | 13.5 [3.5–31.3] | 0.0011 |
| Therapies | |||
| Mechanical Ventilation, n (%) | 95 (95.0) | 147 (84.0) | 0.0072 |
| Vasoactive Agent Infusions, n (%) | 88 (88.0) | 124 (70.9) | 0.0012 |
| Antibiotics, n (%) | 86 (86.0) | 152 (86.9) | 0.842 |
| Steroids, n (%) | 48 (48.0) | 95 (54.3) | 0.322 |
| Location of Death | 0.313 | ||
| PICU, n (%) | 95 (95.0) | 157 (89.7) | |
| Hospital General Care, n (%) | 2 (2.0) | 10 (5.7) | |
| Other, n (%) | 3 (3.0) | 8 (4.6) |
Wilcoxon Rank Sum
Chi-squared
Fisher’s Exact
PICU: Pediatric Intensive Care Unit; LOS: Length of stay; IQR: Interquartile range
There were 62 deaths designated as medical examiner cases, of which 76% were autopsied by the medical examiner. Of the 100 autopsies, 47 were conducted by the medical examiner (Table 4). There were no significant differences in median age or payer type between medical examiner and the non-medical examiner autopsies; however, no infants < 14 days old were medical examiner autopsies. Children who had medical examiner autopsies were more likely to have normal baseline functional status. All autopsied patients who had trauma and the majority of patients with cardiac arrests (85.3%) had them performed by the medical examiner. Among autopsied children, those admitted to the ICU from an inpatient location or operative procedure were less likely to have medical examiner autopsies than those with unscheduled admissions or from the emergency department or referral hospital. The primary system of dysfunction on admission was different between medical examiner autopsies and non-medical examiner autopsies, with 89% of autopsied children admitted with neurological dysfunction having medical examiner autopsies, compared to less than half with other dysfunction types. Medical examiner cases had more physiological instability than other autopsied children (median PRISM scores: 23 vs. 11, p < 0.001), and had shorter median hospital length of stay (2.8 days vs 8.2 days, p = 0.003). The intensive care therapies of mechanical ventilation and vasoactive agent infusions were similar between the two groups, while non-medical examiner cases received significantly more (less aggressive) therapies of antibiotics and steroids (p < 0.05).
Table 4:
Comparison of Medical Examiner and Non-Medical Examiner Autopsies
| Category | Variable | Medical Examiner Autopsies (n=47) | Non-Medical Examiner Autopsies (n=53) | Significance Level |
|---|---|---|---|---|
| Socio-Demographics | ||||
| Gender (%) | 0.661 | |||
| Male | 26 (49.1) | 27 (50.9) | ||
| Female | 21 (44.7) | 26 (55.3) | ||
| Age, median [IQR] | 1.1 [0.3–8.6] | 0.8 [0.0–5.9] | 0.172 | |
| Age category (%) | 0.0033 | |||
| 0 to <14 days | 0 (0.0) | 13 (100.0) | ||
| 14 days to <1 month | 1 (50.0) | 1 (50.0) | ||
| 1 month to <12 months | 20 (55.6) | 16 (44.4) | ||
| 12 months to <60 months | 11 (61.1) | 7 (38.9) | ||
| 60 months to < 144 months | 10 (45.5) | 12 (54.5) | ||
| >144 months | 5 (55.6) | 4 (44.4) | ||
| Payer Type | 0.123,4 | |||
| Government | 29 (43.3) | 38 (56.7) | ||
| Commercial | 13 (54.2) | 11 (45.8) | ||
| Other | 3 (100.0) | 0 (0.0) | ||
| Missing | 2 (33.3) | 4 (66.7) | ||
| Baseline Function | ||||
| Baseline FSS, median [IQR] | 6 [6–6] | 6 [6–9] | <0.0012 | |
| Underlying Conditions | ||||
| Cancer Diagnosis: Present | 1 (20.0) | 4 (80.0) | 0.373 | |
| Absent | 46 (48.4) | 49 (51.6) | ||
| Congenital Heart Disease: Present | 2 (6.1) | 31 (93.9) | <0.0011 | |
| Absent | 45 (67.2) | 22 (32.8) | ||
| Events prior to admission | ||||
| Trauma: Yes | 14 (100.0) | 0 (0.0) | <0.0011 | |
| No | 33 (38.4) | 53 (61.6) | ||
| Cardiac Arrest: Yes | 29 (85.3) | 5 (14.7) | <0.0011 | |
| No | 18 (27.3) | 48 (72.7) | ||
| Admission Status | ||||
| Elective (scheduled) | 4 (23.5) | 13 (76.5) | 0.0331 | |
| Emergent (unscheduled) | 43 (51.8) | 40 (48.2) | ||
| Admission Source | 0.0051 | |||
| Post-Operative, n (%) | 6 (28.6) | 15 (71.4) | ||
| Inpatient, n (%) | 5 (23.8) | 16 (76.2) | ||
| Direct Admission from Referral Hospital, n (%) | 22 (61.1) | 14 (38.9) | ||
| Emergency Department, n (%) | 14 (63.6) | 8 (36.4) | ||
| Primary System of Dysfunction | <0.0013 | |||
| Respiratory, n (%) | 8 (36.4) | 14 (63.6) | ||
| Cardiovascular, n (%) | 22 (44.9) | 27 (55.1) | ||
| Cancer, n (%) | 0 (0.0) | 2 (100.0) | ||
| Neurologic, n (%) | 16 (88.9) | 2 (11.1) | ||
| Other, n (%) | 1 (11.1) | 8 (88.9) | ||
| Severity of Illness | ||||
| PRISM Score, median [IQR] | 23 [17–31] | 11 [5–19] | <0.0012 | |
| Resource Use | ||||
| PICU LOS, median [IQR] | 2.8 [1.1–6.3] | 4.2 [1.4–22.0] | 0.112 | |
| Hospital LOS, median [IQR] | 2.8 [1.1–6.8] | 8.2 [2.4–42.0] | 0.0032 | |
| ICU Therapies | ||||
| Mechanical Ventilation, n (%) | 46 (97.9) | 49 (92.5) | 0.373 | |
| Vasoactive Agent Infusions, n (%) | 40 (85.1) | 48 (90.6) | 0.401 | |
| Antibiotics, n (%) | 37 (78.7) | 49 (92.5) | 0.0481 | |
| Steroids, n (%) | 16 (34.0) | 32 (60.4) | 0.0091 | |
| Location of Death | 0.253 | |||
| PICU, n (%) | 46 (97.9) | 49 (92.5) | ||
| Hospital General Care, n (%) | 1 (2.1) | 1 (1.9) | ||
| Other, n (%) | 0 (0.0) | 3 (5.7) |
Chi-squared
Wilcoxon Rank Sum
Fisher’s Exact
Missing variables excluded (2 patients with ME autopsies and 4 patients with non-ME autopsies)
IQR: Interquartile range; FSS: Functional Status Scale; PRISM: Pediatric Risk of Mortality
PICU: Pediatric Intensive Care Unit; LOS: Length of stay
Discussion
This is the largest and only multicenter contemporary analysis of autopsy rates in pediatric patients. The autopsy rate in this study was 36%, similar to other published data from single center North American pediatric studies (26–40%) [2, 7, 8] and lower than international single center pediatric studies with rates of 40 to 60% [9, 17, 18].
A number of observations may be drawn from this analysis. First, patient deaths receiving autopsies are more likely to have had severe, acute conditions. Patient deaths receiving autopsies were more likely to have trauma and cardiac arrests prior to PICU admission, present with greater physiological instability, and more frequently received aggressive PICU care than those who did not have autopsies. These children had shorter lengths of stay and may have had more limited ante-mortem diagnostic efforts. Patients not receiving autopsies were more likely to have conditions where the diagnosis was known and more likely to have been comprehensively investigated, such as cancer or congenital heart disease.
Second, medical examiner autopsies comprise about half of all autopsies. This remains consistent with data from over two decades ago by Goldstein and colleagues, who report a single-center rate of 44% in the PICU [19]. Medical examiner patients predominantly had traumatic injury and/or cardiac arrest. Requirements to refer deaths to medical examiners are dependent on jurisdiction; it was out of the scope of this study to examine these local requirements of each institution. However, to gain better understanding of this we surveyed each of the sites for autopsy practices. We found only 1 of 7 sites (14%) have mandated referrals of all deaths to the medical examiners. The remainder of cases are referred based on a set of clinical and historical guidelines, which includes suspicious circumstance or evidence of trauma (100%), operative or post-operative death (66.7%) and time from admission to death (83.3%). It is also unclear whether families would have elected to have an autopsy performed if their child was not mandated to have one conducted by the medical examiner. We also analyzed children as medical examiner autopsies only if their autopsy was conducted by the medical examiner. There were 62 medical examiner referrals, of which 15 (24%) were not conducted by the medical examiner. Though not known in our cohort, reasons for this may include the ME denying the referral, lack of expertise of the medical examiner to conduct the autopsy, or instances of organ donation where the medical examiner is present to observe the organ procurement but does not conduct an autopsy.
Most socio-demographic characteristics associated with autopsies in this analysis were similar to previous studies [8, 20]. Kumar and colleagues examined socio-demographic factors including age, race and insurance status and found no difference in autopsy status based on these variables. However, their study found that autopsies were more common in patients over 5 years while our study found a higher rate of autopsies in those ages 1 month to 1 year and a lower rate in adolescents. The current study is the first to assess the baseline functional status of children receiving autopsies finding that those receiving autopsies had normal or near-normal baseline functional status.
Although this study is characterized by many strengths including the use of robust data collected initially to assess the relationship of physiological status to morbidity and mortality, there are also limitations. For example, the dataset excluded patients who had vital signs incompatible with life within the first few hours of admission. These children likely presented after a sudden event, but their autopsy rate and their characteristics at PICU admission are unknown. Additionally, the pathological results of the autopsies were not abstracted, and thus, there could be no attempt to correlate these results with clinical diagnoses. While this information is central to the need for autopsies, it is better collected prospectively with reliable assessments of clinical care, the knowledge of the care givers, and the potential clinical impact of the pathological results. Survey of our sites did show 4/7 (57.1%) of sites had a systematic way in which autopsy results were reviewed, yet only 2/7 (28.6%) had a similar systematic review of medical examiner case results. Finally, while our intention was to look at overall trends in PICUs, our cohort showed institutional heterogeneity among study sites in autopsy rates (~16% to 50%) and in the percentage of medical examiner cases (0 to ~42%). This might reflect the different demographic characteristics of each institution.
Conclusion
This is the first multicenter pediatric study of autopsy rates in children. Approximately one-third of PICU patients who die have an autopsy conducted, of which half are conducted by the medical examiner. Autopsies are more likely to be performed on previously healthy children with no pre-existing medical conditions and normal functional status that incur severe, acute events prior to admission. The autopsy rates in this contemporary study are consistent with other single center pediatric studies in the US from prior decades.
Individuals Acknowledged and Roles
Teresa Liu, MPH, CCRP; University of Utah (project management, Data Coordinating Center )
Jean Reardon, MA, BSN, RN; Children’s National Medical Center (institutional project management, data collection)
Elyse Tomanio, BSN, RN; Children’s National Medical Center (institutional project management, data collection)
Morella Menicucci, MD, CCRP; Children’s National Medical Center (data collection)
Fidel Ramos, BA; Children’s National Medical Center (institutional project management, data collection)
Aimee Labell, MS, RN; Phoenix Children’s Hospital (institutional project management, data collection)
Courtney Bliss, BS, DTR; Phoenix Children’s Hospital (data collection)
Jeffrey Terry, MBA; Children’s Hospital Los Angeles (data collection)
Margaret Villa, RN; Children’s Hospital Los Angeles and Mattel Children’s Hospital UCLA (institutional project management, data collection)
Jeni Kwok, JD; Children’s Hospital Los Angeles and Mattel Children’s Hospital (institutional project management, data collection)
Amy Yamakawa, BS; Children’s Hospital Los Angeles and Mattel Children’s Hospital UCLA (data collection)
Ann Pawluszka, BSN, RN; Children’s Hospital of Michigan (institutional project management)
Symone Coleman, BS, MPH; Children’s Hospital of Michigan (data collection)
Melanie Lulic, BS; Children’s Hospital of Michigan (data collection)
Mary Ann DiLiberto, BS, RN, CCRC; Children’s Hospital of Philadelphia (institutional project management, data collection)
Carolann Twelves, BSN, RN; Children’s Hospital of Philadelphia (data collection)
Monica S. Weber, RN, BSN, CCRP; University of Michigan (institutional project management, data collection)
Lauren Conlin, BSN, RN, CCRP; University of Michigan (data collection)
Alan C. Abraham, BA, CCRC; Children’s Hospital of Pittsburgh of University of Pittsburgh Medical Center (institutional project management, data collection)
Jennifer Jones, RN; Children’s Hospital of Pittsburgh of University of Pittsburgh Medical Center (data collection)
Jeri Burr, MS, RN-BC, CCRC; University of Utah (project management, Data Coordinating Center)
Nichol Nunn, BS, MBA; University of Utah (project management, Data Coordinating Center)
Alecia Peterson, BS, CMC; University of Utah (project management, Data Coordinating Center)
Carol Nicholson, MD (former Project Officer, Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Institutes of Health, Department of Health and Human Services, for part of the study period)
Tammara L. Jenkins, MSN, RN; Pediatric Trauma and Critical Illness Branch, Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD), the National Institutes of Health (NIH), Bethesda, MD
Robert Tamburro, MD, MSc; Pediatric Trauma and Critical Illness Branch, Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD), the National Institutes of Health (NIH), Bethesda, MD
Funding Source: Supported, in part, by the following cooperative agreements from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Institutes of Health, Department of Health and Human Services: U10HD050096, U10HD049981, U10HD049983, U10HD050012, U10HD063108, U10HD063106, U10HD063114 and U01HD049934. This content is solely the responsibility of the authors and does not necessarily represent the views of the National Institutes of Health.
Footnotes
Copyright form disclosure:
Drs. Basu, Holubkov, Dean, Meert, Berg, Carcillo, and Pollack received support for article research from the National Institutes of Health (NIH).
Drs. Holubkov, Dean, Meert, Berg, Carcillo, and Pollack institutions received funding from the NIH.
Dr. Holubkov received funding from Pfizer (DSMB membership), Medimmune (DSMB membership), Physicians Committee for Responsible Medicine (biostatistical consulting), St Jude Medical (biostatistical consulting, past), Armaron Inc (DSMB membership, past), and the American Burn Association (DSMB membership, past).
Dr. Newth received funding from Philips Research North America.
Clinical Trials Registration: Not Applicable
Contributor Information
Sonali Basu, Department of Pediatrics, Children’s National Health System and the George Washington University School of Medicine and Health Sciences, Washington DC.
Richard Holubkov, Department of Pediatrics, University of Utah School of Medicine, Salt Lake City, UT.
J. Michael Dean, Department of Pediatrics, University of Utah School of Medicine, Salt Lake City, UT.
Kathleen L. Meert, Department of Pediatrics, Children’s Hospital of Michigan, Detroit, MI.
Robert A. Berg, Department of Pediatrics, Children’s Hospital of Philadelphia, Philadelphia, PA.
Joseph Carcillo, Department of Critical Care Medicine, Children’s Hospital of Pittsburgh, Pittsburgh, PA.
Christopher J. L. Newth, Department of Anesthesiology and Critical Care Medicine, Children’s Hospital Los Angeles, University of Southern California Keck School of Medicine, Los Angeles, CA.
Rick E. Harrison, Department of Pediatrics, University of California at Los Angeles, Los Angeles, CA.
Murray M. Pollack, Department of Pediatrics, Children’s National Health System and the George Washington University School of Medicine and Health Sciences, Washington DC.
Eunice Kennedy Shriver, National Institute of Child Health and Human Development Collaborative Pediatric Critical Care Research Network (CPCCRN)..
References:
- 1.Kischer LT: Autopsy and mortality statistics. JAMA 1992; 267:1264–1268. [DOI] [PubMed] [Google Scholar]
- 2.Stambouly JJ, Kahn E, Boxer RA: Correlation between clinical diagnoses and autopsy findings in critically ill children. Pediatrics 1993; 92:248–251. [PubMed] [Google Scholar]
- 3.Goldman L, Sayson R, Robbins S: Value of autopsy in three medical eras. N Engl J Med 1983; 308:1000–1005. [DOI] [PubMed] [Google Scholar]
- 4.von Dessauer B, Velozo L, Benavente C, et al. : Postmortem studies in the contemporary pediatric intensive care unit. Pediatr Crit Care Med 2011; 12:617–621. [DOI] [PubMed] [Google Scholar]
- 5.Fernandez-Segoviano P, Lazaro A, Esteban A: Autopsy as quality assurancein the intensive care unit. Crit Care Med 1988; 16:683–685. [DOI] [PubMed] [Google Scholar]
- 6.Stolman CJ, Castello F, Yorio M, et al. : Attitudes of pediatricians and pediatric residents toward obtaining permission for autopsy. Arch Pediatr Adolesc Med 1994; 148:843–847. [DOI] [PubMed] [Google Scholar]
- 7.Kay MH, Moddie DS, Sterba R: The values of autopsy in congenital heart disease. Clin Pediatr 1991; 30:450–454. [DOI] [PubMed] [Google Scholar]
- 8.Kumar P, Taxy J, Angst D: Autopsies in Children: Are the Still Useful? Arch Pediatr Adolesc Med 1998; 152:558–563. [DOI] [PubMed] [Google Scholar]
- 9.Carlotti AP, Bachette LG, Carmona F, et al. : Discrepancies between clinical diagnoses and autopsy findings in critically ill children a prospective study. Am J Clin Pathol 2016; 146:701–708. [DOI] [PubMed] [Google Scholar]
- 10.Seftel MD, Ho M, Pruthi D, et al. : High rate of discordance between clinical and autopsy diagnoses in blood and marrow transplantation. Bone Marrow Transplant 2007; 40:1049–1053. [DOI] [PubMed] [Google Scholar]
- 11.Meert KL, Keele L, Morrison W,et al. : Eunice Kennedy Shriver National Institute of Child Health and Human Development Collaborative Pediatric Critical Care Research Network. End-of-Life Practices Among Tertiary Care PICUs in the United States: A Multicenter Study. Pediatr Crit Care Med 2015; 16:e231–e238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pollack MM, Holubkov R, Funai T, et al. : Eunice Kennedy Shriver National Institute of Child Health and Human Development Collaborative Pediatric Critical Care Research Network. Simultaneous Prediction of New Morbidity, Mortality, and Survival Without New Morbidity From Pediatric Intensive Care: A New Paradigm for Outcomes Assessment. Crit Care Med 2015; 43:1699–709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pollack MM, Holubkov R, Funai T, et al. : Eunice Kennedy Shriver National Institute of Child Health and Human Development Collaborative Pediatric Critical Care Research Network. Pediatric intensive care outcomes: development of new morbidities during pediatric critical care. Pediatr Crit Care Med 2014; 15:821–827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pollack MM, Patel KM, Ruttimann UE: PRISM III: an updated Pediatric Risk of Mortality score. Crit Care Med 1996; 24:743–752. [DOI] [PubMed] [Google Scholar]
- 15.Pollack MM, Holubkov R, Funai T, et al. : Eunice Kennedy Shriver National Institute of Child Health and Human Development Collaborative Pediatric Critical Care Research Network. The Pediatric Risk of Mortality Score: Update 2015. Pediatr Crit Care Med 2016; 17:2–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pollack MM, Holubkov R, Glass P, et al. : Eunice Kennedy Shriver National Institute of Child Health and Human Development Collaborative Pediatric Critical Care Research Network. Functional Status Scale: new pediatric outcome measure. Pediatrics 2009; 124:e18–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pons M, Luaces C, Lobera E: A study regarding correlation between clinical and autopsy findings in a pedaitric intensive care unit. Medicine Intensiva. 1997; 21:9–12. [Google Scholar]
- 18.Cardoso MP, Bourguignon DC, Gomes MM, et al. : Comparison between clinical diagnoses and autopsy findings in a pediatric intensive care unit in Sao Paolo, Brazil. Pediatr Crit Care Med 2006; 7:423–427. [DOI] [PubMed] [Google Scholar]
- 19.Goldstein B, Metlay L, Cox C, et al. : Association of pre mortem diagnosis and autopsy findings in the pediatric intensive care unit versus emergency department versus ward patients. Crit Care Med 1996; 24(4): 683–686. [DOI] [PubMed] [Google Scholar]
- 20.Whitehouse SR, Kisoon N, Singh N: The utility of autopsies in a pediatric emergency department. Pediatr Emerg Care 1994: 10:72–75. [DOI] [PubMed] [Google Scholar]