Abstract
Objective:
No gold standard for ideal body weight (IBW) determination in children exists. We aimed to compare 4 methods of IBW calculation and determine level of agreement between methods and impact of measurement variance on tidal volumes (TV) prescribed in mechanically ventilated pediatric acute respiratory distress syndrome (PARDS).
Design:
Post-hoc analysis of 4 multicenter PARDS studies
Setting:
26 academic pediatric intensive care units
Patients:
589 patients
Measurements and Main Results:
IBW was calculated by 4 common methods: National Center for Health Statistics (NCHS), McLaren, Moore, and BMI, and compared in 3 ways: (1) determine the proportion of the cohort for which each method could successfully calculate IBW, (2) compare the level of agreement between the IBW methods by Bland-Altman analysis, (3) evaluate the difference in TV when 6mL/Kg IBW was prescribed. We a priori defined the better method to be one that could calculate IBW in most subjects, had good agreement with other methods, and led to a lower TV. Only 55% could have IBW measured by all four methods. NCHS, McLaren and Moore methods could calculate IBW in ≥90%, while BMI method was successful in only 61% due to no BMI validation in <2 year olds. In comparing each method to the others, there was great variance, particularly in ≥10 year olds. This variance was greatest between Moore and BMI methods with ≥10Kg difference in IBW in some subjects. The McLaren method had the best agreement with all other methods, and yielded similar prescribed TV in 2–10 year olds and lower TV in ≥10 years old.
Conclusions:
There is substantial variation in calculated IBW among 4 commonly used methods, particularly in adolescents. Since varying IBW may lead to discrepancies in PARDS care, a standard approach to IBW measurement is needed. We recommend the McLaren method to calculate IBW in children with PARDS until a gold standard method is validated.
Keywords: pediatric acute respiratory distress syndrome, acute lung injury, pediatric, ideal body weight
Introduction
Lung protective ventilation strategy has become the standard of care in adults with acute respiratory distress syndrome (ARDS)(1). A key element of a lung protective strategy is the application of a minimal tidal volume scaled to a predicted rather than actual body weight. This is based on the assumption that volutrauma might be minimized by delivering a volume appropriate to the patient’s lung capacity(1). Recently, the Pediatric Acute Lung Injury Consensus Conference recommended a similar strategy, stating “tidal volumes should be 3–6 mL/kg predicted body weight for patients with poor respiratory system compliance and closer to the physiologic range (5–8 mL/kg ideal body weight) for patients with better preserved respiratory system compliance”(2).
Ideal body weight (IBW), also referred to as predicted body weight, is a calculated weight determined for a specific age or height that is deemed optimal for nutritional status(3). Height, and therefore IBW, are excellent predictors of lung volume, which increases as the size of the thoracic cavity increases. It makes sense, then, that IBW be used for the prescription of tidal volumes in pediatric ARDS(4–6). However, there is no gold standard method to determine IBW in children.
Four IBW methods are commonly used in pediatrics: (1) National Center for Health Statistics data tables(7), (2) the McLaren method(8), (3) the Moore method(9), and (4) the body mass index (BMI) method(10). We compared these 4 methods to determine whether one method may be better suited to prescribe tidal volume and provide lung protective ventilation strategies than the others. First, we determined the proportion of the cohort for which each method could be used to successfully calculate the IBW; second, we compared the level of agreement between each possible combination of 2 out of the 4 IBW methods by Bland Altman analysis(11, 12); finally, we evaluated the differences in tidal volume prescribed by each method. Bland Altman analysis is a standardized method to compare a measurement to a gold standard or to compare two methods measuring the same variable in a standardized, descriptive way.
Methods and Materials
Design, Setting and Patients:
Our cohort combined 4 prospective PARDS studies (1 clinical trial, 3 observational studies) that were completed between 2000 and 2010 via the Pediatric Acute Lung Injury and Sepsis Investigators Network at 26 sites. Pediatric ARDS (ARDS) and pediatric acute lung injury (ALI) were identified based on the 1994 North American-European Consensus Conference criteria: a PaO2 to FiO2 ratio (PF ratio) of <300, bilateral infiltrates on chest radiograph, and no evidence of left atrial hypertension(13). Because IBW is a theoretical or predicted weight, we a priori defined the better method for IBW calculation would be one that was (a) easy to calculate, (b) was able to calculate IBW in most subjects, (c) had good agreement (or low mean IBW difference) with the other methods, and (d) led to similar or lower median tidal volume prescription in all age groups than the other methods.
We restricted analysis to all patients younger than 18 years old. Those with no documented admission age, weight, or height were excluded. This study received IRB exemption from UCSF Benioff Children’s Hospital, Oakland.
Measurements and Data Collection
IBW was calculated by four common methods, (1) National Center for Health Statistics (NCHS) data tables(7), (2) the McLaren method(8), (3) the Moore method(9), and (4) the body mass index (BMI) method(10). These methods are below; all account for subject gender, age and admission height. For the McLaren, Moore and BMI methods, we used growth charts published by the Center for Disease Control (CDC) as reference growth charts(14). Growth chart data was plotted by hand by at least one of the research team members.
1. NCHS data tables.
These data tables and growth charts were derived from the Health Examination Survey (HES) and the Health and Nutrition Examinations Survey (HANES) in the 1970s(7). They provide weight-for-stature percentiles but do not extend beyond a height of 137cm for females and 145cm for males. Adult IBW determination methods were used for individuals who exceeded these heights, per NCHS recommendations(7).
2. McLaren Method.
This method is based on validated growth charts that compare weight and height in relation to a child’s age(15, 16). It can be accomplished using the following steps: (a) plot the child’s height for age on the appropriate growth chart; (b) extend a line horizontally to the 50th percentile height-for-age line; (c) extend a line vertically from the 50th percentile height-for-age line to the corresponding 50th percentile weight; (d) note this weight as the IBW(8). Figure S1 in the online supplement demonstrates the above steps using the CDC growth charts. Children who are taller than 163cm (females) and 177cm (males) cannot have IBW calculated by this method, and were removed for any McLaren to other IBW method comparisons.
3. Moore Method.
The Moore method suggests that the IBW should correspond to the same standard deviation from the mean as the child’s height-for-age. For example, a child with a height at the 10th percentile will have an IBW determined by evaluating the growth chart and finding the weight at the 10th percentile for his or her age(9). Figure S2 in the online supplement demonstrates these steps. IBW calculation by this method requires chart-based estimations and may be more subject to error at the extremes of weight percentiles.
4. Body Mass Index (BMI) Method.
BMI is calculated by the formula weight (in kilograms) divided by the square of height (in meters)(17). Both the CDC and the World Health Organization (WHO) have provided pediatric BMI growth charts which can be used to determine IBW using the BMI method(14, 16). To calculate IBW with this method, use the formula IBW = [BMI at 50th percentile for age x (height in meters)2]. For example, the IBW for a 5-year old male who is 110cm (1.1m) tall can be calculated by determining the 50th percentile BMI value (in this case 15.4) and multiplying by 1.1m2 as follows, IBW = [15.4 x (1.1)2] = 18.6Kg. Children less than 2 years old cannot utilize the BMI method for IBW calculation and were removed for any BMI to other IBW method comparisons.
For each method, we evaluated the proportion of the cohort whose IBW could be successfully measured by that method and assessed whether age, race, ethnicity and gender were associated with failure to determine IBW by any given method. The median age of those whose IBW could be determined versus those whose IBW could not be determined by a given method were compared by Wilcoxon rank sum analysis while differences by race, ethnicity and gender were assessed by X2 or Fischer Exact tests.
Comparison of IBW Methods to Each Other.
Bland Altman analysis was used to compare the 4 IBW methods to each other(11, 12) to assess level of agreement, or variance, between the methods. Using this methodology, each possible combination of 2 out of the 4 methods was compared. According to the Bland Altman analysis, because no gold standard method exists, the mean IBW value between the 2 methods in each comparison was calculated and was assumed to be closer to the “truth” than either method(18). Next, the IBW calculated from one method was subtracted from the IBW calculated from the second method. This difference represented the “measurement error” observed for each patient. A 95% tolerance bound, mean error ±2SD, was then computed, and labeled the “limits of agreement”. These values are then displayed graphically with the mean IBW on the x-axis and the mean IBW difference on the y-axis. After comparison of the four IBW methods to each other for the whole cohort, we stratified into those < 10 years of age (to represent the pre-pubertal population) and those ≥ 10 years old (to represent the pubertal and post-pubertal population) and repeated Bland-Altman analyses separately on each strata. Such age stratification has been utilized before for analyses in the pediatric critical care population(19).
Since the amount of error that represents “clinically acceptable measurement error” in IBW measurement are likely age specific, i.e. a 2Kg difference may not be relevant for an adolescent but would be for an infant, we did not define an objective measure of good agreement between the methods(20). Instead, we relied on examination of the Bland Altman plots to assess agreement with stipulations that methods with good agreement would have (a) a narrow range between the mean difference and the upper and lower levels of agreement, preferably <2–3Kg, and (b) few subjects outside the limits of agreement. Further analyses of clinical and demographic factors were performed to assess if such variables were associated with the proportion of subjects outside the limits of agreement for a given comparison. These variables included age, gender, race, ethnicity, known chronic disease, immune compromised state, and PRISM-III score, a score of illness severity calculated within the first 24 hours of ICU admission(21). These analyses were performed by logistic regression.
Evaluation of Prescribed Tidal Volumes by each IBW Method
To determine if the IBW differences between the 4 methods yield large differences in delivered tidal volume, we determined the mean tidal volume (in mL) that would be delivered if a tidal volume of 6mL/Kg of IBW were prescribed. The mean tidal volumes calculated by each IBW method were compared to each other within the two age strata, 2–10 year olds and ≥10 year olds. Those < 2 years old were excluded because the BMI method cannot be used in this age group. Differences in mean prescribed tidal volumes within each strata were compared by paired t-test.
For all analyses, a p-value of <0.05 was accepted as being statistically significant. All analyses were performed using STATA software, version 13.1 (StataCorp, College Station, Texas).
Results
After combining the four PARDS studies, 721 unique patients were identified. We excluded 10 with no age or weight recorded and 113 with no admission height recorded, leaving 589 patients for analysis (Table 1). The median age was 4 years (IQR 0.7 to 11 years) and 56% were male. A prior comorbidity was reported in 319 (54%) of the subjects and 89 (15%) were immune compromised at time of enrollment. Ninety-nine subjects (17%) died during their hospitalization, a proportion consistent with prior ARDS observational studies.
Table 1:
Demographics and Clinical Summary of the Cohort
| Characteristic | n(%) or Median (IQR) |
|---|---|
| Male | 329 (56) |
| Age Category, years | |
| < 2 | 230 (39) |
| 2 to 5 | 96 (16) |
| 6 to 10 | 83 (14) |
| 11 to 15 | 107 (18) |
| > 15 | 73 (12) |
| Race/Ethnicity | |
| Caucasian | 323 (55) |
| African American | 95 (16) |
| Asian/ Pacific Islander | 25 (4) |
| Hispanic/Latino | 100 (17) |
| Other/Unknown | 46 (8) |
| Any chronic comorbidity | 319 (54) |
| Immune compromised | 89 (15) |
| Oncologic disease | 72 (12) |
| Duration of mechanical ventilation, days | 8 (4–16) |
| ICU length of stay, days | 11 (7–20) |
| Hospital length of stay, days | 20 (11–34) |
| Died | 99 (17) |
Performance of the Individual Methods
Only 327 (55%) could have IBW determined by all 4 IBW methods. The NCHS, McLaren and Moore methods were all able to calculate IBW in at least 90% of the cohort. The BMI method was only able to determine IBW in 357 (61%), largely because BMI growth charts have not been validated for those less than 2 years of age. Gender and race did not reach statistical significance for ability to determine IBW by any method. Age, as suspected, was statistically significantly associated with the proportion of subjects for which each method could successfully determine IBW. For NCHS, Moore, and BMI methods, the median age of subjects without a calculable IBW was 0.2 to 0.3 years while the median age of those with a successful IBW measurement was 4 years (for NCHS and Moore) and 10 years (for BMI method), Table 2. There was no difference in mean age among the groups with successful and unsuccessful IBW measurement with the McLaren method.
Table 2:
Comparison of Success of IBW Measurement by each IBW Method and Effect of Age on Successful Measurement
| Comparison Metric | IBW Measurement Method | |||
|---|---|---|---|---|
| NCHS | McLaren | Moore | BMI | |
| IBW measurement possible, n(%) | 576 (98) | 530 (90) | 576 (98) | 357 (61) |
| Age if measurement is possible, yearsa | 4 (0.7–11) | 4 (0.8–11) | 4 (0.7–11) | 10 (5–14) |
| Age if measurement is not possible, yearsa | 0.2 (0.1–0.17) | 0.5 (0.1–15) | 0.2 (0.2–0.9) | 0.3 (0.1–0.9) |
| p-value for age difference between IBW possible & not possible |
<0.0001 | 0.4 | 0.02 | <0.0001 |
Expressed as median (interquartile range).
Evaluation of Agreement between IBW Measurement Methods
Figure 1 shows the Bland-Altman plots for all 6 possible combinations of IBW methods while Table 3 summarizes the agreements between these combinations. In all comparisons, age greatly affected the levels of agreement between the IBW methods. Older children were more likely to plot outside the limits of agreement. This can be seen statistically in Table 3 and by noting the greater variation in IBW measurements at the higher averaged ideal body weights in Figure 1.
Figure 1:
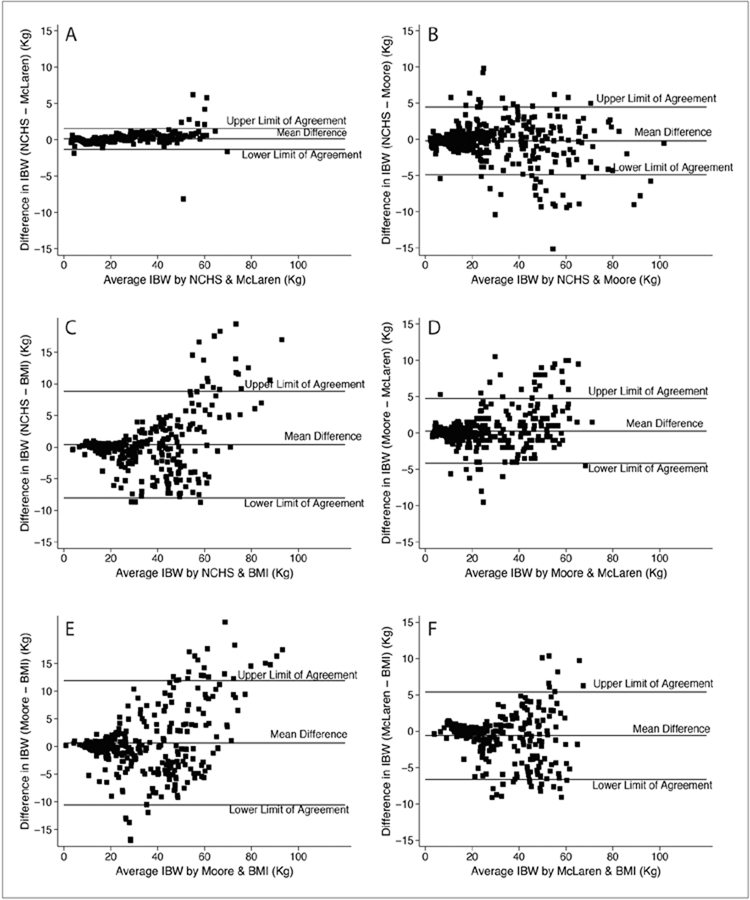
Bland-Altman plots comparing each of the 4 IBW methods to each other for the whole cohort. There comparison are as follows: NCHS to McLaren (A), NCHS to Moore (B), NCHS to BMI (C), Moore to McLaren (D), Moore to BMI (E), McLaren to BMI (F). A comparison with good agreement between the methods has a narrow range between upper and lower levels of agreement and few subjects outside the limits of agreement.
Table 3:
Limits of the Agreement Between Methods in Calculation of Ideal Body Weight
| Variables of Agreement | NCHS-McLaren | NCHS-Moore | NCHS-BMI | Moore-McLaren |
|---|---|---|---|---|
| Number of subjects in comparison, n(%) | 530 (90) | 571 (97) | 356 (67) | 525 (89) |
| Mean difference (SD), Kg | 0.14 ± 0.6 | −0.19 ± 2.2 | 0.44 ± 4.3 | 0.3 ± 2.2 |
| Upper limit of agreement (95% CI), Kg | 1.4 (1.3, 1.5) | 4.3 (3.9, 4.6) | 8.8 (8, 9.6) | 4.6 (4.3, 5) |
| Lower limit of agreement (95% CI), Kg | −1.1(−1.2, −1) | −4.6(−4.9, −4.3) | −8(−8.7, −7.2) | −4(−4.4, −3.7) |
| Median age within limits of agreement, (IQR), years | 4 (0.8–10.3)* | 3.3 (0.6–10)* | 9 (4.5–13.4)* | 3.4 (0.7–10)* |
| Median age outside limits of agreement, (IQR), years | 14 (13–15)* | 12 (10–16)* | 15 (13–16)* | 11.2 (10–13)* |
| Other variables affecting agreement | Gender | Chronic illness |
Good agreement between methods is determined by (a) more subjects within the area of agreement, and (b) narrow area of agreement.
represents p-value < 0.001 between the age of those within and outside of the limits of agreement. § No longer statistically significant after adjusting for age.
The two methods with the closest agreement were the NCHS and McLaren (Figure 1a). In this comparison, on average the NCHS method determined an IBW that was 0.14 ± 0.6Kg greater than the McLaren method. The upper and lower limits of agreement were +1.4Kg (95%CI 1.3, 1.5) and −1.1Kg (95%CI −1.2, −1) respectively. Therefore, there is 95% confidence that the true measurement difference between the 2 methods is between +1.4Kg and −1.1Kg, a level of agreement that seems clinically acceptable for most ages. Additionally, there were only 15 subjects (3%) whose differences in IBW measurement were outside the limits of agreement. Those outside the limits of agreement were much older, with a median age of 14 years (IQR 13 to 15) compared to a median age of 4 years (0.8 to 10.3) for those within the limits of agreement, p<0.0001. Additionally, those outside the limits of agreement were mostly female (73%) while the gender distribution of those within the limits of agreement were more equal (44% female, 56% male), p = 0.03.
Regarding all other comparisons, NCHS-Moore (Fig 1b), NCHS-BMI (Fig 1c), Moore-McLaren (Fig 1d), Moore-BMI (Fig 1e), and McLaren-BMI (Fig 1f), the limits of agreement were poor. All exhibited upper and lower limits of agreement greater than ± 4.5Kg, which may be clinically relevant for many patients. In the Moore-BMI comparison (Fig 1e), the upper and lower limits of agreement were over ±10Kg in difference between the two IBW measurements.
In all whole cohort comparisons, evaluations of association for race, ethnicity, gender (except in NCHS-McLaren as noted above) or PRISM-III with subjects within versus outside the limits of agreement did not reach statistical significance. In the NCHS-BMI and the McLaren-BMI comparisons, acute or chronic illness was associated with IBW measurement differences being outside versus within the limits of agreement, however in the BMI-McLaren comparison, this association is no longer statistically significant after adjusting for age. In the NCHS-BMI comparison, a greater proportion of those outside the limits of agreement (11%) reported chronic illness compared to 4% of those within the limits of agreement, p=0.046. In the McLaren-BMI comparison, a greater proportion of those outside the limits of agreement (43%) were immune compromised compared to 19.5% of those within the limits of agreement, p=0.01.
To determine if agreement of the IBW methods were different before and during/after puberty, we stratified the cohort at 10 years old. Figure 2 contains the Bland-Altman plots for subjects less than 10 years old, and Figure 3 shows the Bland-Altman plots for those 10 years or older.
Figure 2:
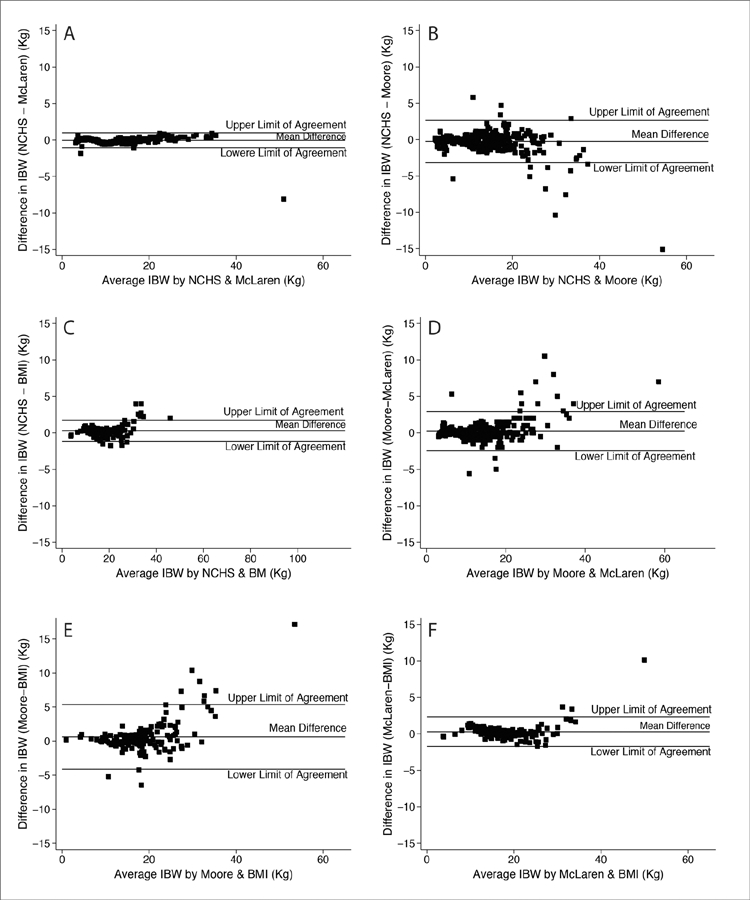
Bland-Altman plots comparing each of the 4 IBW methods to each other for subjects <10 years old. There comparison are as follows: NCHS to McLaren (A), NCHS to Moore (B), NCHS to BMI (C), Moore to McLaren (D), Moore to BMI (E), McLaren to BMI (F). A comparison with good agreement between the methods has a narrow range between upper and lower levels of agreement and few subjects outside the limits of agreement.
Figure 3:
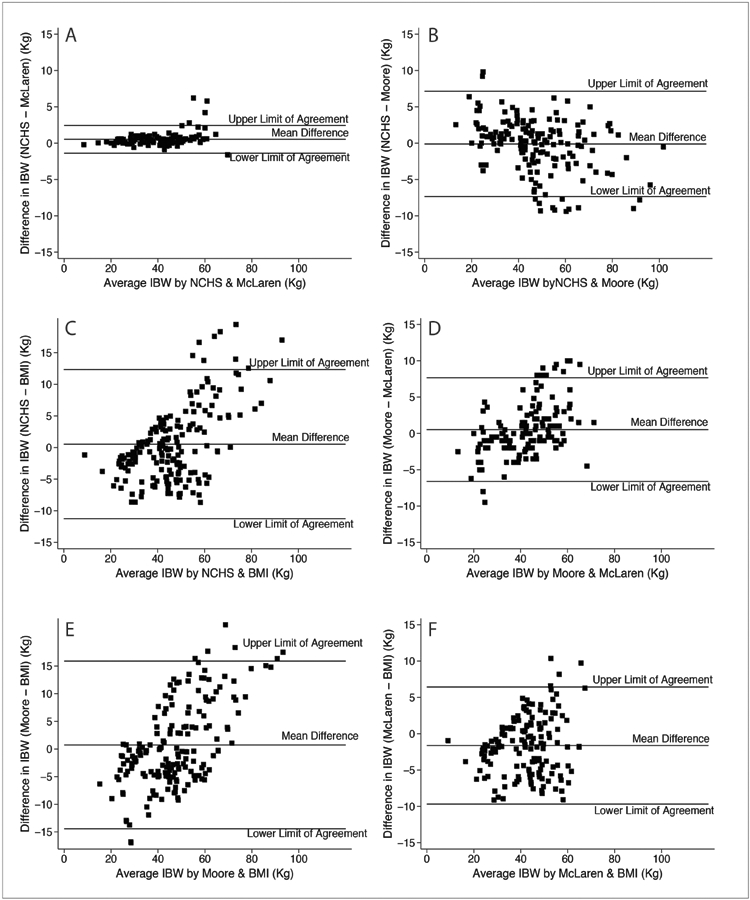
Bland-Altman plots comparing each of the 4 IBW methods to each other for subjects 10 years or older. There comparison are as follows: NCHS to McLaren (A), NCHS to Moore (B), NCHS to BMI (C), Moore to McLaren (D), Moore to BMI (E), McLaren to BMI (F). A comparison with good agreement between the methods has a narrow range between upper and lower levels of agreement and few subjects outside the limits of agreement.
In the <10-year old stratum, the agreement between methods was greater than within the older stratum. For all <10-year old comparisons except Moore-BMI, the upper and lower limits of agreement were within ±2.8Kg in mean difference between the 2 methods. For the Moore-BMI comparison (Fig 2e), the limits of agreement were greater at +5.2Kg (95%CI 4.5, 5.9) for the upper limit and −4Kg (95%CI −4.6, −3/4) for the lower limit. Age remained associated with those within versus outside the limits of agreement, with those outside the limits being older. The median age of those outside the limits of agreement ranged from 6.7 to 8.2 years for all comparisons. The median age of those within the limits of agreement ranged from 1.4 to 1.6 years for comparisons that did not include BMI method and was 4.5 years for comparisons with BMI method. In all comparisons, there were no other reported clinical or demographic variables that were notably different between subjects with IBW measurements within or outside the limits of agreement.
In the ≥10-year old stratum, the agreement between the IBW methods was very poor. Again, the closest agreement was between the NCHS and McLaren methods (Fig 3a). In this comparison, the upper and lower limits of agreement were within a likely clinically acceptable range at +2.5Kg (95%CI 2.2, 2.7) and −1.4Kg (95%CI −1.6, −1.1) respectively. All other comparisons exhibited upper and lower limits of agreement of greater than ±6Kg, with the widest range in the NCHS-BMI (Fig 3c) and Moore-BMI (Fig 3e) where the limits of agreement exceed ±10Kg in difference between the 2 methods. In all comparisons in the stratum, no reported clinical or demographic variables were notably different between subjects with IBW measurements within or outside the limits of agreement.
Evaluation of Prescribed Tidal Volumes by each IBW Method
Figure 4 shows the tidal volumes calculated by the 4 IBW methods for children ages 2–10 years and ≥10 year old when a 6mL/Kg IBW tidal volume is prescribed. In the 2–10 year old group, the mean prescribed tidal volume ranged from 107mL to 111mL with no clinical or statistically significant difference by IBW method used. However, the tidal volumes prescribed to the ≥10 year old subjects were more varied depending on the IBW method used. In this age group, the mean tidal volume prescribed in order of magnitude were: (a) McLaren 249 ±70mL, (b) BMI 277 ±80mL, (c) NCHS 281 ±99mL, and (d) Moore 285 ±104mL. These mean tidal volume differences reached statistical significance with p<0.0001 in the McLaren and BMI method comparison (mean difference of 9.8mL, 95% CI 5.9–13.6) and for the McLaren and NCHS method comparison (mean difference of 3.2mL, 95% CI 2.3–4.1). A sub-analysis was performed after removing the 5 subjects with prescribed tidal volumes of > 500mL when calculated by both NCHS and Moore but with no McLaren data because they were too tall for accurate IBW calculation by this method. The results of this sub-analysis were the same as above, signifying that these outliers did not skew the data.
Figure 4:
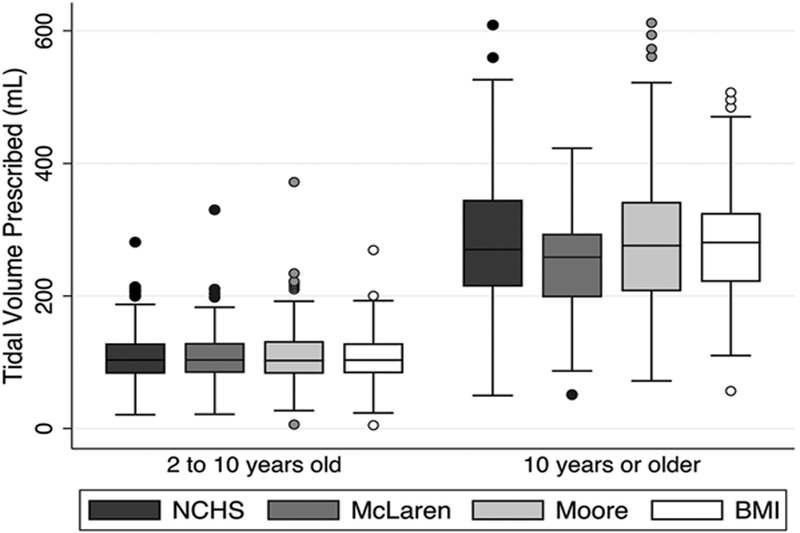
Tidal volumes calculated by the 4 IBW methods for children ages 2–10 years old and ≥10 years old when a 6mL/Kg IBW tidal volume is prescribed. P <0.001 for mean difference between McLaren and NCHS and McLaren and BMI methods in the ≥ 10 year old group.
Discussion
Since volutrauma was found to be a key driver of lung injury in mechanically ventilated adult ARDS patients(1), low tidal volumes of 5 to 8 mL per kilogram of IBW have been recommended for pediatric and adult ARDS management(1, 2). A major barrier to the use of IBW is the lack of clear consensus on the correct definition or method for determination of IBW in children.
In this analysis comparing NCHS, Moore, McLaren and BMI methods of pediatric IBW determination, we found great variance in calculated IBW among the methods, sometimes as much as a 10 Kg mean difference between two methods. We found the McLaren method to be the better IBW method. This conclusion is based on facts that this method is (a) easy to calculate using readily available growth charts, (b) is able to calculate IBW in over 90% of subjects, (c) had good agreement with the other methods, and (d) leads to a similar tidal volume prescription in young children and a lower tidal volume prescription in adolescents thereby potentially attenuating the risk of volutrauma in mechanically ventilated PARDS patients.
Other investigators have compared IBW methods in children and consistently found considerable variance among methods. In several studies using IBW as a marker of adequate nutrition, the number of children classified as malnourished varied substantially when different IBW methods were used(22–24). Phillips and colleagues compared Moore, McLaren and BMI methods in healthy subjects 3 months to 20 years old. They note good correlation between the methods at the 50th percentile for height and greater discrepancies in IBW measurements at the height percentile extremes. These studies emphasize the need for consensus on IBW method for both healthy and ill children.
The greatest discrepancies in our analysis occurred in the adolescent (≥10-year old) population. It is in this age group that the IBW measures led to statistically significant differences in tidal volume calculations for lung protective mechanical ventilation. Lung volumes, and therefore function, change as the size of the thoracic cage changes; however, the relationship is not linear. During the pubertal growth spurt the anthropometric proportions change and the growth spurt of the lung and thoracic cavity lag behind standing height(25–28). Therefore, at the start of puberty, adolescents tend to have small lungs for their stature. The difference in IBW measurement, and therefore tidal volume prescription, by the different IBW methods is especially important in these early adolescents given this lag in lung growth.
While we conclude that the McLaren method is the better method of IBW measurement, it does have shortcomings. This method is height based and not age based and children who are “too tall” (> 163cm in females and > 177cm in males) cannot have IBW measured by McLaren method. McLaren and colleagues advised that adult IBW formulae by used for these subjects, which are also height and not age based. With this method, children who are 2 or 3 years apart in age who have the same height will have the same calculated IBW. The importance of this age distinction has been debated in the past and remains unclear(29, 30). However, since 54% of this cohort reported prior chronic comorbidity, which may affect growth and nutritional status, a height-based method seems more appropriate. Our analysis showed that prior comorbidity affected the level of agreement between BMI and NCHS methods and between BMI and McLaren methods. Further investigation of the trajectory of lung growth in very tall adolescents and in those with chronic medical conditions is needed before additional recommendations can be provided.
This study has some limitations. There were no admission heights recorded in 113 (15%) subjects. While this reduced the size of the study cohort, it is unlikely to have greatly affected the conclusion since the data is likely missing at random. This does, however, reveal the lack of focus of intensive care practitioners on both nutritional status and tidal volume prescription in this very ill population. An additional limitation is the lack of statistical approach to compare several clinical measurement methods to each other when no gold standard exists. We used Bland Altman analysis to make several comparisons of two methods to each other. This methodology is descriptive in nature only, particularly in this case when a single clinically relevant difference in IBW measurement cannot be determined for all children and is probably age dependent.
In conclusion, this study evaluating IBW measurements by four commonly used methods reveals that there is great variance in calculated IBW among the methods, particularly in the pubertal/post-pubertal population. For critically ill children, particularly those with PARDS, a standard approach to IBW measurement is needed, since the varying results may lead to relevant discrepancies in care. We recommend that the next PARDS consensus statements address this issue in determining the method of IBW for wide use. Until broader consensus is achieved, we recommend the use of the McLaren method to calculate IBW in children with PARDS for both evaluation of nutritional status and for prescription of a low tidal volume, lung protective mechanical ventilation strategy. However, further analysis of lung volume and growth rate in adolescents, and especially in those with chronic medical conditions is necessary to better guide ventilator management in critically ill PARDS patients. Additional next steps include prospective evaluation of different IBW methods in all children admitted to the PICU and subsequent impact on a variety of aspects of care, including nutritional evaluation and medication dosing.
Supplementary Material
Acknowledgements:
We wish to thank Dr. Peter Bacchetti from the UCSF Departmentment of Epidemiology and Biostatistics for his valuable input to this analysis. We also wish to thank members of the Pediatric Acute Lung Injury and Sepsis Investigators (PALISI) network for their contribution to one or more of the original studies used to create the combined PARDS cohort.
Supported by National Institutes of Health grants 5T32HD049303–08 (Ward), K12HD047349 (Ward), NHLBI HL51856 (Matthay), K24 DK113381 (Liu)
Footnotes
Copyright form disclosure:
Dr. Ward’s institution received funding from the National Institutes of Health (NIH)/National Institute for Child Health and Development. Drs. Ward, Flori, and Matthay received support for article research from the NIH. Dr. Liu’s institution received funding from the NIH/National Heart, Lung, and Blood Institute (NHLBI) and the National Institute of Diabetes and Digestive and Kidney Disease, and she received funding from Achaogen, Durect (consulting), Z S Pharma (Advisory Board participant), Theravance (consulting), Quark (consulting), Potrero Med (consulting), Amgen (stockholder), the American Society of Nephrology (funding for travel), the National Kidney Foundation (ACKD Associate Editor), and National Policy Forum on Critical Care and Acute Renal Failure (funding for travel). Dr. Flori’s institution received funding from the NIH, and she received funding from Genentech, expert testimony reimbursement from a private law firm, and honoraria for educational lectures at referring hospital. Dr. Matthay’s institution received funding from the NIH/NHLBI/FDA, the Department of Defense, Bayer Pharmaceuticals, and GlaxoSmithKline; and he received funding from consulting for CS Berhling, Boerhinger-Ingelheim, Cerus Therapeutics, Quark Pharmaceuticals, and Thesan Pharmaceuticals. The remaining authors have disclosed that they do not have any potential conflicts of interest.
References:
- 1.The Acute Respiratory Distress Syndrome Network: Ventilation With Lower Tidal Volumes As Compared With Tradtional Tidal Volumes For Acute Lung Injury And The Acute Respiratory Distress Syndrome. N Engl J Med 2000; 342:1301–1308 [DOI] [PubMed] [Google Scholar]
- 2.Khemani R, Smith LS, Zimmerman JJ, et al. : Pediatric Acute Respiratory Distress Syndrome: Consensus Recommendations From the Pediatric Acute Lung Injury Consensus Conference. Pediatr Crit Care Med 2015; 16:428–39 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shah B, Sucher K, Hollenbeck CB: Comparison of Ideal Body Weight Equations and Published Height-Weight Tables With Body Mass Index Tables for Healthy Adults in the United States. Nutr Clin Pract 2006; 21:312–319 [DOI] [PubMed] [Google Scholar]
- 4.Degroodt EG, Quanjer PH, Wise ME, et al. : Changing relationships between stature and lung volumes during puberty. Respir Physiol 1986; 65:139–153 [DOI] [PubMed] [Google Scholar]
- 5.Cook CD, Hamann JF: Relation of lung volumes to height in healthy persons between the ages of 5 and 38 years. J Pediatr 1961; 59:710–714 [DOI] [PubMed] [Google Scholar]
- 6.Borsboom GJJM, Van Pelt W, Quanjer PH: Pubertal Growth Curves of Ventilatory Function: Relationship with Childhood Respiratory Symptoms. Am Rev Respir Dis 1993; 147:372–378 [DOI] [PubMed] [Google Scholar]
- 7.Hamill PV, Drizd TA, Johnson CL, et al. : Physical growth: National Center for Health Statistics percentiles. Am J Clin Nutr 1979; 32:607–629 [DOI] [PubMed] [Google Scholar]
- 8.Mclaren D, Read WC: Classification of nutritional status in early childhood. Lancet 1972; 3:146–148 [DOI] [PubMed] [Google Scholar]
- 9.Moore DJ, Durie PR, Forstner GG, et al. : The assessment of nutritional status in children. Nutr Res 1985; 5:797–799 [Google Scholar]
- 10.Ringwald-Smith K, Cartwright C, Mosby T: Medical nutrition therapy in pediatric oncology In: Elliott L, Molseed L, McCallum P, editor(s). The Clinical Guide to Oncology Nutrition Chicago, Il: American Diabetic Association; 2006. p. 114–116. [Google Scholar]
- 11.Martin Bland J, Altman D: Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986; 327:307–310 [PubMed] [Google Scholar]
- 12.Bland JM, Altman DG: Measuring agreement in method comparison studies. Stat Methods Med Res 1999; 8:135–160 [DOI] [PubMed] [Google Scholar]
- 13.Bernard GR, Artigas A, Brigham KL, et al. : The American-European Consensus Committee on ARDS: Definitions, Mechanisms, Relevant Outcomes, and Clinical Trial Coordination. Am J Respir Crit Care Med 1994; 149:818–824 [DOI] [PubMed] [Google Scholar]
- 14.Kuczmarski RJ, Ogden CL, Guo SS, et al. : 2000. CDC Growth Charts for the United States: methods and development 2002. [PubMed] [Google Scholar]
- 15.Barlow SE: Expert Committee Recommendations Regarding the Prevention , Assessment , and Treatment of Child and Adolescent Overweight and Obesity : Summary Report. Pediatrics 2007; 120:S164–S192 [DOI] [PubMed] [Google Scholar]
- 16.Onis M De Onyango AW, Borghi E, et al. : Development of a WHO growth reference for school-aged children and adolescents 2007; 43497:660–667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Barlow SE, Dietz WH: Obesity Evaluation and Treatment: Expert Committee Recommendations. Pediatrics 1998; 102:e29 LP–e29 [DOI] [PubMed] [Google Scholar]
- 18.Giavarina D: Lessons in Biostatistics: Understanding Bland Altman Analysis. Biochem Medica 2015; 25:141–151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wong HR, Shanley TP, Sakthivel B, et al. : Genome level expression profiles in pediatric septic shock indicate a role for altered zinc homeostasis in poor outcome. Physiol Genomics 2007; 30:146–155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hamilton C, Stamey J: Using Bland−Altman to Assess Agreement between Two Medical Devices – Don’t Forget the Confidence Intervals! J Clin Monit Comput 2007; 21:331–333 [DOI] [PubMed] [Google Scholar]
- 21.Pollack MM, Holubkov R, Funai T, et al. : The pediatric risk of mortality score: update 2015. Pediatr Crit Care Med 2016; 17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wright JA, Ashenburg CA, Whitaker RC: Comparison of methods to categorize undernutrition in children. J Pediatr 1994; 124:944–946 [DOI] [PubMed] [Google Scholar]
- 23.Lasky-Su J, Lyon HN, Emilsson V, et al. : On the Replication of Genetic Associations: Timing Can Be Everything! Am J Hum Genet 2008; 82:849–858 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhang Z, Lai H-C: Comparison of the use of body mass index percentiles and percentage of ideal body weightto screen for malnutrition in children with cystic fibrosis. Am J Clin Nutr 2004; 80:982–91 [DOI] [PubMed] [Google Scholar]
- 25.Seely J, Guzman C, Becklake M: Heart and lung function at rest and during exercise in adolescence. J Appl Physiol 1974; 36:34–40 [DOI] [PubMed] [Google Scholar]
- 26.Schrader P, Quanjer P, von Zomeren B, et al. : Changes in FEV1-height relationship during pubertal growth. Clin Resp Physiol 1984; 20:381–388 [PubMed] [Google Scholar]
- 27.Cole T: Linear and proportional regression models in the predicition of ventilatory function. Stat Soc A 1975; 138:297–338 [Google Scholar]
- 28.Simon G, Reid L, Tanner JM, et al. : Growth of Radiologically Determined Heart Diameter, Lung Width, and Lung Length from 5–19 Years, with Standards for Clinical Use. Arch Dis Child 1972; 47:373–381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Flegal K, Wei R, Odgen C: Weight-for-stature compared with body mass index-for-age growth charts for the United States from Disease Control and Prevention. Am J Clin Nutr 2002; 75:761–6 [DOI] [PubMed] [Google Scholar]
- 30.Phillips S, Edlbeck A, Kirby M, et al. : Ideal Body Weight in Children. Nutr Clin Pr 2007; 22:240–245 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


