Abstract
Objective.
Research supports the clinical importance of childhood irritability, as well as its developmental implications for later anxiety and depression. Appropriate treatment may prevent this progression; however, little evidence exists to guide clinician decision-making regarding treatment for chronic irritability symptoms. Given the empirical support for irritability as a dimension of oppositional defiant disorder (ODD), behavioral interventions that improve ODD symptoms, especially through emotion regulation training, are strong candidates for identifying effective treatment strategies for irritability.
Method.
Data from a randomized controlled effectiveness trial were used to assess hypotheses regarding irritability. The Stop Now and Plan (SNAP) Program was developed for pre-adolescent youths demonstrating clinically high rates of conduct problems. 252 boys ages 6 to 11 were assigned to participate in either SNAP or standard services; data were collected at four time points over 15 months.
Results.
Although lower irritability scores over time were seen for the SNAP group compared to standard services, the main effect for treatment was small and did not reach statistical significance. However, a significant indirect effect of SNAP treatment on irritability via improved emotion regulation skills was found; improved emotion regulation skills were associated with significant and substantial reduction in irritability.
Conclusions.
Specific effects of SNAP for the improvement of emotion regulation skills function as a mechanism for subsequent reductions in irritability, supporting the distinction between emotion regulation and irritability symptoms. Enhancing increased emotion regulation skills within existing evidence-based interventions for children with ODD should provide a strong foundation for treatments to target irritability symptoms.
Keywords: irritability, emotion regulation, oppositional defiant disorder, cognitive-behavioral therapy, intervention research
Childhood irritability
A growing literature base highlights the significance of the construct of childhood chronic irritability (e.g., Burke et al., 2014; Lochman et al., 2015). Researchers and clinicians distinguish between chronic and episodic irritability (Leibenluft, Cohen, Gorrindo, et al., 2006), the latter of which represents a marked change from typical functioning as in depression or pediatric bipolar disorder. In contrast, chronic irritability – often being touchy, angry and having temper outbursts – is seen as typical of an individual’s functioning, is more enduring, and is not circumscribed to episodic changes. Recent changes to diagnostic criteria in the Diagnostic and Statistical Manual of Mental Disorders (5th ed.; DSM-5; American Psychiatric Association, 2013) reflect the clinical significance of irritability as one of three dimensions within oppositional defiant disorder (ODD). Additionally, chronic irritability is a core feature of a new diagnosis, disruptive mood dysregulation disorder (DMDD), although important differences in persistence and frequency of these symptoms distinguish DMDD from the ODD irritability dimension.
The irritability dimension of ODD is formally characterized in the DSM-5 by the symptoms “often angry and resentful,” “often touchy or easily annoyed,” and “often loses temper.” This construct of irritability follows several empirical studies (e.g., Stringaris & Goodman, 2009a, 2009b) and has been supported by confirmatory factor analytic methods utilizing five large community samples comprising over 16,000 children (Burke, Boylan, Rowe, et al., 2014). On the other hand, debate remains about whether the aforementioned symptoms best index irritability. Other studies identify an alternative model in which the ODD symptoms of often being spiteful (instead of losing temper), along with being touchy and angry, best measure irritability (e.g. Burke, 2012; Burke, Hipwell, & Loeber, 2010; Lavigne, Bryant, Hopkins, & Gouze, 2015). Despite these differences, however, these studies are consistent in distinguishing a dimension within ODD symptoms that is characterized by persisting anger and touchiness. Studies are also consistent in finding associations between chronic irritability and depression and anxiety, along with an absence of prediction to other psychopathology (e.g., Lochman, Evans, Burke, et al., 2015; Vidal-Ribas, Brotman, Valdivieso, Leibenluft, & Stringaris, 2016). For the present analyses, we will measure chronic irritability using the symptoms of losing temper, being angry, and being touchy, following the model of Burke and colleagues (2014) and the DSM-5.
Research indicates that the irritable mood and defiant behavior dimensions of ODD are highly correlated but distinct components of the disorder (Burke et al., 2014; Stringaris & Goodman 2009b). Separate developmental courses support the utility of this distinction: while behavioral symptoms predict the development of conduct disorder (CD), irritability symptoms predict heightened risk for concurrent emotional disorders (Stringaris & Goodman, 2009a) and later anxiety and depression (Burke, 2012; Burke & Loeber, 2010; Burke, Hipwell, & Loeber, 2010; Rowe, Costello, Angold, et al., 2010; Stringaris & Goodman, 2009b, Vidal-Ribas et al., 2016). Even after controlling for baseline internalizing disorders, children and adolescents with elevated irritability symptoms are more likely to meet diagnostic criteria for “distress disorders” of depression and generalized anxiety disorder at three-year follow-up (Stringaris & Goodman, 2009b). This trend continues into emerging adulthood with irritability predicting greater risk for depression at age 18 (Burke, 2012). While researchers have begun to examine differential treatment effectiveness depending on ODD dimension presentation (Scott & O’Connor, 2012), there is presently an absence of intervention studies for these specific symptoms; thus, there is not yet a validated psychosocial treatment strategy for chronic irritability. Given the associated risks of this symptom profile across child development and into emerging adulthood, it is crucial to advance a reliable approach for reducing irritability.
Emotion regulation and treatment of ODD
The specificity in the connection between irritability within ODD and depression and anxiety suggests that individuals elevated on those symptoms of ODD may struggle in particular in how they manage emotions of anger and touchiness. Evidence has linked ODD (and disruptive behavior disorders more broadly) with difficulties in emotion regulation (ER), marked by the inability to modulate one’s affect for contextually appropriate functioning and to cope with negative and positive emotions (Dunsmore, Booker, & Ollendick, 2013; Green & Doyle, 1999; Shields & Cicchetti, 1998). While problems with ER are associated with a range of psychopathology, reflecting ER as a transdiagnostic construct, children with disruptive behaviors may be particularly at risk for emotional under-control (Southam-Gerow & Kendall, 2002).
Varied studies have linked symptoms associated with ODD to weaker ER skills. In a sample of children with ODD ranging from middle childhood to early adolescence, lower ER scores were related to elevated disruptive behavior problems (Dunsmore, Booker, Ollendick, & Greene, 2015). Five- to nine-year-olds presenting with severe temper outbursts, 88% of whom met criteria for ODD, were less able than control peers to regulate negative emotional expressivity in response to a frustration-eliciting task (Roy, Klein, Angelosante, et al., 2013). Shields and Cicchetti (1998) linked higher levels of an aggressive behavior construct (which included ODD symptoms and related behaviors) to less adaptive ER and more inappropriate affect expression within a mixed group of maltreated and non-maltreated 6- to 12-year-olds. Children presenting with ODD may also demonstrate greater emotional lability, a heightened reactivity to emotional stimuli accompanied by frequently shifting phases of intense negative affect (Dunsmore et al., 2013). Emotional lability is often, though not always, negatively associated with ER, which may be more skill-based in contrast to temperamentally-driven emotional lability (Dunsmore et al., 2013, 2015; Gouley, Brotman, Huang, & Shrout, 2008; Shields & Cicchetti, 1998).
Evidence strongly supports cognitive-behavioral treatments (CBT) as the first line of care for ODD and CD (Chorpita et al., 2011; Eyberg, Nelson, & Boggs, 2008). These interventions are predominantly focused on increasing compliance and reducing behavioral problems. Highly effective strategies directly target parenting behaviors, such as Parent Management Training (Kazdin, 2010) and Parent-Child Interaction Therapy (Zisser & Eyberg, 2010). Cognitive-behavioral strategies that engage with children themselves, such as Problem Solving Skills Training (PSST), also demonstrate significant improvement in disruptive behavior symptomology (Kazdin, 2010). Given the evidence that irritability is a distinct dimension of ODD symptoms, the success of psychosocial strategies for ODD underscores their promise for the treatment of irritability. Adapting existing empirically-supported treatment modalities (ESTs), especially those impacting ER, has the potential to efficiently generate a targeted and readily applicable intervention specific to irritability.
Although treatments for ODD predominantly focus on the reduction of the behavioral features of the disorder, aspects of ER in both caregivers and children have been shown to play a role in outcomes of existing treatment models for disruptive behavior. Some CBT programs enhanced by an ER component teach parents skills for their own affect management. One such approach, the Rational Positive Parenting Program, yielded greater reductions in oppositional-defiant behaviors at follow-up than standard CBT (David, David, & Dobrean, 2014). For emotionally labile children receiving Parent Management Training or Collaborative Problem Solving, greater behavioral symptom change was seen if mothers engaged in emotional coaching with their children prior to participating in treatment (Dunsmore et al., 2015). Oppositional kindergarteners with symptoms of irritability and spitefulness, labeled as “emotionally dysregulated,” experienced greater reduction in conduct problems from the Incredible Years intervention than did children whose symptoms were primarily behavioral; irritable and spiteful children may be differentially sensitive to the parenting environment (Scott & O’Connor, 2012).
The Stop Now and Plan (SNAP) Program is a cognitive-behavioral intervention enhanced by a focus on ER and direct instruction about social problem-solving skills (Augimeri, Farrington, Koegl, & Day, 2007; Burke & Loeber, 2015). SNAP was developed in Canada for pre-adolescent youth who have had contact with juvenile justice or manifest clinically high levels of conduct problems or aggressive behavior (Augimeri et al., 2007; Koegl, Farrington, Augimeri, & Day, 2008). A multi-component treatment, SNAP utilizes concurrent parent and child treatment groups for 12 weeks followed by individualized therapeutic, academic, or other support services as needed (Augimeri et al., 2007; Koegl et al., 2008).
Though SNAP was specifically designed for children referred for severe conduct problems, initial investigations of SNAP treatment outcomes demonstrated significant improvements not only for conduct symptoms and rates of police contact, but across both behavioral and affective symptom domains (Burke & Loeber, 2015, 2016). Compared to children receiving standard community care, children in SNAP displayed greater reductions of internalizing and externalizing problem behaviors, as well as symptom counts of ADHD, ODD, anxiety, and depression (Burke & Loeber, 2015). Unlike other hypothesized mechanisms for SNAP treatment effectiveness, including increased problem-solving ability and reduced parental distress, only enhanced ER skills mediated reductions in both aggressive behavior and anxiety-depression scores on the Child Behavior Checklist (CBCL; Achenbach & Rescorla, 2001; Burke & Loeber, 2016).
While previous reports demonstrated benefits of SNAP for targeted problem behaviors, the program has not yet been evaluated for its impact on chronic irritability. To the best of our knowledge, no psychosocial treatment has yet been demonstrated to be specifically effective in improving irritability symptoms among youth with behavioral problems in middle childhood. The absence of evidence surrounding treatment for chronic irritability underscores the salience of the current investigation. The present study examines data from a randomized controlled effectiveness trial of the SNAP Program (Burke & Loeber, 2015) for outcomes related to irritability symptoms of anger, touchiness, and temper, in order to generate novel information about potential key components effective in the specific treatment of irritability. Based on prior research, we hypothesize that SNAP will be associated with significant reductions in irritability over treatment as usual, and that this effect will be significantly mediated by improvements in ER skills (Figure 1). Finally, prosocial skills and defiant behavioral symptoms of ODD are key components of the measures from which constructs of emotion regulation and irritability are derived. Thus, we will include prosocial skills and defiant behavior as covariates predicted to be highly related to the indirect effect, and we hypothesize that controlling for changes in these constructs will not explain the effect of improved ER skills on the reduction of irritability.
Figure 1.
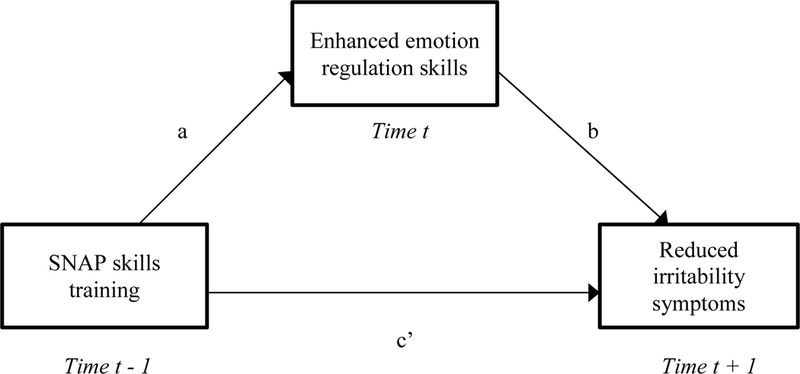
Model of the indirect effect of SNAP on irritability via emotion regulation.
Method
Data from the Pittsburgh SNAP Evaluation were used in this study. The study recruitment procedures, random assignment to treatment conditions, and assessment protocols have been reviewed in prior publications (Burke & Loeber, 2015, 2016). In brief, of 481 parents who inquired about treatment at one of two agencies providing SNAP services and received information about the study, 337 were interested in screening for enrollment. After exclusions due to study ineligibility, declining further participation, or being lost to contact, 252 participants were randomized into the study. Participant children were boys between the ages of 6 and 11, along with a parent each. Girls were excluded since only the SNAP treatment model for boys was being implemented in the region at the time of the study.
Participants were required to show significant behavioral problems in the form of a T-score greater than 70 on any of the aggressive, rule-breaking, or DSM conduct disorder subscales of the CBCL, or a T-score of 64 on the overall externalizing behavior subscale. Participants were required to have an IQ of 70 or above. Participants already involved in either SNAP treatment or high-intensity community services were excluded from the study, but those involved in less intensive behavioral health or pharmacotherapy services were not excluded. Siblings were not excluded from participation; there were 77 siblings in 36 sibling clusters. Randomization was performed based on parent participants; 122 were assigned to treatment as usual and 130 to SNAP participation.
Data collection.
Parents and children were interviewed in four waves: at baseline prior to randomization and commencement of study treatment, and then again at 3 months, 9 months, and 15 months after baseline. Parent-reported measures were collected via laptop interviews conducted by trained research staff who functioned independently from SNAP service providers. Participants were financially compensated for completing interviews. Interviews were typically conducted in family homes, but all families were offered the choice of alternate locations. Participants were informed of all study procedures prior to agreeing to study participation; written informed consent was obtained from all parents, as was assent from all children. Study procedures were overseen by the Institutional Review Board of the University of Pittsburgh.
SNAP Treatment.
The SNAP Program model includes two distinct phases. The first is an initial three-month period in which children participate in weekly small group treatment sessions, which include manualized training in problem-solving skills, ER skills, role-play activities, videotaped review, and peer critique of problem-solving strategies. During this time, parents participate in corresponding small groups to review treatment techniques, engage in problem-solving training, and discuss parenting practices and concerns. In the second phase of treatment, subsequent to the completion of the group component, families are reassessed to identify specific needs. To meet these needs, SNAP providers draw from an array of treatment modules, including for example SNAP family counseling, individual SNAP booster sessions, academic tutoring, school advocacy, mentoring, victim restitution, or intervention for fire-setting. These treatment components were delivered for as long as clinical staff deemed them necessary, based on individual needs. The Child Development Institute of Toronto, Canada (originators of the SNAP Program) monitored the implementation fidelity of the model. Study team members also conducted local fidelity checks. Adherence to specific SNAP treatment protocols was at least 92% or greater for all treatment groups.
Standard Services.
Those assigned to the standard services (STND) condition were given assistance by project staff to engage in behavioral health services, including initial referrals to providers of a high-intensity wraparound service. Youth in this condition may have received individual outpatient services, other group treatment, or other mental health services typically representative of the region’s standard of care.
Treatment Participation and Assessments.
The timing of assessments in this study was developed to provide for an assessment of change associated with the initial three-month group treatment period of the SNAP program, along with follow ups at six months and one year after the conclusion of the group treatment phase. It should be kept in mind that participants continued to receive individualized treatment that persisted potentially throughout this period and beyond, depending on individual clinical needs. Similarly, treatment in the standard service condition persisted throughout all assessment points in this study. Prior outcome research on the Pittsburgh SNAP Evaluation suggests that the greatest treatment gains in symptom reduction follow the three-month group component of SNAP, prior to onset of individualized services (Burke & Loeber, 2015).
Additionally, this study used an intent-to-treat design, meaning that once assigned to condition, participants were retained in the study regardless of their actual participation in services. Finally, the design of this study involved group participation (for the initial three months of treatment) in one treatment arm and individualized treatment in the other arm, resulting in a partially nested design. This means that observations in one arm may have been correlated with one another due to common group participation. However, empirical tests using a three-level modeling approach demonstrated a lack of systematic influence on observations due to treatment group participation. Further details regarding specific aspects of treatment participation, its relevance to outcomes, and the evaluation of the effect of partial nesting can be found in Burke and Loeber (2015, 2016).
Measures
Irritability.
Irritability, along with other behavioral symptoms of ODD, was measured using the Child Symptom Inventory-4: Parent Checklist (CSI-4; Gadow & Sprafkin 2002). The CSI-4 is a self-administered symptom checklist for parent report, directing parents to respond to each symptom item in a way that “best describes your child’s overall behavior,” from a choice of “never,” “sometimes,” “often,” or “very often.” Along with other measures, parents completed the checklist at four time points. Although theory and empirical evidence support the characterization of irritability as measured in the context of ODD to be chronic, it should be noted that the CSI-4 does not explicitly query the chronicity of symptoms over time. Thus, the use of the term “chronic irritability” for this construct rests on a presumption not explicitly assessed in the measurement, and should be interpreted with that in mind. Test-retest reliability and internal consistency alpha for ODD reported by Sprafkin and colleagues (2002) were 0.78 and 0.86, respectively. Based on the prior evidence for item assignment to dimensions (Burke et al., 2014), irritability was represented by the summed responses on the four-point scale from 0 (“never”) to 3 (“very often”) for the items “often loses temper,” “is touchy or easily annoyed,” and “is angry and resentful.” Defiant behavior was represented as the sum of the remaining five ODD items.
Prosocial Behavior and Emotion Regulation Skills.
The Social Competence Scale-Parent Version (SCS) is a 12-item measure created for the Fast Track Project (Conduct Problems Prevention Research Group, 1995). The scale includes two subscales for parents to assess their children’s ER skills and prosocial behavior skills on a five-point scale from 0 (“not at all”) to 4 (“very well”). The six ER items measured skills such as how well the child can accept things not going his way, how often he thinks before acting, or how well he can calm down when excited. Reliability alpha at baseline was 0.71, and the mean was 5.12 (SD = 3.3). The prosocial behavior construct consisted of six items measuring skills such as how well the child resolves problems on his own, listens to others’ points of view, or is helpful to others. Reliability alpha at baseline for this construct was 0.79; the mean score at baseline was 8.38 (SD = 4.2). The SCS has demonstrated concurrent validity with other measures of ER capacities: high social competence scores corresponded to high ER on the Emotion Regulation Checklist (Shields & Cicchetti, 1997; Gouley et al., 2008). Burke and Loeber (2016) demonstrated that anxiety and depression symptom improvement among children with behavioral problems were linked to the ER skills subscale specifically.
Data Analysis
The present data analytic strategy had to account for correlated observations at multiple levels in this data, including the clustering of siblings within families and repeated observations for individuals over time. In order to examine mediational models in this multilevel data, we used the ml_mediation procedure developed for Stata, which was adapted from the approach described by Krull and MacKinnon (2001). This procedure generates results for three equations: 1) a test of the c path; 2) a test of the a path; and 3) a test of the b and c’ paths, and offers options for subsequent bootstrap analysis. Subsequent analyses employed multilevel autoregressive mediational models to test each path separately. A Sobel test was used to evaluate the significance of the mediation effect.
Temporal ordering for causal analysis was preserved by assessing predictor, mediator, and outcome at three separate time points: SNAP treatment at time t - 1, ER skills at time t, and irritability at time t + 1. Maxwell and Cole (2007) have recommended this approach to prevent biased estimates of mediation due to simultaneous variable measurement. Values of the mediators were lagged by one wave relative to the outcome measurement of irritability, and age and wave were included as covariates. Next, a more rigorous test of longitudinal mediation was conducted to account for prior wave measurement of the outcomes of each path, controlling for emotion regulation and irritability respectively at time t - 1. Subsequent to tests of the hypotheses regarding mediation, regression models were tested to include additional covariates of ER skills. Effect sizes were estimated using Cohen’s f2, or the proportion of explained variance due to the specific effect of a given predictor, where values of .02 or greater are considered small, .15 or greater denote medium, and values above .35 indicate a large effect.
Results
Descriptive statistics in Table 1 demonstrate group-level demographic characteristics and baseline scores of irritability, defiant behavior, ER, and prosocial behavior. At baseline, there were no significant differences between SNAP and STND on irritability symptoms (F(1,247) = 2.19, p = .14), ER skills (F(1,250) = 2.44, p = .12), or prosocial behavior skills (F(1,250) = 1.74, p = .19).
Table 1.
Group-level demographic and baseline characteristics of children assigned to SNAP or Standard Services (STND).
| SNAP | STND | |
|---|---|---|
| African-American | 86.15% | 87.70% |
| M (SD) | M (SD) | |
| Age | 8.58 (1.73) | 8.38 (1.92) |
| ER Skills | 5.24 (3.75) | 4.50 (3.75) |
| Prosocial Skills | 8.42 (4.97) | 7.62 (4.63) |
| Irritability | 4.60 (2.21) | 5.02 (2.21) |
| Defiant Behavior | 7.60 (3.49) | 8.59 (3.53) |
Note. ER = Emotion Regulation. Group differences were non-significant.
Mediational model.
Table 2 shows the results of the three equations in the mediational model, assessing treatment, emotion regulation, and irritability at separate sequential time points. Controlling for age and wave, the direct effect of SNAP on irritability (c path) did not reach significance (B = −.35, SE = .29, p = .24). SNAP predicted significantly higher ER skills (a path; B = 1.48, SE = .51, p = .004), though the effect size was small. Higher ER skills were associated with significantly lower levels of irritability in the following wave (b path; B = −.12, SE = .03, p < .001), with a large effect size, and the effect of SNAP on irritability after accounting for the b path was reduced (c’ path; B = −.18, SE = .28, p = .51).
Table 2.
Tests of the mediational effect of emotion regulation (ER, time t) in the prediction from treatment group (SNAP, time t - 1) to irritability (IRR, time t + 1).
| Effect | Path | B | SE | f2 (ES) | p | 95% Conf. Int. | |
|---|---|---|---|---|---|---|---|
| Model 1 | |||||||
| SNAP on | |||||||
| IRR (direct) | c | −0.35 | 0.29 | 0.01 | 0.24 | −0.92 | 0.23 |
| Model 2 | |||||||
| SNAP on ER | a | 1.48 | 0.51 | 0.06 | 0.004** | 0.48 | 2.49 |
| Model 3 | |||||||
| ER on IRR | b | −0.12 | 0.03 | 0.37 | <0.001*** | −0.16 | −0.07 |
| SNAP on | |||||||
| IRR (indirect) | c’ | −0.18 | 0.28 | <0.01 | 0.51 | −0.73 | 0.36 |
Note. ES indicates effect size measured using Cohen’s f2, where f2 ≥ .02 denotes a small effect, ≥ .15 a medium effect, and ≥ .35 a large effect.
p < .05.
p < .01.
p < .001
While it might be argued (e.g., Baron & Kenny, 1986) that the non-significant c path suggests that there is not a treatment group effect present to be mediated, more recent approaches to mediation highlight the importance of evaluating indirect effects and suggest that significant a and b paths are the primary elements of concern (e.g., MacKinnon, Lockwood, Hoffman, West, & Sheets, 2002). The latter is true in the present analyses, and the indirect effect was significant (Sobel test = −2.44, SE = .07, p = .01). In terms of the mediation effect size, the ratio of the indirect effect to the total effect was .48; the ratio of the indirect to the direct effect was .94. A bootstrap replication of the multilevel mediation procedure, with 500 replications, resulted in the estimates shown in Table 3.
Table 3.
Estimates of the confidence interval and p value for the effects of the mediational model with three separate time points from bootstrap replication.
| Effect | B | Bootstrap SE | p | 95% Conf. Int. | |
|---|---|---|---|---|---|
| Indirect | −0.17 | 0.08 | 0.03* | −0.33 | −0.01 |
| Direct | −0.18 | 0.27 | 0.49 | −0.71 | 0.34 |
| Total | −0.36 | 0.29 | 0.22 | −0.92 | 0.21 |
Note.
p < .05.
p < .01.
p < .001.
Autoregressive mediational model.
To further explore the mediational model in the present analyses, we subjected it to a more rigorous test as recommended by Cole and Maxwell (2003) and Maxwell and Cole (2007). Specifically, we ran autoregressive mediational models in which we controlled for prior wave levels of the dependent variables in each of the a and b paths, as well as age and wave. The a path demonstrating the positive effect of SNAP on ER skills (time t) remained significant even after controlling for prior wave ER (time t – 1; B = 1.16, SE = .43, p = .007, 95% CI [0.32, 2.00]), and yielded a small effect (f2 = .07). The b path, predicting decreased irritability (time t) from ER skill improvement, also remained significant after controlling for prior wave irritability (time t – 1; B = .42, SE = .05, p < .001, 95% CI [0.32, 0.52]), and was reduced from a large to a medium effect size (f2 = .15). Even after controlling for prior wave measurement and limiting mediational analysis to three separate time points, the consistent strength of this path further supports the indirect effect.
Covariates closely associated with irritability or ER skills could also account for the observed relationship between the two variables. In particular, changes in prosocial skills, also measured by the SCS, or levels of the defiant behavior dimension of ODD might account for the observed relationship. Because prior research has found high intercorrelations between the two subscales of the SCS (Corrigan, 2003; CPPRG, 1995), as well as between the two dimensions of ODD symptoms (Burke et al., 2014), it was important to account for the potential explanatory effects of these covariates on the outcomes of interest. To evaluate this, a model was tested predicting irritability from prior wave measures of ER skills, prosocial skills, defiant behavior and treatment condition, and controlling for prior wave irritability, age, and wave. ER skills remained significantly predictive of reductions in irritability (B = −.07, SE = .03, p = .02, 95% CI [−0.13, −0.01]) while controlling for the significant and positive relationship between defiant behavior symptoms and later irritability (B = .09, SE = .04, p = .03, 95% CI [0.01, 0.18]). Prosocial skills (B = .01, SE = .02, p = .81, 95% CI [−0.04, 0.05]) did not significantly predict irritability.
Discussion
The current study aimed to identify whether a CBT program designed to treat disruptive behavioral problems among boys in middle childhood also yielded improvements in symptoms of chronic irritability: anger, touchiness, and loss of temper. An additional goal of the study was to understand whether enhanced ER played a specific role in reducing irritability. Our initial hypothesis was not supported, in that the difference in irritability reduction between SNAP and treatment as usual (STND) did not reach significance, with children in both treatment conditions showing improvements in irritability symptoms.
Our hypotheses regarding an indirect effect involving improved ER skills were supported. The SNAP treatment was associated with a significant increase in ER skills, which in turn predicted improvements in irritability symptoms. This relationship held when controlling for prior levels of ER and irritability, as well as changes in prosocial skills and behavioral ODD symptoms. The conservative mediational modeling approach, controlling for prior levels of outcome variables for each path, suggests the indirect effect is robust and meaningful. Even after accounting for the autoregressive effects of prior irritability, ER skills added to the explanation of future irritability symptoms, suggesting that while mechanistically related, ER skills appear to act independently of irritability. These findings thus highlight the need to attend to distinctions in these two constructs.
The finding that SNAP is associated with indirect improvement in irritability via ER skills is especially promising as it fills a gap in the treatment literature for middle childhood. The intervention utilizes a two-pronged approach for targeting emotion regulation skills: reducing negative affect reactivity and practicing and reinforcing the implementation of prosocial behaviors as alternatives to displays of anger and irritability. Because SNAP shares many core characteristics with other CBT-based ESTs, such as identifying links among emotions, thoughts, and behaviors, as well as teaching coping skills, other interventions may yield similar effects in the treatment of irritability. Though we are currently unable to evaluate effects of SNAP relative to other specific interventions, future research should address whether characteristics unique to group-based treatments like SNAP provide greater in-session practice and subsequent improvement in the self-regulation of affect. Participating in role plays of challenging social scenarios, watching one’s role plays in video review, and receiving and participating in peer feedback may all contribute to enhanced outcomes relative to treatments that do not include such components. These elements provide children with opportunities to collaborate with peers to develop ER strategies, and to practice the use of ER skills as steps to greater prosocial behavior and problem-solving skills during distressing interactions. It may be that in vitro practice with peers further enhances the positive effects of improvements in ER on the increased risks for negative peer interactions that have been associated with irritability (Evans, Pederson, Fite, Blossom, & Cooley, 2015; Stringaris & Goodman, 2009a).
Because of the evidence linking irritability to later depression and anxiety, the present results may suggest a method to not only reduce irritability, but to potentially reduce subsequent depression (Stringaris, Maughan, Copeland, et al., 2013) or anxiety (Stoddard, Stringaris, Brotman, et al., 2014). These broader effects depend on a chain of mechanistic linkages, from ER skills to irritability to depression or anxiety. By and large, evidence supports these linkages independently, but it is not difficult to imagine factors that might potentially influence the strength of each link, such as gender, age, family functioning, or comorbid psychopathology among a host of others. Much remains in the work needed to evaluate the circumstances under which this particular mechanism might have the most utility, but the present work identifies this indirect pathway as a potentially important guide to refining interventions.
One possible intervention following from these results may be the development of a stand-alone module for irritability. Children with disruptive behavior disorders and dysregulated mood seeking outpatient services have been treated with psychotropic medications in increasing numbers by psychiatrists and by non-psychiatric physicians (Olfson, Blanco, Wang, Laje, & Correll, 2014). For clinicians working with children who are irritable and have ODD or DMDD, an evidence-based CBT module offers a compelling psychosocial treatment option. This may be preferable to the use of psychotropic medications, particularly in advance of any evidence validating the effectiveness of pharmacotherapy for chronic irritability. Additionally, these results highlight the use of SNAP for the improvement of ER abilities in general, independent of their subsequent effect on irritability. Emotion dysregulation, in varied forms, is present in most psychological disorders (Southam-Gerow & Kendall, 2002). Many children seeking mental health services struggle with affective regulation and would benefit from improvements in their coping strategies.
Limitations.
While the current study supports CBT strategies for irritability, methodological limitations of sampling and outcome measurement must be considered. The current study sample was representative of individuals seeking treatment for disruptive behavior in the urban neighborhoods in which the study was conducted, and was over-representative of African-American children. However, this limits our ability to generalize our findings to children who identify as neither African-American nor Caucasian. Importantly, the current study’s findings cannot yet be generalized to girls; research is warranted to understand the relationship between irritability and emotion regulation across genders. It is also unclear whether the intervention’s indirect effect would hold if SNAP were implemented during mid-adolescence, when chronic irritability severity peaks for both boys and girls (Leibenluft et al., 2006). Additionally, because this study utilized a single-rater evaluation of symptomology, it is possible that the association between improved ER and reduced irritability was influenced by parent bias in indicating improvement across outcome domains. That said, rater bias is unlikely to fully explain the relationship between ER and irritability, since parent-endorsed improvements in defiant behavior and prosocial skills did not explain the effects of interest. Future studies employing multiple informants and measurement strategies are needed to address this concern.
An additional limitation of the current research is the measurement of ER using the SCS six-item subscale, which may provide a less nuanced illustration of a child’s skills in comparison to more comprehensive measures. However, our finding of significant predictive ability of ER skills independent of SCS prosocial behavior suggests that this construct of ER has validity, which is consistent with prior research (Burke & Loeber, 2016; Gouley et al., 2008). Future studies may benefit from multiple forms of ER measurement, which would better capture which self-regulatory strategies are most readily adopted and employed by children who manifest a reduction in irritability. In addition, the relationship between irritability and affective functioning is likely multifaceted, and further exploration should include the role of emotional lability (Dunsmore et al., 2013). More in-depth understanding of the roles played by both ER and emotional lability in the development of chronic irritability may inform more sophisticated treatment approaches targeting affective dysregulation.
The implications of this study are clear: preliminary evidence supports the provision of psychosocial treatment for irritability, and a specific group-format CBT program, SNAP, indirectly improves irritability among boys with behavioral problems. The mechanism of ER in this model of change indicates a key target for the adaptation of current therapeutic modalities. If existing CBT programs can be modified to more effectively promote ER skills in children, clinicians may harness these treatments to better address both affective and behavioral symptoms among young clients with chronic irritability.
Acknowledgments
FUNDING
This work was supported by a grant (07–365-01) from the Department of Health of the Commonwealth of Pennsylvania to Drs. Loeber and Burke, and by a grant to Dr. Burke (MH 074148) from the National Institute of Mental Health.
Footnotes
Ms. Derella, Mr. Johnston, and Drs. Burke and Loeber have no conflicts of interest to report.
Contributor Information
Olivia J. Derella, Department of Psychological Sciences, University of Connecticut. 406 Babbidge Rd Unit 1040, Storrs, CT 06269
Oliver G. Johnston, Department of Psychological Sciences, University of Connecticut. 406 Babbidge Rd Unit 1040, Storrs, CT 06269
Rolf Loeber, Rolf Loeber, Department of Psychiatry, University of Pittsburgh, Sterling Plaza 201 N Craig St, Pittsburgh, PA 15213.
Jeffrey D. Burke, Department of Psychological Sciences, University of Connecticut. 406 Babbidge Rd Unit 1040, Storrs, CT 06269
References
- Achenbach TM & Rescorla LA (2001). Manual for the ASEBA school-age forms & profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth, & Families. [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: Author. [Google Scholar]
- Augimeri LK, Farrington DP, Koegl CJ, & Day DM (2007). The SNAP™ under 12 outreach project: Effects of a community based program for children with conduct problems. Journal of Child and Family Studies, 16, 799–807. [Google Scholar]
- Baron RM & Kenny DA (1986). The moderator–mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology, 51, 1173–1182. [DOI] [PubMed] [Google Scholar]
- Burke JD (2012). An affective dimension within oppositional defiant disorder symptoms among boys: Personality and psychopathology outcomes into early adulthood. Journal of Child Psychology and Psychiatry and Allied Disciplines, 53, 1176–1183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burke JD, Boylan K, Rowe R, Duku E, Stepp SD, Hipwell AE, & Waldman ID (2014). Identifying the irritability dimension of ODD: Application of a modified bifactor model across five large community samples of children. Journal of Abnormal Psychology, 123, 841–851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burke J, & Loeber R (2010). Oppositional defiant disorder and the explanation of the comorbidity between behavioral disorders and depression. Clinical Psychology: Science and Practice, 17, 319–326. [Google Scholar]
- Burke JD, & Loeber R (2015). The effectiveness of the stop now and plan (SNAP) program for boys at risk for violence and delinquency. Prevention Science, 16, 242–253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burke JD, & Loeber R (2016). Mechanisms of behavioral and affective treatment outcomes in a cognitive behavioral intervention for boys. Journal of Abnormal Child Psychology, 44, 179–189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chorpita BF, Daleiden EL, Ebesutani C, Young J, Becker KD, Nakamura BJ, … Starace N (2011). Evidence-based treatments for children and adolescents: An updated review of indicators of efficacy and effectiveness. Clinical Psychology-Science and Practice, 18, 154–172. [Google Scholar]
- Cole DA, & Maxwell SE (2003). Testing mediational models with longitudinal data: Questions and tips in the use of structural equation modeling. Journal of Abnormal Psychology, 112, 558–577. [DOI] [PubMed] [Google Scholar]
- Conduct Problems Prevention Research Group (CPPRG). (1995). Social Competence Scale (Parent Version). University Park, PA: Pennsylvania State University. [Google Scholar]
- Corrigan A (2003). Social Competence Scale – Parent Version, Grade 2 /Year 3 (Fast Track Project Technical Report). University Park, PA: Pennsylvania State University. [Google Scholar]
- David OA, David D, & Dobrean A (2014). Efficacy of the Rational Positive Parenting Program for child externalizing behavior: Can an emotion-regulation enhanced cognitive-behavioral parent program be more effective than a standard one? Journal of Evidence-Based Psychotherapies, 14, 159–178. [Google Scholar]
- Dunsmore JC, Booker JA, & Ollendick TH (2013). Parental emotion coaching and child emotion regulation as protective factors for children with oppositional defiant disorder. Social Development, 22, 444–466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunsmore JC, Booker JA, Ollendick TH, & Greene RW (2015). Emotion socialization in the context of risk and psychopathology: Maternal emotion coaching predicts better treatment outcomes for emotionally labile children with oppositional defiant disorder. Social Development, 25, 8–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans SC, Pederson CA, Fite PJ, Blossom JB, & Cooley JL (2015). Teacher-reported irritable and defiant dimensions of oppositional defiant disorder: Social, behavioral, and academic correlates. School Mental Health, 7, 1–13. [Google Scholar]
- Eyberg SM, Nelson MM, & Boggs SR (2008). Evidence-based psychosocial treatments for children and adolescents with disruptive behavior. Journal of Clinical Child and Adolescent Psychology, 37, 215–237. [DOI] [PubMed] [Google Scholar]
- Gadow KD, & Sprafkin J (2002). Childhood Symptom Inventory-4 Screening and Norms Manual. Stony Brook, NY: Checkmate Plus. [Google Scholar]
- Gouley KK, Brotman LM, Huang KY, & Shrout PE (2008). Construct validation of the social competence scale in preschool-age children. Social Development, 17, 380–398. [Google Scholar]
- Greene RW, & Doyle AE (1999). Toward a transactional conceptualization of oppositional defiant disorder: Implications for assessment and treatment. Clinical Child and Family Psychology Review, 2, 129–148. [DOI] [PubMed] [Google Scholar]
- Kazdin AE (2010). Problem-Solving Skills Training and Parent Management Training for oppositional defiant disorder and conduct disorder In Weisz JR, & Kazdin AE (Eds.). Evidence-based psychotherapies for children and adolescents, 2nd Ed. (211–226). New York, NY, USA: Guilford Press. [Google Scholar]
- Koegl CJ, Farrington DP, Augimeri LK, & Day DM (2008). Evaluation of a targeted cognitive-behavioral program for children with conduct problems--The SNAP Under 12 Outreach Project: Service intensity, age and gender effects on short- and long-term outcomes. Clinical Child Psychology and Psychiatry, 13, 419–434. [DOI] [PubMed] [Google Scholar]
- Krull JL, & MacKinnon DP (2001). Multilevel modeling of individual and group level mediated effects. Multivariate Behavioral Research, 36, 249–277. [DOI] [PubMed] [Google Scholar]
- Leibenluft E, Cohen P, Gorrindo T, Brook JS, & Pine DS (2006). Chronic versus episodic irritability in youth: A community-based, longitudinal study of clinical and diagnostic associations. Journal of Child and Adolescent Psychopharmacology, 16, 456–466. [DOI] [PubMed] [Google Scholar]
- Lochman, J. E, Evans, S. C, Burke, J. D, Roberts, M. C, Fite, P. J, Reed, G. M, … Elena Garralda M (2015). An empirically based alternative to DSM-5’s disruptive mood dysregulation disorder for ICD-11. World Psychiatry, 14, 30–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon DP, Lockwood CM, Hoffman JM, West SG, & Sheets V (2002). A comparison of methods to test mediation and other intervening variable effects. Psychological Methods, 7, 83–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maxwell SE, & Cole DA (2007). Bias in cross-sectional analyses of longitudinal mediation. Psychological Mediation, 12, 23–44. [DOI] [PubMed] [Google Scholar]
- Olfson M, Blanco C, Wang S, Laje G, & Correll CU (2014). National trends in the mental health care of children, adolescents, and adults by office-based physicians. JAMA Psychiatry, 71, 81–90. [DOI] [PubMed] [Google Scholar]
- Rowe R, Costello J, Angold A, Copeland W, & Maughan B (2010). Developmental pathways in oppositional defiant disorder and conduct disorder. Journal of Abnormal Psychology, 119, 726–738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roy AK, Klein RG, Angelosante A, Bar-Haim Y, Leibenluft E, Hulvershorn L, … Spindel, C. (2013). Clinical features of young children referred for impairing temper outbursts. Journal of Child and Adolescent Psychopharmacology, 23, 588–596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott S, & O’Connor TG (2012). An experimental test of differential susceptibility to parenting among emotionally dysregulated children in a randomized controlled trial for oppositional behavior. Journal of Child Psychology and Psychiatry, 53, 1184–1193. [DOI] [PubMed] [Google Scholar]
- Shields AM, & Cicchetti D (1997). Emotion regulation among school-age children: The development and validation of a new criterion Q-sort scale. Developmental Psychology, 33, 906–916. [DOI] [PubMed] [Google Scholar]
- Shields AM, & Cicchetti D (1998). Reactive aggression among maltreated children: The contributions of attention and emotion dysregulation. Journal of Clinical Child Psychology, 27, 381–395. [DOI] [PubMed] [Google Scholar]
- Southam-Gerow MA, & Kendall PC (2002). Emotion regulation and understanding: Implications for child psychopathology and therapy. Clinical Psychology Review, 22, 189–222. [DOI] [PubMed] [Google Scholar]
- Stoddard J, Stringaris A, Brotman MA, Montville D, Pine DS, & Leibenluft E (2014). Irritability in child and adolescent anxiety disorders. Depression and Anxiety, 31, 566–573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stringaris A, & Goodman R (2009a). Three dimensions of oppositionality in youth. Journal of Child Psychology and Psychiatry and Allied Disciplines, 50, 216–223. [DOI] [PubMed] [Google Scholar]
- Stringaris A, & Goodman R (2009b). Longitudinal outcome of youth oppositionality: Irritable, headstrong, and hurtful behaviors have distinctive predictions. Journal of the American Academy of Child and Adolescent Psychiatry, 48, 404–412. [DOI] [PubMed] [Google Scholar]
- Stringaris A, Maughan B, Copeland WS, Costello EJ, & Angold A (2013). Irritable mood as a symptom of depression in youth: Prevalence, developmental, and clinical correlates in the Great Smoky Mountains Study. Journal of the American Academy of Child and Adolescent Psychiatry, 52, 831–840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vidal-Ribas P, Brotman MA, Valdivieso I, Leibenluft E, & Stringaris A (2016). The status of irritability in psychiatry: A conceptual and quantitative review. Journal of the American Academy of Child & Adolescent Psychiatry, 55, 556–570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zisser A, & Eyberg SM (2010). Parent-Child Interaction Therapy and the treatment of disruptive behavior disorders In Weisz JR, & Kazdin AE (Eds.), Evidence-based psychotherapies for children and adolescents, 2nd Ed. (179–193). New York, NY: Guilford Press. [Google Scholar]


