Abstract
This case report represents a novel technique for the treatment of a pseudoaneurysm of the aorta. Pseudoaneurysm of the aorta has been reported in patients post heart surgery. This case report is about a patient who had a pseudoaneurysm most probably following tuberculosis. Traditionally, the treatment of choice is surgical correction; however, in the current era, there are case reports describing the use of either stent grafts or Amplatzer occluders for occlusion of the pseudoaneurysm in high-risk surgical cases. We performed successful closure of the aortic pseudoaneurysm using atrial septal occluder.
<Learning objective: Tuberculous arteritis can result in pseudoaneurysm rarely. Our patient had a large aneurysm compressing adjoining vital structures and was very high surgical risk case. This is the first case report of closure of tuberculous pseudoaneurysm by using atrial septal occluder in a young patient. In this case we have demonstrated that large pseudoaneurysms with narrow neck can be closed very safely using atrial septal occluder with immediate symptom relief and thrombosis of pseudoaneurysm at follow-up of three months.>
Keywords: Pseudoaneurysm of aorta, Atrial septal occlude, Device closure
Introduction
Aortic pseudoaneurysms have been described following surgery, trauma, or tuberculosis. Tuberculous pseudoaneurysm has been described with an incidence of 0.3% in more than 20,000 autopsies [1]. Tuberculous pseudoaneurysms are caused by contained aortic rupture following tuberculous aortitits. Aortitis is generally secondary to extension of infection from periaortic foci [2]. Presentation of tuberculous pseudoaneurysm can be either due to tuberculous infection or compressive symptoms due to compression of neighboring structures such as esophagus, trachea, or bleeding from aneurysm or embolic episodes. With current advanced imaging techniques such as computed tomography (CT) scan or magnetic resonance imaging diagnosis is generally made. Even though surgery is the most described therapy for patients with aortic pseudoaneurysm, it carries definite risks of morbidity and mortality. There have been case reports describing use of endovascular grafts and atrial septal occluders [4], [5], [6], [7], [8], [9] for closure of aortic pseudoaneurysms following cardiac surgery in elderly patients. We describe endovascular closure by atrial septal occluder of large tuberculous aortic pseudoaneurysm in a young patient who was deemed unsuitable for surgery.
Case report
A 25-year-old female presented with symptoms of gradual onset dyspnea over a period of 3 months and had dyspnea at rest [New York Heart Association (NYHA) grade IV] two weeks prior to presentation. She also had dull chest pain along with persistent dry hacking cough. On examination, she was breathless at rest and orthopneic. Oxygen saturation in seated position with high flow oxygen was 90% which would fall to 70% on assuming the supine position.
She was on anti-tuberculous therapy for the treatment of tuberculous pericardial effusion since 5 months which included 3 months of five-drug regimen (streptokinase, isoniazid, rifampicin, pyrazinamide, and ethambutol) and was currently receiving two drugs (isoniazid and rifampicin). Her serial chest X-rays revealed homogenous opacity from left hilum extending into left upper lobe of the left lung which had increased in size over a period of four months. Her echocardiography revealed dilated right atrium and right ventricle secondary to external compression of the main pulmonary artery. There was peak gradient of 58 mmHg across compressed main pulmonary artery. On further investigation with a CT scan it was found that she had a pseudoaneurysm arising from the undersurface of the aortic arch originating opposite to the origin of the right subclavian artery (Fig. 1). This aneurysm was extending up to the sternum. Echo review suggested a communication neck measuring 9 mm between arch of aorta and aneurysm (Fig. 1).
Fig. 1.
(1) Echocardiography showing communication between aorta (A) and pseudoaneurysm (B) with well-defined margins. (2) Computed tomography (CT) scan of thorax with contrast revealing large pseudoaneurysm arising from arch of aorta, extending anteriorly up to sternum. (3) CT scan of thorax with contrast revealing large pseudoaneurysm seen compressing main pulmonary and right pulmonary artery. (4) CT scan of thorax with contrast revealing large pseudoaneurysm arising from arch of aorta occupying left upper side of thorax.
Cardiac surgery was deemed high risk considering that the aneurysm was in close proximity to the sternum and overall poor condition of patient. The pseudoaneurysm was compressing the main pulmonary artery trunk and pushing its way under the bifurcation of the trachea compressing the left main bronchus. Considering the location of communication opposite to neck vessels a stent graft was not possible. We considered percutaneous closure of the communication using an atrial septal occluder.
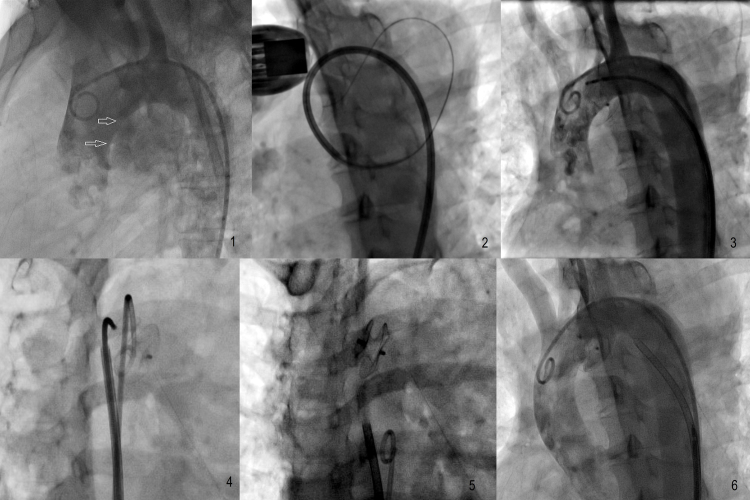
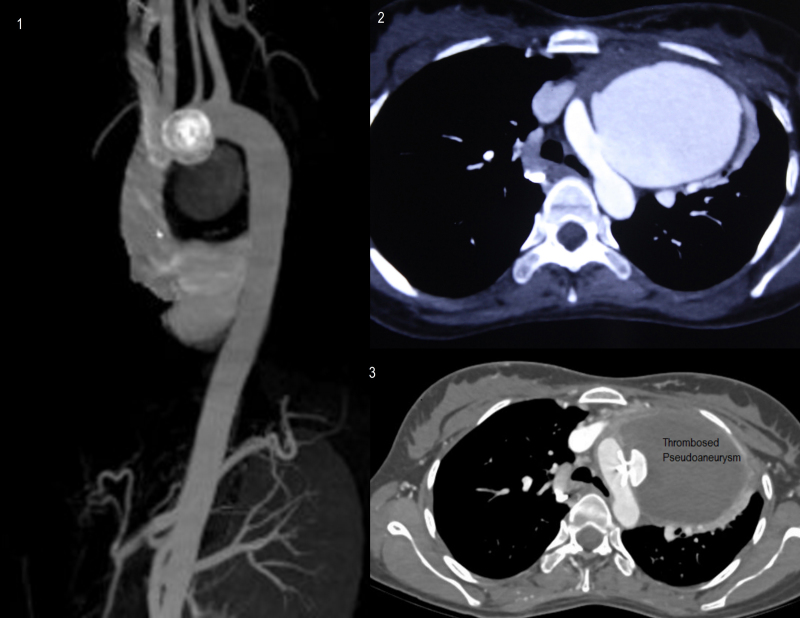
Under local anesthesia a 7 Fr bifemoral access was taken. The patient had received 325 mg of aspirin and 300 mg of clopidogrel prior to the procedure; 5000 units of unfractionated heparin were administered. A review angiography in the left anterior oblique and lateral view revealed a 9 mm opening within the undersurface of the aortic arch (Fig. 2, Video 1). Communication was entered using a 6F JR catheter with the help of a 300 cm Terumo wire [Japan]. A 7F long cocoon curved sheath was inserted into the aneurysm. Curved sheath was selected to overcome angulation of the arch of aorta (Fig. 2). A 10 mm Cocoon ASD device[Vascular Innovations Thailand] was inserted, and its position was checked with contralateral aortic pigtail shoot in both right anterior oblique and left anterior oblique views and with transthoracic echocardiography (Video 2). The device was released after confirmation of sealing of communication on echocardiography and angiography (Fig. 2, Video 3). A small leak remained on echocardiography and angiography post procedure. Her follow-up echocardiography showed 90% thrombosis of aneurysm on the third day with complete cessation of the leak. The patient showed gradual improvement in saturation over one week. She was discharged on the 7th day on dual antiplatelet therapy of aspirin and clopidogrel. On discharge, her oxygen saturation at rest was 94% at room air. Over a period of three months her dyspnea resolved completely, and only mild intensity dry cough persisted. Her echocardiograph at her three-month visit showed a gradient of 22 mm across the pulmonary artery. Her follow-up CT scan revealed thrombosed residual pseudoaneurysm with central colliquation and device in situ (Fig. 3). Echocardiography revealed reduction in main pulmonary artery compression. Gradient across main pulmonary artery had reduced to 16 mmHg. Symptomatically, the patient had no dyspnea and was NYHA Grade I/II.
Fig. 2.
(1) Aortogram in left anterior oblique (LAO) 60 view shows communication (arrows) between aorta and pseudoaneurysm. (2) 7F long-curved sheath seen entering the aneurysm. (3) Aortogram in LAO view showing release of both discs nearly occluding the defect. (4) Aortogram in right anterior oblique (RAO) view confirming the separation of both discs on both sides. (5) Released device in RAO view. (6) Aortogram confirming sealing of communication with minimal foaming.
Fig. 3.
(1) Reconstructed follow-up computed tomography (CT) aortogram at one month revealing complete sealing of communication between aorta and pseudoaneurysm. (2) Preprocedure CT contrast image showing opacification of aorta and pseudoaneurysm with communication (arrows). (3) Follow-up CT contrast image showing opacification of aorta, device and nonopacification and thrombosis of pseudoaneurysm.
Discussion
Pseudoaneurysms of aorta have been reported rarely following surgery, trauma, or tuberculosis [1], [2]. Surgical repair has remained the therapy of choice but with high morbidity and mortality. There are reports of various percutaneous methods such as the use of stent grafts [3], coils, or injection of thrombin for closure of pseudoaneurysms [4]. Use of Amplatzer ASD device [St Jude Medical, USA] has been described in various case reports [5], [6], [7].
Most of the patients described before have been elderly post-operative patients. Our patient is a young woman with no discernible cause, most probably secondary to previous tuberculosis infection. We demonstrated successful use of cocoon ASD device in a patient with spontaneous pseudoaneurysm with immediate and a three-month follow-up. Cocoon atrial septal occluder is more or less similar to the Amplatzer septal occluder used in previous reports. The cocoon septal occluder is used in transcatheter atrial septal defect closure. It is made of nitinol wires covered with platinum using nano fusion technology. The septal occluder is a self-expandable, double-disk device connected by a waist at the center of the discs. The discs are filled with polypropylene fabric to assist in thrombogenecity.
In our opinion, an ASD device with the use of a curved sheath to overcome the angulation of the aortic arch is a suitable option in selected patients with pseudoaneurysm with good immediate- and medium-term outcome. Relative ease and safety of procedure in the hands of an experienced operator may lead to this procedure becoming the treatment of choice in selected patients. Immediate benefit of occlusion may be due to reduction in systolic pressure inside pseudoaneurysm resulting in reduced pressure on the pulmonary artery. Even though immediate outcome was good in this patient, we will follow up this patient with CT imaging to see the long-term outcome. We also feel that this type of therapy may be useful in selected patients who are at high-risk surgically as bridge therapy before definitive surgery.
Conflicts of interest
The authors declare no conflicts of interest.
Footnotes
Supplementary data associated with this article can be found, in the online version, at http://dx.doi.org/10.1016/j.jccase.2016.10.004.
Appendix A. Supplementary data
The following are the supplementary data to this article:
Aortogram in left anterior oblique 60 degrees view shows communication between aorta and pseudoaneurysm.
Aortogram in right anterior oblique view shows separation of both discs and occlusion of the communication with minimal foaming of contrast.
Aortogram in left anterior oblique view after the release of device reveals almost complete occlusion of defect with minimal contrast foaming.
References
- 1.Parkhurst G.F., Decker J.P. Bacterial aortitis and mycotic aneurysm of the aorta: a report of twelve cases. Am J Pathol. 1955;31:821–835. [PMC free article] [PubMed] [Google Scholar]
- 2.D’Attellies N., Diemont F.F., Julia P.L., Cardon C., Fabiani J.N. Management of pseudoaneurysm of the ascending aorta performed under circulatory arrest by port-access. Ann Thorac Surg. 2001;71:1010–1011. doi: 10.1016/s0003-4975(00)02265-7. [DOI] [PubMed] [Google Scholar]
- 3.Zhang C., Chen B., Gu Y., Luo T., Yang S., Liang W., Wang Z. Tuberculous abdominal aortic pseudoaneurysm with renal and vertebral tuberculosis: a case and literature review. J Infect Dev Ctries. 2014;8:1216–1221. doi: 10.3855/jidc.4954. [DOI] [PubMed] [Google Scholar]
- 4.Fann J.I., Samuels S., Slonim S., Burdon T.A., Dalman R.L. Treatment of abdominal aortic anastomotic pseudoaneurysm with percutaneous coil embolization. J Vasc Surg. 2002;35:811–814. doi: 10.1067/mva.2002.121744. [DOI] [PubMed] [Google Scholar]
- 5.Lin P.H., Bush R.L., Tong F.C., Chaikof E., Martin L.G., Lumsden A.B. Intra-arterial thrombin injection of an ascending aortic pseudoaneurysm complicated by transient ischemic attack and rescued with systemic abciximab. J Vasc Surg. 2001;34:939–942. doi: 10.1067/mva.2001.116968. [DOI] [PubMed] [Google Scholar]
- 6.Stasek J., Polansky P., Bis J., Brtko M., Klzo L., Babu A., Vojacek J. The percutaneous closure of a large pseudoaneurysm of the ascending aorta with an atrial septal defect Amplatzer occluder: two-year follow-up. Can J Cardiol. 2008;24:e99–e101. doi: 10.1016/s0828-282x(08)70703-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bashir F., Quaife R., Carroll J.D. Percutaneous closure of ascending aortic pseudoaneurysm using Amplatzer septal occluder device: the first clinical case report and literature review. Catheter Cardiovasc Interv. 2005;65:547–551. doi: 10.1002/ccd.20422. [DOI] [PubMed] [Google Scholar]
- 8.Kanani R.S., Neilan T.G., Palacios I.F., Garasic J.M. Novel use of the Amplatzer septal occluder device in the percutaneous closure of ascending aortic pseudoaneurysms: a case series. Catheter Cardiovasc Interv. 2007;69:146–153. doi: 10.1002/ccd.20794. [DOI] [PubMed] [Google Scholar]
- 9.Hussain J., Strumpf R., Wheatley G., Diethrich E. Percutaneous closure of aortic pseudoaneurysm by Amplatzer occluder device—case series of six patients. Catheter Cardiovasc Interv. 2009;73:521–529. doi: 10.1002/ccd.21833. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Aortogram in left anterior oblique 60 degrees view shows communication between aorta and pseudoaneurysm.
Aortogram in right anterior oblique view shows separation of both discs and occlusion of the communication with minimal foaming of contrast.
Aortogram in left anterior oblique view after the release of device reveals almost complete occlusion of defect with minimal contrast foaming.