Abstract
Background
In industrial countries, home care of community dwelling elderly people is rapidly growing. Frequent injuries in home caregivers result from slips, trips, and falls (STFs). The current study tests attentional cognitive failure to mediate the association between work stressors and STFs.
Methods
A sample of 125 home caregivers participated in a questionnaire study and reported work interruptions, unreasonable tasks, quality-threatening time pressure, conscientiousness, attentional cognitive failures, and STFs.
Results
In structural equation modeling, the mediation model was shown to fit empirical data. Indirect paths with attentional cognitive failures as the link between work stressors and STF were all significant in bootstrapping tests. An alternative accident-prone person model, that suggests individual differences in conscientiousness to predict attentional cognitive failures that predict more frequent work stressors and STFs, showed no significant paths between work conditions and STFs.
Conclusion
To prevent occupational injury, work should be redesigned to reduce work interruptions, unreasonable tasks, and quality-threatening time pressure in home care.
Keywords: fall prevention, home care, occupational health
1. Introduction
In Switzerland, 30,000 home care nurses are employed in that profession. Demographic trends forecast that the need for home care will increase in future years [1]. Accidents at work among home care nurses are frequent and tend to increase; in Switzerland, in the decade from 2003 to 2012, the number of accidents rose from 69.2 to 76.1 accidents per 1000 full-time home care nurses [1]. Therefore, the risk of accident is higher than the average in health care (60 accidents per 1000 full-time employees) [1]. An examination of the types of accidents in home care nurses shows that the most frequent type, which accounts for 36% of all accidents, is slips, trips, and falls (STFs) [1]. Within STFs, most accidents occur on dry, even flooring, with no patient involvement (30%), followed by STF on stairways with no patient involvement (25%). STF of nurses with no patient involvement happen on wet or slippery surfaces inside the residency 6% of the time and outside of the residency 11% of the time. Some STF involve carrying objects (4%) or commuting to and from patients' homes (4%). Comparably, few STF of home care nurses involve STF of patients (“safe the patient-situations,” 4%). Phillips characterizes care in the client's home to be comparatively uncontrolled [2]. Hignett et al [3] report strong evidence that interruptions and distractions from pets, relatives, children, and television are related to safety risks. In addition, close interaction with patients and relatives often results in requests which “were not on the treatment plan and/or outside the caregiver job description” [3, p. 5], i.e., requests that include unreasonable tasks. Home care requires nurses to cope with inadequate infrastructure in homes, such as narrow bedrooms and small bathrooms [4]. In addition to ergonomic risk factors, some task-related risk factors at work are also high. For example, time pressure is high not only because of the care timetable but also because of additional time targets that are required by the clients and their relatives [5]. Therefore, in interviews, home care nurses often mention time as a salient safety concern [6]. Confirmative evidence showed a recent review of safety risks for home care nurses that reported time pressure as a threat to safety [3]. One of the most important differences between home care and hospital care is that home care nurses mostly work alone [3]. When working alone, team support in difficult situations is not available [3]. When working alone, time pressure, missing consumables, and lack or change of devices more often relate to cognitive risks in decision making and risky task execution with regard to medical device use, carrying objects, multitasking, choice of walking route, etc. More risky decisions often inherently generate risky postures and movements [3]. For instance, a risky decision is to carry objects in both hands while entering a stairway and being unable to use the handrail because of the perceived need to hurry and avoid making two trips. Interruptions, unreasonable tasks, and time pressure may trigger more risky decisions regarding how to perform a task [7]. The more risky way of task execution does not imply a lack of attention to the task at hand. Indeed, sometimes attention might be even higher when the risk is evident, e.g., home nurses watching their steps while entering a wet surface instead of making a detour [3]. Nevertheless, time pressure, interruptions, and unreasonable tasks often distract attention from the task at hand [8], [9]. In home care, the tasks at hand often include walking, and attention on potentially slippery surface is adaptive [10], [11]. Human attention to “potentially” slippery surfaces includes significant adaptive differences in gait biomechanics [10]. Attention to slippery flooring conditions and associated change in heel contact dynamics lower the slip parameters even with risky footwear like Crocs and flip-flops [12], [13]. Thus, attentional cognitive failures are plausible when mediating between time pressure, interruptions, and unreasonable tasks on the one hand and STF on the other. Wallace and Chen define attentional cognitive failure as the failure to keep one's attention focused on the on-task (i.e., task-relevant) information while working [9, p. 617]. Hence, the current study tests attentional cognitive failures as a partial mediator of the link between work stressors and STFs.
1.1. Attentional cognitive failure and STF
In everyday life, stressful situations and maintenance of postural control are habitual, and slips can even occur without detection. However, these are extremely low magnitude slips that do not require a postural corrective response. Such slips are easily forgotten unless a daily protocol calls attention to them [6]. Laboratory experiments showed that postural control is worse when individuals simultaneously engage in another attention-demanding task. Lower postural control is associated with higher risk of STF and high attention demands as requested by a Stroop task corresponded to lower concurrent postural control (and higher risk of STF) [9]. Using the experimental dual-task paradigm, undertaking a cognitively demanding task (e.g., a Stroop task) led to reduced balance performance in the middle-aged workforce [9]. Laboratory research shows self-reported stress levels and salivary cortisol levels to be negatively related to postural control performance in young women [14]. In sum, experimental studies have demonstrated the close association between postural control and attentional control [15]. In occupational life, STF may result from cognitive failure. In a test of this risk model in naval accidents, cognitive failure—including attentional cognitive failure—mediated the link between stress experience and accidents during routine walking activities on board (e.g., knocks against foreign objects, tripping on gangplanks, and falling through open hatches [16]). Hence, we suggest that attentional cognitive failure contributes to STFs and task-related stressors, such as interruptions, unreasonable tasks, and time pressure, can lead to attentional cognitive failure (which can lead to STFs).
1.2. Work interruptions, attention, and STF
In the work of home care nurses, interruptions from patients and their relatives, as well as from children and pets, seem to be common [2]. Interruptions are not bad per se [17], [18]. In many care-giving situations, there is a need to switch from one task to another more “urgent” task [18]. Thus, in emergency situations, interruptions can be beneficial, but in many other situations—such as being asked for advice while dispensing drugs—they are not [18]. Recently, work interruptions have been shown to be related to attention failure in surgical nurses [8]. In many situations, interruptions distract attention from the task at hand, and caregivers have to store in their working memory the intent to restart the interrupted operation and where to begin again [17], [18]. Overall, evidence shows that interruptions are linked to increased mental workload [19], [20], [21], [22] and therefore, interruptions are expected to be linked with STFs. Hence, we expect work interruptions to decrease the level of cognitive attention, leading to STFs.
1.3. Unreasonable tasks, attention, and STF
A task is perceived as unreasonable when employees think they should not have to carry out this task [23], [24], [25], such as requests frequently received by home care nurses which are outside the nurse's job description [2]. Caregiving activities played a role in the development of the concept of unreasonable tasks when qualitative reports from nurses were analyzed [24]. In those reports, nurses' tasks were seen as unreasonable if they fell outside the range of one's occupational role [26]—for example, a home caregiver being asked to do work that is regarded as a service rather than a nursing activity (e.g., opening a window for a client who can easily to do that by him or herself). The unique contribution of unreasonable tasks to well-being and strain has been confirmed beyond the effects of other stressful working conditions [24]. Unreasonable tasks threaten occupational self-esteem (“I should not have to do this” [27]) and, therefore, shift one's mind to himself or herself instead of the task at hand. Therefore, attentional cognitive failure in care is a likely consequence of unreasonable tasks. Until now, no study has tested unreasonable tasks to predict attentional cognitive failure and STFs in home caregivers.
1.4. Time pressure, attention, and STF
Time pressure is common in the work of home care nurses [2]. Nurses feel rushed when the amount of work to be performed within a certain timeframe exceeds their individual capabilities. Time pressure at work is often related to the focusing of attention on prioritizing task completion goals, while safety goals become less salient and receive less attention [28], [29]. For safety concerns including STFs, attention to safety goals, including “moving safely,” is important. The safety goal of moving safely involves secondary task activities, such as clearing something that is on the steps of a staircase out of the way before climbing the stairs. Such secondary task activities are likely to be reduced when under time pressure at work [30]. Quality-threatening time pressure explicitly focuses on the need to adapt action regulation to time pressure, even when quality goals—including safety goals—must be lowered to finish tasks in time [31], [32]. Safe movement as a safety goal is likely to be weakened when quality-threatening time pressure is high. Hence, we expect quality-threatening time pressure to reduce the attention paid to safe movement and posture and to predict STFs.
1.5. The present study
The main research question that guided the present study was whether work stressors in home care predict attentional cognitive failure, and whether attentional cognitive failure predicts STF. Work interruption, unreasonable tasks, and time pressure were expected to be positively associated with attentional cognitive failure and STFs. Attentional cognitive failure is expected to mediate partially the link between work stressors and STFs. It was previously shown that conscientiousness is negatively related to attentional cognitive failure [9]. In this study, the focus is on working conditions; associations between work stressors and attentional cognitive failure and STFs should hold, even when conscientiousness is controlled for in the analyses.
2. Materials and methods
2.1. Sample
Two agencies of a nationwide home care organization were contacted for participation in the questionnaire study. Both adjacent agencies in a large city agreed to participate and allocated 0.5 hours of work to their employees for filling out a questionnaire. All 206 members of the home care staff were invited to fill out the questionnaire that included the all self-report instruments measuring work interruptions, unreasonable tasks, time pressure, conscientiousness, attention failure, and STF. The participation rate was 63%, with 130 participants who gave informed consent and filled out the questionnaire. Five questionnaires were excluded from the analysis because of too much missing information (more than 5% of all questions were not answered [33]). Among 125 participants, 113 were women (90.4%). Mean age was 43.9 years (SD = 12.9 years). Most participants were of Swiss nationality (79.2%). Mean tenure was 5 years in home care and 3 years in the current organization. The job qualifications were a home care assistant degree (10%), home care vocational certificate degree (42.4%), university home care degree (36.8%), or other degree (12.8%). Only 8.4% of the participants worked full-time (42 h/wk), 48.6% of participants worked between 84 hours (part-time) and 150 hours (full time: 168 hours), 43% worked less than part-time (42 hours). All responses to questionnaire questions were anonymous. The study was carried out in accordance with the code of ethics of the World Medical Association (Declaration of Helsinki) and the Swiss Society of Psychology.
2.2. Measure
2.2.1. Work interruptions
Interruptions of work were assessed by three items from a shortened version of the Instrument for Stress-Oriented Task Analysis (version 5.1 [34]). A sample question is “How often are you interrupted by other colleagues during the course of your work activity?” With response options ranging from 1 (very rarely/never) to 5 (very often/several times an hour). Cronbach α was 0.85.
2.2.2. Unreasonable tasks
The Bern Illegitimate Tasks Scale [24] assesses unreasonable tasks with four items. Items are introduced with the lead-in phrase “Do you have work tasks to take care of, which you believe…,” followed by statements such as “… should be done by someone else?” Responses ranged from 1 (never) to 5 (frequently). Cronbach α was 0.83.
2.2.3. Time pressure
Quality-threatening time pressure in the workplace was assessed using three items [31], [32], which go beyond other questionnaires on time pressure intensity by focusing on time pressure that is too high to perform well [31], [32], [35]. Participants rated three statements on a 5-point scale, ranging from 1 (does not apply) to 5 (fully applies). A sample question is “Time pressure at work is so great that quality sometimes suffers”. Cronbach α was 0.81.
2.2.4. Conscientiousness
Conscientiousness is part of the 5-factor model of personality [36]. The 5-factor model questionnaire used in the present study was based on an adjective rating list developed by Ostendorf and Angleitner [37]. The adjective rating list was reduced by Schallberger and Venetz, who demonstrated that a shorter questionnaire version was satisfactory in terms of factorial structure and internal consistency of scale [38]. Conscientiousness scale consisted of bipolar items on a 6-point scale, with each pole marked as 1 or 6 (very), followed by 2 and 5 (quite), with the center being 3 and 4 (rather). Conscientiousness included three items (e.g., unthoughtful vs. proper). Cronbach α was 0.61.
2.2.5. Attention failure
Attention failure at work was assessed with the subscale on attention failure from the Workplace Cognitive Failure Scale [9] in the German validated translation [39]. The scale consisted of five self-report items with a 5-point Likert response format, ranging from 1 (very rarely/never) to 5 (very often). A sample question is “(How often do you)… day-dream when you ought to be listening to somebody?” The internal consistency of the scale was satisfactory (Cronbach α = 0.81).
2.2.6. Slips, trips, and falls
STFs at work were assessed by an adapted scale from Elfering et al [40]. Five items asked about stumbling, slipping, and near-falling in the previous 4 weeks at work. The directions were “The following question refers to near-accidents occurring during work during the last 4 weeks. Near-accidents characterize situations in which you narrowly escaped experiencing an accident. For instance, near-accidents that occur while you are walking include stumbling on something without falling.” Items were “I stumbled,” “I slipped,” “I nearly fell on the stairs,” “I lost body balance,” and “I bruised my arm or leg,” with five response options from 1 (never) to 5 (very often). Cronbach α was 0.84.
2.3. Data analyses
An a priori power calculation based on expectation of a moderate effect size (f2 = 0.15) for a multiple linear regression of STFs on five predictor variables and a requirement of an 80% power to detect an existing deviation of f2 from zero resulted in a required sample size of 92 participants. AMOS 24.0 was applied to model the latent path structure of the hypothesized mediation model. Root mean square error of approximation (RMSEA) and comparative fit index indicated the fit between empirical correlations and structural models (0.05 < RMSEA ≤ 0.08 and comparative fit index > 0.90 indicate acceptable fit; [41]). The mediation hypotheses were tested by a bootstrap test of the indirect effects. In addition to a test of the hypothesized structural equation model, an alternative plausible model should be considered. Persons differ in attention regulation, and trait attention regulation was also suggested as a potential cause of errors and action slips [42]. Thus, a plausible alternative model is a person-oriented “accident-prone person” model, which postulates that individuals lower in conscientiousness tend to have higher attentional cognitive failure that causes them to increase both their STF and their mental load at work by themselves, for example, by interrupting themselves by checking electronic messages or forgetting tasks and timelines, thus generating time pressure that would not have existed otherwise. Hence, for an “accident-prone person,” self-made mental workload might mediate the effects of (stable) attentional cognitive failures on STFs. As hypotheses were directional, one-tailed tests of significance are appropriate [43], [44].
3. Results
3.1. Mean levels
Table 1 shows the range, mean values, standard deviations (SDs), and estimates of reliability of self-report measures. Interruptions at work were moderate (mean = 2.55, SD = 1.00). The mean level of unreasonable tasks was lower (mean = 1.94, SD = 0.74). Time pressure at work was moderate (mean = 2.35, SD = 0.86). The mean level of attentional cognitive failures was 2.20 (SD = 0.60) and a bit higher than values for 323 participants from various occupations, as reported by Wallace and Chen (2.04) [9]. The mean level of conscientiousness in the study sample was 4.84 (SD = 0.75). Mean values for STFs at work in last 4 weeks were low (mean = 1.71, SD = 0.57).
Table 1.
Descriptive statistics and internal consistencies (Cronbach α).
| Scales | Items | Range | M | SD | Cronbach α |
|---|---|---|---|---|---|
| Work interruptions | 3 | 1–5 | 2.55 | 1.00 | 0.85 |
| Unreasonable tasks | 4 | 1–5 | 1.94 | 0.74 | 0.83 |
| Quality-threatening time pressure | 3 | 1–5 | 2.35 | 0.86 | 0.84 |
| Conscientiousness | 3 | 1–6 | 4.84 | 0.75 | 0.61 |
| Attentional cognitive failures | 5 | 1–5 | 2.20 | 0.60 | 0.81 |
| STFs | 5 | 1–5 | 1.71 | 0.57 | 0.84 |
M, mean; SD, standard deviation; STFs, slips, trips, and falls.
N = 113.
3.2. Correlations
Table 2 shows correlations among study variables. Interruptions, unreasonable tasks, and time pressure were significantly related [r(113) = 0.34 to .46, p < 0.001]. Interruptions, unreasonable tasks, and time pressure were positively related to attentional cognitive failures [r(113) = 0.42 to .49, p < 0.001]. Conscientiousness was negatively related to interruptions [r(113) = −0.29, p < 0.01], but conscientiousness was not associated with unreasonable tasks [r(113) = −0.05, ns] and time pressure [r(113) = −0.05, ns]. Correlations between work stressors and STFs were positive [interruptions: r(113) = 0.20, p < 0.05; unreasonable tasks: r(113) = 0.31, p < 0.001; time pressure: r(113) = 0.25, p < 0.01]. Attentional cognitive failures and STFs were positively related [r(113) = 0.43, p < 0.001], but STFs and conscientiousness were not [r(113) = −0.06, ns].
Table 2.
Pearson correlations among study variables.
| Scales | (1) | (2) | (3) | (4) | (5) | (6) |
|---|---|---|---|---|---|---|
| (1) Work interruptions | ||||||
| (2) Unreasonable tasks | 0.34*** | |||||
| (3) Quality-threatening time pressure | 0.38*** | 0.46*** | ||||
| (4) Conscientiousness | −0.29** | −0.05 | −0.05 | |||
| (5) Attentional cognitive failures | 0.49*** | 0.44*** | 0.42*** | −0.27** | ||
| (6) STFs | 0.20* | 0.31*** | 0.25** | −0.06 | 0.43*** |
STFs, slips, trips, and falls.
N = 113; *p < 0.05, **p < 0.01, ***p < 0.001, one-tailed.
3.3. Structural equation analyses
Table 3 shows the results of the tests of the structural equation model, including several indicators of model fit. In the notes, there are comments that explain when fit indices can be considered to represent a good model fit. A model that assumes independence (Model 1: independence model) between manifest variables and a latent variable has very poor fit and thus did not represent the data at all. In contrast, a saturated model that estimates all relations between variables reached maximal fit (Model 2), and both the independence model and saturated model provide a frame of reference for specific model tests. Hypothesis testing started with a test of the measurement model. The measurement model included interruptions, unreasonable tasks, time pressure, conscientiousness, attentional cognitive failures, and STFs as latent variables, with all items of scale as manifest indicator variables of the latent variable. Thus, every latent variable represents factor values of a scale from confirmatory factor analysis. The measurement model represented the empirical data well (RMSEA = 0.062) [38]. Thus, the confirmatory factor analyses within the measurement model proved the hypothetical factor structure. The hypothesized mediation model also represented the empirical data well (RMSEA = 0.062). Indeed, the measurement model and the hypothesized mediation model were identical in model fit.
Table 3.
Structural equation models fit to empirical data.
| Models | χ2 | df | χ2/df | p | RMSEA | CFI | AIC |
|---|---|---|---|---|---|---|---|
| (1) Independence model | 1340.47 | 253 | 5.30 | 0.000 | 0.196 | 0 | 1432.47 |
| (2) Saturated model | 0 | 0 | 0 | – | – | 1.00 | 761.09 |
| (3) Hypothesized mediation model | 307.642 | 215 | 1.43 | 0.000 | 0.062 | 0.915 | 429.64 |
| (4) Alternative accident-prone person model | 313.55 | 216 | 1.45 | 0.000 | 0.063 | 0.910 | 433.55 |
The models are as follows: (1) independence model assumes there are no associations between study variables; (2) saturated model assumes all variables were interrelated—estimates best possible fit of model variables and empirical data; (3) hypothesized mediation model = mediation model shown in Fig. 1; (4) alternative accident-prone person model = trait model, conscientiousness predicts attentional cognitive failure, and attentional cognitive failure predicts time pressure, interruptions, and unreasonable tasks. χ2 = chi-square value indicates the minimum discrepancy between empirical covariance structures and those implied by the model; df = degrees of freedom; p = probability the discrepancy will differ from zero (should be non-significant in a good model); χ2/df = minimum discrepancy divided by its degrees of freedom, as an indicator of fit; p = p value of minimum discrepancy divided by its degrees of freedom, which should be nonsignificant; RMSEA = root mean square error of approximation, a measure of fit that takes into account the population moments rather than sample moments; CFI = comparative fit index; AIC = Akaike information criterion, which should be as low as possible. χ2/df below 2, RMSEA value below 0.08 and CFI higher than 0.90 reflect acceptable fit of the model [41]. The comparably low Akaike information criterion attests to the parsimonious informative modeling in the hypothesized mediation model.
3.3.1. Test of direct paths
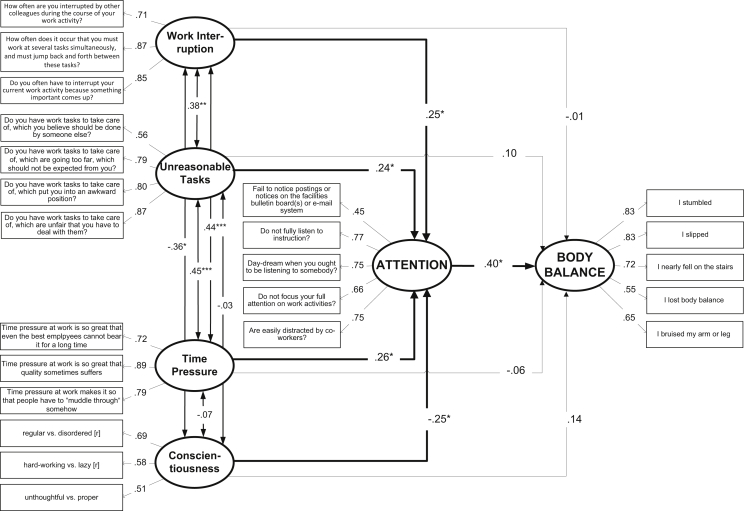
Fig. 1 shows the standardized path coefficients of the hypothesized mediation model. All direct paths to attentional cognitive failures and from attentional cognitive failures to STFs were significant. Direct paths from interruptions, unreasonable tasks, time pressure, and conscientiousness to STFs were not significant.
Fig. 1.
Model of attentional cognitive failure as mediator of the effects of work interruptions, unreasonable tasks, time pressure, and conscientiousness on STFs. *p < 0.05, **p < 0.01, ***p < 0.001, one-tailed.
STFs, slips, trips, and falls.
3.3.2. Test of indirect paths
The test of indirect (i.e., mediation) effects using the bootstrapping approach resulted in a significant indirect effect for work interruptions → attentional cognitive failures → STFs path [β = 0.094, 90% confidence interval (CI) = 0.004–0.222]. The test of the second mediation path resulted in a significant indirect effect for the unreasonable tasks → attentional cognitive failures → STFs path (β = 0.095, 90% CI = 0.010–0.215). The test of the third mediation path resulted in a significant indirect effect for the time pressure → attentional cognitive failures → STFs path (β = .093, 90% CI = 0.008–0.229). The fourth indirect conscientiousness → attentional cognitive failures → STFs path was also statistically relevant (β = −0.098, 90% CI = −0.243 to −0.005).
3.3.3. Alternative model testing
The hypothesized model of mediation represented the empirical data well; however, alternative models might be equally good or even better. Hence, a hypothesized model should be compared to a plausible alternative model. A plausible alternative model is the person-oriented “accident-prone person” model that postulates that individuals high in attentional cognitive failures increase their mental load at work by themselves, for example, by paying attention to electronic messages during work, which causes interruptions and delays and generates time pressure that would have otherwise been preventable. Hence, workload then might mediate the effects of attentional cognitive failures on STFs. The alternative “accident-prone person” model was also acceptable in fit, although it was significantly worse in fit than the hypothesized mediation model [Δ χ2 (1) = 5.91, p = 0.015]. Moreover, direct paths from work stressors to STFs were not significant, so tests of mediation were obsolete (β work interruptions > STFs = 0.08, p = 0.290; β unreasonable tasks > STFs = 0.21, p = 0.110; β time pressure > STFs = 0.06, p = 0.656).
4. Discussion
Craven et al provided a conceptual framework of types of safety concerns in home care [6]. In their framework, spatial concerns at the private residences of patients share an intersection with temporal, interpersonal, and physical safety concerns. Working alone in a rather uncontrolled workplace, spatial concerns often cause temporal concerns (e.g., spending a lot of time to reach a bathroom on a different floor), physical concerns (e.g., having to take poor posture combinations because of spatial limitations [4]), and interpersonal concerns (e.g., being interrupted by comments and demands of other family members [45]). Therefore, spatial concerns often cannot be addressed sufficiently, and as Craven et al pointed out, spatial safety concerns may serve as a potential source of stress for home care nurses who have to accept some risks, even though they are potentially avoidable [6]. Spatial safety concerns contribute to poor posture during work of home care nurses [4]. In addition, spatial concerns are likely to have played a causing or aggravating role in quality-threatening time pressure, interruptions, and unreasonable tasks that appeared to be safety concerns in the present study. The present study also pointed to another process, addressing the issue of attention during task execution: quality-threatening time pressure, interruptions, and unreasonable tasks all have the potential to distract from the task at hand. It is noteworthy that a mediation model with attentional cognitive failure as a mediator was confirmed when individual differences in conscientiousness were controlled. Quality-threatening time pressure, interruptions, and unreasonable tasks were relevant beyond stable individual differences of home care nurses in attentional cognitive failure. Broadbent et al viewed attentional cognitive failure as a more stable failure of executive control [42]. Following Broadbent, we expect conscientiousness to predict attentional cognitive failure and attentional cognitive failure to predict STF [42]. That mediation was significant in the present study, confirming that stable individual differences in attention regulation are relevant. However, an alternative model that focused on individual differences in attentional cognitive failure as a major source of higher time pressure, interruptions, and unreasonable tasks was not empirically supported. Therefore, time pressure, interruptions, and unreasonable tasks should be targeted in prevention of STF. So far, in Switzerland, like in Canada, the focus of prevention in home care is primarily on spatial and physical safety concerns [6]. Indeed, work redesign should address buckled carpets, unclean or wet surfaces, change in elevation, insufficient light, and use of appropriate lifting aids [1]. However, the current findings also showed that task-related stressors, such as time pressure, interruptions, and unreasonable tasks, should be reduced to prevent STF in home care nurses. From research on the intentions of home care nurses regarding whether to stay in their profession for the next 5 years, we can see that that nurses who perceive their work to be of high quality are more likely to intend to remain employed [46]. It appears that quality-threatening time pressure, interruptions, and unreasonable tasks are a threat both to employment and safety. The common link is the stress process and attentional cognitive failure as a (cognitive) part of a stress response. Home care organizations should engage home care nurses in the development and evaluation of strategies that improve care quality [46]. Thus, organizations who facilitate the meeting of quality goals contribute to occupational health not only by increasing occupational well-being and recovery after work [47] but also by reducing the risk of STFs [48]. An intervention study that included a team-based health and safety intervention in home care workers showed a significant decrease in negative affectivity and an increase in safety behaviors, such as corrected home hazards and communication of hazards [48].
4.1. Limitations and strengths
The hypothesized mediation model fits the empirical data well. However, this does not confirm causal mediation. The hypothesized mediation model proved to be the more plausible model because the alternative model failed to fit the empirical data. Thus, the alternative trait-based “accident-prone person” model, which only centered on individual differences in attentional cognitive failures in accounting for individual differences in work stressors and STFs, did not receive empirical support.
An important limitation arises from the cross-sectional nature of the data. Preferably, our model would have been tested longitudinally using a prospective falls calendar [49]. Therefore, our study requires replication, as longitudinal event-sampling studies are better-equipped to study the processes involved, including methods like ambulatory assessment [50] and daily reports [51]. Experimental simulation approaches are also promising [52].
A second limitation is that bias from common-source variance may have boosted the correlations in this study. Employees who perceive a high level of cognitive failure might also perceive more near-falls [20]. Further studies should also use methods other than self-reporting, by including, for example, the reports of significant others living at the same place and measuring postural sway with force plates [53] or standardized balance tests [54].
5. Conclusions
In addition to spatial safety concerns, quality-threatening time pressure, interruptions, and unreasonable tasks pose demands on home care nurses that may exceed their physical and cognitive capabilities and make STF more likely. Training nurses, managers, and clients on how to reduce interruptions, quality-threatening time pressures, and unreasonable tasks should be included in broad-scale prevention programs that are shown to be effective in the prevention of STFs in home care nurses [48].
Conflict of interest
The authors declare that they have no conflict of interest.
References
- 1.Eidgenössische Koordinationskommission für Arbeitssicherheit . [Safety and health prevention in home health care]. EKAS; Luzern, Switzerland: 2016. Arbeitssicherheit und Gesundheitsschutz in der Hilfe und Pflege zu Hause (Spitex) p. 132.http://www.ekas.admin.ch/redirect.php?cat=f%2BR3rLeQL4g%3D&id=675 Available from: [Google Scholar]
- 2.Phillips J.P. Workplace violence against health care workers in the United States. N Engl J Med. 2016;374:1661–1669. doi: 10.1056/NEJMra1501998. [DOI] [PubMed] [Google Scholar]
- 3.Hignett S., Otter M.E., Keen C. Safety risks associated with physical interactions between patients and caregivers during treatment and care delivery in Home Care settings: A systematic review. Int J Nurs Stud. 2016;59:1–14. doi: 10.1016/j.ijnurstu.2016.02.011. [DOI] [PubMed] [Google Scholar]
- 4.European Agency for Occupational Safety & Heath at Work . Publications Office of the European Union; Luxembourg: 2014. Current and emerging issues in the healthcare sector, including home and community care; p. 148. [Google Scholar]
- 5.Büssing A., Höge T., Glaser J., Heinz E. vol. 63. [Analysis of mental and physical work load in outpatient nursing. Method development and results from organization screening and task analyses]. Berichte aus dem Lehrstuhl für Psychologie der Technischen Universität München, Bericht; München: 2002. p. 70. (Erfassen psychischer und physischer Belastungen in der ambulanten Pflege. Entwicklung und Validierung eines Belastungsscreening). [Google Scholar]
- 6.Craven C., Byrne K., Sims-Gould J., Martin-Matthews A. Types and patterns of safety concerns in home care: staff perspectives. Int J Qual Health Care. 2012;24:525–531. doi: 10.1093/intqhc/mzs047. [DOI] [PubMed] [Google Scholar]
- 7.Elfering A., Grebner S. Stress and patient safety. In: Halbesleben J.R.B., editor. The handbook of stress and burnout in health care. Nova Science Publishers; Hauppauge, NY: 2008. pp. 173–186. [Google Scholar]
- 8.Pereira D., Müller P., Elfering A. Interruptions, social stressors from supervisor(s) and attention failure in surgery personnel. Ind Health. 2015;53:427–433. doi: 10.2486/indhealth.2013-0219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wallace J.C., Chen G. Development and validation of a work-specific measure of cognitive failure: Implications for occupational safety. J Occup Organ Psychol. 2005;78:615–632. [Google Scholar]
- 10.Cham R., Redfern M.S. Changes in gait when anticipating slippery floors. Gait & Posture. 2002;15:159–171. doi: 10.1016/s0966-6362(01)00150-3. [DOI] [PubMed] [Google Scholar]
- 11.Di Domenico A., Mc Gorry R.W., Chang C.-C. Association of subjective ratings of slipperiness to heel displacement following contact with the floor. Appl Erg. 2007;38:533–539. doi: 10.1016/j.apergo.2006.09.001. [DOI] [PubMed] [Google Scholar]
- 12.Chander H., Garner J.C., Wade C. Heel contact dynamics in alternative footwear during slip events. Int J Ind Erg. 2015;48:158–166. [Google Scholar]
- 13.Chander H., Wade C., Garner J.C., Knight A.C. Slip initiation in alternative and slip-resistant footwear. Int J Occup Safe Erg. 2017;23:558–569. doi: 10.1080/10803548.2016.1262498. [DOI] [PubMed] [Google Scholar]
- 14.Coco M., Fiore A.S., Perciavalle V., Maci T., Petralia M.C., Perciavalle V. Stress exposure and postural control in young females. Mol Med Rep. 2015;11:2135–2140. doi: 10.3892/mmr.2014.2898. [DOI] [PubMed] [Google Scholar]
- 15.Kerr B., Condon S.M., McDonald L.A. Cognitive spatial processing and the regulation of posture. J Exp Psychol. 1985;11:617–622. doi: 10.1037//0096-1523.11.5.617. [DOI] [PubMed] [Google Scholar]
- 16.Day A., Brasher K., Bridger R.S. Accident proneness revisited: The role of psychological stress and cognitive failure. Acc Anal Prev. 2012;49:532–535. doi: 10.1016/j.aap.2012.03.028. [DOI] [PubMed] [Google Scholar]
- 17.Weigl M., Müller A., Zupanc A., Glaser J., Angerer P. Hospital doctors' interruptions and activities: An observation study. BMJ Qual Safety. 2011;20:491–497. doi: 10.1136/bmjqs.2010.043281. [DOI] [PubMed] [Google Scholar]
- 18.Grundgeiger T., Sanderson P. Interruptions in healthcare: Theoretical views. Int J Med Inf. 2009;78:293–307. doi: 10.1016/j.ijmedinf.2008.10.001. [DOI] [PubMed] [Google Scholar]
- 19.Rivera-Rodriguez A.J., Karsh B.T. Interruptions and distractions in healthcare: Review and reappraisal. BMJ Qual Safe Health Care. 2010;19:304–312. doi: 10.1136/qshc.2009.033282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Semmer N., Grebner S., Elfering A. Psychische Kosten von Arbeit: Beanspruchung und Erholung, Leistung und Gesundheit. In: Kleinbeck U., Schmidt K.-H., editors. Arbeitspsychologie. [Psychological costs of work: workload, recovery, performance, and health]. Hogrefe; Göttingen: 2010. pp. 325–370. [Google Scholar]
- 21.Elfering A., Grebner S., Ebener C. Interruptions, cognitive failure and near-accidents in health care. Psychol Health Med. 2015;20:139–147. doi: 10.1080/13548506.2014.913796. [DOI] [PubMed] [Google Scholar]
- 22.Tams S., Thatcher J., Grover V., Pak R. Selective attention as a protagonist in contemporary workplace stress: implications for the interruption age. Anxiety Stress Coping. 2015;28:663–686. doi: 10.1080/10615806.2015.1011141. [DOI] [PubMed] [Google Scholar]
- 23.Semmer N.K., Jacobshagen N., Meier L.L., Elfering A. Occupational stress research: the “stress-as-offence-to-self” perspective. In: Houdmont J., McIntyre S., editors. Occupational health psychology: European perspectives on research, education and practice. ISMAI Publishers; Maia, Portugal: 2007. pp. 43–60. [Google Scholar]
- 24.Semmer N.K., Jacobshagen N., Meier L., Elfering A., Beehr T., Kaelin W., Tschan F. Illegitimate tasks as a source of work stress. Work Stress. 2015;29:32–56. doi: 10.1080/02678373.2014.1003996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Semmer N.K., Jacobshagen N. Selbstwert und Wertschätzung als Themen der arbeitspsychologischen Stressforschung. In: Hamborg K.C., Holling H., editors. Innovative Personal- und Organisationsentwicklung. [Self-esteem and appreciation as topics in organizational stress research]. Hogrefe; Göttingen: 2003. pp. 131–155. [Google Scholar]
- 26.Sabo K. Protecting the professional role. A study to review non-nursing activities and recommendations for change. Can J Nurs Admin. 1990;3:15–18. [PubMed] [Google Scholar]
- 27.Björk L., Bejerot E., Jacobshagen N., Härenstam A. I shouldn't have to do this: Illegitimate tasks as a stressor in relation to organizational control and resource deficits. Work Stress. 2013;27:262–277. [Google Scholar]
- 28.Zohar D. Safety climate: Conceptual and measurement issues. In: Quick J.C., Tetrick L.E., editors. Handbook of occupational health psychology. American Psychological Association; Washington, DC: 2003. pp. 123–142. [Google Scholar]
- 29.Zohar D. Work safety. In: Spielberger C., editor. Enzyclopedia of applied psychology. Elsevier; New York: 2004. pp. 719–724. [Google Scholar]
- 30.Hockey G.R.J. Cognitive-energetical control mechanisms in the management of work demands and psychological health. In: Baddeley A.D., Weiskrantz L., editors. Attention, selection, awareness and control: a tribute to Donald Broadbent. Oxford University Press; Oxford, UK: 1993. pp. 328–508. [Google Scholar]
- 31.Kälin W., Semmer N.K., Elfering A. Die Folgen von Zeitdruck und der Qualitätsbeeinträchtigung durch Zeitdruck auf das Befinden Schweizer Berufsanfänger. In: Lösel F., Bender D., editors. 45. Kongress der Deutschen Gesellschaft für Psychologie. Humane Zukunft gestalten. [Consequences of time pressure and quality threatening time pressure on well-being of Swiss job beginners]. Pabst; Lengerich, Germany: 2006. p. 163. [Google Scholar]
- 32.Semmer N.K., Kälin W., Elfering A. When time pressure really hurts: The case of performance impairment. In: Gil-Monte P., Houdmont J., Hassard J., editors. 8th conference of the European Academy of Occupational Health Psychology: Book of proceedings. University of Valencia, Spain: EAOHP; 2008. p. 137.http://www.eaohp.org/uploads/1/1/0/2/11022736/bop8.pdf Available from: [Google Scholar]
- 33.Lüdtke O., Robitzsch A., Trautwein U., Köller O. Umgang mit fehlenden Werten in der psychologischen Forschung - Probleme und Lösungen. Handling of missing data in psychological research: problems and solutionsPsychol Rund. 2007;58:103–117. [Google Scholar]
- 34.Semmer N., Zapf D., Dunckel H. Assessing stress at work: a framework and an instrument. In: Svane O., Johansen C., editors. Work and health: scientific basis of progress in the working environment. Office for Official Publications of the European Communities; Luxembourg: 1995. pp. 105–113. [Google Scholar]
- 35.Hächler P., Pereira D., Elfering A. Recovery experiences during vacation and their relation to job stressors and health. Psychol Writ. 2017;10:13–30. [Google Scholar]
- 36.Costa P.T., Jr., McCrae R.R. Psychological Assessment Resources; Odessa: 1985. The NEO Personality Inventory manual; p. 44. [Google Scholar]
- 37.Ostendorf F., Angleitner A. On the generality and comprehensiveness of the Five-Factor model of personality. Evidence for five robust factors in questionnaire data. In: Caprara G.V., van Heck G.L., editors. Modern personality psychology: critical reviews and new directions. Harvester Wheatsheaf; New York: 1992. pp. 73–109. [Google Scholar]
- 38.Schallberger U., Venetz M. [Brief versions of Ostendorf’s MRS inventory for the assessment of the Big-Five personality factors]. Universität Zürich: Berichte aus der Abteilung Angewandte Psychologie; 1999. Kurzversionen des MRS-Inventars von Ostendorf (1990) zur Erfassung der fünf “grossen” Persönlichkeitsfaktoren; pp. 1–51. [Google Scholar]
- 39.Elfering A., Grebner S., Dudan A. Job characteristics in nursing and work specific cognitive failure. SHAW (Saf Health Work) 2011;2:1–7. doi: 10.5491/SHAW.2011.2.2.194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Elfering A., Grebner S., Boillat C. Busy at work and absent-minded at home: Mental work load, cognitive failure and domestic falls. Swiss J Psychol. 2013;72:219–228. [Google Scholar]
- 41.Schermelleh-Engel K., Moosbrugger H., Müller H. Evaluating the fit of structural equation models: test of significance and descriptive goodness-of-fit measures. Meth Psychol Res Online. 2003;8:23–74. [Google Scholar]
- 42.Broadbent D.E., Cooper P.F., Fitzgerald P., Parkes K.R. The Cognitive Failures Questionnaire (CFQ) and its correlates. Brit J Clin Psychol. 1982;21:1–16. doi: 10.1111/j.2044-8260.1982.tb01421.x. [DOI] [PubMed] [Google Scholar]
- 43.Cho H.C., Abe S. Is two-tailed testing for directional research hypotheses tests legitimate? J Bus Res. 2013;66:1261–1266. [Google Scholar]
- 44.Ludbrook J. Should we use one-sided or two-sided P values in tests of significance? Clin Exp Pharmacol Physiol. 2013;40:357–361. doi: 10.1111/1440-1681.12086. [DOI] [PubMed] [Google Scholar]
- 45.Beer J.M., McBride S.E., Mitzner T.L., Rogers W.A. Understanding challenges in the front lines of home health care: A human-systems approach. Appl Ergon. 2014;45:1687–1699. doi: 10.1016/j.apergo.2014.05.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Tourangeau A.E., Patterson E., Saari M., Thomson H., Cranley L. Work-related factors influencing home care nurse intent to remain employed. Health Care Manage Rev. 2017;42:87–97. doi: 10.1097/HMR.0000000000000093. [DOI] [PubMed] [Google Scholar]
- 47.Pereira D., Semmer N.K., Elfering A. Illegitimate tasks and sleep quality: an ambulatory study. Stress Health. 2014;30:209–221. doi: 10.1002/smi.2599. [DOI] [PubMed] [Google Scholar]
- 48.Olson R., Thompson S.V., Elliot D.L., Hess J.A., Rhoten K.L., Parker K.N., Wright R.R., Wipfli B., Bettencourt K.M., Buckmaster A., Marino M. Safety and health support for home care workers: The COMPASS Randomized Controlled Trial. Am J Pub Health. 2016;106:1823–1832. doi: 10.2105/AJPH.2016.303327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Mackenzie L., Byles J., D’Este C. Research: longitudinal study of the home falls and accidents screening tool in identifying older people at increased risk of falls. Austral J Ageing. 2009;28:64–69. doi: 10.1111/j.1741-6612.2009.00361.x. [DOI] [PubMed] [Google Scholar]
- 50.Klumb P., Elfering A., Herre C. Ambulatory assessment in I/O Psychology: Fruitful examples and methodological issues. Eur Psychol. 2009;14:120–131. [Google Scholar]
- 51.Heijnen M.J.H., Rietdyk S. Falls in young adults: Perceived causes and environmental factors assessed with a daily online survey. Hum Move Sci. 2016;46:86–95. doi: 10.1016/j.humov.2015.12.007. [DOI] [PubMed] [Google Scholar]
- 52.Jones J., Wilkins M., Caird J., Kaba A., Cheng A., Ma I.W.Y. An experimental study on the impact of clinical interruptions on simulated trainee performances of central venous catheterization. Ad Simul. 2017;2:5. doi: 10.1186/s41077-017-0038-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Elfering A., Schade V., Stöcklin L., Baur S., Burger C., Radlinger L. Stochastic resonance whole-body vibration improves postural control in health-care professionals: A worksite randomised controlled trial. Workplace Health Safe. 2014;64:187–196. doi: 10.1177/216507991406200503. [DOI] [PubMed] [Google Scholar]
- 54.Elfering A., Arnold S., Schade V., Burger C., Radlinger L. Stochastic resonance whole-body vibration, musculoskeletal symptoms and body balance: A worksite training study. SHAW. 2013;4:149–155. doi: 10.1016/j.shaw.2013.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]