Abstract
Osteoarticular tuberculosis (OATB) is a secondary chronic infection with paubacillary bacillus Koch (BK) that has bone and joint interest. Today in Romania, tuberculosis is a primary public health problem, according to World Health Organization (WHO) in 2015 alone, there have been 10.4 million new cases of tuberculosis (TB) in the world, of which 15.195 in Romania. Pulmonary and extrapulmonary tuberculosis, especially the osteoarticular form, with multiple outbreaks should of had a minimal impact, but because of the multiple characteristics such as: epidemiological, geographic, associated diseases, diagnosis capacity, therapeutic options, gene pool and racial evolutiv traits, the disease spreading and management in both developed and underdeveloped countries, the TB infection has seen an increase in the number of cases (e.g. Africa and Asia). Today there is a fecundity upsurge of BK infection, especially pronounced in low income populations, country side people being the most affected. There are multiple breakthroughs in the understanding of Mycobacterium tuberculosis physiopathology. This fact offers us a modern and genetically guided approach in the diagnosis, evolutive patterns and treatment involving the OATB.
Keywords: osteoarticular tuberculosis, epidemiology, genetics
History
The spinal form of the TB has been known for over 3400 years, being discovered in some Egyptians mummies [1,2,3]. Hippocrates himself has described the relationship between the gibbus deformity and the slow progressive deposits that burst in the axillary and lumbar regions, even though they were incurable and difficult to understand at times.
Percival Pott was the first person to present the classic description of spinal tuberculosis (TB) in 1779; hence, spinal TB was called ‘Pott’s Disease [4,5,6]. Friedlandl and Koster discovers in 1869 the tuberculosis follicle, which bares their names followed by Robert Koch’s breakthrough of discovering and describing the tuberculosis bacilli.
Thilesen and Hennies shed the light on pubic symphysis tuberculosis, as a rare form of OAT, during the period of 1855-1888 allowing Sorell and Déjerine to describe in the year 1932 in depth the OATB form and pathology, and focus yet again on the rare symphysis tuberculosis [7,8,9,10,11,12,13,14].
Introduction
OAT has its place among the most frequent forms of extrapulmonary tuberculosis, having at this time a surge in frequency. Today it represents 10% of the sum total of extrapulmonary forms, right after peripheral lymphatic nodes manifestation (50.3%), pleural manifestations (24.4%), peritoneum manifestations, pericardium manifestations (8.2%) and genitourinary system manifestations (4%) [15,16].
The African region has the highest tuberculosis rate, 281/100.000 cases, females being more affected than males (1.58%). The average age of infection is at about 45 years, give or take 18 years [17].
The average time-lapse from contracting the disease to a positive diagnostic is around 13.5 months (between 1 to 36 months), 60% of the patients accusing prior TB contact while 30% have had a former TB infection in the past, rest of them with no contact in the past [18].
Despite the progress that has been done during the last decade, tuberculosis is still a worldwide health issue, globally causing the most deaths among the infectious diseases. In 2015, there were an estimated 10.4 million new (incident) TB cases worldwide, of which 5.9 million (56%) were men, 3.5 million (34%) women and 1.0 million (10%) children [19]. Romania having its share, 15.195 of both pulmonary and extrapulmonary tuberculosis cases [19].
Until now the screening and treatment programs initiated prior to 1990 were supposed to render tuberculosis into an extremely rare disease in Romania, but the reality failed to meet the expectations. About 10% of total extrapulmonary tuberculosis cases have an osteoarticular location, the vertebral forms being a majority [19]. It can affect all the joints, but the most frequent locations after the vertebral are: hip, knee, ankle, feet, fists and shoulder. The pubic symphysis tuberculosis is a rare and uncharacteristic. In the last 30 years only 9 cases were reported [7].
The particularity of OAT is the fact that it has multiple infection focuses, in 16% of the cases having 2 infectious focuses, 4% having 3, 1% having 4 and 0.25% having 5 infectious sites.
What is the meaning of multiple infectious sites in OAT? Due to a drop in immunity or a hematologic/lymphatic propagation a reactivation of the latent focuses within the primary infection complex areas occurs, followed by the awakening of the Mycobacterium tuberculosis from the pulmonary and extrapulmonary sites [18,20].
The process of diagnosis can sometimes give rise to major errors and late diagnosis due to the blending of the typical and atypical clinical forms.
The disease is rare, with unspecific symptomatology which makes it hard to differentiate it from other multiple bone lesions (blood disease and metastases) [21].
The diagnosis is done by an elimination process of other high presumption pathologies, associated with an confirmed progressive tuberculosis site. It is mandatory to confirm the diagnostic by biological, radiological, CAT, MRI, scintigraphy, histological, bacteriologic profile and antibiogram criteria as shown in Table 1 [21,22].
Table 1.
Diagnostic criteria and elements
| Diagnostic criteria | Diagnostic elements |
| Clinical symptomatology | Vesperal fever, physical, psychological and sexual weakness up to adynamism, severe weight loss and tuberculosis facies. In some cases of spinal OAT osifluent abscess can be present [13,18].(Fig. 1a,b) |
| Biological trials | Increased HSS, PCR’s value well over 20-25, on the blood count you can see a lymphocytosis and moderate leukocytosis, tuberculin IDR positive with Palmer 4 type, the inactivation of which, has a weak diagnosis value and simple positive IDR lays as a witness for a recent TB contact [13,18,20]. |
| Standard radiological examination | Destruction (osteolysis, eroded aspect, transparent bone contours and geodes) also known as Phemister triad (Fig. 1c,d) |
| Bone reconstruction (bone condensation and osteitis) [9]. | |
| Bone fusion alongside the bone edge, sclerosis, fact which suggests a late and impairing phase [21]. | |
| Echographic examination | N/A |
| Computerized Axial Tomography (CAT) | N/A |
| Magnetic Resonance Imaging (MRI) | Bone edema, synovial reaction (synovitis), abscesses, often needing a full rachis investigation [21,23,24].(Fig. 1e,f) |
| Scintigraphic examination | Uneven bone hyperfluorescence (Fig. 1g) |
| Bacteriological profile and antibiogram | Done on the puss and fluid harvested through a fine needle aspiration (FNA) [22]. |
| Histopathological exam | On the core needle biopsy (CNB) or surgical biopsy [22]. |
Particularities
In the OAT diagnostic process there are few characteristics that depend on epidemiology, immune situation, treatment, patient evolution and genetic studies.
Epidemiology-young age, the children being the most vulnerable age group.
Frail immunity or the presence of antibiotic resistance germs which implies a certain degree of immunodepression.
Therapeutic particular features: the disease has a longer plateau stage.
Evolutive variations determine either a possible exitus during treatment or a favorable evolution which has the following criteria shown in Table 2.
Table 2.
Criteria of favorable treatment outcome
| Weight gain with an overall general improvement of the patient status |
| A decrease in the bone and joint pain |
| Inflammatory syndrome absence |
| On the radiological, MRI and echographic examination abscess should be absent |
| The existence of a rebound, which implies the patient’s observation over a minimum of 2 years (the average rebound has a time frame of 5 years-between 2 and 23 years). |
Figure 1.
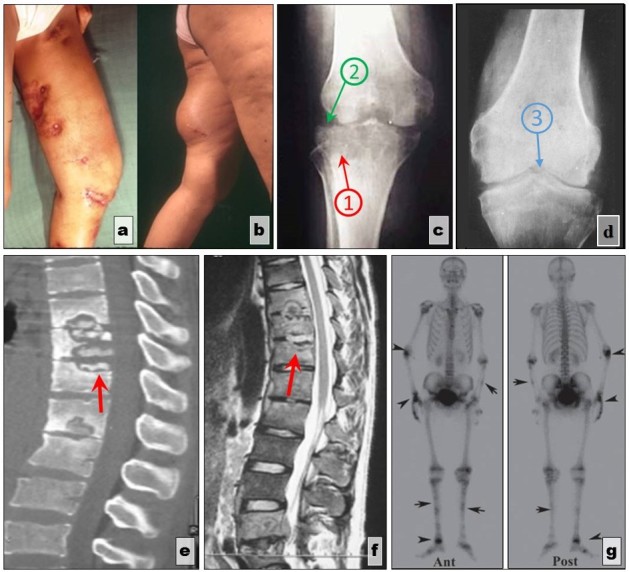
Features of clinical and imagistic diagnosis. (a, b) Ossifluent hip abscess: a-posterior view; b-anterior view; Phemister triad: (c) X-ray anteroposterior view of the knee joint: 1-Juxta-articular osteopaenia/osteoporosis (red arrow). 2-Peripheral osseous erosions (green arrow) (d) 3-Gradual narrowing of joint space (blue arrow); (e, f) Mirror like vertebral erosions-MRI sagital views; Scintigraphic examination. (g) Scintigraphic aspects of OATB-anteroposterior view (left) and posteroanterior view (right) [Collection of the Department of Orthopedics]
Genetic studies give us a better understanding of the immune answer physiopathology in response to KB infection.
Soon after the areal infection with Mycobacterium tuberculosis (MT) in the joints and vertebrae there is a release of proinflammatory cytokines (IL-1, IL-6) and Inflammatory chimiokines MCP1, MIP, RANTES, thus increasing macrophage numbers and activating them. The granulome, which appears next acts as a buffer controlling the infection and blocking its spreading further into the organism [25]. When the infection control is absent the inflammation spreads, causing tissue damage which exhibits joint and bone effects: bone resorption due to the activation of the osteoclasts. Normally the infected subject spreads the disease through aerial dissemination, exposing others to the bacteria and spreading it. 90% of the people have a suppressed infection and 10% (depending on the level of the immune suppression or a former infection with herpetic virus, HIV and germ concentration in the body overlaid with the genetic predisposition) manifest the disease over their lifetime [26].
The involvement of these genetic factors is shown through countless epidemiological findings-there is a difference in susceptibility depending on the race and ethnic factors:
- The Lubeck experiment (Germany);
- Studies performed on monozygotic twins show that there are genetic variations in the levels of Han-362G /C protein in Chinese population [27,28] (Fig. 2).
Figure 2.
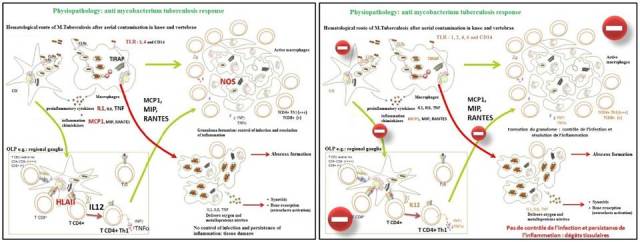
Inflammatory response to tuberculosis bacillus(left) and the absence of the inflammatory respons (right) [modified after Mecabih, 2016 [29]]
This experiment actually describes the association of some functional polymorphisms related to resistance and susceptibility to tuberculosis. There are, in fact, patients which have a confirmed diagnosis of bone or joint TB and yet show no signs of pulmonary manifestations.
Those who possess the TLR4-6143A, GRS1927914 gene have an excessive inflammatory reaction with a high degree of cell recruitment, cells which are responsible for inflammation: monocytes, dendritic cells, type T lymphocytes which possess metalloprotein based enzymes that act as chemical mediators [30].
The most important characteristics are as follows:
- Certain genes ar associated with OAT: second class HLA, TLR4;
- Other genes are associated with particular forms of OAT: MC1 is correlated with the axillar form meanwhile MOS2 is relates with the peripheral form;
- Class 2 HLA alleles give a predisposition to a clinical manifestation of OAT. Overall there is a need for deeper research of the correlated genetic factors so that we can obtain a better understanding of the disease physiopathology and treatment strategies [25,26].
Treatment
The National Program for Control, Survival and Prevention of TBC (NPCSP) through the Unit for Technical Assistance and Management of TBC (UTAM) has the following recommendations for both the newly diagnosed and severe forms of OAT with confirmed Mycobacterium:
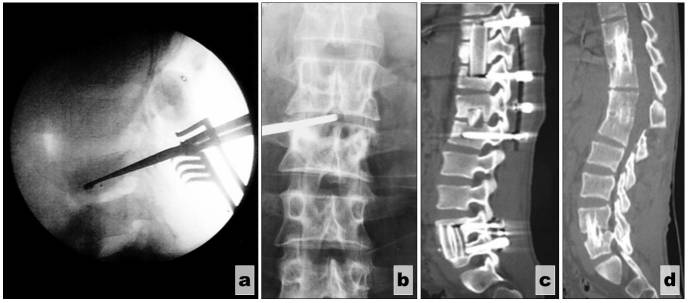
- Diagnose purposed biopsy regardless of the abscesses drainage (Fig. 3a,b);- Rhachis compression reduction and stability increase for the spine located infection [31];
Figure 3.
(a) Surgical biopsy of the spine. Sagital view. (b) Punctual biopsy under radiographic guidance. Anteroposterior view. [Collection of the Department of Orthopedics] (c)MRI aspect of multifocal metallic stability implant after vertebral curettage and segmental stabilization system with somatic graft. (d) Consolidate bone aspect after osteosynthesis material removal (right) [Abdelkefi, 2016 [33]]
- Immobilization with plaster casts (due to the fact that segment stability cannot always be obtained by using transpedicular screws) [32] (see Fig. 3c,d);
- Drug treatment: Hydrazide-300 mg/day (5-10mg/day), Rifampicin-600mg/day (10mg/kg/day), Ethambutol-1g/day (15mg/day), Pyrazinamide-1,5g/day (25-30mg/kg/day), under Strictly Surveyed Treatment (SST) associated with C, D and B vitamins group over a period of 6 months. If during the last 3 months the results are positive the 3 drugs based therapy can be introduced in SST, also associated with C, D and B vitamins group. If segment stability cannot be obtained through osteosynthesis with transpedicular screws, but the plaster cast was well tolerated by the patient for a minimal period of 60-75 days, then you can associate Bisphosphonates in order to prevent fractures with a single dose/month (Zolendronic acid) [9].
Conclusions
AOT is the most frequent forms of extrapulmonary tuberculosis, representing 10% of the total extrapulmonary tuberculosis cases.
The highest frequency locations in OAT are: thoracic and upper lumbar spine, pelvic girdle with a preference for the sacroiliac joints, meanwhile the ilium and ischial bone alone have a lower infection rate, followed by the greater trohanter, knees, foot, fist, elbow and shoulder. In theory the OAT can be found in every bone in the body (the clavicle has often been quoted in scientific literature) [21].
The possibility of different interpretation of the clinical signs renders the diagnosis as a difficult feat. The lack of genitourinary symptomatology increases the difficulty even further, making it so that it can be easily mistaken with: unspecific osteitis, blood diseases and bone metastasise [7,34,35].
Even today the therapeutic trials can be admitted as a positive diagnostic tool, especially in hard to reach places for biopsy, even for core needle biopsy (CNB) but also in the event of a blind biopsy, according to The National Program for Control, Survival and Prevention of TBC, but partially accepted by The Unit for Technical Assistance and Management of TBC.
OAT is influenced by class 2 HLA alleles, TLR4 and IL-1. Alleles that are associated with the axillary form are MCP-1 and those which are associated with the peripheral form are MOS-2.
NPCSP and UTAM claims that an early diagnosis and a rigorous treatment can prevent the disease dissemination and the development of severe forms that can evolve even with death at the cost of colossal human financial and social resources.
It is mandatory to perform a deeper research of the genetic factors involved in order to achieve a better understanding of the disease physiopathology and treatment strategies.
Genetic engineering can prevent the infection with Mycobacterium tuberculosis to occur given the fact that certain genes have the ability to influence the susceptibility to KB.
References
- 1.Garg RK, Somvanshi DS. Spinal tuberculosis: a review. J Spinal Cord Med. 2011;34(5):440–454. doi: 10.1179/2045772311Y.0000000023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Watts HG, Lifeso RM. Current Concepts Review: Tuberculosis of Bones and Joints. The Journal of Bone and Joint Surgery. 1996;78(2):288–298. doi: 10.2106/00004623-199602000-00019. [DOI] [PubMed] [Google Scholar]
- 3.Martini M. La tuberculose ostéoarticulaire. In: Martini M, editor. Berlin: Heidelberg: Springer-Verla; 1988. [Google Scholar]
- 4.Ansari S, Amanullah F, Ahmad K, Rauniyar RK. Pott’s Spine: Diagnostic Imaging Modalities and Technology Advancements. N Am J Med Sci. 2013;5(7):404–411. doi: 10.4103/1947-2714.115775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Padyana M, Bhat RV, Dinesha M, Nawaz A. HIV Tuberculosis: A Study of Chest X Ray Patterns in Relation to CD4 Count. N Am J Med Sci. 2012;4(5):221–225. doi: 10.4103/1947-2714.95904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Moore SL, Rafi M. Imaging of musculoskeletal and spinal tuberculosis. Radiol Clin North Am. 2001;39(2):329–442. doi: 10.1016/s0033-8389(05)70280-3. [DOI] [PubMed] [Google Scholar]
- 7.Bali K, Kumar V, Patel S, Mootha AK. Tuberculosis of symphysis pubis in a 17 year old male: A rare case presentation and review of literature. J Orthop Surg Res. 2010;27(5):63–63. doi: 10.1186/1749-799X-5-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fares G, Pagani A. Tubercular osteitis of the pubis [Article in Italian] Minerva Ortop. 1966;17(8):459–469. [PubMed] [Google Scholar]
- 9.Ker NB. Tuberculosis of the pubic symphysis. J R Soc Med. 1986;79(7):429–300. doi: 10.1177/014107688607900716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rozadilla A, Nolla JM, Rodriguez J, Del Blanco J, Roig ED. Tuberculosis of the pubis symphysis. J Rheumatol. 1991;18(8):1271–1272–1271–1272. [PubMed] [Google Scholar]
- 11.Tsay MH, Chen MC, Jaung GY, Pang KK, Chen BF. Atypical skeletal tuberculosis mimicking tumor metastases: report of a case. J Formos Med Assoc. 1995;94(7):428–431. [PubMed] [Google Scholar]
- 12.Benbouazza K, Allali F, Bezza A, el Hassani S, el Maghraoui A, Lazrak N, Hassouni F, Hajjaj Hassouni. Pubic tuberculous osteo-arthritis. Apropos of 2 cases. Rev Chir Orthop Reparatrice Appar Mot. 1997;83(7):670–672. [PubMed] [Google Scholar]
- 13.Bayrakci K, Daglar B, Tasbas BA, Agar M, Gunel U. Tuberculosis osteomyelitis of symphysis pubis. Orthopedics. 2006;29(10):948–950. doi: 10.3928/01477447-20061001-15. [DOI] [PubMed] [Google Scholar]
- 14.Herzog H. History of tuberculosis. . Respiration. 1998;65(1):5–15. doi: 10.1159/000029220. [DOI] [PubMed] [Google Scholar]
- 15.Marjorie PG, Holenarasipur R. Extrapulmonary Tuberculosis: An Overview. Am Fam Physician. 2005;72(9):1761–1768. [PubMed] [Google Scholar]
- 16.Kulchavenya E. Extrapulmonary tuberculosis: are statistical reports accurate? Therapeutic Advances in Infectious Disease. 2014;2(2):61–70. doi: 10.1177/2049936114528173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.World Health Organization. 20. Geneva: World Health Organization; 2015. Global Tuberculosis Report, pp. 2–10. [Google Scholar]
- 18.Barbu Z. Tuberculoza primara, Diseminarile hematogene postprimare, Tuberculoza extrarespiratorie. In: Moisescu V, editor. Tratat de Ftiziologie. Cluj-Napoca: Dacia Press; 1977. pp. 145–264. [Google Scholar]
- 19.World Health Organization. Switzerland: World Health Organizatio; 2016. Global Tuberculosis Report; pp. 1–162. [Google Scholar]
- 20.Koné S, Gbané-Koné M, Bana A, Touré SA, Kouassi AN, Koffi AG, Eti E, Kouakou NM. Unusual multifocal osteoarthritis tuberculosis in an immunocompetent patient. Pan Afr Med J. 2015;20:212–212. doi: 10.11604/pamj.2015.20.212.6015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Engin G, Acunas B, Acunas G, Tunaci M. Imaging of Extrapulmonary Tuberculosis. Radigrafics. 2000;20(2):471–488. doi: 10.1148/radiographics.20.2.g00mc07471. [DOI] [PubMed] [Google Scholar]
- 22.Rajwanshi A, Bhambhani S, Das DK. Fine-needle aspiration cytology diagnosis of tuberculosis. Diagn Cytopathol. 1987;3(1):13–16. doi: 10.1002/dc.2840030104. [DOI] [PubMed] [Google Scholar]
- 23.Narlawar RS, Shah JR, Pimple MK, Patkar DP, Patankar T, Castillo M. Isolated tuberculosis of posterior elements of spine: Magnetic resonance imaging findings in 33 patients. Spine. 2002;27(3):275–281. doi: 10.1097/00007632-200202010-00015. [DOI] [PubMed] [Google Scholar]
- 24.Yusof MI, Hassan E, Rahmat N, Yunus R. Spinal tuberculosis: The association between pedicle involvement and anterior column damage and kyphotic deformity. Spine. 2009;34(7):713–717. doi: 10.1097/BRS.0b013e31819b2159. [DOI] [PubMed] [Google Scholar]
- 25.Saukkonen JJ, Bazydlo B, Thomas M, Strieter RM, Keane J, Kornfeld H. ß-Chemokines Are Induced by Mycobacterium tuberculosis and Inhibit Its Growth. Infect Immun. 2002;70(4):1684–1693. doi: 10.1128/IAI.70.4.1684-1693.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fahey TJ 3rd, Tracey KJ, Tekamp-Olson P, Cousens LS, Jones WG, Shires GT, Cerami A, Sherry B. Macrophage inflammatory protein-1 modulates macrophage function. J Immunol. 1992;148(9):2764–2769. [PubMed] [Google Scholar]
- 27.Guo C, Zhang H, Gao Q, He D, Tang M, Liu S, Deng A, Wang Y, Lu J, Yin X, Guo Q. Monocyte chemoattractant protein-1 in spinal tuberculosis: -362G/C genetic variant and protein levels in Chinese patients. Diagnostic Microbiology and Infectious Disease. 2014;78(1):49–52. doi: 10.1016/j.diagmicrobio.2013.07.024. [DOI] [PubMed] [Google Scholar]
- 28.Zhang HQ, Deng A, Guo CF, Wang YX, Chen LQ, Wang YF, Wu JH, Liu JY. Association between Fok I Polymorphism in Vitamin D Receptor Gene and Susceptibility to Spinal Tuberculosis in Chinese Han Population. Archives of Medical Research. 2010;41(1):46–49. doi: 10.1016/j.arcmed.2009.12.004. [DOI] [PubMed] [Google Scholar]
- 29.Mecabih F. Oran: 2016. table ronde, 15-ème congrès de l'AOLF. [Google Scholar]
- 30.Sánchez D, Rojas M, Hernández I, Radzioch D, García LF, Barrera LF. Role of TLR2- and TLR4-mediated signaling in Mycobacterium tuberculosis-induced macrophage death. Cell Immunol. 2010;260(2):128–136. doi: 10.1016/j.cellimm.2009.10.007. [DOI] [PubMed] [Google Scholar]
- 31.Sajid A, Farid A, Kaleem A, Rauniyar RK. Pott's Spine: Diagnostic Imaging Modalities and Technology Advancements. N Am J Med Sci. 2013;5(7):404–411. doi: 10.4103/1947-2714.115775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Surendar M Tuli. Historical aspects of Pott’s disease (spinal tuberculosis) management. Eur Spine J. 2013;22(Suppl 4):529–538. doi: 10.1007/s00586-012-2388-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Abdelkefi M. Oran: 2016. table ronde, 15-ème congrès de l'AOLF. [Google Scholar]
- 34.Knoeller SM, Markus Uhl. Herget GW. Osteitis or osteomyelitis of the pubis ? A diagnostic and therapeutic challenge: report of 9 cases and review of the literature. Acta Orthop Belg. 2006;72(5):541–548. [PubMed] [Google Scholar]
- 35.Burke G, Joe C, Levine M, Sabio H. Tc-99 m bone scan in unilateral osteitis pubis. Clin Nucl Med. 1994;19(6):535–535. doi: 10.1097/00003072-199406000-00015. [DOI] [PubMed] [Google Scholar]