ABSTRACT
Background: Appropriate provider recommendation is crucial to raising HPV vaccination uptake, yet scant research has explored actual conversations between providers and parents, the effect of parental pre-visit vaccine intention on vaccination, or the effect of conversation style on parental satisfaction with that conversation.Methods: We analyzed 146 audio-recorded clinical encounters between providers, parents/guardians, and HPV vaccine-eligible adolescents, from May 2015 to March 2017, at eight practices in Northeastern U.S. Parents completed pre-visit measures of intent to vaccinate and post-visit assessments of satisfaction with vaccine conversations. We qualitatively analyzed transcribed audio recordings and evaluated associations between providers' vaccine introductions and vaccine receipt.Results: Provider recommendations were empirically defined as “indicated” (clear recommendation that the child receive HPV vaccination at that visit), “elective” (vaccination presented as optional), or “contraindicated” (delay recommended). The vaccination rates were 87%, 68%, and 0% following “indicated,” “elective,” and “contraindicated” presentations respectively. Providers' statements attesting to the vaccine's value to the child did not affect receipt. Parental pre-visit intent to vaccinate was associated with vaccine receipt: 100% for likely/very likely compared to 28% for very unlikely. The association between vaccine recommendation style and vaccine receipt was most pronounced with undecided parents, with 92% accepting vaccination after an “indicated” recommendation vs. 68% after an “elective” recommendation. Satisfaction with vaccine conversations was high regardless of recommendation style.Conclusions: The results suggest that the words used to introduce HPV vaccination have the potential to inform parents' HPV vaccination decisions. Providers should be encouraged to simply state, “Your child is due for the HPV vaccine today.”
KEYWORDS: Human Papillomavirus (HPV) vaccine, provider-parent communication, patient satisfaction
Introduction
The HPV vaccine has the potential to prevent up to 90% of HPV-related cancers.1 While the uptake of other adolescent vaccines in the U.S. has been relatively swift, only 65.1% of females and 56.0% of males aged 13–17 years initiated HPV vaccination in 2016.2 The most consistent predictor of HPV vaccination is whether a child's medical provider recommends the vaccine.3-5
Studies find that providers use different communication strategies to recommend the HPV vaccine and that some styles may be more effective at increasing vaccine receipt.6-11 However, most studies rely on providers' and parents' reports of vaccine recommendation rather than on actual conversations, and the validity of recall-based data may be limited by social desirability and recall biases. In the only known analysis of audio-recorded HPV discussions, Sturm et al. (2017) noted that many pediatricians recommended delay or provided parents with mixed messages about vaccination.9
Because scant research has explored actual conversations between providers and parents, the effect of parental pre-visit vaccine intention on vaccination, or the effect of conversation style on parental satisfaction, we collected data on parental pre-visit vaccine intentions, providers' recommendation styles, vaccine uptake, and parent satisfaction, using parent surveys and audio-recordings of parent-provider-child vaccine discussions during medical visits at samples of diverse participating sites. Our analysis sought to: (1) identify different vaccine recommendation styles, (2) examine the associations between recommendation styles and HPV vaccine receipt, including potential moderation of associations by parents' intentions to vaccinate, and (3) explore the potential effect of recommendation style on parents' satisfaction with vaccine conversations.
Results
Demographic characteristics and parental baseline vaccine intentions
The recruitment rate across our eight sites was 80% (208 of 261 parent-child pairs). Of the 208 parent-child pairs who were recruited, 32 were excluded due to incomplete participation (e.g. parent had to leave for work before completing the post-visit survey) or ineligibility (e.g. revealed later in the visit to have already received their first HPV vaccine). Because this analysis specifically examined the potential effect of providers' HPV vaccine recommendation styles on vaccination controlling for parental vaccine hesitancy, the sample was restricted to transcripts in which the parent completed all relevant portions of the survey and the provider initiated the HPV vaccination discussion. This resulted in the exclusion of an additional 30 cases. Reasons for exclusion of transcripts included parents or children raising the issue of vaccination before the provider (12), parents failing to complete the pre-visit vaccine intention question (2), provider determination that the child was too ill to receive vaccination at that visit (1), provider not mentioning the HPV vaccine (i.e. missed opportunity) (5), parents answering the pre-visit vaccine intention question based on a sibling also in the visit (1), lack of clarify about whether the provider was recommending the HPV vaccine before the parent consented (i.e. parent agreed after provider said the child would be getting a number of vaccines but before the provider specified which ones) (2), provider asking parent which vaccines the child needed (2), parent not bringing the vaccine record (1), and possibility that a vaccine conversation happened without being recorded (4).
This left a total of 146 audio recordings for analysis in which the providers initiated the HPV vaccine conversation (i.e. vaccination was not brought up by the parent), and the parent indicated their intent to vaccinate in the pre-visit survey. Study participants were 46% White, 25% Hispanic, and 20% Black (Table 1). Household income ranged broadly from less than $25,000 to more than $200,000, with a median of about $38,000. Variation in education was similarly broad: 35% reported four or more years of college, while 14% did not complete high school. Participating children were equally likely to be male or female, but 83% of parents/guardians were female. Prior to the medical visit, 41% of parents indicated that they were likely or very likely to vaccinate, 34% were undecided, and 26% were unlikely or very unlikely. However, after speaking with their medical providers, 74% of parents chose HPV vaccination for their child at that visit.
Table 1.
Child and parent demographics and summary statistics.
| Percentage | n | |
|---|---|---|
| Child's race | ||
| Black | 20% | 29 |
| Hispanic | 25% | 37 |
| Other | 9% | 13 |
| White | 46% | 67 |
| Child's gender | ||
| Female | 51% | 75 |
| Male | 49% | 71 |
| Child's age (years) | Mean: 12 | Range: 9–17 |
| Parent's race | ||
| Black | 20% | 29 |
| Hispanic | 24% | 35 |
| Other | 8% | 11 |
| White | 49% | 71 |
| Parent's gender | ||
| Female | 83% | 121 |
| Male | 17% | 25 |
| Parent's age (years) | Mean: 43 | Range: 28–69 |
| Parent's education | ||
| Less than high school | 14% | 20 |
| High school degree or GED | 20% | 29 |
| Some college / Associates degree | 29% | 43 |
| Four-year college or higher | 35% | 51 |
| Household income1 | ||
| Less than $25,000 | 23% | 33 |
| $25,001-$50,000 | 23% | 34 |
| $50,001-$100,000 | 25% | 36 |
| $100,001-$200,000 | 12% | 17 |
| Greater than $200,000 | 4% | 6 |
| Parent's intent to vaccinate prior to the visit | ||
| Very likely | 18% | 26 |
| Likely | 23% | 34 |
| Undecided | 34% | 49 |
| Unlikely | 12% | 17 |
| Very unlikely | 14% | 20 |
| Child received HPV vaccine at visit | ||
| Yes | 74% | 108 |
| No | 26% | 38 |
| Parent's satisfaction with vaccine recommendation1 | ||
| Very satisfied | 61% | 83 |
| Satisfied | 25% | 34 |
| Somewhat satisfied | 0% | 0 |
| Dissatisfied | 0% | 0 |
| Very dissatisfied | 4% | 5 |
| Not mentioned | 2% | 3 |
Percentages do not sum to 100% due to non-response for income question, and addition of satisfaction question 2 months after study start.
Provider presentation of HPV vaccination: Recommendation style and stated value
We identified two main dimensions of vaccine presentations: (1) vaccine recommendation style, which we coded as indicated, elective, or contraindicated and (2) the vaccine's value to the child, which we categorized as low, medium, high, or not mentioned (Table 2). Presentations including statements such as “You are due for the HPV vaccine” or “I recommend the HPV vaccine” were coded as indicated because the staff member's language makes it clear that HPV vaccination is a recommended treatment at the visit. In contrast, if staff discouraged vaccination at any point in the visit, the presentation was coded as contraindicated. Medical staff's presentations were coded as elective when they did not clearly express any recommendation for the vaccination decision, thus framing the HPV vaccine as an option that could be chosen if the parent wished: for example, “If you want to start today, you can, or you can wait until next year.” Statements that opened discussion of HPV vaccination with a non-directive question such as “Are you familiar with the HPV vaccine?” were also coded as elective.
Table 2.
Example presentations by vaccine recommendation style and vaccine value to child.
| Vaccine recommendation style |
|||
|---|---|---|---|
| Vaccine value to child | Indicated | Elective | Contraindicated |
| Not mentioned | You're due for the HPV vaccine. | And you can get the HPV vaccine if you want. | And the HPV vaccine we can do next year. |
| Low | (Male patient) You're due for the HPV vaccine. One of the primary reasons for getting immunized is to help protect women. | Are you going to start the HPV vaccine today? It's a very common one that some people have reservations about. | (11-year-old) I start talking about Gardasil just to let you start thinking about it. I usually start it at 12. Um, that's against genital warts. |
| Medium | The HPV vaccine is recommended to prevent cancer. | If you want, you can start the HPV vaccine, which prevents cervical cancer. | You got the info sheet on the HPV and that's something we definitely recommend. We can probably start the series next year. |
| High | Both of you can get a shot called HPV. And I highly recommend it. Because it protects against cervical cancer in women and genital warts in men. And it's – We routinely give it to all children who are nine or above. Can we go ahead and do that today? | The HPV vaccine. Um, it's not only cervical cancer, it's penile cancer, anal cancer, head and neck cancers, throat cancers, it's a lot of different things. | The HPV vaccine is very important and you can get it starting next year. |
Medical staff expressed the vaccine's value to the child in a variety of ways, such as mentioning the vaccine's cancer preventative benefits or strongly endorsing the vaccine. Presentations were coded as high if staff framed the vaccine as important, expressed a desire to have the child vaccinated, or emphasized the risk of death from vaccine or pain to the child. Presentations were coded as medium if the staff mentioned cancer prevention but did not use language that emphasized the vaccine's or cancer prevention's importance. Presentations were coded as low if the provider mentioned the vaccine was not important for the child at that time, e.g., when staff said to a male patient that HPV vaccination would primarily benefit women. Introductions where staff did not make any mention regarding the vaccine's value or did not endorse the vaccine were coded as value not mentioned.
Association between provider recommendation style and HPV vaccine uptake
The indicated style of presentation was observed in 78 of the 146 (53%) visit in 68 of these cases (87%), the child received the first dose of the HPV vaccine series at that visit. In contrast, only 67% (n = 40) of the 59 parent child pairs that received elective introductions chose to vaccinate (p = 0.006). None of the nine parent-child pairs that received a contraindicated presentation vaccinated, even though six of the parents (67%) reported prior to the visit that they were very likely/likely to vaccinate their children at that visit.
The effect of recommendation style appeared to vary by parents' expressed intent to vaccinate. Recommendation style primarily affected parents who reported that they were undecided regarding vaccination immediately prior to the visit; there was little difference when parents were likely or very likely to vaccinate, or very unlikely to do so. As shown in the stratified analysis of Fig. 1, among parents who were initially undecided, 17 of 25 (68%) who received an elective introduction decided in favor of vaccination, but 22 of the 24 (92%) who received an indicated introduction agreed to having their child vaccinated (p = 0.04). Among parents who were very unlikely pre-visit but changed their minds and vaccinated their children, written comments indicated that it was not the initial presentation, but subsequent informative conversations with their providers that made a difference, with statements such as “She answered some of the questions I had” and “She talked about how it prevents disease.” While adolescents were present during these encounters, they rarely made statements that appeared to influence vaccine receipt.
Figure 1.
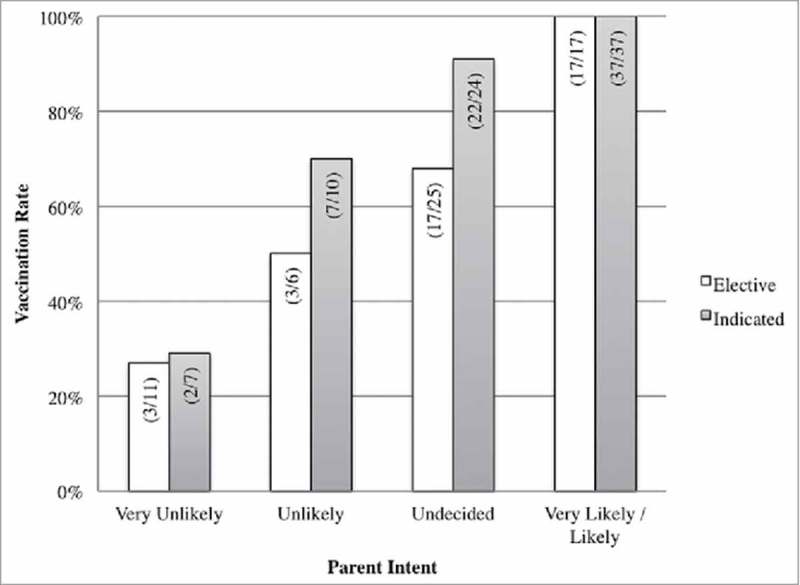
HPV vaccination rate, by HPV vaccine recommendation style and parent intent to vaccinate (N = 146).
Association between vaccine value to child and HPV vaccine receipt
Among the 146 parent-child pairs, 13% (n = 19), 25% (n = 36), and 4% (n = 6) received high, medium, and low value presentations, respectively, while value was not mentioned to 58% (n = 85). In contrast to vaccine recommendation style, value statements had no apparent association with vaccine receipt, either when considering all parents together or stratifying by pre-visit vaccine intent. Analyses also indicated little effect of value strength, so low, medium, and high value categories were collapsed into the single category.
Parent satisfaction with vaccine conversations
Satisfaction with vaccine conversations was uniformly high, with no differences by vaccine recommendation style. As shown in Fig. 2, among parents receiving indicated introductions, 74% (n = 51) were very satisfied, and 24% (n = 17) were satisfied, compared to 61% (n = 33) and 32% (n = 17) respectively for elective introductions (p = 0.29). Using an indicated style did not appear to impact parents' comfort with asking questions or expressing their concerns to providers or parents' feelings of autonomy, as indicated by free-response comments: “I was very comfortable discussing and asking questions in regards (sic) research studies and reviews” and “Doctor explained the vaccine very well. Very informative and no pressure to get it.”
Figure 2.
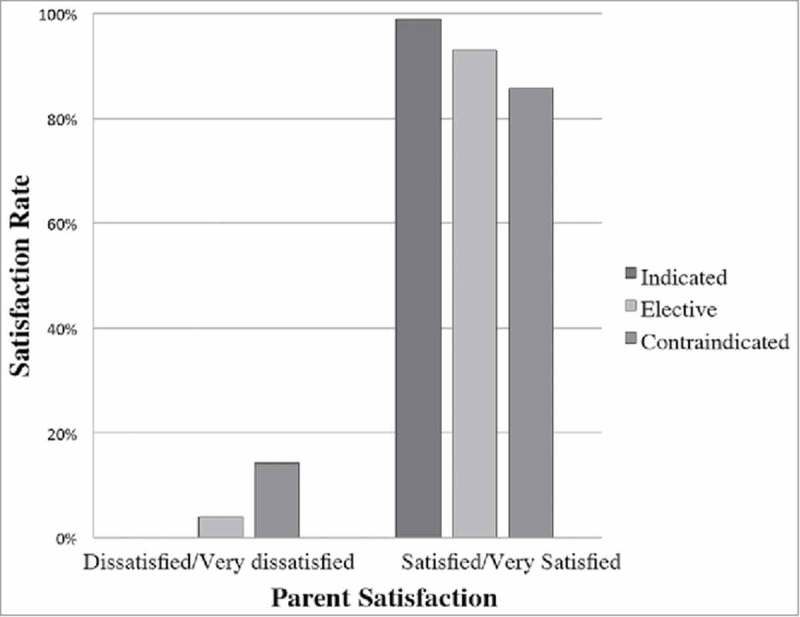
Satisfaction with vaccine conversation, by HPV vaccine recommendation style and parent intent to vaccinate (N = 146).
Parental satisfaction did not appear to vary by inclusion of value statements in vaccine introductions either when analyzed by low, medium, high or no value statement, or when dichotomized by the presence or absence of a value statement. Among parents who received a presentation with a value statement, 73% (n = 36 of 49) were very satisfied compared to 71% (n = 53 of 75) of parents who did not hear a value statement (p = 0.40).
Discussion
Our results suggest that introducing HPV vaccination as an indicated medical treatment to eligible patients may increase HPV vaccine uptake. Based on our analysis, we estimate that if all parents in our sample had received an indicated rather than an elective or contraindicated introduction, our total vaccination rate might have increased from to 74% to 87%. Our findings are consistent with prior literature that demonstrates the importance of provider recommendations.9,12,13 Our study advances research, however, by identifying the specific characteristics of a vaccine presentation that could encourage vaccine uptake. The simple initial framing of HPV vaccination as a “due” or “needed” vaccine appears to increase parents' likelihood of vaccinating, irrespective of whether the provider describes the vaccine's value in the initial presentation. Current HPV vaccine initiation rates nationwide in the US have now reached 60%,2 so ensuring that all providers present HPV vaccination as an indicated medical treatment to all age-eligible patients could facilitate reaching the Healthy People 2020 goal of 80% population-wide coverage.
In contrast, we found that a provider recommendation of delay for any reason resulted in non-vaccination, even among parents who wanted the HPV vaccine for their children. Nearly 67% of parents in our study who received recommendations to delay by their providers expressed strong support for vaccination prior to the visit. Of note, all of these providers stated that they supported HPV vaccination overall but were recommending delay of vaccination to a subsequent visit. Therefore, providers themselves may be unaware that they are in effect withholding vaccination from a substantial proportion of parents who wish to vaccinate. In theory, delay is not problematic as long as vaccination is initiated in a timely manner. However, some parents who intended to merely delay vaccination have reported that their children ultimately were never vaccinated.10,14
We found vaccine recommendation style may be persuasive for parents who are undecided about vaccination prior to speaking with their providers. One explanation for this finding may relate to perceived ambiguity in medical decision-making. Ambiguity arises from confusion around the reliability and trustworthiness of medical information and can occur when patients receive incomplete or conflicting recommendations.15 Medical ambiguity is further complicated by patients' rising reliance on social and mass media for information, which casts doubt upon medical professionals' expert knowledge.16,17 Research on medical decision-making indicates that when confronted with ambiguous information about potential benefits and risks, people often judge risks pessimistically and avoid making decisions – such as opting to delay vaccination.16,18,19,20,21 We theorize that one reason undecided parents are less likely to vaccinate after an elective introduction may be due to higher levels of perceived ambiguity. Thus, parents and guardians who are unsure of whether HPV vaccination is appropriate prior to their appointments may choose to delay in the absence of a clear, unambiguous recommendation from their healthcare provider. Being clear that the HPV vaccine is recommended appears to play a far more important role than expressing the value of vaccination, as we found that introductory statements about why vaccination is valuable to the patient were not associated with vaccine uptake.
In contrast, parents with favorable attitudes toward HPV vaccination at baseline are very likely to vaccinate their children unless explicitly directed not to by their provider. Therefore, strategies aimed at increasing parental confidence in HPV vaccination may also have worth. However, additional research is needed to understand how to achieve this goal, as studies indicate that educational messages intended to increase confidence and dispel myths may paradoxically raise doubts and increase perceived safety risks.22 As many negative messages are found on social media, there is great interest in harnessing the influence of social media for positive outcomes, but little is known to date about effective uses of this medium for increasing vaccine confidence.23
An important consideration when approaching vaccine communication is parental satisfaction with the interaction. In contrast to one study that noted a minor decrement in patient satisfaction with the use of “presumptive” compared to “participatory” language,24 we found that nearly all patients who received indicated vaccine introductions were satisfied or very satisfied with the interaction. Indeed, several parents wrote in statements praising their providers' vaccine-related communication. Our analysis exclusively examined the impact of vaccine recommendation style – the first statement by the medical provider and thus the parents' first impression of expectations around vaccination. We did not explore the subsequent conversations and negotiations that followed the initial opening, leaving them for a separate analysis. Yet, for now, we note that framing HPV vaccination as indicated does not appear to limit subsequent conversations. Indeed, discussions following vaccine recommendations may be particularly important for hesitant parents. Indeed, written comments from parents with vaccine concerns prior to the visit who chose to vaccinate their children indicated that informative conversations with providers influenced their decisions to vaccinate.
While our conclusion that stating HPV vaccine is indicated for the child at the current visit tends to lead to vaccine acceptance has found support in previous studies, the data and analysis presented here are significant additions. First, we can accurately assess provider HPV vaccine recommendation styles and assess their association with vaccine receipt since we are one of the few studies to base our analysis on actual parent-provider vaccine discussions. Second, we report on the apparent interaction between parental intention to vaccinate, provider communication, and vaccine acceptance. While we have known that both parents and providers affect vaccine conversations, the interplay between parental attitudes and provider statements in the context of a single medical visit has not previously been examined. Third, we use audio recordings to link parent-provider conversations with actual vaccine receipt in real time, eliminating recall bias, and providing a data piece missing from survey studies. Fourth, we report the effect that providers' vaccine recommendation styles may have on parents' satisfaction with vaccine conversations. This is a relatively understudied but important research gap since providers often report hesitation to strongly recommend the HPV vaccine out of concern that they will upset parents and harm their therapeutic relationship. Based on our findings, that concern may be unwarranted. The ability to reassure pediatricians that recommended communication techniques are compatible with strong patient-provider relationships is crucial if we intend to design and implement interventions based on effective communication techniques.
So can providers be trained to introduce HPV vaccination as indicated instead of elective? A randomized controlled trial by Brewer et al. delivered a one-hour session to train providers to “announce” versus have “conversations” about the HPV vaccine and demonstrated a 5% increase in HPV vaccination rates for 11–12 year olds at intervention compared to control clinics.9 While this is an important result, the magnitude of the increase was small, and the extent to which providers implemented “announcements” in practice was not evaluated. Thus, additional research is needed to determine effective and efficient ways to improve provider communication.
Limitations
This was a qualitative study of audio-recorded interactions between clinicians, parents, and adolescents. Due to the exploratory nature of qualitative data and limited sample size, multivariable logistic regression analyses are not possible. While our sample has substantial diversity related to race/ethnicity, parental education level, socioeconomic status, practice setting, urban/suburban/rural variation, and baseline vaccine intentions, all data were collected in the Northeast, which could limit generalizability to other U.S. regions. We recruited only parents who spoke either English or Spanish, although we had many patients from other countries who spoke English in addition to their native languages. In addition, non-participants could differ in important ways from parents who agreed to participate in the study. Our data collection methods – asking parents to complete surveys prior to visits and audio recording visits – may have affected vaccine conversations and decisions. We attempted to limit this bias to the extent possible by framing the study as a general vaccine study rather than an HPV vaccine study, placing audio recorders in less evident positions in the exam room, and not specifically alerting providers when a visit was recorded. Social desirability bias may have affected parents' survey responses and providers' recommendation styles, though we tried to ameliorate this effect by ensuring that research staff had no medical role in the clinical space, keeping surveys anonymous, and not specifically informing providers when visits were audio-recorded. We do not believe there was significant social desirability bias as a substantial proportion of parents expressed disagreement with current vaccine recommendations, and many providers did not follow CDC recommendations for vaccine discussions. If providers were conscious of audio recording when discussing vaccination, then recordings represent a best-case scenario for communication. We do not believe there was significant recall bias related to pre-visit intention, vaccine receipt, or satisfaction with the vaccine conversation because the pre-visit surveys were collected immediately before the visit, the post-visit surveys were collected within 10 minutes of the conclusion of the visit, and the patient-provider conversations were audio-recorded in real time. Finally, we did not explore conversations and negotiations beyond the initial vaccine recommendation within the scope of this paper as we wanted to focus solely on vaccine introduction—an actionable target for behavior change—in this analysis. Future research should validate these findings in larger samples and may also more deeply explore the role of adolescents in vaccine decision-making.
Conclusion
Introducing the HPV vaccine as a clearly indicated medical treatment appears to substantially improve vaccination rates. In this sense, we are advocating that providers present the HPV vaccine similarly to other vaccines, by opening the conversation with a simple statement such as: “Your child is due for the HPV vaccine today.”
Patients and methods
Setting
Audio recordings of primary-care, clinical interactions between medical staff and parents/guardians were collected between May 2015 and March 2017 at three urban community health centers and one hospital-based practice serving largely uninsured and Medicaid-insured patients and four urban and suburban practices serving a mix of Medicaid-insured and privately insured patients in the Northeastern United States. The health centers and hospital-based practice are part of two different affiliated networks. At all sites, clinical leadership agreed to participate in the study. The eight practices served diverse populations, including White, Black, and Hispanic patients; immigrants from the Americas, the Caribbean, Eastern Europe, and Africa; and patients of varying socioeconomic and educational backgrounds. In the US at the time of this study, out-of-pocket costs were not a barrier to vaccination since all types of insurance in the US, including Medicaid, cover HPV vaccination, while the federal Vaccines for Children Program covers costs for uninsured children.
Participants
Parent/legal guardian-child pairs were eligible to participate if the child was eligible to initiate HPV vaccination and the parent spoke English or Spanish. Practice schedules were reviewed to identify eligible patients. Research staff approached parents/legal guardians of all eligible patients who had appointments during the recruitment periods in the waiting areas or exam rooms to determine their interest in participating. After giving written informed consent, parents completed two surveys, one before seeing the provider and one immediately afterwards.
Parent/guardian surveys
Parents were asked to complete a 5–10 minute pre-and post-visit survey. Along with demographic characteristics, the pre-visit survey included a question on parental likelihood of accepting HPV vaccination rated on a five-level Likert scale ranging from very unlikely to very likely to vaccinate that day, based on the NIS-Teen survey.25 To assess parents' general vaccine hesitancy and to position the study as a general adolescent vaccine study rather than one focused on HPV, parents were also asked to assess a number of general vaccine statements.26 These responses are not evaluated here. The post-visit survey asked parents whether the child had received the HPV vaccine that day and how satisfied the parent felt with the vaccine conversations, rated on a five-level Likert scale ranging from very dissatisfied to very satisfied. Participants were compensated with gift cards.
Provider audio recording
All medical providers who discussed vaccination during the patient encounter were recorded, including physicians, advanced practice professionals (nurse practitioners and physician assistants), nurses, and medical assistants. Providers were recruited through study physicians at each site; no compensation was provided. Nearly all eligible providers (98.5%; n = 132 of 134) agreed to audio recordings. The institutional review boards of Boston University Medical Center and Harvard University approved this study.
Coding procedures
All vaccine-related verbal interaction by medical staff, parents, and children was transcribed verbatim. Non-English transcripts were transcribed in Spanish with English translation and coded by two bilingual coders (RP and TE). Three coders (AF, TE, and RP) read entire transcripts and determined where vaccine introduction statements began and ended via consensus.
Our analytic approach draws upon the ethnography of communication, particularly negotiation, and previous research on HPV provision.9,27,28,29 We sought to identify providers' presentational styles, that is, specific ways of formulating the presentation of HPV vaccination in the local context of a clinical encounter associated with the receipt of HPV vaccination during the clinical encounter. We audio-recorded entire visits but focused on vaccine discussions, and specifically the language providers used to present HPV vaccination as part of the agenda of the visit, informed by previous research. We identified three phases of vaccine discussions: (1) providers' initial vaccine presentation to the parent/guardian and child; (2) parent/guardian's vaccine decision; and (3) if parents or children had questions or concerns about vaccination, negotiations about the vaccine. We focused exclusively on the initial vaccine presentation because a) providers tended to repeat the same language, or script, when introducing vaccines and b) parents' vaccine decisions were often made following a short initial presentation. We compared cases where the vaccine was provided and where it was not to define a parsimonious set of qualitatively distinct forms of presentation associated with vaccine receipt. The association between type of presentation and receipt of HPV vaccination was then examined further with the chi-square test.
HPV vaccine receipt
HPV vaccine receipt – whether or not the child received the HPV vaccine at that visit – was coded based on evidence from the audio recording that the child was vaccinated (i.e. the portion of the visit where the nurse administered the vaccine), which occurred in 123 of the 146 recordings. If actual vaccine administration was not recorded, we used parents' post-visit survey responses. To preserve patient anonymity, we did not perform medical record review. However, the post-visit surveys were completed before the parent and child left the healthcare facility, minimizing the likelihood of recall bias. The association between presentation style and vaccine receipt was assessed using the chi-square test. Significance was accepted at p<0.05.
Funding Statement
American Cancer Society (US) source. This work was supported by an American Cancer Society Research Scholar Grant [grant number 128607-RSG-15-150-01-CPHPS]. No commercial support was obtained.
Abbreviations
- HPV
Human Papillomavirus
Disclosure of potential conflicts of interest
No potential conflicts of interest were disclosed
References
- 1.Centers for Disease Control and Prevention (CDC) Human papillomavirus-associated cancers United States, 2004–2008. MMWR Morb Mortal Wkly Rep. 2012;61:258–61. PMID:22513527. [PubMed] [Google Scholar]
- 2.Walker TY, Elam-Evans LD, Singleton JA, Yankey D, Markowitz LE, Fredua B, Williams CL, Meyer SA, Stokley S. National, regional, state, and selected local area vaccination coverage among Adolescents Aged 13–17 Years – United States, 2016. MMWR Morb Mortal Wkly Rep. 2017;66(33):874–82. doi: 10.15585/mmwr.mm6633a2. PMID:28837546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dorell CG, Yankey D, Santibanez TA, Markowitz LE. Human papillomavirus vaccination series initiation and completion, 2008–2009. Pediatrics. 2011;128(5):830–9. doi: 10.1542/peds.2011-0950. PMID:22007006. [DOI] [PubMed] [Google Scholar]
- 4.Smith PJ, Stokley S, Bednarczyk RA, Orenstein WA, Omer SB. HPV vaccination coverage of teen girls: The influence of health care providers. Vaccine. 2016;34(13):1604–10. doi: 10.1016/j.vaccine.2016.01.061. PMID:26854907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Darden PM, Thompson DM, Roberts JR, Hale JJ, Pope C, Naifeh M, Jacobson RM. Reasons for not vaccinating adolescents: National immunization survey of teens, 2008–2010. Pediatrics. 2013;131(4):645–51. doi: 10.1542/peds.2012-2384. PMID:23509163. [DOI] [PubMed] [Google Scholar]
- 6.Hughes CC, Jones AL, Feemster KA, Fiks AG. HPV vaccine decision making in pediatric primary care: a semi-structured interview study. BMC Pediatr. 2011;11:74. doi: 10.1186/1471-2431-11-74. PMID:21878128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McRee AL, Gilkey MB, Dempsey AF. HPV vaccine hesitancy: Findings from a statewide survey of health care providers. J Pediatr Health Care. 2014;28(6):541–9. doi: 10.1016/j.pedhc.2014.05.003. PMID:25017939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gilkey MB, Malo TL, Shah PD, Hall ME, Brewer NT. Quality of physician communication about human papillomavirus vaccine: Findings from a National Survey. Cancer Epidemiol Biomarkers Prev. 2015;24(11):1673–9. doi: 10.1158/1055-9965.EPI-15-0326. PMID:26494764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sturm L, Donahue K, Kasting M, Kulkarni A, Brewer NT, Zimet GD. Pediatrician-parent conversations about human papillomavirus vaccination: An analysis of audio recordings. J Adolesc Health. 2017;61(2):246–51. doi: 10.1016/j.jadohealth.2017.02.006. PMID:28455129. [DOI] [PubMed] [Google Scholar]
- 10.Perkins RB, Clark JA, Apte G, Vercruysse JL, Sumner JJ, Wall-Haas CL, Rosenquist AW, Pierre-Joseph N. Missed opportunities for HPV vaccination in adolescent girls: A qualitative study. Pediatrics. 2014;134(3):e666–74. doi: 10.1542/peds.2014-0442. PMID:25136036. [DOI] [PubMed] [Google Scholar]
- 11.Hughes CC, Jones AL, Feemster KA, Fiks AG. HPV vaccine decision making in pediatric primary care: a semi-structured interview study. BMC Pediatr. 2011;11:74. doi: 10.1186/1471-2431-11-74. PMID:21878128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gilkey MB, Calo WA, Moss JL, Shah PD, Marciniak MW, Brewer NT. Provider communication and HPV vaccination: The impact of recommendation quality. Vaccine. 2016;34(9):1187–92. doi: 10.1016/j.vaccine.2016.01.023. PMID:26812078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vadaparampil ST, Malo TL, Sutton SK, Ali KN, Kahn JA, Casler A, Salmon D, Walkosz B, Roetzheim RG, Zimet GD, et al.. Missing the target for routine human papillomavirus vaccination: Consistent and strong physician recommendations are lacking for 11–12 year old males. Cancer Epidemiol Prev Biomark. 2016;25(10):1435–46. cebp-1294. doi: 10.1158/1055-9965.EPI-15-1294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Niccolai LM, Hansen CE, Credle M, Shapiro ED. Parents' recall and reflections on experiences related to HPV vaccination for their children. Qual Health Res. 2016;26(6):842–50. doi: 10.1177/1049732315575712. PMID:25779984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Han PKJ, Moser RP, Klein WMP. Perceived ambiguity about cancer prevention recommendations: associations with cancer‐related perceptions and behaviours in a US population survey. Health Expect. 2007;10(4):321–36. doi: 10.1111/j.1369-7625.2007.00456.x. PMID:17986069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Han PKJ, Moser RP, Klein WMP, Beckjord EB, Dunlavy AC, Hesse BW. Predictors of perceived ambiguity about cancer prevention recommendations: Sociodemographic factors and mass media exposures. Health Commun. 2009;24(8):764–72. doi: 10.1080/10410230903242242. PMID:20183385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fox RC. The Evolution of Medical Uncertainty. Milbank Mem Fund Q Health Soc. 1980;58(1):1–49. doi: 10.2307/3349705. PMID:6903782. [DOI] [PubMed] [Google Scholar]
- 18.Volk RJ, Spann SJ, Cass AR, Hawley ST. Patient education for informed decision making about prostate cancer screening: A randomized controlled trial with 1-Year Follow-Up. Ann Fam Med. 2003;1(1):22–8. doi: 10.1370/afm.7. PMID:15043176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ritov I, Baron J. Reluctance to vaccinate: Omission bias and ambiguity. J Behav Decis Mak. 1990;3(4):263–77. doi: 10.1002/bdm.3960030404. [DOI] [Google Scholar]
- 20.Meszaros JR, Asch DA, Baron J, Hershey JC, Kunreuther H, Schwartz-Buzaglo J. Cognitive processes and the decisions of some parents to forego pertussis vaccination for their children. J Clin Epidemiol. 1996;49(6):697–703. doi: 10.1016/0895-4356(96)00007-8. PMID:8656233. [DOI] [PubMed] [Google Scholar]
- 21.Brashers DE. Communication and uncertainty management. J Commun. 2001;51(3):477–97. doi: 10.1111/j.1460-2466.2001.tb02892.x. [DOI] [Google Scholar]
- 22.Nyhan B, Reifler J, Richey S, Freed GL. Effective messages in vaccine promotion: a randomized trial. Pediatrics. 2014;133(4):e835–42. doi: 10.1542/peds.2013-2365. PMID:24590751. [DOI] [PubMed] [Google Scholar]
- 23.Politi MC, Jones KM, Philpott SE. The role of patient engagement in Addressing Parents' Perceptions about immunizations. Jama. 2017;318(3):237–8. doi: 10.1001/jama.2017.7168. PMID:28654974. [DOI] [PubMed] [Google Scholar]
- 24.Opel DJ, Mangione-Smith R, Robinson JD, Heritage J, DeVere V, Salas HS, Zhou C, Taylor JA. The influence of provider communication behaviors on parental vaccine acceptance and visit experience. Am J Public Health. 2015;105(10):1998–2004. doi: 10.2105/AJPH.2014.302425. PMID:25790386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25].CDC NIS-Teen Hard Copy Questionnaire [Internet]. 2017 [cited 2018April12];Available from: https://www.cdc.gov/vaccines/imz-managers/nis/downloads/NIS-Teen-Questionnaire-Q3-2017.pdf
- 26.Rosenthal SL, Weiss TW, Zimet GD, Ma L, Good MB, Vichnin MD. Predictors of HPV vaccine uptake among women aged 19–26: importance of a physician's recommendation. Vaccine. 2010;29(5):890–5. doi: 10.1016/j.vaccine.2009.12.063. PMID:20056186. [DOI] [PubMed] [Google Scholar]
- 27.Perkins RB, Clark JA. What affects human papillomavirus vaccination rates? A qualitative analysis of providers' perceptions. Womens Health Issues. 2012;22(4):e379–86. doi: 10.1016/j.whi.2012.04.001. PMID:22609253. [DOI] [PubMed] [Google Scholar]
- 28.Perkins RB, Chigurupati NL, Apte G, Vercruysse J, Wall-Haas C, Rosenquist A, Lee L, Clark JA, Pierre-Joseph N. Why don't adolescents finish the HPV vaccine series? A qualitative study of parents and providers. Hum Vaccin Immunother. 2016;12(6):1528–35. doi: 10.1080/21645515.2015.1118594. PMID:26810765.27413667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Henrikson NB, Tuzzio L, Gilkey MB, McRee A-L “You're never really off time”: Healthcare providers' interpretations of optimal timing for HPV vaccination. Prev Med Rep. 2016;4:94–7. doi: 10.1016/j.pmedr.2016.05.002. PMID:27413667. [DOI] [PMC free article] [PubMed] [Google Scholar]


