ABSTRACT
There is an urgent need to examine the magnitude and factors responsible for missed opportunities for vaccination, to rapidly achieve national immunization targets. The objective of the study was to examine the influence of individual, neighbourhood and country level socioeconomic position on missed opportunities for vaccination (MOV) in Sub-Saharan Africa. We used multilevel logistic regression analysis on Demographic and Health Survey data collected between 2007 and 2016 in sub-Saharan Africa. We analysed data on 43,637 children aged 12 to 23 months (Level 1) nested within 15,122 neighbourhoods (Level 2) from 35 countries (Level 3). After adjustment for individual-, neighbourhood- and country-level factors, the following appeared as significant risk factors for increased odds of MOV: high birth order, high number of under-five children in the house, poorest household, lack of maternal education, lack of media access, and living in poorer neighbourhood. According to the intra-country and intra-neighbourhood correlation coefficient, 18.4% and 37.4% of the variance in odds of MOV could be attributed to the country and neighbourhood level factors, respectively; and if a child moved to another country or neighbourhood with a higher probability of MOV, the median increase in their odds of MOV would be 2.47 and 2.56 fold respectively. This study has revealed that the risk of missed opportunities for vaccination in sub-Saharan Africa is influenced by not only individual factors but also by compositional factors such as family’s financial capacity, place of birth and upbringing.
Keywords: missed opportunity for vaccination, sub-Saharan Africa
Introduction
It is undeniable that the use of vaccines have prevented more premature deaths, permanent disability and suffering, in all regions of the world, than any other medical discovery or intervention.1,2 According to the 2016 Global Burden of Disease Study, the number of children dying before their fifth birthday declined from 16.4 million to 5.0 million between 1970 and 2016 respectively.3 Each year, more than 100 million infants are immunized, saving 2–3 million lives annually.4 However, the number of unvaccinated and undervaccinated children in sub-Saharan African countries is disproportionately high, with consequent high child mortality in the region. Despite the availability of vaccines within the health systems, children who require them are still missed, thus resulting in missed opportunities for vaccination (MOV).5
In 2016, the World Health Organization’s (WHO) highest advisory group on all immunization-related issues; Strategic Advisory Group of Experts (SAGE) on immunization, approved the updated MOV strategy in light of the slow pace towards the attainment of immunization coverage targets globally. They defined MOV as missing the benefit of getting immunized by an eligible individual who is unvaccinated or partially vaccinated (with no contraindication), despite contact with health services.6 A global comparison between the current prevalence of MOV and the prevalence documented in the first report on MOV by the WHO in 19937 shows no improvement over a 22 year time span.8 Traditionally the proportion of children who receive the full series of three doses of diphtheria-tetanus-pertussis containing vaccines (DTP3) by 12 months of age is used as a key performance indicator for vaccine coverage.9 Therefore, the updated MOV strategy is a potentially useful plan for ensuring equitable and timely access to vaccination for all children.6
If global vaccination coverage were improved, an additional 1.5 million deaths from dipththeria, neonatal tetanus and pertussis could be averted.10 Understanding the determinants of missed opportunities for vaccination at the individual, neighbourhood and country level is important for designing and implementing interventions that will increase vaccination coverage. Much research have focused on individual-level socio-demographic factors.11–14 Yet, theories suggest that determinants in population health are epistemologically multilevel contextual factors (involving community and societal level).15 Focusing only on one level – either the micro individual level or the macro scale of contexts – generates conceptual and practical problems. Single level ecological analyses that use only aggregated data are prone to “ecological fallacy”, when aggregate level associations are wrongly inferred to exist at the individual level. Similarly, a single-level approach, where only individual level data are used for modelling is prone to “atomistic fallacy”, when individual level associations are wrongly inferred to exist at the aggregate level.16 Therefore, the objectives of this study were to determine the prevalence of missed opportunities for vaccination in sub-Saharan Africa and to examine the separate and independent association of individual, neighbourhood and country level factors associated with missed opportunities for vaccination in children from sub-Saharan Africa countries.
Results
Sample characteristics
We analysed information on 43,934 children aged 12 to 23 months (Level 1) nested within 15,246 neighbourhoods (Level 2) from 35 countries (Level 3) in sub-Saharan Africa (Table 2). The median number of neighbourhoods sampled was 374, ranging from 90 in Sao Tome and Principe to 1382 in Kenya. The median number of children aged 12 to 23 months was 942 (range: 304 to 5506) with over half of the children being males. The average age of the children was 17 months. About 47% of the mothers were between 25 to 34 years old and about 40% had no formal education. One third of the mothers were not working at the time of the survey. Most of the respondents were living in the rural areas (70%). Table 1 shows the countries, year of data collection, and the surveys characteristics.
Table 2.
Summary of pooled sample characteristics of the demographic and health surveys data in sub-Saharan Africa.
| Missed Opportunities for Vaccination |
||||
|---|---|---|---|---|
| Overall |
Yes |
NO |
||
| Number (%) | Number (%) | Number (%) | ||
| 43934 | 23751 | 20183 | ||
| Child’s age (mean (sd)) | 17.10 (3.42) | 17.17 (3.40) | 17.02 (3.45) | < 0.001 |
| Male (%) | 22248 (50.6) | 12063 (50.8) | 10185 (50.5) | 0.502 |
| High birth order (%) | 13691 (31.2) | 6954 (29.3) | 6737 (33.4) | < 0.001 |
| Under-five children (mean (sd)) | 2.04 (1.23) | 2.01 (1.24) | 2.08 (1.21) | < 0.001 |
| Maternal age (%) | 0.237 | |||
| 15–24 | 14601 (33.2) | 7810 (32.9) | 6791 (33.6) | |
| 25–34 | 20560 (46.8) | 11177 (47.1) | 9383 (46.5) | |
| 35–49 | 8773 (20.0) | 4764 (20.1) | 4009 (19.9) | |
| Wealth index(%) | < 0.001 | |||
| poorest | 11212 (25.5) | 5540 (23.3) | 5672 (28.1) | |
| poorer | 9646 (22.0) | 4943 (20.8) | 4703 (23.3) | |
| middle | 8578 (19.5) | 4577 (19.3) | 4001 (19.8) | |
| richer | 7754 (17.6) | 4435 (18.7) | 3319 (16.4) | |
| richest | 6744 (15.4) | 4256 (17.9) | 2488 (12.3) | |
| Maternal education (%) | < 0.001 | |||
| no education | 17448 (39.7) | 9426 (39.7) | 8022 (39.8) | |
| primary | 15320 (34.9) | 7685 (32.4) | 7635 (37.8) | |
| secondary+ | 11161 (25.4) | 6637 (27.9) | 4524 (22.4) | |
| Not working (%) | 14277 (32.5) | 7855 (33.1) | 6422 (31.8) | 0.005 |
| Media access (%) | < 0.001 | |||
| 0 | 15010 (34.2) | 7538 (31.7) | 7472 (37.0) | |
| 1 | 13657 (31.1) | 7394 (31.1) | 6263 (31.0) | |
| 2 | 10733 (24.4) | 5942 (25.0) | 4791 (23.7) | |
| 3 | 4534 (10.3) | 2877 (12.1) | 1657 (8.2) | |
| Rural (%) | 30473 (69.4) | 16109 (67.8) | 14364 (71.2) | < 0.001 |
| Neighbourhood SES (%) | < 0.001 | |||
| Quintile 1 (least disadvantaged) | 9018 (20.5) | 5402 (22.7) | 3616 (17.9) | |
| Quintile 2 | 8651 (19.7) | 4675 (19.7) | 3976 (19.7) | |
| Quintile 3 | 8817 (20.1) | 4543 (19.1) | 4274 (21.2) | |
| Quintile 4 | 8816 (20.1) | 4592 (19.3) | 4224 (20.9) | |
| Quintile 5 (most disadvantaged) | 8632 (19.6) | 4539 (19.1) | 4093 (20.3) | |
| Human Development Index (%) | < 0.001 | |||
| Low HDI | 14425 (32.8) | 8280 (34.9) | 6145 (30.4) | |
| Moderate HDI | 15931 (36.3) | 8647 (36.4) | 7284 (36.1) | |
| High HDI | 13578 (30.9) | 6824 (28.7) | 6754 (33.5) | |
Table 1.
Description of demographic and health surveys data by countries, in sub-Saharan Africa, 2007 to 2016.
| Human Development Index |
||||||
|---|---|---|---|---|---|---|
| Country | Survey year | Number of children | Number of neighbourhoods | MOV (%) | Value | Category* |
| Angola | 2016 | 1334 | 555 | 54.72264 | 0.533 | High HDI |
| Benin | 2012 | 2400 | 698 | 57.83333 | 0.485 | Moderate HDI |
| Burkina Faso | 2011 | 1357 | 513 | 18.42299 | 0.402 | Low HDI |
| Burundi | 2010 | 743 | 322 | 22.34186 | 0.404 | Low HDI |
| Cameroon | 2011 | 1124 | 478 | 41.81495 | 0.518 | Moderate HDI |
| Chad | 2015 | 1838 | 585 | 47.22524 | 0.396 | Low HDI |
| Comoros | 2012 | 549 | 218 | 36.97632 | 0.727 | High HDI |
| Congo | 2012 | 942 | 346 | 64.43737 | 0.592 | High HDI |
| Congo DR | 2014 | 1687 | 516 | 63.36692 | 0.435 | Low HDI |
| Cote d’ Ivoire | 2012 | 706 | 295 | 51.27479 | 0.474 | Moderate HDI |
| Ethiopia | 2016 | 1813 | 583 | 53.44732 | 0.448 | Low HDI |
| Gabon | 2012 | 730 | 278 | 88.76712 | 0.697 | High HDI |
| Gambia | 2013 | 722 | 235 | 21.05263 | 0.452 | Low HDI |
| Ghana | 2014 | 563 | 297 | 36.94494 | 0.579 | High HDI |
| Guinea | 2012 | 666 | 264 | 54.95495 | 0.414 | Low HDI |
| Kenya | 2014 | 3764 | 1382 | 43.33156 | 0.555 | High HDI |
| Lesotho | 2014 | 304 | 205 | 35.52632 | 0.497 | Moderate HDI |
| Liberia | 2013 | 665 | 285 | 54.28571 | 0.427 | Low HDI |
| Madagascar | 2009 | 1013 | 473 | 55.97236 | 0.512 | Moderate HDI |
| Malawi | 2016 | 1073 | 600 | 42.03169 | 0.476 | Moderate HDI |
| Mali | 2013 | 914 | 380 | 59.40919 | 0.442 | Low HDI |
| Mozambique | 2011 | 2099 | 579 | 31.49119 | 0.418 | Low HDI |
| Namibia | 2013 | 405 | 289 | 19.75309 | 0.64 | High HDI |
| Niger | 2012 | 977 | 416 | 46.26407 | 0.353 | Low HDI |
| Nigeria | 2013 | 5506 | 889 | 43.35271 | 0.527 | Moderate HDI |
| Rwanda | 2015 | 722 | 382 | 59.9723 | 0.498 | Moderate HDI |
| SaoTomeP | 2009 | 357 | 90 | 22.12885 | 0.574 | High HDI |
| Senegal | 2011 | 880 | 335 | 48.75 | 0.494 | Moderate HDI |
| SierraLeone | 2013 | 944 | 374 | 30.50847 | 0.42 | Low HDI |
| Swaziland | 2007 | 473 | 213 | 16.06765 | 0.541 | High HDI |
| Tanzania | 2016 | 2006 | 573 | 44.7657 | 0.531 | High HDI |
| Togo | 2014 | 690 | 273 | 34.49275 | 0.487 | Moderate HDI |
| Uganda | 2011 | 448 | 272 | 60.49107 | 0.493 | Moderate HDI |
| Zambia | 2014 | 2455 | 691 | 64.92872 | 0.579 | High HDI |
| Zimbabwe | 2015 | 1065 | 362 | 16.90141 | 0.516 | Moderate HDI |
*HDI = Human Development Index
Measurement of the prevalence of MOV, special and common cause variations
As shown in Figures 1 and 2, we found a wide variation in the missed opportunity for vaccination. It ranged from about 16% in Swaziland and Zimbabwe to as high as 89% in Gabon. From the funnel plot, we identified only 6 (17%) countries within the 99% control limits indicating common-cause variation. Fifteen (43%) countries were above the upper control limit (higher than the average) and 14 (40%) countries were below the lower control limit (lower than the average), indicating special-cause variation.
Figure 1.
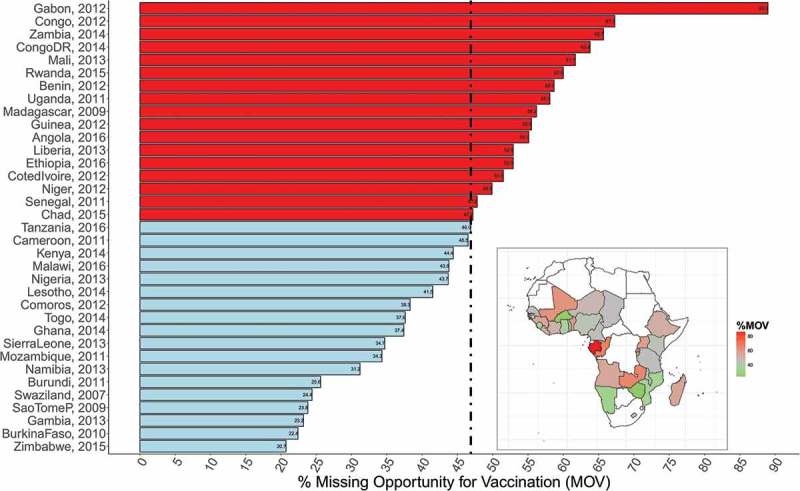
Percentage missed opportunities for vaccination, by countries.
Figure 2.
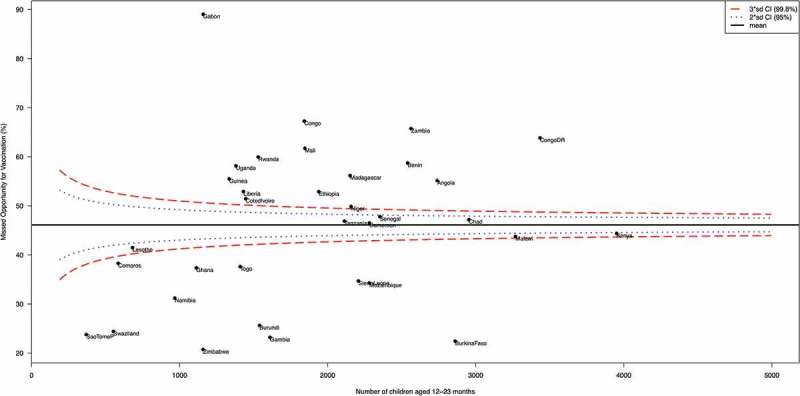
Funnel plot showing common- and special-cause variations in missed opportunities for vaccination in sub-Saharan Africa.
Measures of associations (fixed effects)
The results of different models are shown in Table 3. In the fully adjusted model controlling for the effects of individual, neighbourhood and country level factors, child’s age, birth order, number of under-five children, maternal age, wealth index, education attainment, media access and neighbourhood socio-economic disadvantage were significantly associated with odds of missed opportunity for vaccination.
Table 3.
Individual compositional and contextual factors associated with missed opportunities for vaccination in sub-Saharan Africa identified by multivariable multilevel logistic regression models.
| Model 1a | Model 2b | Model 3c | Model 4d | Model 5e | |
|---|---|---|---|---|---|
| Fixed-effect | OR (95% CrI) | OR (95% CrI) | OR (95% CrI) | OR (95% CrI) | |
| Individual-level factors | |||||
| Age | 0.98 (0.98, 0.99) | 0.98 (0.98, 0.99) | |||
| Male (vs female | 1.02 (0.97, 1.06) | 0.99 (0.95, 1.04) | |||
| Birth order (high vs low) | 1.18 (1.10, 1.25) | 1.16 (1.09, 1.24) | |||
| Number of under-five children | 1.05 (1.02, 1.07) | 1.04 (1.01, 1.05) | |||
| Maternal age | |||||
| 15–24 | 1 (reference) | 1 (reference) | |||
| 25–34 | 0.92 (0.87, 0.98) | 0.90 (0.86, 0.97) | |||
| 35–49 | 0.83 (0.76, 0.90) | 0.83 (0.76, 0.91) | |||
| Wealth | |||||
| poorest | 1.46 (1.33, 1.59) | 1.35 (1.21, 1.51) | |||
| poorer | 1.41 (1.30, 1.54) | 1.31 (1.19, 1.44) | |||
| middle | 1.31 (1.20, 1.42) | 1.24 (1.13, 1.36) | |||
| richer | 1.20 (1.11, 1.31) | 1.17 (1.07, 1.26) | |||
| Richest | 1 (reference) | 1 (reference) | |||
| Maternal education | |||||
| no education | 1.11 (1.02, 1.20) | 1.14 (1.05, 1.23) | |||
| primary | 1.25 (1.16, 1.34) | 1.28 (1.19, 1.36) | |||
| Secondary or higher | 1 (reference) | 1 (reference) | |||
| Not working | 0.97 (0.92, 1.03) | 0.94 (0.93, 1.04) | |||
| Media access | 0.95 (0.92, 0.98) | 0.96 (0.93, 0.99) | |||
| Neighbourhood factor | |||||
| Neighbourhood disadvantage | |||||
| Quintile 1 (least disadvantaged) | 1 (reference) | 1 (reference) | |||
| Quintile 2 | 1.43 (1.31, 1.55) | 1.23 (1.12, 1.33) | |||
| Quintile 3 | 1.52 (1.39, 1.67) | 1.28 (1.16, 1.39) | |||
| Quintile 4 | 1.60 (1.45, 1.75) | 1.22 (1.09, 1.35) | |||
| Quintile 5 (most disadvantaged) | 1.60 (1.45, 1.75) | 1.19 (1.06, 1.31) | |||
| Country-level factor | |||||
| Human Development Index | |||||
| Low HDI | 1 (reference) | 1 (reference) | |||
| Moderate HDI | 1.38 (0.52, 2.70) | 1.36 (0.71, 2.82) | |||
| High HDI | 1.04 (0.52, 1.57) | 1.34 (0.92, 1.91) | |||
| Random-effect | |||||
| Country-level | |||||
| Variance (95% CrI) | 0.97 (0.58, 1.58) | 0.88 (0.54, 1.42) | 0.92 (0.56, 1.48) | 0.94 (0.57, 1.55) | 0.90 (0.55, 1.48) |
| VPC (%, 95% CrI) | 18.4 (12.1, 26.5) | 17.1 (11.4, 24.6) | 17.7 (11.8, 25.2) | 18.0 (11.9, 26.1) | 17.4 (11.6, 25.4) |
| MOR (95% CrI) | 2.56 (2.07, 3.32) | 2.45 (2.02, 3.12) | 2.50 (2.04, 3.19) | 2.52 (2.05, 3.28) | 2.47 (2.03, 3.19) |
| Neighbourhood-level | |||||
| Variance (95% CrI) | 1.00 (0.93, 1.09) | 0.98 (0.90, 1.06) | 0.98 (0.89, 1.08) | 1.00 (0.91, 1.09) | 0.97 (0.89, 1.05) |
| VPC (%, 95% CrI) | 37.4 (31.4, 44.8) | 36.1 (30.4, 43.0) | 36.6 (30.6, 43.7) | 37.1 (31.0, 44.5) | 36.2 (30.4, 43.5) |
| MOR (95% CrI) | 2.60 (2.51, 2.71) | 2.57 (2.47, 2.67) | 2.57 (2.46, 2.69) | 2.60 (2.48, 2.71) | 2.56 (2.46, 2.66) |
| Model fit statistics | |||||
| DIC | 53,805 | 53,498 | 53,671 | 53,807 | 53,490 |
| Sample size | |||||
| Country-level | 35 | 35 | 35 | 35 | 35 |
| Neighbourhood-level | 15,246 | 15,121 | 15,123 | 15,123 | 15,121 |
| Individual-level | 43,937 | 43,631 | 43,637 | 43,637 | 43,631 |
aModel 1 – empty null model, baseline model without any explanatory variables (unconditional model)
bModel 2 – adjusted for only individual-level factors
cModel 3 – adjusted for only neighbourhood-level factors
dModel 4 – adjusted for only country-level factors
eModel 5 – adjusted for individual-, neighbourhood-, and country-level factors (full model)
OR – odds ratio, CrI – credible interval, MOR – median odds ratio, VPC – variance partition coefficient, DIC – Bayesian Deviance Information Criteria
For every one-month increase in child’s age, the odds of missing an opportunity for vaccination reduces by 2% (OR = 0.98, 95% CrI 0.98 to 0.99). Children with high birth order had a 16% increase in the odds of missing an opportunity for vaccination (OR = 1.16%, 95% CrI 1.09 to 1.24). For every increase in the number of under-five children in the household by one child, the odds of MOV increased by 4% (OR = 1.04, 95% CrI 1.01 to 1.05). The odds of MOV decreased with an increase in maternal age, such that mothers aged between 35 to 45 years were 17% less likely to have a child with MOV compared to those aged between 15 to 24 years (OR = 0.83, 95% CrI 0.76 to 0.91). Mothers from poorest households were 35% times more likely to have had a child with MOV than those from richest households (OR = 1.35, 95% CrI 1.21 to 1.51). In addition, mothers with no formal education had a 14% increase in the likelihood of having a child with MOV than those with secondary or higher education (OR = 1.14, 95% CrI 1.05 to 1.23). Mothers with access to media were 4% times less likely to have had a child with MOV (OR = 0.96, 95% CrI 0.93 to 0.99).
Children living in the most socioeconomic position (SEP) disadvantaged neighbourhood were 23% more likely to have MOV than those living in least SEP disadvantaged neighbourhood (OR = 1.23, 95% CrI 1.12 to 1.33).
Measures of variations (random effects)
As shown in Table 3, in Model 1 (unconditional model), there was a significant variation in the odds of MOV across the countries ( 0.97, 95% CrI 0.58 to 1.58) and across the neighbourhoods ( 1.00, 95% CrI 0.93 to 1.09). According to the intra-country and intra-neighbourhood correlation coefficient, 18.4% and 37.4%, the variance in odds of MOV could be attributed to country and neighbourhood level factors, respectively. Results from the median odds ratio (MOR) also confirmed evidence of neighbourhood and societal contextual phenomena shaping child MOV. From the full model (Model 5), it was estimated that if a child moved to another country or neighbourhood with a higher probability of MOV, the median increase in their odds of MOV would be 2.47 (95% CrI 2.03 to 3.19) and 2.56-fold (95% CrI 2.46 to 2.66) respectively.
Discussion
In our study, we found a wide variation of MOV, ranging from as high as 89% in Gabon to as low as 16% in Swaziland and Zimbabwe. After adjustment for individual, neighbourhood and country level factors, we observed that child’s age, birth order, number of under-five children, maternal age, wealth index, education attainment, media access and neighbourhood socio-economic disadvantage were significantly associated with odds of missed opportunity for vaccination. The odds of MOV also varied significantly across countries and neighbourhoods.
Children with high birth order were 16% times more likely to miss vaccination opportunities. This finding corresponds to what Verma and colleagues found in their study on high birth order as an important factor for missed opportunity for immunization.17 In the present study we also found sibship size in the household to be associated with the chance of being unimmunized. For every increase in under-five children in the household, the odds of remaining unimmunised increased. This suggest that children with high birth order and within a large sibship are more likely to be out of reach for health services. Our findings correlates with the WHO recent calls for the need of reaching the “fifth child” through outreach services based on the assumption that the 5th child has no access to the health services.18 The findings of this study are similar to those by Sridgar and colleagues who also report child’s age, maternal age and parental education as determinants of MOV.8 However, the review by Sridhar and colleagues included several studies with varied methods of data collection. We address this limitation by conducting a multilevel logistitic regression using DHS surveys whose methods are similar and comparable across various countries.
From the analysis of the socio-economic factors, we found that families from disadvantaged backgrounds were more likely to miss vaccination. For example, mothers with a low wealth quintile (from poorest households) were 35% more likely to have a child with MOV than those from richest households. In addition, mothers without a formal education were 14 times more likely to have a child with MOV than those with secondary or higher education. In addition, we observed that in relation to SEP, children living in most disadvantaged neighbourhood were 23% more likely to have MOV than those living in least SEP disadvantaged neighbourhoods.
It is not possible to infer causal inference due to cross-sectional nature of the data. In addition, the assest-based wealth index may not produce similar results to those from direct measure of household incomes.19,20 However, despite these limitations, the strengths are important. We harmonised large population-based data from 35 countries. The surveys were comparable and nationally representative, making the findings generalisable to the entire nation. In addition, the Bayesian approach we took provides more robust estimates and unbiased estimates for the factors associated with missed opportunity for vaccination.21,22
We found evidence of geographical clustering in missed opportunities for vaccination. About 18.4% and 37.4% of the variation in missed opportunities for vaccination is conditioned by differences between neighbourhoods and countries, respectively. If a child moved to another neighbourhood or another country with a higher probability of missed opportunities for vaccination, their odds of missed opportunities for vaccination may increase by about 147% and 156%, respectively. It is instinctual that people living from the same neighbourhood may be more similar to each other in relation to their attitudes and beliefs towards childhood vaccination than to others from other neighbourhoods. 23 Suggesting that the public health interventions should not only focus on high-risk children but also high-risk areas.
In conclusion, individual compositional and contextual measures of socioeconomic position were independently associated with missed opportunities for vaccination in sub-Saharan Africa, which underscores the need to implement interventions to improve child immunization update not only at the individual level taking into account socioeconomic position, but also at the contextual levels.
Methods
Study design and data
We used cross-sectional data from Demographic and Health Surveys (DHS), which are nationally representative household surveys conducted in sub-Saharan Africa. This study used data from 35 recent DHS surveys conducted between 2007 and 2016 available as of May 2018. The DHS uses a multi-stage, stratified sampling design with households as the sampling unit.24 Eligible women and men living in households were interviewed. The survey data are comparable across countries as all surveys instruments and procedures were implemented similarly.
Outcome variable
We used the World Health Organisation (WHO) definition of missed opportunity for vaccination (MOV) as the outcome variable, defined as a binary variable that takes the value of 1 if the child 12–23 months had any contact with health services but remained unavaccinated to any vaccine doses for which the child is eligible. Contact with health services were defined using the following six variables: skilled birth attendance, baby postnatal check within 2 months, received vitamin A dose in first 2 months after delivery, has health card and medical treatment of diarrhea/fever/cough.
Explanatory variables
Individual level factors
The following individual-level factors were included in the models: child’s age, sex of the child (male and female), high birth order (> 4 birth order), number of under five children in the household, maternal age (15 to 24, 25 to 34, 35 or older), employment status (working or not working), maternal education (no education, primary or secondary or higher), media access (radio, television or newspaper), and wealh index (poorest, poorer, middle, richer and richest).20,25
Neighbourhood-level factors
We considered neighbourhood socioeconomic disadvantage for the community-level variable in this study. Neighbourhood socioeconomic disadvantage was operationalized with a principal component comprised of the proportion of respondents with: no formal education, unemployed, rural resident, and living below the poverty level (asset index below 20% poorest quintile). A standardized score with mean 0 and standard deviation 1 was generated from this index; with higher scores indicative of lower socieo-economic position (SEP). We divided the resultants scores into quintiles.
Country level factors
Country level data were collected from the reports published by the United Nations Development Program.26 At country-level, we included human development index, a measure of country’s intensity of deprivation, which is the average percentage of deprivation experienced by people in multidimensional poverty. Like wealth index, intensity of deprivation was computed using principal components based on data on household deprivations in education, health and living standards, however, at the country-level26. The country-level variables were categorized into three tertiles (low, middle and high levels).
Statistical analyses
We used multivariable multilevel logistic regression models to analyse the association between individual, compositional and contextual factors associated with missed opportunity for vaccination. We specified a 3-level model for binary response reporting missed opportunity for vaccination or not, for a child (at level 1), in a neighbourhood (at level 2) living in a country (at level 3) (see Figure 3). Five different models were developed. First, was the unconditional or empty model without any determinant variables. The aim of this model was to decompose the amount of variance in odds of missed opportunity vaccination between countries and neighbourhoods. Model 2 included only individual-level factor, model 3 included only neighbourhood-level factors, and model 4 included only the country-level factors. The fifth model, included all individual-, neighbourhood- and country-level factors simulteneously.
Figure 3.
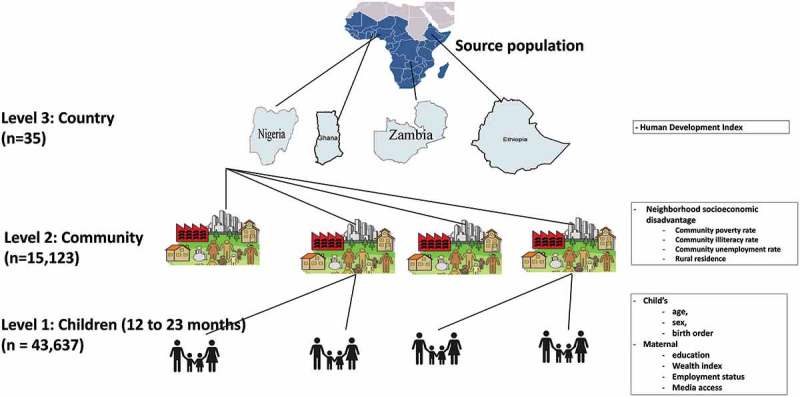
Multilevel data structure.
We reported the measures of association as odds ratios (ORs) with their 95% credible intervals (CrIs).
Measures of variations were explored using the intraclass correlation (ICC) and median odds ratio (MOR) 27,28. The ICC represents the percentage of the total variance in the odds of missed opportunities for vaccination that is related to the neighbourhood and country level, i.e. measure of clustering of odds of missed opportunities for vaccination in the same neighbourhood and country. MOR estimates the probability of missed opportunities for vaccination that can be attributed to neighbourhood and country context.
Multilevel analysis was performed using the MLwinN software, version 2.3129,30 using the Bayesian Markov Chain Monte Carlo procedure.29
Common and special cause variations
We generated scatter plots of performance, as a percentage, against the number of missed opportunities for vaccination children (the denominator for the percentage). The mean country performance and exact binomial 3 sigma limits were calculated for all possible values for the number of cases and used to create a funnel plot using the method described by Spiegelhalter.31,32 If a state lies with the 99% CI, it has crude missed opportunities for vaccination rate that is statistically consistent with the average rate (common-cause variation). If a country lies outside the 99% CI, then it has crude missed opportunities for vaccination rate that is statistically different from the average rate (special-cause variation).
Biography
OAU and CSY conceived the study. OAU and CSY obtained funding for the study. OAU collected and analysed initial data. AA, ABW, CSY, DN, EZS, ABW and OAU participated in refining the data analysis. OAU and DN wrote the first manuscript. AA, ABW, CSY, DN, EZS, GB, JO, OAU, TO and SY contributed to further analysis, interpreting and shaping of the argument of the manuscript and participated in writing the final draft of the manuscript. All the authors read and approved the final manuscript.
Funding Statement
This paper presents independent research supported wholly by the National Research Foundation of South Africa (Grant Number: 106035).
Acknowledgments
The authors are grateful to DHS Program for providing them with the survey data. Olalekan Uthman is supported by the National Institute for Health Research using Official Development Assistance (ODA) funding. The views expressed in this publication are those of the author(s) and not necessarily those of the NHS, the National Institute for Health Research and Social Care.
Disclosure of potential conflicts of interest
No potential conflicts of interest were disclosed.
Consent for publication
Not applicable.
References
- 1.Bloom DE. The value of vaccination. Adv Exp Med Biol. 2011;697:1–8. [published Online First: 2010/12/02]. doi: 10.1007/978-1-4419-7185-2_1. [DOI] [PubMed] [Google Scholar]
- 2.Wiysonge CS, Nomo E, Mawo JN, Ticha JM. Accelerated measles control in sub-Saharan Africa. Lancet. 2006;367(9508):394–395. [published Online First: 2006/02/07]. doi: 10.1016/s0140-6736(06)68133-6. [DOI] [PubMed] [Google Scholar]
- 3.Collaborators GBDM Global, regional, and national under-5 mortality, adult mortality, age-specific mortality, and life expectancy, 1970-2016: a systematic analysis for the global burden of disease study 2016. Lancet. 2017;390(10100):1084–1150. [published Online First: 2017/09/19] doi: 10.1016/S0140-6736(17)31833-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Andre FE, Booy R, Bock HL, Clemens J, Datta SK, John TJ, Lee BW, Lolekha S, Peltola H, Ruff TA, et al. Vaccination greatly reduces disease, disability, death and inequity worldwide. Bull World Health Organ. 2008;86(2):140–146. [published Online First: 2008/02/26]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Favin M, Steinglass R, Fields R, Banerjee K, Sawhney M. Why children are not vaccinated: a review of the grey literature. Int Health. 2012;4(4):229–238. [published Online First: 2013/09/14]. doi: 10.1016/j.inhe.2012.07.004. [DOI] [PubMed] [Google Scholar]
- 6.World Health Organization Missed Opportunities for Vaccination (MOV) Strategy 2018 [9 January 2018]. Available from: http://www.who.int/immunization/programmes_systems/policies_strategies/MOV/en/.
- 7.Hutchins SS, Jansen HA, Robertson SE, Evans P, Kim-Farley RJ. Studies of missed opportunities for immunization in developing and industrialized countries. Bull World Health Organ. 1993;71(5):549–560. [published Online First: 1993/01/01]. [PMC free article] [PubMed] [Google Scholar]
- 8.Sridhar S, Maleq N, Guillermet E, Colombini A, Gessner BD. A systematic literature review of missed opportunities for immunization in low- and middle-income countries. Vaccine. 2014;32(51):6870–6879. [published Online First: 2014/12/03]. doi: 10.1016/j.vaccine.2014.10.063. [DOI] [PubMed] [Google Scholar]
- 9.Okwo-Bele JM, Cherian T. The expanded programme on immunization: a lasting legacy of smallpox eradication. Vaccine. 2011;29(Suppl 4):D74–9. [published Online First: 2012/04/18]. doi: 10.1016/j.vaccine.2012.01.080. [DOI] [PubMed] [Google Scholar]
- 10.World Health Organization Immunization coverage 2018 [9 January 2018]. Available from: http://www.who.int/mediacentre/factsheets/fs378/en/.
- 11.Ushie BA, Fayehun OA, Ugal DB. Trends and patterns of under-5 vaccination in Nigeria, 1990-2008: what manner of progress? Child Care Health Dev. 2014;40(2):267–274. [published Online First: 2013/04/12]. doi: 10.1111/cch.12055. [DOI] [PubMed] [Google Scholar]
- 12.Jung M, Lin L, Viswanath K. Effect of media use on mothers’ vaccination of their children in sub-Saharan Africa. Vaccine. 2015;33(22):2551–2557. [published Online First: 2015/04/22]. doi: 10.1016/j.vaccine.2015.04.021. [DOI] [PubMed] [Google Scholar]
- 13.Restrepo-Mendez MC, Barros AJ, Wong KL, Johnson HL, Pariyo G, França GV, Wehrmeister FC, Victora CG. Inequalities in full immunization coverage: trends in low- and middle-income countries. Bull World Health Organ. 2016;94(11):794–805b. [published Online First: 2016/11/09]. doi: 10.2471/blt.15.162172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Olorunsaiye CZ, Langhamer MS, Wallace AS, Watkins ML. Missed opportunities and barriers for vaccination: a descriptive analysis of private and public health facilities in four African countries. Pan Afr Med J. 2017;27(Suppl3):6 [published Online First: 2018/01/04]. doi: 10.11604/pamj.supp.2017.27.3.12083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fink DS, Keyes KM, Cerda M. Social determinants of population health: A systems sciences approach. Curr Epidemiol Rep. 2016;3(1):98–105. [published Online First: 2016/09/20]. doi: 10.1007/s40471-016-0066-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Diez Roux AV. A glossary for multilevel analysis. J Epidemiol Community Health. 2002;56(8):588–594. [published Online First: 2002/07/16]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Verma SK, Mourya HK, Yadav A, Mourya S, Dabi DR. Assessment of missed opportunities of immunization in children visiting health facility. Int J Contemp Pediatrics. 2017;4(5):1748–1753. doi: 10.18203/2349-3291.ijcp20173778. [DOI] [Google Scholar]
- 18.WHO, UNICEF, World Bank State of the world’s vaccines and immunization. 3rd ed. Geneva (Switzerland): World Health Organization; 2009. [Accessed January 11, 2018]. Available at: http://apps.who.int/iris/bitstream/10665/44169/1/9789241563864_eng.pdf. [Google Scholar]
- 19.Filmer D, Pritchett LH. Estimating wealth effects without expenditure data–or tears: an application to educational enrollments in states of India. Demography. 2001;38(1):115–132. [DOI] [PubMed] [Google Scholar]
- 20.Montgomery MR, Gragnolati M, Burke KA, Paredes E. Measuring living standards with proxy variables. Demography. 2000;37(2):155–174. [PubMed] [Google Scholar]
- 21.Browne WJ, Draper D. A comparison of Bayesian and likelihood-based methods for fitting multilevel models. Bayesian Analysis 2006;473–514. doi: 10.1214/06-BA117. [DOI] [Google Scholar]
- 22.Stegmueller D. How many countries for multilevel modeling? A comparison of frequentist and bayesian approaches. Am J Pol Sci. 2013;57(3):748–761. doi: 10.1111/ajps.12001. [DOI] [Google Scholar]
- 23.Merlo J, Chaix B, Yang M, Lynch J, Råstam L. A brief conceptual tutorial of multilevel analysis in social epidemiology: linking the statistical concept of clustering to the idea of contextual phenomenon. J Epidemiol Community Health. 2005;59(6):443–449. doi: 10.1136/jech.2004.023473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rutstein SO, Rojas G. Guide to DHS statistics: demographic and health surveys methodology. Calverton (Maryland): ORC Macro; 2006. [Google Scholar]
- 25.Vyas S, Kumaranayake L. Constructing socio-economic status indices: how to use principal components analysis. Health Policy Plan. 2006;21(6):459–468. [published Online First: 2006/10/13]. doi: 10.1093/heapol/czl029. [DOI] [PubMed] [Google Scholar]
- 26.United Nations Development Programme Human development report 2014. Sustaining human progress: reducing vulnerabilities and building resilience. NY (USA): United Nations Development Programme; 2014. [Google Scholar]
- 27.Snijders T, Bosker R. multilevel analysis – an introduction to basic and advanced multilevel modelling. Thousand Oaks (California): SAGE publications; 1999. [Google Scholar]
- 28.Larsen K, Merlo J. Appropriate assessment of neighborhood effects on individual health: integrating random and fixed effects in multilevel logistic regression. Am J Epidemiol. 2005;161(1):81–88. doi: 10.1093/aje/kwi017. [DOI] [PubMed] [Google Scholar]
- 29.Browne WJ. MCMC Estimation in MLwiN v2.31. UK: University of Bristol: Centre for Multilevel Modelling; 2014. [Google Scholar]
- 30.Rasbash J, Charlton C, Browne WJ, et al. MLwiN Version 2.31. UK: University of Bristol: Centre for Multilevel Modelling; 2014. [Google Scholar]
- 31.Spiegelhalter D. Funnel plots for institutional comparison. Qual Saf Health Care. 2002;11(4):390–391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Spiegelhalter DJ. Funnel plots for comparing institutional performance. Stat Med. 2005;24(8):1185–1202. doi: 10.1002/sim.1970. [DOI] [PubMed] [Google Scholar]


