ABSTRACT
We examined the roles of determining factors responsible for acute respiratory infections and diarrhoea among immunised human immunodeficiency virus (HIV)-exposed children in sub-Saharan Africa. This study used demographic and health surveys obtained from 27 sub-Saharan African countries. The outcome variable is defined as symptoms of acute respiratory infections or episode of diarrhoea in the child of an HIV-infected mother who is vaccinated with the third dose of diphtheria-tetanus-pertussis containing vaccines. Multivariable logistic regression models were used to analyse the association between individual and contextual factors. The odds of developing symptoms of acute respiratory infections increased among those living in communities with high unemployment rate (Odds ratio = 1.15, 95% credible interval 1.05 to 1.26). The odds of developing diarrhoea increased among young mothers such that children of women aged 15–24 years were two times likely to develop diarrhoea compared to children of women aged 35–49 years (Odds ratio = 2.22, 95% credible interval 1.66 to 2.93). Public healthcare programmes should target adolescent and young women, and their family members on how to prevent diarrhoea. Efforts should be made to identify the hotspots for development of acute respiratory diseases especially in communities with high rate of unemployment and to develop strategies to combat the diseases in such communities. Initiatives such as the integrated Global Action Plan for the Prevention and Control of Pneumonia and Diarrhoea which recommends an interrelated approach for the elimination of preventable diarrhoea and pneumonia deaths should be adopted.
Keywords: acute respiratory infections, diarrhoea, HIV, sub-Saharan Africa, demographic and health surveys, multilevel analysis
Background
Acute diarrhoea disease and pneumonia are major causes of morbidity and mortality among children especially among the human immunodeficiency virus (HIV)-exposed and infected ones.1 Acute respiratory infections and diarrhoeal diseases are mostly caused by vaccine-preventable diseases and these diseases are avoidable particularly if children are properly immunised.1,2 In addition to diarrhoea and pneumonia, HIV still contributes substantially to children mortality especially in Africa and South East Asia which incidentally are regions with high burden of HIV.3,4
Immunisation programmes has proven to be a successful and cost-effective global public health interventions.5,6 Expanded Program on Immunization (EPI) has led to considerable decline in the morbidity and mortality attributed to vaccine-preventable diseases.7 Global Alliance for Vaccines and Immunisation (GAVI) initiatives has been recording reduction in childhood morbidity and mortality secondary to vaccine-preventable diseases among supported countries primarily as a result of vaccines use.2 More diseases and deaths could still be averted if there is an improvement in the global vaccination coverage.2 Africa accounts for a substantial proportion of the global vaccine-preventable diseases burden and for the highest proportion of under-five years of age mortality from these diseases.8,9 Meanwhile, only 74% of the World Health Organization (WHO) African member states achieved ≥ 90% national coverage for the three doses of diphtheria-tetanus-pertussis vaccines (DTP3) as at 2016.10
Understanding the association between HIV status, uptake of childhood vaccination, acute respiratory infections and diarrhoeal diseases is of great importance in countries with high HIV prevalence especially in sub-Saharan African region. Despite the high prevalence of HIV in many African countries, HIV testing is still not optimal. The knowledge of status among all people living with HIV ranged between 29–87%. There is lack of information on socio-economic factors such as employment status, education status, mother’s age, wealth index and residence which are the likely determinants of morbidities like acute respiratory infections, diarrhoeal diseases, fever etc. among the immunised children of HIV-positive mothers. Adequate knowledge of these determining factors is very crucial in making recommendations concerning public health interventions for prevention of acute respiratory infections and diarrhoeal diseases among immunised and HIV exposed children.
DTP3 is a key indicator used by international and national organisations such as United Nations Children’s Fund (UNICEF) and WHO for assessing the effectiveness of childhood immunisation services.11 The series of immunisations known as DTP can prevent diphtheria, pertussis (whooping cough) and tetanus, but these three diseases still kill 600,000 children and afflict millions of others every year in developing countries. The percentage of children receiving the final dose (DTP3) is therefore a revealing and vital gauge of how well countries are providing immunisation coverage for their children.11 To be fully protected, DTP-containing vaccines are normally given in three doses at the age of 6, 10 and 14 weeks with three booster doses at 12–23 months, 4–7 years and 9–15 years. Diphtheria toxoid-containing vaccines are given to the older children as booster vaccine.12
We examined the roles of the socio-economic factors in relation to uptake of DTP3 vaccines among HIV-exposed children. A multilevel study was designed to assess the independent contributions of individual, community, and country-level socio-economic factors. We also developed and tested model for the determinants as they relate to non-uptake of DTP3 vaccines among HIV-exposed children (Figure 1).
Figure 1.
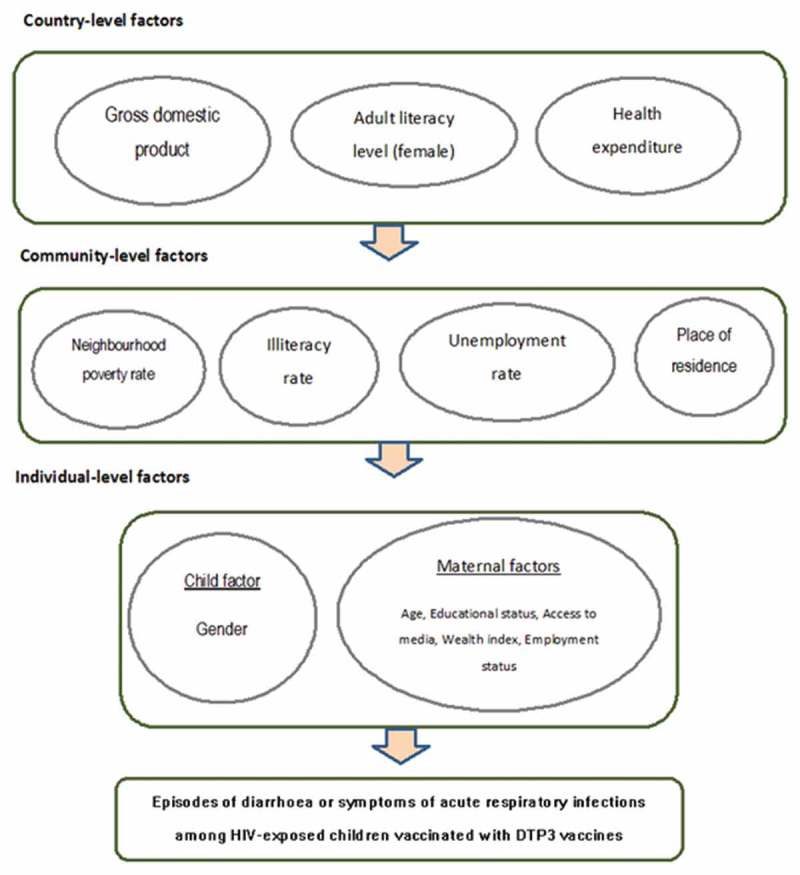
Conceptual framework showing the factors determining episodes of diarrhoea or symptoms of acute respiratory infections among HIV-exposed children vaccinated with DTP3 vaccines.
Results
Sample characteristics
The country surveys were conducted between 2003 and 2016 in the included countries (Table 1). Adult literacy rate in the included countries ranged from 15.5% in Niger to 90.1% in Sao Tome and Principe. The health expenditure per capita ranged from US$19.1 in Niger to US$321.3 in Gabon. Gross domestic product (GDP) per capita data shows that Gabon and Namibia are the upper middle-income countries while eight other countries namely; Angola, Cameroun, Cote d’Ivoire, Ghana, Kenya, Senegal, Swaziland and Zambia are lower middle-income countries and the rest are low-income countries.
Table 1.
Year of DHS survey and country level characteristics of 27 study countries in sub-Saharan Africa.
| Country | Year of survey | GDP per capita | Adult literacy rate | Health expenditure |
|---|---|---|---|---|
| Angola | 2016 | 3110.8 | 66 | 179.4 |
| Burkina Faso | 2010 | 649.7 | 34.6 | 35.2 |
| Burundi | 2011 | 285.7 | 61.6 | 21.6 |
| Cameroon | 2011 | 1032.6 | 71.3 | 58.7 |
| Chad | 2015 | 664.3 | 22.3 | 37.1 |
| Congo DR | 2014 | 444.5 | 77 | 19.1 |
| Cote d’Ivoire | 2012 | 1526.2 | 43.9 | 88.4 |
| Ethiopia | 2003 | 706.8 | 39 | 26.6 |
| Gabon | 2012 | 7179.3 | 82.3 | 321.3 |
| Gambia | 2013 | 473.2 | 42 | 30.7 |
| Ghana | 2014 | 1513.5 | 71.5 | 57.9 |
| Guinea | 2012 | 508.1 | 32 | 37.3 |
| Kenya | 2009 | 1455.4 | 78.7 | 77.7 |
| Lesotho | 2014 | 998.1 | 76.6 | 105.1 |
| Liberia | 2013 | 455.4 | 42.9 | 46.3 |
| Malawi | 2016 | 300.8 | 62.1 | 29 |
| Mali | 2013 | 780.5 | 33.1 | 47.8 |
| Namibia | 2012 | 4140.5 | 88.3 | 499 |
| Niger | 2013 | 363.2 | 15.5 | 24.4 |
| Rwanda | 2015 | 702.8 | 68.3 | 52.5 |
| Sao T&P | 2009 | 1756.1 | 90.1 | 165.6 |
| Senegal | 2011 | 958.1 | 42.8 | 49.5 |
| Sierra Leone | 2013 | 496 | 32.4 | 85.9 |
| Swaziland | 2007 | 2775.2 | 83.1 | 247.9 |
| Togo | 2014 | 578.5 | 63.8 | 33.9 |
| Zambia | 2014 | 1178.4 | 83 | 85.9 |
| Zimbabwe | 2015 | 1008.6 | 88.7 | 57.7 |
GDP: gross domestic product, HDI: human development index, n/a: not available)
GDP – Low-income economies are defined as those with a GDP per capita of $1,025 or less; lower middle-income economies: $1,026 – $4,035; upper middle-income economies: $4,036 – $12,475;
high-income economies: ≥ $12,476. HDI – low: < 0.549; medium: 0.550 – 0.770.
(Source: Demographic and Health Surveys, World Bank, Joint United Nations Programme on HIV/AIDS, United Nations Development Programme)
Table 2 shows the summary of symptoms of acute respiratory infections and episodes of diarrhoea among the children of HIV-positive mothers vaccinated with DTP3 at different levels in this study. For the summary of symptoms of acute respiratory infections, a total of 1,482 children aged 12–23 months (Level 1), within 1076 communities (Level 2), from 26 countries (Level 3) in sub-Saharan Africa were included. For the episodes of diarrhoea, a total of 4,027 children aged 12–23 months (Level 1), within 2267 communities (Level 2), from 27 countries (Level 3) in sub-Saharan Africa. Male and female children of HIV-infected women were evenly distributed. An estimated half of the included mothers were aged between 25 and 34 years, about three-fifth were not employed and two-fifth were in the richer wealth index group. Most of the respondents were living in rural areas, within low poverty rate and low illiteracy rate group.
Table 2.
Summary of symptoms of acute respiratory infections and episodes of diarrhoea among the children of HIV-positive mothers with DTP3 uptake at different levels.
| Symptoms of acute respiratory infections |
Episodes of diarrhoea |
|||||
|---|---|---|---|---|---|---|
| Variables | No | Yes | p-value | No | Yes | p-value |
| Individual-level factors | ||||||
| Gender | ||||||
| Female | 533 (50.6) | 196 (45.9) | 0.104 | 1,663 (49.4) | 324 (49.0) | 0.855 |
| Male | 521 (49.4) | 231 (54.1) | 1,703 (50.6) | 337 (51.0) | ||
| Age (in years) | ||||||
| 15–24 | 269 (25.5) | 115 (26.9) | 0.592 | 751 (22.3) | 197 (29.8) | 0.000 |
| 25–34 | 512 (48.6) | 212 (49.7) | 1,706 (50.7) | 333 (50.4) | ||
| 35–49 | 273 (25.9) | 100 (23.4) | 909 (27.0) | 131 (19.8) | ||
| Education | ||||||
| No education | 74 (7.0) | 62 (14.5) | 0.000 | 451 (13.4) | 78 (11.8) | 0.072 |
| Primary | 479 (45.5) | 175 (41.0) | 1,448 (43.0) | 316 (47.8) | ||
| Secondary+ | 501 (47.5) | 190 (44.5) | 1,467 (43.6) | 267 (40.4) | ||
| Employment status | ||||||
| Unemployed | 636 (60.3) | 270 (63.2) | 0.301 | 2,115 (62.8) | 425 (64.3) | 0.476 |
| Employed | 418 (39.7) | 157 (36.8) | 1,251 (37.2) | 236 (35.7) | ||
| Wealth index | ||||||
| Poorer | 325 (30.8) | 126 (29.5) | 0.842 | 893 (26.5) | 197 (29.8) | 0.165 |
| Middle | 305 (28.9) | 129 (30.2) | 996 (29.6) | 196 (29.7) | ||
| Richer | 424 (40.3) | 172 (40.3) | 1,477 (43.9) | 268 (40.5) | ||
| Access to media | ||||||
| Nil | 298 (28.3) | 92 (21.5) | 0.035 | 715 (21.3) | 162 (24.5) | 0.195 |
| Access to 1 outlet | 309 (29.3) | 139 (32.6) | 1,041 (30.9) | 290 (31.6) | ||
| Access to 2 outlets | 289 (27.4) | 117 (27.4) | 991 (29.4) | 181 (27.4) | ||
| Access to all outlets | 158 (15.0) | 96 (18.5) | 619 (18.4) | 109 (16.5) | ||
| Community-level factors | ||||||
| Place of residence | ||||||
| Urban | 444 (42.1) | 166 (38.9) | 0.250 | 1,494 (44.4) | 283 (42.8) | 0.457 |
| Rural | 610 (57.9) | 261 (61.1) | 1,872 (55.6) | 378 (57.2) | ||
| Poverty rate | ||||||
| Low | 625 (59.3) | 258 (60.4) | 0.690 | 2,103 (62.5) | 391 (59.2) | 0.107 |
| High | 429 (40.7) | 169 (39.6) | 1,263 (37.5) | 270 (40.8) | ||
| Unemployment rate | ||||||
| Low | 526 (49.9) | 194 (45.4) | 0.119 | 1,723 (51.2) | 329 (49.8) | 0.506 |
| High | 528 (50.1) | 233 (54.6) | 1,643 (48.8) | 332 (50.2) | ||
| Illiteracy rate | ||||||
| Low | 744 (70.6) | 271 (63.5) | 0.008 | 2,264 (67.3) | 424 (64.2) | 0.120 |
| High | 310 (29.4) | 156 (36.5) | 1,102 (32.7) | 237 (35.8) | ||
Acute respiratory infections
Measures of associations (fixed effects)
Table 3 shows the multilevel multivariate logistics regression models of the factors associated with symptoms of acute respiratory infections by children of HIV-infected women. At the community-level, the odds of developing symptoms of acute respiratory infections increased among those living in communities with high unemployment rate such that the children were 15% more likely to develop acute respiratory infections (odds ratio [OR] = 1.15, 95% credible interval [CrI] 1.05 to 1.26).
Table 3.
Factors associated with symptoms of acute respiratory infections by children of HIV-infected women identified by multilevel multivariate logistics regression models.
| Model 1a |
Model 2b |
Model 3c |
Model 4d |
Model 5e |
|
|---|---|---|---|---|---|
| OR (95% Crl) | OR (95% Crl) | OR (95% Crl) | OR (95% Crl) | OR (95% Crl) | |
| Fixed-effect | |||||
| Individual-effect factors | |||||
| Male (vs female) | 1.23 (0.95 −1.58) | 1.22 (0.94 – 1.57) | |||
| Mother’s age(in years) | |||||
| 35–49 | 1 (reference) | 1 (reference) | |||
| 25–34 | 1.18 (0.86 – 1.58) | 1.19 (0.86 – 1.59) | |||
| 15–24 | 1.11 (0.76 – 1.54) | 1.11 (0.75 – 1.58) | |||
| Wealth index | |||||
| Richer | 1 (reference) | 1 (reference) | |||
| Middle | 1.10 (0.78 – 1.50) | 1.00 (0.67 – 1.40) | |||
| Poorer | 1.04 (0.71 – 1.48) | 0.94 (0.56 – 1.43) | |||
| Education | |||||
| Secondary+ | 1 (reference) | 1 (reference) | |||
| Primary | 0.84 (0.62– 1.11) | 0.83 (0.61 – 1.11) | |||
| No education | 1.55 (0.95 – 2.37) | 1.52 (0.88 – 2.43) | |||
| Not employment | 1.02 (0.77 – 1.35) | 0.84 (0.60 – 1.15) | |||
| Access to media | 1.02 (0.88 – 1.18) | 1.01 (0.88 – 1.19) | |||
| Community-level factors | |||||
| Rural (vs urban) | 1.26 (0.88 – 1.77) | 1.35 (0.91 – 2.00) | |||
| High (vs low) poverty rate | 0.98 (0.87 – 1.10) | 0.99 (0.87 – 1.12) | |||
| High (vs low) unemployment rate | 1.15 (1.05 – 1.26)* | 1.17 (1.05 – 1.30)* | |||
| High (vs low) illiteracy rate | 1.01 (0.93 – 1.10) | 0.98 (0.89 – 1.08) | |||
| Country-level factors | |||||
| Middle (vs low) GDP | 1.16 (0.40 – 2.52) | 1.15 (0.36 – 2.90) | |||
| High (vs low) Adult literacy rate | 0.68 (0.27 – 1.37) | 0.64 (0.21 – 1.44) | |||
| Average (vs low) Health expenditure | 1.06 (0.28 – 3.11) | 1.23 (0.24 – 3.19) | |||
| Random effects | |||||
| Country-level | |||||
| Variance (95 Crl) | 0.763 (0.359 – 1.514) | 0.734 (0.341 – 1.460) | 0.788 (0.359 – 1.578) | 0.830 (0.363 – 1.691) | 0.871 (0.378 – 1.792) |
| ICC (%) | 18.81 | 18.21 | 19.27 | 20.13 | 20.92 |
| MOR ((%, 95% Crl) | 2.29 | 2.26 | 2.32 | 2.38 | 2.43 |
| Explained variation (%) | Reference | 3.7 | −3.3 | −8.8 | −14.2 |
| Community-level | |||||
| Variance (95 Crl) | 0.002 (0.001 – 0.006) | 0.008 (0.002 – 0.017) | 0.012 (0.001–0.416) | 0.001 (0.000 – 0.004) | 0.003 (0.001 – 0.009) |
| ICC (%) | 18.85 | 18.42 | 19.56 | 20.16 | 21.00 |
| MOR ((%, 95% Crl) | 1.04 | 1.09 | 1.11 | 1.03 | 1.05 |
| Explained variation (%) | Reference | −380.2 | −566.0 | 26.6 | −79.4 |
| Model fit statistics | |||||
| DIC | 1550 | 1529 | 1548 | 1551 | 1556 |
ICC – intra-cluster correlation; MOR – median odds ratio; OR- odds ratio; CrI – credible interval.
aModel 1 is null model, baseline model without any determinant variable. bModel 2 is additionally adjusted for individual-level factors.
cModel 3 is additionally adjusted for community-level factors. dModel 4 is additionally adjusted for country-level factors.
eModel 5 is additionally adjusted for individual-, community-, and country-level factors
Measures of variations (random effects)
In model 1 (unconditional model), there was a significant variation in the odds of developing symptoms of acute respiratory infections among the children of HIV-infected mothers across the countries (σ2 = 0.763, 95% CrI 0.359 to 1.514) and across the communities (σ2 = 0.002, 95% CrI 0.001 – 0.006) (as shown in Table 3). The intra-country and intra-community correlation coefficients show that 18.81% and 18.85% of the variance in odds of developing symptoms of acute respiratory infections are linked to country- and community-level factors respectively. From the full model (Model 5), it is assumed that a child who moved to another country or community with a higher probability of developing symptoms of acute respiratory infections, the median increase in the odds of developing symptoms of acute respiratory infections would be 20.92% and 21.00% respectively.
Episodes of diarrhoea
Measures of associations (fixed effects)
Table 4 shows the multilevel multivariate logistics regression models of the factors associated with episodes of diarrhoea by children of HIV-infected women. At the individual level, the odds of developing diarrhoea increased among young mothers such that children of women aged 15–24 years were two times likely to develop diarrhoea compared to children of women aged 35–49 years (OR = 2.22, 95% Crl 1.66 to 2.93).
Table 4.
Factors associated with episodes of diarrhoea by children of HIV-infected women identified by multilevel multivariate logistics regression models.
| Model 1a |
Model 2b |
Model 3c |
Model 4d |
Model 5e |
|
|---|---|---|---|---|---|
| OR (95% Crl) | OR (95% Crl) | OR (95% Crl) | OR (95% Crl) | OR (95% Crl) | |
| Fixed-effect | |||||
| Individual-effect factors | |||||
| Male (vs female) | 1.00 (0.83 −1.20) | 1.01 (0.83 – 1.22) | |||
| Mother’s age (in years) | |||||
| 35–49 | 1 (reference) | 1 (reference) | |||
| 25–34 | 1.52 (1.15 – 1.95)* | 1.58 (1.23 – 2.02)* | |||
| 15–24 | 2.13 (1.57 – 2.80)* | 2.22 (1.66 – 2.93)* | |||
| Wealth index | |||||
| Richer | 1 (reference) | 1 (reference) | |||
| Middle | 1.05 (0.80 – 1.32) | 1.04 (0.77 – 1.38) | |||
| Poorer | 1.20 (0.90 – 1.58) | 1.17 (0.82 – 1.66) | |||
| Education | |||||
| Secondary+ | 1 (reference) | 1 (reference) | |||
| Primary | 1.24 (0.98 – 1.57) | 1.27 (0.98 – 1.57) | |||
| No education | 0.94 (0.63 – 1.32) | 0.90 (0.58 – 1.28) | |||
| Not employment | 0.82 (0.66 – 1.00) | 0.82 (0.65 – 1.03) | |||
| Access to media | 0.97 (0.87 – 1.08) | 1.00 (0.88 – 1.11) | |||
| Community-level factors | |||||
| Rural (vs urban) | 0.96 (0.73 – 1.24) | 0.96 (0.69 – 1.29) | |||
| High (vs low) poverty rate | 1.05 (0.96 – 1.15) | 1.02 (0.92 – 1.14) | |||
| High (vs low) unemployment rate | 0.98 (0.91 – 1.06) | 1.00 (0.93 – 1.09) | |||
| High (vs low) illiteracy rate | 1.04 (0.97 – 1.13) | 1.06 (0.98 – 1.15) | |||
| Country-level factors | |||||
| Middle (vs low) GDP | 0.91 (0.61 – 1.35) | 0.89 (0.44 – 1.69) | |||
| High (vs low) Adult literacy rate | 1.29 (0.86 – 1.92) | 1.32 (0.62 – 2.58) | |||
| Average (vs low) Health expenditure | 0.68 (0.42 – 1.08) | 0.69 (0.34 – 1.27) | |||
| Random effects | |||||
| Country-level | |||||
| Variance (95 Crl) | 0.223 (0.058 – 0.532) | 0.241 (0.072 – 0.566) | 0.229 (0.056 – 0.556) | 0.083 (−0.010– 0.178) | 0.253 (0.039 – 0.673) |
| ICC (%) | 5.23 | 5.57 | 2.16 | 5.37 | 5.63 |
| MOR ((%, 95% Crl) | 1.57 | 1.59 | 1.32 | 1.58 | 1.61 |
| Explained variation (%) | Reference | −8.3 | 62.4 | −4.4 | −13.5 |
| Community-level | |||||
| Variance (95 Crl) | 0.744 (0.302 – 1.273) | 0.801 (0.437 – 0.122) | 0.846 (0.510–1.246) | 0.501 (0.251– 0.751) | 0.947 (0.494 – 1.432) |
| ICC (%) | 22.71 | 24.06 | 15.09 | 24.03 | 26.73 |
| MOR ((%, 95% Crl) | 2.27 | 2.34 | 1.96 | 2.35 | 2.52 |
| Explained variation (%) | Reference | −7.7 | 32.7 | −8.6 | −27.3 |
| Model fit statistics | |||||
| DIC | 3501 | 3534 | 3494 | 3495 | 3470 |
ICC – intra-cluster correlation; MOR – median odds ratio; OR- odds ratio; CrI – credible interval.
aModel 1 is null model, baseline model without any determinant variable. bModel 2 is additionally adjusted for individual-level factors. cModel 3 is additionally adjusted for community-level factors. dModel 4 is additionally adjusted for country-level factors.
eModel 5 is additionally adjusted for individual-, community-, and country-level factors
Measures of variations (random effects)
In model 1, there was a significant variation in the odds of developing diarrhoea among the children of HIV-infected mothers across the countries (σ2 = 0.223, 95% CrI 0.058 to 0.532) and across the communities (σ2 = 0.744, 95% CrI 0.302– 1.273) (as shown in Table 4). The intra-country and intra-community correlation coefficients show that 5.23% and 22.71% of the variance in odds of developing diarrhoea are linked to country- and community-level factors respectively. The variance in odds of not developing diarrhoea were also attributable to the country- and community-level factors respectively. From the full model (Model 5), it is assumed that a child who moved to another country or community with a higher probability of developing diarrhoea, the median increase in the odds of developing diarrhoea would be 5.63% and 26.73% respectively.
Discussion
Main findings
This study shows that the individual, community and country contexts are significant in explaining the variations in acute respiratory infections and diarrhoea among the children of HIV-infected mothers in the selected sub-Saharan African countries. Developing symptoms of acute respiratory infections is more likely in the children of HIV-infected women who live in communities with high unemployment rate. Our findings show that children of young HIV-infected women are more likely to develop diarrhoea than the children of older women in sub-Saharan African countries.
Communities with high unemployment rates have the characteristics of poor neighbourhood such as poor housing, limited access to public services like healthcare, transportation etc.13 High unemployment communities are linked with lower socioeconomic status and are characterised by crowded rooms, poor nutrition, poor sanitation and hygienic conditions.14 Women living with HIV in these communities more or less belong to the lower socioeconomic status.15 Deprived neighbourhoods with high unemployment rate are associated with increased risk of mortality.16 Cohen also shows that unemployment status is strongly associated with increased susceptibility to acute respiratory infection in humans due to reduction in resistance to infection and increased exposure to infectious agents.14 There is also a strong correlation between parental unemployment and children’s poor health outcome.17
A multinational research in developing countries located in Africa, Americas, Asia and the Pacific shows the prevalence of acute respiratory infections among both HIV-infected and HIV-uninfected children to be 13%. The study also shows that factors like living in high-risk indoor environment, male gender, employed mothers and low birthweight were positively associated with acute respiratory infections. Planned pregnancy, maternal education, older maternal age, breastfeeding for more than 6 months, and immunisation were associated with reduction in respiratory infections.18
Younger mothers are not as experienced as older women and are mostly learning to care for their first child.19 The first child of adolescent and young mothers are most susceptible to both poor health outcomes and mortality.19 The children of first time young mothers are at higher risk of developing diarrhoea, stunting and anaemia.19 A multinational study on acute diarrhoea in developing countries among both immunised and non-immunised children shows that country inequalities, maternal illiteracy and unemployment were greatly associated with diarrhoea.20 Female children, normal birthweight, older children, complete immunisation coverage, advanced maternal age, planned pregnancy, good sanitation and rich household were associated with reduction in episodes of diarrhoea.20
Furthermore, the findings from the multinational studies.18,20 involved children that were both immunised and unimmunised. The study participants were both HIV-exposed and non-exposed children. The multinational studies show association with many factors while this multilevel analytic research included only HIV-exposed children who were vaccinated with DTP3 and shows few associations.
Consistent, equitable availability and access to vaccination especially among the most vulnerable and poorest communities is essential in addressing non-uptake of basic vaccines in HIV-exposed children. Integrated Global Action Plan for the Prevention and Control of Pneumonia and Diarrhoea (GAPPD) which recommends an interrelated approach for the elimination of preventable diarrhea and pneumonia deaths has vaccination as one of the key interventions.21 GAPPD brings together essential services and interventions such as promotion of practices that can protect children from these respiratory and diarrhoeal diseases and make sure that every child has access to suitable preventive measures and proper treatment.21
Strengths and limitations
The use of DHS gives this study a good quality and representation because the surveys were done in different regions of the included countries. However, this study has certain significant limitations. Firstly, the surveys were not conducted concurrently and within the same time frame in each of the countries. Social conditions do change and expected to change over time in these countries. The surveys were conducted in different countries over a time space of a decade and this may have some effect on the study findings. Secondly, DHS methodology being cross-sectional in nature, it does not give room for establishing causality. Haemophilus Influenzae type b (Hib) vaccine and rotavirus vaccine coverage as at 2016 were 74% and 43% among the African countries. Pneumococcal vaccine global coverage was estimated at 42% in 2016.22 The use of pneumococcal and rotavirus vaccination data would have provided added information with respect to independent contributions of various factors because as at the time when the surveys were conducted most of the African countries were yet to introduce Hib, pneumococcal and rotavirus vaccines. Another gap noticed in this study is the lack of knowledge of the HIV status of the children. The children were not tested for HIV infection during the survey.
Conclusions
This study gives an insight concerning the determinants of key morbidity factors among the immunised and HIV-exposed children in sub-Saharan Africa. The study reveals that residence in communities with high unemployment was an independent predictor of acute respiratory infections among immunised and HIV-exposed children. HIV-exposed children born to women aged 15–24 or 25–34 years old were significantly more likely to develop diarrheal diseases in sub-Saharan Africa.
These findings are important because they have policy implications on the implementation of child healthcare programmes for respiratory infections and diarrhoeal diseases particularly among HIV-exposed and infected children in sub-Saharan Africa. Public healthcare programmes should target adolescent and young women, and their family members on how to prevent diarrhoea. Efforts should be made to identify the hotspots for acute respiratory diseases especially in communities with high rate of unemployment and to develop strategies to combat the diseases in such communities.
Further large data research is needed in studying the effect of rotavirus, pneumococcal and Hib vaccines on the prevalence of diarrhoea and respiratory infection in sub-Saharan Africa population. It is recommended that DHS should include the newer vaccines and HIV status for the children as part of the collected data so as to have a large database for a robust study of vaccine-preventable diseases in HIV-infected children across developing countries.
Methods
Data sources
This study used 27 nationally represented and cross-sectional surveys as of November 2017. The demographic and health surveys (DHS) were implemented by different national institutions and ICF International, Calverton, Maryland, USA. United States Agency for International Development, Global Fund to Fight AIDS, Tuberculosis and Malaria, and others provided financial support. The survey methods and data collection procedures were described in another publication.23 Included DHS were selected based on the availability of data on childhood immunisation, maternal HIV status, symptoms of acute respiratory infections and diarrhoea. DHS data were household sample surveys and the sampling design involved selecting and interviewing samples of women aged 15–49 years was based on multi-stage cluster sampling. The DHS surveys instruments were standardised questionnaires administered by interviewers. Women aged 15–49 years were tested for HIV infection while children were not tested during the survey.
Outcome variable
The outcome variable is defined as a DTP3 vaccinated child of an HIV-infected mother with symptoms of acute respiratory infections or an episode of diarrhoea two weeks prior to the survey. The vaccinees were within the 12–23 months age range at the time of various surveys and at that age they were expected to have taken most of the basic childhood vaccines as specified by each country.
DHS defined symptoms of acute respiratory infections as a cough associated with short and rapid breathing in an ill under-five child within the last two weeks preceding the survey. Diarrhoea is charaterised by loose and watery stools three or more times a day in children.
Determinant variables
Individual-level
Five measures of individual socio-economic position were considered in the model, namely: age of the mother, educational level, wealth index, employment status and place of residence. The age of the mother was in completed years (15 to 24, 25 to 34, 35 to 49); level of educational as no formal education, primary education, and secondary or higher education; wealth index as either poorer, middle and richest; and employment status as currently employed or unemployed.
Community-level factors
We included the following community-level factors in the model: neighbourhood poverty rate defined as the percentage of households that are below 20% of wealth index, illiteracy rate which is the percentage of women without formal education within the community, unemployment rate defined as the percentage of women who are currently unemployed within the community and place of residence which is either urban or rural. We also classified the rates to be low or high.
Country-level factors
The study included the following country-level factors in the model: gross domestic product (GDP) per capita, adult literacy rate and health expenditure (Table 1). We obtained these data from the World Bank database.24 The country-level variables were also categorised into either low or high classes in order to assess nonlinear effects and for easy interpretation of results for policy decision making.
Statistical analyses
The distribution of respondents by various key variables were expressed as percentages. Pearson’s chi-squared test was used for analysing contingency tables. We used individual weights for the descriptive statistics reported by this study. Multivariable logistic regression models were used to analyse the association between individual and contextual factors associated with symptoms of acute respiratory infections or diarrhoea among the children of women living with HIV and with history of uptake of DTP3 vaccines.
We used a 5-level model for the binary variable, namely:
First model: empty null model, an unconditional model without any explanatory variables
Second model: for only individual-level factors
Third model: for only community-level factors
Fourth model: for only country-level factors
Fifth model (Full model): that controlled for individual-, community- and country-level factors simultaneously.
The fixed-effects model results were presented as odds ratio (ORs) with 95% credible intervals (CrIs). The random effects measures included intra-cluster correlation (ICC) and variance partition coefficient and median odds ratio (MOR). We calculated ICC by the use of formula described by Snijders and Bosker.25 The method used for the calculation of MOR was described by Larsen et al.26,27. All the included tests were two tailed with the probability level of less than 0.05 considered to be significant. The models were fitted with MLwiN 3.01.28 Statistical analysis were performed with the use of STATA 14.0.29
Ethics statement
This research was a secondary analysis of existing survey data which were obtained with permission from the DHS program database21 These surveys were conducted after ethical approval by the Institutional Review Board of ICF International, Calverton, Maryland, USA and by respective National Ethical Review Committees in Angola, Burkina Faso, Burundi, Cameroun, Chad, Democratic Republic of the Congo, Cote d’Ivoire, Ethiopia, Gabon, Gambia, Ghana, Guinea, Kenya, Lesotho, Liberia, Malawi, Mali, Namibia, Niger, Rwanda, Sao Tome and Principle, Senegal, Sierra Leone, Swaziland, Togo, Zambia and Zimbabwe. The study participants gave informed consent at the time of the surveys and their confidentiality respected.
Biography
Olatunji O. Adetokunboh conceived the study. OOA did the data analysis, interpreted the results and wrote the initial manuscript. OAU and CSW reviewed and edited the manuscript. All authors read and approved the final version of the manuscript.
Funding Statement
Olatunji O. Adetokunboh and Charles S. Wiysonge are supported by the National Research Foundation of South Africa (Grant Numbers:106035 and 108571) and the South African Medical Research Council. Olalekan A. Uthman is supported by the National Institute of Health Research using Official Development Assistance funding. The views expressed in this publication are those of the authors and not necessarily those of the National Health Service, the National Institute for Health Research, South African Medical Research Council and National Research Foundation of South Africa.
Abbreviations
- AIDS
Acquired Immunodeficiency Syndrome
- ARV
antiretroviral drugs
- CrI
Credible interval
- DHS
Demographic and health survey
- DTP
Diphtheria-tetanus-pertussis
- EPI
Expanded Program on Immunization
- GAPPD
Integrated Global Action Plan for the Prevention and Control of Pneumonia and Diarrhoea
- GAVI
Global Alliance for Vaccines and Immunisation
- GDP
Gross domestic product per capita
- HDI
Human development index
- HIV
Human immunodeficiency virus
- ICC
Intra-cluster correlation
- MOR
Median odds ratio
- OR
Odds ratio
- PMTCT
Prevention of mother-to-child transmission
- UNICEF
United Nations Children’s Fund
Disclosure of potential conflicts of interest
No potential conflict of interest was reported by the authors.
Acknowledgments
We are grateful for the MEASURE DHS for releasing the data for this study.
Consent for publication
Not applicable.
References
- 1.United Nations Children’s Fund. The state of world’s children Children in a digital world; 2017 [accessed 2018 Feb 22]. https://www.unicef.org/publications/files/SOWC_2017_ENG_WEB.pdf.
- 2.Global Alliance for Vaccines and Immunisation GAVI annual report 2016; 2017 [accessed 2017 Dec 22]. http://www.gavi.org/progress-report/.
- 3.Abajobir AA, Abbafati C, Abbas KM, Abd-Allah F, Abera SF, Aboyans V, Adetokunboh O, Afshin A, Agrawal A, Ahmadi A, et al. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980–2016: a systematic analysis for the Global Burden of Disease Study 2016. The Lancet. 2017;390(10100):1151–1210. doi: 10.1016/S0140-6736(17)32152-9 PMID: 28919116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Thea DM, St. Louis ME, Atido U, Kanjinga K, Kembo B, Matondo TT , et al. A prospective study of diarrhea and HIV-1 infection among 429 Zairian infants. N Engl J Med. 1993;329(23):1696–1702. doi: 10.1056/NEJM199312023292304 PMID: 8232458. [DOI] [PubMed] [Google Scholar]
- 5.Miller MA, Hinman A.. Economic analyses of vaccine policies In: Plotkin SA, editor. Vaccines. Philadelphia (PA): Elsevier Inc; 2004. [Google Scholar]
- 6.Hadler SC, Cochi SL, Bilous J, Cutts F.. Vaccination programs in developing countries In: Plotkin SA, editor. Vaccines. Philadelphia (PA.): Elsevier Inc; 2004. [Google Scholar]
- 7.Andre FE, Booy R, Bock HL, Clemens J, Datta SK, John TJ, Lee BW, Lolekha S, Peltola H, Ruff TA, et al., Vaccination greatly reduces disease, disability, death and inequity worldwide. Bull World Health Organ. 2008;86(2):140–146. PMID: 18297169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.World Health Organization Estimates of disease burden and cost effectiveness; 2017. http://www.who.int/immunization/monitoring_surveillance/burden/estimates/en/.
- 9.Abajobir AA, Abate KH, Abbafati C, Abbas KM, Abd-Allah F, Abera SF, Abraha HN, Abu-Raddad LJ, Nme A-R, Adedeji IA, et al. Global, regional, and national under-5 mortality, adult mortality, age-specific mortality, and life expectancy, 1970–2016: a systematic analysis for the Global Burden of Disease Study 2016. The Lancet. 2017;390(10100):1084–1150. doi: 10.1016/S0140-6736(17)31833-0 PMID: 28919115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Global Alliance for Vaccines and Immunisation GAVI annual report 2016; 2017 [accessed 2017 Dec 27]. http://www.gavi.org/progress-report/.
- 11.Machingaidze S, Wiysonge CS, Hussey GD. Strengthening the expanded programme on immunization in Africa: looking beyond 2015. PLoS Medicine. 2013;10:1–5. doi: 10.1371/journal.pmed.1001405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.World Health Organization Table 1 : summary of WHO position papers - recommendations for routine immunization; 2018 [accessed 2018 Jul 7]. http://www.who.int/immunization/policy/Immunization_routine_table1.pdf?ua=1.
- 13.Wilson WJ. When work dissapears. 1st ed. New York: Alfred A. Knoff, Inc; 1996 [Google Scholar]
- 14.Cohen S. Social status and susceptibility to respiratory infections. Annals of the New York Academy of Science. 1999;896(1):246–253. PMID: 10681901. [DOI] [PubMed] [Google Scholar]
- 15.Ogunmola OJ, Oladosu YO, Olamoyegun MA. Relationship between socioeconomic status and HIV infection in a rural tertiary health center. HIV AIDS (Auckl). 2014;6:61–67. doi: 10.2147/HIV.S59061 PMID: 24790469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Van Lenthe FJ, Borrell LN, Costa G, Diez Roux AV, C Tm K, Marinacci C, Martikainen P, Regidor E, Stafford M, Valkonen T. Neighbourhood unemployment and all cause mortality: A comparison of six countries. J Epidemiol Community Health. 2005;59(3):231–237. doi: 10.1136/jech.2004.022574 PMID: 15709084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mörk E, Sjögreny A, Svalerydz H. Parental unemployment and child health. CESifo Economic Studies. 2014;60:366–401. doi: 10.1093/cesifo/ifu016. [DOI] [Google Scholar]
- 18.Ám P-R, Aguilera-Otalvaro P, Zárate-Ardila C, Hoyos-Martínez A. Acute respiratory infection in children from developing nations: a multi-level study. Paediatr Int Child Health. 2016;36(2):84–90. doi: 10.1179/2046905515Y.0000000021 PMID: 25936959. [DOI] [PubMed] [Google Scholar]
- 19.Finlay JE, Özaltin E, Canning D. The association of maternal age with infant mortality, child anthropometric failure, diarrhoea and anaemia for first births: evidence from 55 low- and middle-income countries. BMJ Open. 2011;1(2):e000226. doi: 10.1136/bmjopen-2011-000226 PMID: 22021886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ám P-R, Zárate-Ardila C, Hoyos-Martínez A, Ám R-S, Vélez-Van-Meerbeke A. Country characteristics and acute diarrhea in children from developing nations: a multilevel study. BMC Public Health. 2015;15:811. doi: 10.1186/s12889-015-2120-8 PMID: 26293136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.World Health Organization, The United Nations Children’s Fund Ending preventable child deaths from Pneumonia and Diarrhoea by 2025: the integrated Global Action Plan for Pneumonia and Diarrhoea (GAPPD). Geneva (Switzerland): WHO/UNICEF; 2013 [accessed 2018 Jan 20]. http://apps.who.int/iris/bitstream/10665/79200/1/9789241505239_eng.pdf. [Google Scholar]
- 22.World Health Organization Immunization coverage for selected vaccine preventable diseases; 2018.[accessed 2018 Jul 7]. http://www.who.int/gho/immunization/en/.
- 23.Measure DHS Publications by country; 2017 [accessed 2017 Dec 21]. http://dhsprogram.com/Publications/Publications-by-Country.cfm.
- 24.World Bank The world bank data; 2017. [accessed 2017 Dec 22]. http://data.worldbank.org/.
- 25.Snijders TAB, Bosker RJ. Multilevel analysis: an introduction to basic and advanced multilevel modeling. 2nd ed. London (UK): Sage Publishers; 2012. [Google Scholar]
- 26.Larsen K, Petersen JH, Budtz-Jrgensen E, Endahl L. Interpreting parameters in the logistic regression model with random effects. Biometrics. 2000;56(3):909–914. PMID: 10985236. [DOI] [PubMed] [Google Scholar]
- 27.Larsen K, Merlo J. Appropriate assessment of neighborhood effects on individual health: integrating random and fixed effects in multilevel logistic regression. Am J Epidemiol. 2005;161(1):81–88. doi: 10.1093/aje/kwi017 PMID: 15615918. [DOI] [PubMed] [Google Scholar]
- 28.Rasbash J, Steele F, Browne W, Prosser B. A user’s guide to MLwiN. Centre for Multilevel Modelling, United Kingdom: University of Bristol; 2015. [Google Scholar]
- 29.StataCorp Stata Statistical Software: release 14. College Station (TX): StataCorp LP; 2015. [Google Scholar]


