ABSTRACT
Understanding the gaps in missed opportunities for vaccination (MOV) in sub-Saharan Africa would inform interventions for improving immunisation coverage to achieving universal childhood immunisation. We aimed to conduct a multicountry analyses to decompose the gap in MOV between poor and non-poor in SSA. We used cross-sectional data from 35 Demographic and Health Surveys in SSA conducted between 2007 and 2016. Descriptive statistics used to understand the gap in MOV between the urban poor and non-poor, and across the selected covariates. Out of the 35 countries included in this analysis, 19 countries showed pro-poor inequality, 5 showed pro-non-poor inequality and remaining 11 countries showed no statistically significant inequality. Among the countries with statistically significant pro-illiterate inequality, the risk difference ranged from 4.2% in DR Congo to 20.1% in Kenya. Important factors responsible for the inequality varied across countries. In Madagascar, the largest contributors to inequality in MOV were media access, number of under-five children, and maternal education. However, in Liberia media access narrowed inequality in MOV between poor and non-poor households. The findings indicate that in most SSA countries, children belonging to poor households are most likely to have MOV and that socio-economic inequality in is determined not only by health system functions, but also by factors beyond the scope of health authorities and care delivery system. The findings suggest the need for addressing social determinants of health.
KEYWORDS: Missed opportunities for vaccination, inequality in missed opportunities for vaccination, immunisation coverage, DHS survey data, Decomposition analysis, sub-Saharan Africa
Introduction
Global immunisation coverage data for 2016 indicate that more than 60% of the 19.5 million children worldwide that did not receive the full primary series of three doses of diphtheria-tetanus-pertussis containing vaccines (DTP3) live in low and middle-income countries.1 This suggests that there are missed opportunities for vaccination (MOV) in these countries. MOV refers to any contact with health services by an individual who is eligible for vaccination (e.g. unvaccinated or partially vaccinated and free of contraindications to vaccination), which does not result in the person receiving one or more of the vaccine doses for which he or she is eligible.2 Missed opportunities for vaccination occur in two major settings: (1) during visits for immunisation and other preventive services (e.g., growth monitoring, nutrition assessments, and oral rehydration training sessions), and (2) during visits for curative services. In both settings, eliminating missed opportunities will raise the overall immunisation coverage in a population, particularly when the availability and use of health services are high. When the availability and use of health services are low, immunising at every health care contact is extremely important because the risk for vaccine-preventable diseases is likely to be high in these areas.
Strategies to reduce missed opportunities for vaccination are recommended, many of which emphasize the usefulness of periodic systematic monitoring of vaccine uptake to evaluate the quality of immunisation programme performance at the health service level as well as progress towards reducing missed opportunities.3 A systematic review published in 2014 found the prevalence of MOVs in low- and middle-income countries was high, but the large number of identified reasons precludes standardized solutions. The authors emphasised the importance of the assessement of temporal and geographic variations4
Understanding the gaps in MOV in sub-Saharan Africa would inform interventions for improving immunisation coverage to achieving universal childhood immunisation. We aimed to conduct a multicountry analyses with efforts to decompose the gap in MOV between poor and non-poor in sub-Saharan Africa.
Results
Survey and sample characteristics
The countries, year of data collection, and the survey characteristics are listed in Table 1. The surveys were conducted between 2007 and 2016. The median number of children aged 12 to 23 months was 1847 (range: 370 to 5893). Half of the children were male. The average age of the children was 17 months. About 46% of the mothers were between 25 and 34 years old and about 41% had no formal education. One third of the mothers were not working at the time of the survey. Most of the respondents were living in rural areas (70%). Table 2 presents the descriptive statistics for the final pooled sample.
Table 1.
Description of Demographic and Health Surveys data by countries, in sub-Saharan Africa, 2007 to 2016.
| Country | Survey year | Number of children | MOV (%) | Poor (%) |
|---|---|---|---|---|
| Angola | 2016 | 2740 | 55.1 | 52.7 |
| Benin | 2012 | 2540 | 58.7 | 43.5 |
| Burkina Faso | 2010 | 2861 | 22.4 | 40.2 |
| Burundi | 2011 | 1540 | 25.6 | 40.5 |
| Cameroon | 2011 | 2282 | 46.5 | 43.6 |
| Chad | 2015 | 2954 | 47.2 | 40.7 |
| Comoros | 2012 | 585 | 38.3 | 44.6 |
| Congo | 2012 | 1842 | 67.3 | 71.9 |
| Congo DR | 2014 | 3435 | 63.8 | 48.4 |
| Coted Ivoire | 2012 | 1447 | 51.5 | 48.7 |
| Ethiopia | 2016 | 1940 | 52.9 | 50.6 |
| Gabon | 2012 | 1159 | 89 | 69.8 |
| Gambia | 2013 | 1611 | 23.2 | 51.8 |
| Ghana | 2014 | 1113 | 37.4 | 55.2 |
| Guinea | 2012 | 1335 | 55.5 | 43.5 |
| Kenya | 2014 | 3952 | 44.4 | 55.7 |
| Lesotho | 2014 | 682 | 41.5 | 46.5 |
| Liberia | 2013 | 1431 | 52.9 | 60.4 |
| Madagascar | 2009 | 2152 | 56.2 | 49.7 |
| Malawi | 2016 | 3269 | 43.8 | 45.9 |
| Mali | 2013 | 1847 | 61.7 | 38.8 |
| Mozambique | 2011 | 2282 | 34.3 | 37.4 |
| Namibia | 2013 | 968 | 31.2 | 41.5 |
| Niger | 2012 | 2158 | 49.9 | 33.3 |
| Nigeria | 2013 | 5893 | 43.7 | 45.8 |
| Rwanda | 2015 | 1531 | 60 | 44.6 |
| Sao Tome Principe | 2009 | 370 | 23.8 | 48.6 |
| Senegal | 2011 | 2353 | 47.8 | 55.3 |
| Sierra Leone | 2013 | 2208 | 34.7 | 43.4 |
| Swaziland | 2007 | 553 | 24.4 | 40.1 |
| Tanzania | 2016 | 2113 | 46.9 | 41.2 |
| Togo | 2014 | 1409 | 37.6 | 47.8 |
| Uganda | 2011 | 1381 | 58.1 | 47.3 |
| Zambia | 2014 | 2563 | 65.7 | 49.5 |
| Zimbabwe | 2015 | 1158 | 20.7 | 40.0 |
Table 2.
Summary of pooled sample characteristics of the Demographic and Health Surveys data in sub-Saharan Africa.
| |
Number (%) |
|---|---|
| 69657 | |
| Child's age (mean (sd)) | 17.13 (3.42) |
| Male (%) | 35249 (50.6) |
| High birth order (%) | 21723 (31.2) |
| Under-five children (mean (sd)) | 2.02 (1.32) |
| Maternal age (%) | |
| 15–24 | 23931 (34.4) |
| 25–34 | 31828 (45.7) |
| 35–49 | 13898 (20.0) |
| Wealth index(%) | |
| Poor | 32912 (47.2) |
| Non-poor | 36745 (52.3) |
| Maternal education (%) | |
| no education | 28310 (40.6) |
| primary | 24139 (34.7) |
| secondary+ | 17199 (24.7) |
| Not working (%) | 22032 (31.6) |
| Media access (%) | |
| 0 | 23736 (34.1) |
| 1 | 22378 (32.1) |
| 2 | 16921 (24.3) |
| 3 | 6622 ( 9.5) |
| Rural (%) | 48467 (69.6) |
Prevalence of MOV
There was a wide variation in the MOV rates among chidren of poor and non-poor mothers across the 35 countries (Fig. 1). The rate of MOV among children of mothers from poor households ranged from 22.5% in Swaziland to 87.1% in Gabon, while it ranged from 18.4% in Sao Tome and Principe to 93.4% in Gabon among children of mothers from non-poor households.
Figure 1.
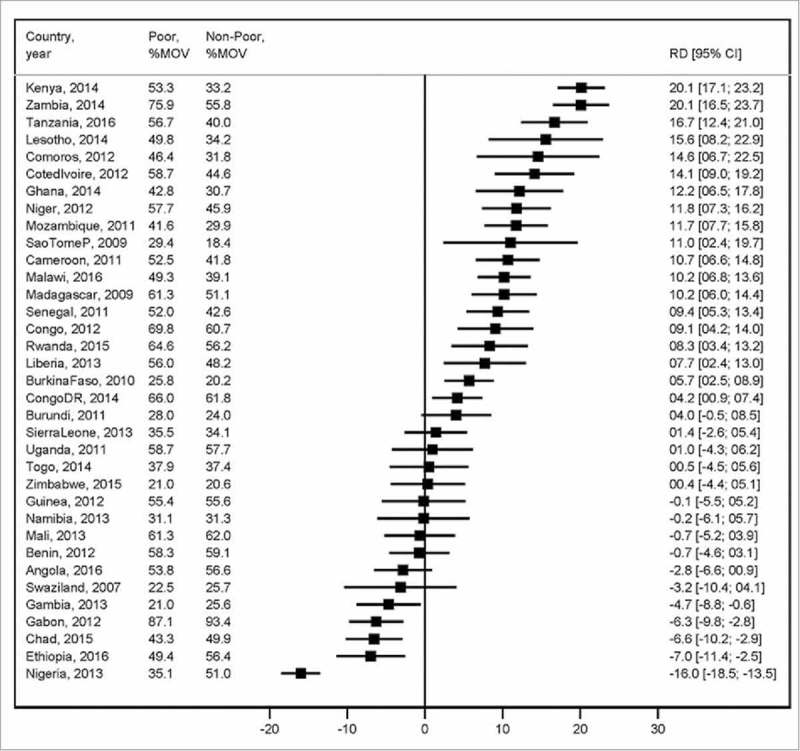
Description of Demographic and Health Surveys data by countries, in sub-Saharan Africa, 2007 to 2016.
Magnitude and variations in education inequality in MOV
Figure 2 shows the risk difference (measure of inequality) between children of mothers from poor and non-poor households. Out of the 35 countries included in this analysis, 19 countries showed pro-poor inequality (i.e. MOV is prevalent among the children of mothers from poor households), five showed pro-non-poor inequality (i.e. MOV is prevalent among children of mothers from non-poor households), and remaining 11 countries showed no statistically significant inequality. Among the countries with statistically significant pro-poor inequality, the risk difference ranged from 4.2% in the Democratic Republic of Congo to 20.1% in Kenya. The risk difference ranged from -16.0% in Nigeria to -4.7% in the Gambia.
Figure 2.
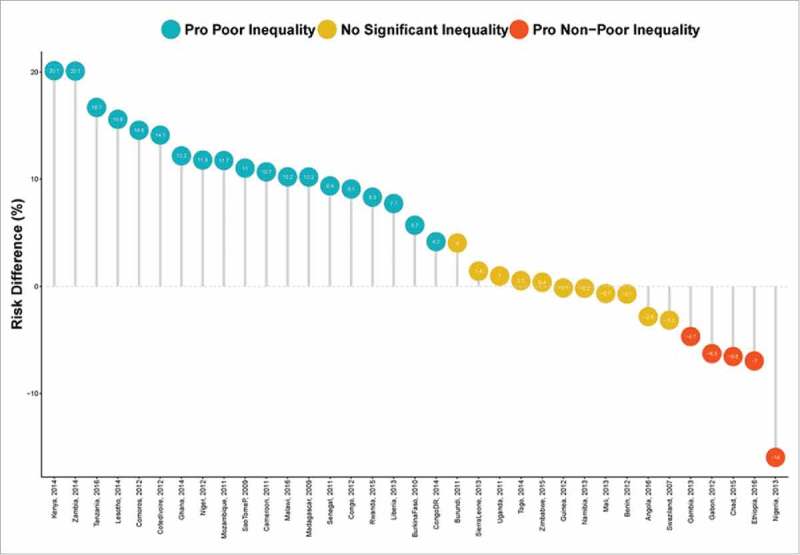
Risk difference between children from poor and non-poor households in missed opportunities for vaccination, by countries.
Figure 3 plots the relationship between rate of MOV and inequality for all countries. The countries can be grouped into distinct categories:
-
•
high MOV and high pro-poor inequality such as Zambia
-
•
high MOV and high pro-non-poor inequality such as Gabon
-
•
low MOV and high pro-poor inequality such as Malawi
-
•
low MOV and non-significant pro-non-poor inequality such as the Gambia
Figure 3.
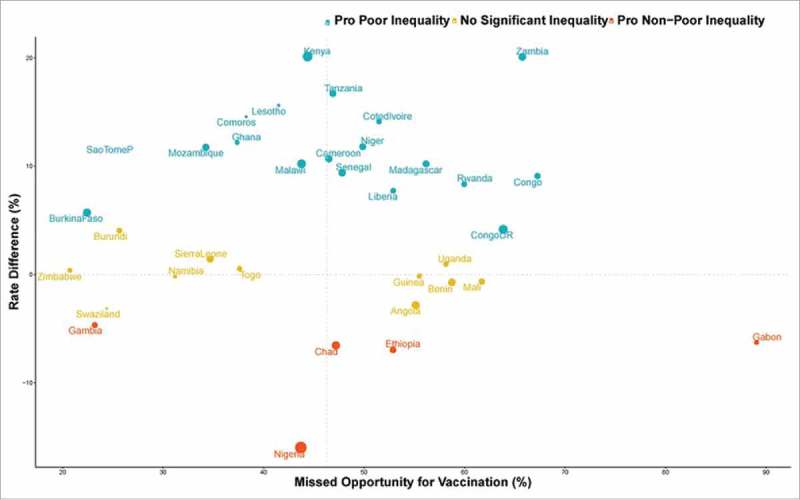
Scatter plot of rate of missed opportunities for vaccination and risk difference between children from poor and non-poor households in sub-Saharan Africa.
Decomposition of education inequality in MOV
The decomposition results are shown in eFig. 1 and Fig. 4. A negative contribution indicates that the determinant was narrowing the relative gap between poor and non-poor households. The contributions of the compositional ‘explained’ and structural ‘unexplained’ components varied across the countries. Compositional effects of the determinants were responsible for most of the inequality in MOV between poor and non-poor households in Madagascar. While in Senegal, Sao Tome and Principe, and Liberia structural effects of the determinants were responsible for most of the inequality in MOV between poor and non-poor households.
Figure 4.
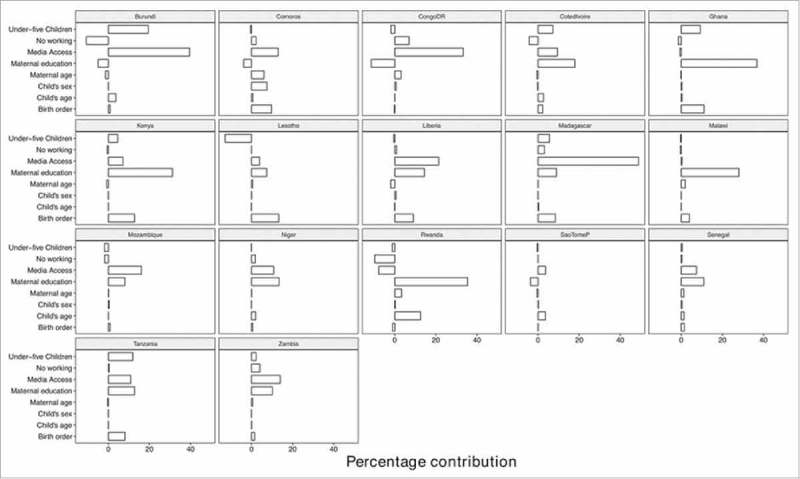
Contributions of differences in the distribution ‘compositional effect’ of the determinants of missed opportunities for vaccination to the total gap between children from poor and non-poor households.
Figure 4 shows the detailed decomposition of the part of the inequality that was caused by compositional effects of the determinants. The important factors responsible for the inequality varied across the countries. In Madagascar, the largest contributions to the inequality in MOV was media access followed by the number of under-five children and maternal education. However, in Liberia media access narrowed the inequality in MOV between poor and non-poor households.
Discussion
MOVs continue to hinder the efforts of increasing vaccine coverage in Sub saharan Africa. We found wide variations in the prevalence of MOV among children of poor and non-poor mothers across 35 countries. MOV rates among children of mothers from poor and non-poor households ranged from 22.5% in Swaziland to 87.1% in Gabon and 18.4% in Sao Tome and Principe to 93.4% in Gabon, respectively. Over 50% of the mothers were of child bearing age and of those 41% had no formal education, one third were unemployed during the survey and 70% of them lived in rural areas. The data presented here suggest that there is substantial MOV variation linked to factors such as maternal education inequality, and should be explored to better understand the issues surrounding poor vaccination coverage in sub-Saharan Africa.
Socioeconomic status seems to be the major contributor for inequalities in child health and is a major concern in sub-Saharan African countries to achieve the Sustainable Development Goal 3 (SDG3) set forth by the United Nations. Evidently in this analysis, nineteen countries showed pro-poor inequality (i.e. MOV is prevalent among the children of mothers from poor households),five showed pro-non-poor inequality (i.e. MOV is prevalent among the children of mothers from non-poor households), and the remaining eleven countries showed no statistically significant inequality. Among the countries with statistically significant pro-illiterate inequality, the risk difference ranged from 4.2% in the Democratic Republic of Congo to 20.1% in Kenya. The risk difference ranged from -16.0% in Nigeria to -4.7 % in the Gambia. This supports the findings that mothers with primary level education or higher were more likely to have children who were fully vaccinated and maternal age and receipt of antenatal or postnatal care were associated with full vaccination of their children.6 Kenya had MOV of 53.3% of children from poor households compared with 33.2% MOV from non-poor households and can be attributed to the observation that slum of residence was also associated with vaccination status, with children in Viwandani being twice as likely to be fully vaccinated compared to those in Korogocho.6 The risk difference ranged from -16.0% in Nigeria to -4.7% in the Gambia attributed to many reasons which include distance to the Mother and Child Care clinics (MCCs), transport costs, negative experiences at MCCs (such as interactions with unfriendly staff), and mothers' feeling of shame provoked by different, often poverty-associated reasons such as attending the clinic with a dirty or poorly clothed child.7 In Nigeria an MOV of 35.1% from poor households compared 51.0% MOV from non-poor household was observed. These observations supports the finding that there is a relationship between wealth and immunisation coverage. Children from families with non-poor economic status have a higher chance of missing opportunities for vaccination than children from poor household.8
The relationship between the rate of MOV and inequality per country was analysed further to understand the relative gap between poor and non-poor households. The contributions of the compositional ‘explained’ and structural ‘unexplained’ components varied across countries. Compositional effects of the determinants were responsible for most of the inequality in MOV between poor and non-poor households in Madagascar. Madagascar is one of the countries in which malnutrition does not affect growth inequality in children under the age of five year;s8 suggesting that poor and non-poor households have other compositional effects that contribute to inequality in MOV.9 However, in Senegal, Sao Tome and Principe, and Liberia structural effects of the determinants were responsible for most of the inequality in MOV between poor and non-poor households. Household wealth and parental education were robustly associated with improved vaccination coverage in children, supporting prior work in other African nations.10-14 If a child is born of an illiterate mother, the risk of not being fully immunised increases by 85%, while the risks are 8% higher for children in rural areas, 35% higher for children of birth order 3 or more. These are some of the compositional effects that can contribute to inequality in MOV as outlined in a survey conducted in India.15 A growing body of empirical work highlights such associations between socioeconomic status (SES) and `vaccination.10-11,16-17 The important factors responsible for the inequality varied across the countries. In Madagascar, the largest contributions to the inequality in MOV was media access followed by number of under-five children and maternal education. This reflects the increasing recognition that social factors influence medical interventions including vaccination. This suggests that individuals with more resources, including money, knowledge, power, prestige, and beneficial social connections, will access vaccination more rapidly, and effectively to curb preventable diseases. However, in Liberia media access narrowed the inequality in MOV between poor and non-poor households. Access to information is at the core of ensuring that rates of MOV are reduced significantly. This can include healthcare workers facilitating education on the importance to vaccination by conducting door to door activities, access to media information which contribute to raising awareness and mobilising social networks about vaccination in communities where access to vaccines may be limited. The other important contributors to reducing MOV have to do with improvement of healthcare services, eliminating the travel costs associated with seeking vaccinations at health facilities to ensure equal access to healthcare facilities. The findings from this paper highlight the need for multiple approaches to resolve the diffential factors that contribute to missed opportunities for vaccination, so as to bridge the gap in vaccination coverage between poor and non-poor in sub-Saharan Africa.
Methods
Study design and data
Data for this cross-sectional study were obtained from Demographic and Health Surveys (DHS), which are nationally representative household surveys conducted in low- and middle-income countries. This study used data from 35 recent DHS surveys conducted between 2007 and 2016 in sub-Saharan Africa available as of December 2017. The DHS uses a multi-stage, stratified sampling design with households as the sampling unit.18 Within each sample household, all women and men meeting the eligibility criteria are interviewed. Because the surveys are not self-weighting, weights are calculated to account for unequal selection probabilities as well as for non-response. With weights applied, survey findings represent the full target population. The DHS surveys include a household questionnaire, a women's questionnaire, and in most countries, a men's questionnaire. All three DHS questionnaires are implemented across countries with similar interviewer training, supervision, and implementation protocols.
Outcome variable
We used the World Health Organisation (WHO) definition of missed opportunity for vaccination (MOV) as the outcome variable, categorized as a binary variable that takes the value of ‘1’ if a child aged 12–23 months had any contact with health services who is eligible for vaccination (e.g. unvaccinated or partially vaccinated and free of contraindications to vaccination), which does not result in the child receiving one or more of the vaccine doses for which he or she is eligible, (and ‘0’ if otherwise). Contact with health services were defined using the following six variables: skilled birth attendance, baby postnatal check within 2 months, received vitamin A dose in first 2 months after delivery, has health card and medical treatment of diarrhea/ fever/cough We limited the analysis to one child per woman in order to minimise over-representation of women with more than one child in the age category.
Main determinant variable
DHS did not collect direct information on household income and expenditure. We used DHS wealth index as a proxy indicator for socioeconomic position. The methods used in calculating DHS wealth index have been described elsewhere.19-20 Briefly, an index of economic status for each household was constructed using principal components analysis based on the following household variables: number of rooms per house, ownership of car, motorcycle, bicycle, fridge, television and telephone as well as any kind of heating device. From these criteria the DHS wealth index quintiles (poorest, poorer, middle, richer and richest) are derived. The bottom two quintiles (lower 40%) were considered as ‘poor’ and remaining three were classified as ‘non-poor’.
Explanatory variables
The following factors were included in the models: child's age, sex of the child (male versus female), high birth order (> 4 birth order), number of under five children in the household, maternal age completed years (15 to 24, 25 to 34, 35 or older), maternal education (no education, primary or secondary or higher), employment status (working or not working), and media access (radio, television or newspaper).
Statistical analyses
The analytical approach included descriptive statistics, univariable analysis and Blinder-Oaxaca decomposition techniques using logistic regressions. We used the descriptive statistics to show the distribution of respondents by the key variables. Values were expressed as absolute numbers (percentages) and mean (standard deviation) for categorical and continuous variables respectively. We calculated the risk difference in missed opportunities between the two groups, from poor or non-poor households. A risk difference greater than 0 suggests that missed opportunities are prevalent among children from poor households (pro-poor inequality). Conversely, a negative risk difference indicates that missed opportunities for vaccination is prevalent among children from non-poor households (pro-non-poor inequality). Finally, we adopted logistic regression method using the pooled cross-sectional data to conduct the Blinder-Oaxaca decomposition analysis.
The Blinder-Oaxaca decomposition21-22 is a counterfactual method with an assumption that “what the probability of missed opportunities for vaccination would be if children from poor households had the same characteristics as their non-poor counterparts?”. The Blinder-Oaxaca method allows for the decomposition of the difference in an outcome variable between 2 groups into 2 components. The first component is the “explained” portion of that gap that captures differences in the distributions of the measurable characteristics (referred to as “compositional” or “endowments”) of these groups. This illustrates the portion of the gap in missed opportunities for vaccination that is attributed to the differences in observable, measurable characteristics between the two groups. Using this method, we can quantify how much of the gap the “advantaged” and the “disadvantaged” groups is attributable to these differences in specific measurable characteristics. The second component is the “unexplained” part, meaning the portion of the gap due to the differences in the estimated regression coefficients and the unmeasured variables between the two groups. This is also referred to in the literature as the “structural” component or the “coefficient” portion of the decomposition. This reflects the remainder of the model not explained by the differences in measurable, objective characteristics. The “unexplained” portion arises from differentials in how the predictor variables are associated with the outcomes for the two groups. This portion would persist even if the disadvantaged group were to attain the same average levels of measured predictor variables as the advantaged group.
Supplementary Material
Funding Statement
This paper presents independent research supported wholly by the National Research Foundation of South Africa (Grant Number: 106035).
Disclosure of potential conflicts of interest
No potential conflicts of interest were disclosed.
Acknowledgments
The authors are grateful to DHS Program for providing them with the survey data. Olalekan Uthman is supported by the National Institute of Health Research using Official Development Assistance (ODA) funding. The views expressed in this publication are those of the author(s) and not necessarily those of the NHS, the National Institute for Health Research.
Declarations
Ethics approval and consent to participate
This study was based on an analysis of existing survey data with all identifier information removed. The survey was approved by the Ethics Committee of the ICF Macro at Fairfax, Virginia in the USA and by the National Ethics Committees in their respective countries. All study participants gave informed consent before participation and all information was collected confidentially.
Consent for publication
Not applicable.
Authors' contribution
OAU and CSY conceived the study. OAU and CSY obtained funding for the study. OAU collected and analysed initial data. AA, ABW, CSY, DN, EZS, ABW and OAU participated contributed in refining the data analysis. OAU and DN wrote the first manuscript. AA, ABW, CSY, DN, EZS, GB, JO, OAU, TO and SY contributed to further analysis, interpreting and shaping of the argument of the manuscript and participated in writing the final draft of the manuscript. All the authors read and approved the final manuscript.
References
- 1.World Health Organization Immunization coverage http://www.who.int/mediacentre/factsheets/fs378/en/.
- 2.Magadzire BP, Joao G, Shendale S, Ogbuanu IU. Reducing missed opportunities for vaccination in selected provinces of Mozambique: A study protocol. Gates Open Res. 2017;1:5. doi: 10.12688/gatesopenres.12761.1. PMID:29528041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hutchins SS, Jansen HA, Robertson SE, Evans P, Kim-Farley RJ. Studies of missed opportunities for immunization in developing and industrialized countries. Bull World Health Organ. 1993;71(5):549–60. PMID:8261558. [PMC free article] [PubMed] [Google Scholar]
- 4.Sridhar S, Maleq N, Guillermet E, Colombini A, Gessner BD. A systematic literature review of missed opportunities for immunization in low- and middle-income countries. Vaccine 2014;32(51):6870–9. doi: 10.1016/j.vaccine.2014.10.063. PMID:25444813. [DOI] [PubMed] [Google Scholar]
- 5.Kruk ME, Prescott MR, de Pinho H, Galea S. Equity and the child health Millennium Development Goal: the role of pro-poor health policies. J Epidemiol Community Health. 2011;65(4):327–33. doi: 10.1136/jech.2009.096081. PMID:20724284. [DOI] [PubMed] [Google Scholar]
- 6.Mutua MK, Kimani-Murage E, Ettarh RR. Childhood vaccination in informal urban settlements in Nairobi, Kenya: who gets vaccinated? BMC Public Health 2011;11(1):6. doi: 10.1186/1471-2458-11-6. PMID:21205306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schwarz NG, Gysels M, Pell C, Gabor J, Schlie M, Issifou S, Lell B, Kremsner PG, Grobusch MP, Pool R. Reasons for non-adherence to vaccination at mother and child care clinics (MCCs) in Lambarene, Gabon. Vaccine. 2009;27(39):5371–5. doi: 10.1016/j.vaccine.2009.06.100. PMID:19616497. [DOI] [PubMed] [Google Scholar]
- 8.Restrepo-Mendez MC, Barros AJ, Wong KL, Johnson HL, Pariyo G, Franca GV, Wehrmeister FC, Victora CG. Inequalities in full immunization coverage: trends in low- and middle-income countries. Bull World Health Organ. 2016;94(11):794–805B. doi: 10.2471/BLT.15.162172. PMID:27821882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Van de Poel E, Hosseinpoor AR, Speybroeck N, Van Ourti T, Vega J. Socioeconomic inequality in malnutrition in developing countries. Bull World Health Organ. 2008;86(4):282–91. doi: 10.2471/BLT.07.044800. PMID:18438517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ndirangu J, Barnighausen T, Tanser F, Tint K, Newell ML. Levels of childhood vaccination coverage and the impact of maternal HIV status on child vaccination status in rural KwaZulu-Natal, South Africa*. Trop Med Int Health. 2009;14(11):1383–93. doi: 10.1111/j.1365-3156.2009.02382.x. PMID:19737375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wado YD, Afework MF, Hindin MJ. Childhood vaccination in rural southwestern Ethiopia: the nexus with demographic factors and women's autonomy. Pan Afr Med J. 2014;17 Suppl 1:9. PMID:24624243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nankabirwa V, Tylleskar T, Tumwine JK, Sommerfelt H, Promise-ebf Study G. Maternal education is associated with vaccination status of infants less than 6 months in Eastern Uganda: a cohort study. BMC Pediatr. 2010;10:92. doi: 10.1186/1471-2431-10-92. PMID:21159193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mekonnen Y, Tensou B, Telake DS, Degefie T, Bekele A. Neonatal mortality in Ethiopia: trends and determinants. BMC Public Health. 2013;13:483. doi: 10.1186/1471-2458-13-483. PMID:23683315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bawah AA, Phillips JF, Adjuik M, Vaughan-Smith M, Macleod B, Binka FN. The impact of immunization on the association between poverty and child survival: evidence from Kassena-Nankana District of northern Ghana. Scand J Public Health 2010;38(1):95–103. doi: 10.1177/1403494809352532. PMID:19884162. [DOI] [PubMed] [Google Scholar]
- 15.Lauridsen J, Pradhan J. Socio-economic inequality of immunization coverage in India. Health Econ Rev. 2011;1(1):11. doi: 10.1186/2191-1991-1-11. PMID:22828353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Polonijo AN, Carpiano RM. Social inequalities in adolescent human papillomavirus (HPV) vaccination: a test of fundamental cause theory. Soc Sci Med. 2013;82:115–25. doi: 10.1016/j.socscimed.2012.12.020. PMID:23337830. [DOI] [PubMed] [Google Scholar]
- 17.Hatzenbuehler ML, Phelan JC, Link BG. Stigma as a fundamental cause of population health inequalities. Am J Public Health. 2013;103(5):813–21. doi: 10.2105/AJPH.2012.301069. PMID:23488505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rutstein SO, Rojas G. Guide to DHS Statistics: Demographic and Health Surveys Methodology. Calverton, Maryland: ORC Macro; 2006. [Google Scholar]
- 19.Montgomery MR, Gragnolati M, Burke KA, Paredes E. Measuring living standards with proxy variables. Demography. 2000;37(2):155–74. doi: 10.2307/2648118. PMID:10836174. [DOI] [PubMed] [Google Scholar]
- 20.Vyas S, Kumaranayake L. Constructing socio-economic status indices: how to use principal components analysis. Health Policy Plan. 2006;21(6):459–68. doi: 10.1093/heapol/czl029. PMID:17030551. [DOI] [PubMed] [Google Scholar]
- 21.Blinder AS. Wage Discrimination: Reduced Form and Structural Variables. J Human Res. 1973;8(4):436–455. doi: 10.2307/144855 [DOI] [Google Scholar]
- 22.Oaxaca R. Male-Female Wage Differentials in Urban Labor Markets. Int Econ Rev. 1973;14:693–709. doi: 10.2307/2525981. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


