ABSTRACT
We reported previously that the annual average mortality rate in the United States in 2008–2011 for varicella listed as the underlying cause declined 87% compared with the prevaccine period (1990–1994). Here, we update the analysis with five additional years of data. We used varicella death data from the 2012–2016 Mortality Multiple Cause-of Death records to calculate mortality rates during 2012–2016 and trends since the prevaccine period and end of 1-dose vaccination program (2005–2007). The annual average age-adjusted mortality rate for varicella as the underlying cause was 0.03 per million population during 2012–2016, a 94% reduction from prevaccine years and a 47% reduction from 2005–2007. Varicella deaths continue to decline due to the varicella vaccination program in the United States.
KEYWORDS: CDC, NCHS, surveillance, vaccine-preventable disease, varicella deaths, varicella mortality, varicella vaccine, VZV
Short Report
Monitoring varicella-related deaths is important for assessing the impact of the varicella vaccination program on severe disease. The varicella vaccination program in the United States was implemented in 1996 as a 1-dose program; since 2007, a routine 2-dose program has been in place. Among children 19–35 months of age, ≥1-dose varicella vaccination coverage was 90.6% in 20161 and has been maintained at 90–92% since 2007. Among teens aged 13–17 years without history of varicella, ≥1 dose varicella vaccination has increased from 76% to 95% and ≥2 dose varicella vaccination from 19% to 86% during 2007–2016.2 We previously summarized varicella deaths from 1990–2011 using data from the Unites States national vital statistics system.3 Through 2008–2011, there was an 87% reduction in varicella deaths compared with the prevaccine period (1990–1994). Availability of 5 years of additional data provided an opportunity to describe characteristics of varicella deaths during 2012–2016 and to assess trends in varicella mortality after 2 decades of the varicella vaccination program in the United States.
We obtained data on varicella deaths for 2012–2016 using the Mortality Multiple Cause-of Death public use records from the National Center for Health Statistics (NCHS). A death from varicella was defined as one for which a varicella diagnosis (ICD-10 code B01) was listed on the death certificate. Deaths are classified with varicella as the underlying or a contributing cause of death by NCHS.3,4 The underlying cause of death is considered to be the disease or injury that initiated the events that directly led to death, whereas contributing cause(s) of death are diseases/conditions that did not directly cause death, but unfavorably influenced the course of disease or injury.5 We used population estimates from the Census Bureau6 to calculate mortality rates overall to calculate mortality rates overall, adjusted for the 2000 census population, and by age groups: <20, 20–49, and ≥50 years.
We calculated percent declines through 2012–2016 compared with the prevaccine period (1990–1994)7 and the end of the 1-dose varicella vaccine period (2005–2007).4 Test for trends were calculated assuming the deaths followed a Poisson distribution and the Pearson Chi-square test was used to compare age distribution of deaths by study period; two-sided P-values <0.05 were considered statistically significant. Information on characteristics of varicella deaths obtained from the vital statistics system was supplemented, when available, with data reported to the Centers for Disease Control and Prevention (CDC) as part of national varicella death surveillance.8 Although there is under-reporting to CDC's national varicella death surveillance, the data that are reported contain additional detailed patient information not available through the vital statistics system—such as vaccination status—that can be used to enhance the description of characteristics of varicella deaths.
During 2012–2016, varicella was listed as the underlying cause of death in 48 records (annual average: 9.6; range, 4–16) and as a contributing cause of death in 50 records (annual average: 10.0; range, 3–19) (Table 1). During this period, the annual average age-adjusted mortality rate attributed to varicella as the underlying cause was 0.03 per million population. This represents a 94% reduction compared with the prevaccine years 1990–1994 (average annual age-adjusted rate of 0.41 per million)7 (p<0.0001) and a 47% reduction from 2005–2007 (average annual age-adjusted rate of 0.05 per million)4 (p=0.002) (Fig. 1). Age-specific mortality rates during 2012–2016 for deaths with varicella listed as the underlying cause of death were 0.0007, 0.01, and 0.07 per million population for persons aged <20 years, 20–49 years, and ≥50 years, respectively; these rates represent a decline of 99%, 95%, and 80% from prevaccine years, respectively (Fig. 2), and all declines were statistically significant (p<0.0001). Overall, among persons aged <50 years of age, the decline was 97.4% from prevaccine years (p<0.0001) and 42.8% from the end of the 1-dose period (2005–2007) (p=0.04) (Fig. 2).
Table 1.
Annual varicella-related deaths, according to underlying or contributing cause, United States, 1990–2016.
| Varicella listed as underlying cause of death |
Varicella listed as contributing cause of death |
|||||||
|---|---|---|---|---|---|---|---|---|
| 1990–1994a | 2005–2007b | 2008–2011c | 2012–2016d | 1990–1994a | 2005–2007b | 2008–2011c | 2012–2016 | |
| Total average no. of deaths per year | 105 | 15 | 17 | 9.6 | 39.6 | 20.3 | 16.3 | 10.0 |
| Average no. (%) of deaths per year | ||||||||
| Age group (years) | ||||||||
| <1 | 8.8 (8.4) | 0 (0.0) | 0.0 (0.0) | 0.0 (0.0) | 3 (7.6) | 0.0 (0.0) | 0.0 (0.0) | 0.0 (0.0) |
| 1–4 | 13.2 (12.6) | 0.7 (4.4) | 0.0 (0.0) | 0.2 (2.1) | 5.2 (13.4) | 0.7 (3.3) | 0.5 (3.1) | 0.2 (2.0) |
| 5–9 | 15.6 (14.9) | 0.3 (2.2) | 0.0 (0.0) | 0.4 (4.2) | 3.2 (8.1) | 0.0 (0.0) | 0.0 (0.0) | 0.0 (0.0) |
| 10–19 | 10.4 (9.9) | 0.7 (4.4) | 0.5 (2.9) | 0 (0.0) | 2.2 (5.6) | 0.3 (1.6) | 0.3 (1.5) | 0.0 (0.0) |
| 20–49 | 35.6 (33.9) | 3.3 (22.2) | 4.5 (26.1) | 1.8 (18.8) | 11.6 (29.3) | 3.0 (14.8) | 2.0 (12.3) | 2.4 (24.0) |
| ≥50 | 21.4 (20.4) | 10.0 (66.7) | 12.3 (71.0) | 7.2 (75.0) | 14.4 (15.3) | 15.3 (80.3) | 13.5 (83.1) | 7.4 (74.0) |
| Gender | ||||||||
| Male | 55.4 (52.8) | 8.7 (57.8) | 9.8 (56.5) | 5.6 (58.3) | 24.8 (62.6) | 11.3 (55.7) | 9.3 (56.9) | 6.0 (60.0) |
| Female | 49.6 (47.2) | 6.3 (42.2) | 7.5 (43.5) | 4 (41.7) | 14.8 (37.4) | 9.0 (44.3) | 7.0 (43.1) | 4.0 (40.0) |
| Race | ||||||||
| White | 78.6 (74.9) | 13.7 (91.1) | 15.0 (87.0) | 7.8 (81.3) | 28.8 (72.7) | 17.3 (85.3) | 14.0 (86.2) | 8.0 (80.0) |
| Black | 19.2 (18.3) | 0.7 (4.4) | 0.8 (4.3) | 1.2 (12.5) | 8.8 (22.2) | 2.0 (9.8) | 1.0 (6.2) | 1.2 (12.0) |
| Other | 7.2 (6.9) | 0.7 (4.4) | 1.5 (8.7) | 0.6 (6.3) | 2.0 (5.1) | 1.0 (4.9) | 1.3 (7.7) | 0.8 (8.0) |
| Ethnicity | ||||||||
| Non-Hispanic | 87.6 (83.4) | 12.3 (82.2) | 14.8 (85.5) | 8.4 (87.5) | 34.2 (86.4) | 19.7 (96.7) | 14.0 (86.2) | 8.2 (82.0) |
| Hispanic | 14.8 (14.1) | 2.7 (17.8) | 2.3 (13.0) | 1.2 (12.5) | 4.4 (11.1) | 0.7 (3.3) | 2.3 (13.8) | 1.6 (16.0) |
Data are from Meyer et al.7
Data are from Marin et al.4
Data are from Leung et al.3
During 2012–2016, the annual number of varicella deaths was 16, 8, 4, 14, and 6 in 2012, 2013, 2014, 2015, and 2016, respectively. During this period, there were 3 deaths among persons <20 years of age: 1 in a 1–4 year-old (2012) and 2 in 5–9 year-olds (2012 and 2016). Among 20–49 year-olds, the annual number of varicella deaths was 2, 2, 2, 3, and 0 in 2012, 2013, 2014, 2015, and 2016, respectively.
Figure 1.
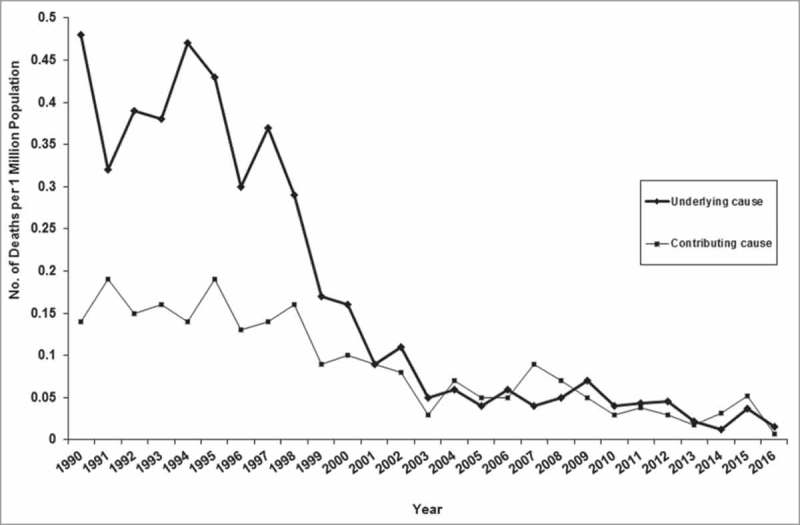
Varicella-related mortality rates, according to underlying or contributing cause, United States, 1990–2016 (age adjusted to the 2000 US population).
Figure 2.
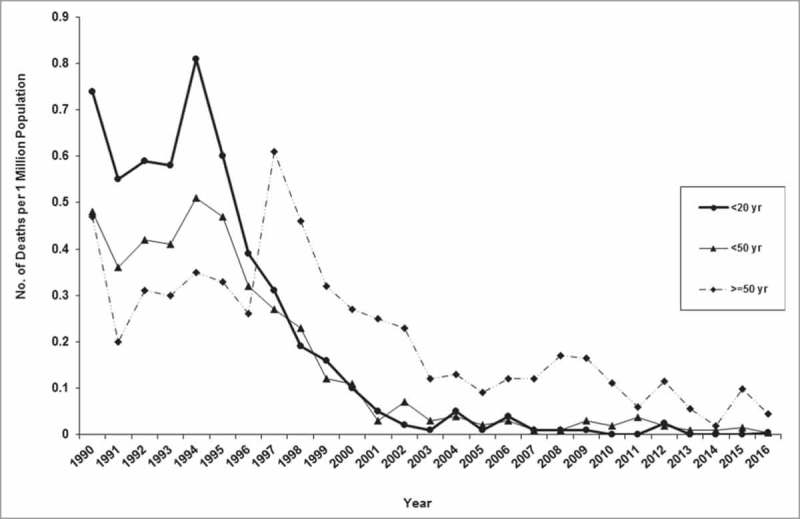
Varicella-related mortality rates for varicella as underlying cause by age group, United States, 1990–2016.
By age group, during 2012–2016, persons aged <20 years accounted for 6% (3/48) of the total deaths with varicella listed as the underlying cause, compared with 46% (240/525) in the prevaccine period (p<0.0001). Of the 3 deaths in this age group during 2012–2016, 1 occurred in a child in the 1–4 years of age group, and 2 in children in the 5–9 years of age group. Two children had preexisting medical conditions that increased the risk for severe varicella4 (leukemia and immunodeficiency, unspecified); for one child no underlying conditions were indicated. These 3 deaths were also reported to CDC as part of national varicella death surveillance; the additional information indicated that 1 of the deaths occurred in a 1-dose vaccinated child (with leukemia)9 while the other 2 children who died were unvaccinated.
Adults aged 20–49 years accounted for 19% (9/48) of the deaths with varicella listed as the underlying cause during 2012–2016 as compared with 34% (178/525) in the prevaccine period (p = 0.03); preexisting medical conditions with high risk for severe varicella were listed for 56% (5/9). Seven deaths in this age group were reported to CDC, and 2/7 persons who died were vaccinated with 1 dose within 1 month prior to death; vaccination status was unknown for the remaining 5. One of the vaccinated persons who died was confirmed to have vaccine-strain varicella-zoster virus (VZV) and specimens were unavailable for laboratory testing for the second. Both persons had immunocompromising conditions (chronic renal failure on immunosuppressive treatment and chronic automimmune disease, respectively).
The annual average age-adjusted mortality rate attributed to varicella as a contributing cause was 0.03 per million population in 2012–2016, an 83% reduction from prevaccine years 1990–1994 (average annual age-adjusted rate of 0.16 per million)7 (p<0.0001) and a 54% reduction from 2005–2007 (average annual age-adjusted rate of 0.06 per million)4 (p<0.0001) (Table 1; Fig. 1).
Since its inception in 1996, the varicella vaccination program has successfully controlled severe disease, including hospitalizations and deaths in the United States.4,7,10–14 These continued declines in varicella deaths are due to increased control of varicella in the United States,10,13 via achieving and sustaining high 1-dose varicella vaccination coverage and increasing 2-dose vaccination coverage. After 2 decades of program implementation, we report a 94% decline overall in deaths with varicella coded as the underlying cause compared with the prevaccine period, and additional declines during the 2-dose period compared with the end of the 1-dose varicella vaccination period. These continued declines were also observed in deaths with varicella coded as a contributing cause, and in all age groups. Among persons aged <20 years, born primarily during the childhood varicella vaccination program, three deaths were reported during 2012–2016 (all in children aged ≤9 years); during the 5 years before vaccine implementation, 240 deaths were reported in this age group (188 in children aged ≤9 years).7
With a vaccine highly efficacious against severe varicella,15 varicella deaths are preventable through vaccination. Additionally, indirect community protection due to increased control of the disease and subsequent decreased circulation of VZV protects those too young to be vaccinated or who have contraindications to vaccination. Data were not available to describe the varicella vaccination status or medical history of all persons who died of varicella. Nevertheless, varicella vaccination remains the best method for preventing varicella and related severe outcomes as seen in declines in disease, hospitalizations, and deaths as vaccination coverage increased. Varicella vaccine is contraindicated for immunocompromised persons, but vaccination of their household contacts is recommended to decrease the likelihood that wild-type VZV will be introduced in the household.16
After 2 decades of varicella vaccination program in the United States, we documented impressive declines in varicella deaths compared with the pre-vaccination period: 94% overall and 97% in persons younger than 50 years of age. Continued varicella surveillance is important to understand characteristics of varicella deaths that are still occurring and to monitor the impact of the varicella vaccination program in the United States.
Abbreviations
- CDC
Centers for Disease Control and Prevention;
- NCHS
National Center for Health Statistics;
- VZV
Varicella-zoster virus
Disclosure of potential conflicts of interest
No potential conflicts of interest were disclosed.
Acknowledgements
We thank Mary Ann Hall, MPH, for her editorial assistance.
Financial Support
There were no sources of financial support.
Disclaimer
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention, US Department of Health and Human Services.
References
- 1.Hill HA, Elam-Evans LD, Yankey D, Singleton JA, Kang Y. Vaccination Coverage Among Children Aged 19–35 Months – United States, 2016. MMWR Morb Mortal Wkly Rep. 2017;66(43):1171–7. doi: 10.15585/mmwr.mm6643a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Walker TY, Elam-Evans LD, Singleton JA, Yankey D, Markowitz LE, Fredua B, Williams CL, Meyer SA, Stokley S, et al. National, Regional, State, and Selected Local Area Vaccination Coverage Among Adolescents Aged 13–17 Years – United States, 2016. MMWR Morb Mortal Wkly Rep. 2017;66(33):874–82. doi: 10.15585/mmwr.mm6633a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Leung J, Bialek SR, Marin M. Trends in varicella mortality in the United States: Data from vital statistics and the national surveillance system. Hum Vaccin Immunother. 2015;11(3):662–8. doi: 10.1080/21645515.2015.1008880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Marin M, Zhang JX, Seward JF. Near elimination of Varicella deaths in the US after implementation of the vaccination program. Pediatrics. 2011;128(2):214–20. doi: 10.1542/peds.2010-3385. [DOI] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention National Center for Health Statistics. Instructions for Classifying the Underlying Cause of Death, 2017. Part 2a; 2017 Aug 30 [accessed 2018 Jan 18]. https://www.cdc.gov/nchs/data/dvs/2a_2017.pdf. [Google Scholar]
- 6.United States Census Bureau Population and Housing Unit Estimates. Washington: (DC: ): United States Department of Commerce; 2017 Dec 28. [accessed 2018 Jan 18]. https://www.census.gov/data/tables/2017/demo/popest/nation-detail.html. [Google Scholar]
- 7.Meyer PA, Seward JF, Jumaan AO, Wharton M. Varicella mortality: trends before vaccine licensure in the United States, 1970–1994. J Infect Dis. 2000;182(2):383–90. doi: 10.1086/315714. [DOI] [PubMed] [Google Scholar]
- 8.Lopez A, Leung J, Schmid S, Marin M. Chapter 17: Varicella. In: Centers for Disease Control and Prevention, ed. Manual for the Surveillance of Vaccine-Preventable Diseases; 2018 Jan 26; [accessed 13 Jan 2018].http://www.cdc.gov/vaccines/pubs/surv-manual/chpt17-varicella.html. [Google Scholar]
- 9.Kriner P, Lopez K, Leung J, Harpaz R, Bialek SR. Notes from the field: varicella-associated death of a vaccinated child with leukemia – California, 2012. MMWR Morb Mortal Wkly Rep. 2014;63(7):161. [PMC free article] [PubMed] [Google Scholar]
- 10.Bialek SR, Perella D, Zhang J, Mascola L, Viner K, Jackson C, et al. Impact of a routine two-dose varicella vaccination program on varicella epidemiology. Pediatrics. 2013;132(5):e1134–40. doi: 10.1542/peds.2013-0863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Leung J, Harpaz R. Impact of the Maturing Varicella Vaccination Program on Varicella and Related Outcomes in the United States: 1994–2012. J Pediatric Infect Dis Soc. 2015;5(4):395–402. doi: 10.1093/jpids/piv044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lopez AS, Zhang J, Brown C, Bialek S. Varicella-related hospitalizations in the United States, 2000–2006: the 1-dose varicella vaccination era. Pediatrics. 2011;127(2):238–45. doi: 10.1542/peds.2010-0962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lopez AS, Zhang J, Marin M. Epidemiology of Varicella During the 2-Dose Varicella Vaccination Program – United States, 2005–2014. MMWR Morb Mortal Wkly Rep. 2016;65(34):902–5. doi: 10.15585/mmwr.mm6534a4. [DOI] [PubMed] [Google Scholar]
- 14.Nguyen HQ, Jumaan AO, Seward JF. Decline in mortality due to varicella after implementation of varicella vaccination in the United States. N Engl J Med. 2005;352(5):450–8. doi: 10.1056/NEJMoa042271. [DOI] [PubMed] [Google Scholar]
- 15.Marin M, Marti M, Kambhampati A, Jeram SM, Seward JF. Global Varicella Vaccine Effectiveness: A Meta-analysis. Pediatrics. 2016;137(3):e20153741. doi: 10.1542/peds.2015-3741. [DOI] [PubMed] [Google Scholar]
- 16.Marin M, Guris D, Chaves SS, Schmid S, Seward JF. Prevention of varicella: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep. 2007;56(RR-4):1–40. [PubMed] [Google Scholar]


