Abstract
Background/Aims
Endoscopy and colonoscopy are frequently performed procedures to evaluate the gastrointestinal system. These procedures are sometimes disturbing and painful for the patient. In gastrointestinal suits, endoscopy and colonoscopy may be performed on awake or sedated patients. Music therapy is a common and non-pharmacological treatment for various medical conditions, pain, and anxiety. The aim of the present study was to add music therapy to sedation administered during endoscopy and colonoscopy. The effect of music treatment on drug consumption, anxiety, and pain was investigated.
Materials and Methods
American Anesthesiologist Association I–III adult patients scheduled for endo/colonoscopy were randomized to music treatment and no music treatment groups. Patients with endoscopic ultrasound and endoscopic retrograde colangiopancreaticography were excluded from the study. Anxiety score and pain severity were evaluated before and after the procedure. Heart rate, mean arterial pressure, and oxygen saturation were recorded before, during, and after the procedure. Total drug consumption was recorded. Patient satisfaction and desire for the same protocol for recurrent procedures were investigated.
Results
Music therapy added to deep sedation administered by anesthesiologists provided decreased anxiety score and propofol consumption. Patient satisfaction was increased, and patients reported a desire for the same protocol for recurrent procedures.
Conclusion
The present study may serve as the beginning of using music therapy for pain treatment in gastroenterology procedures in our hospital with/without sedation. Music and other non-pharmacological treatment methods must be remembered to increase patient comfort during enco/colonoscopies and other painful procedures.
Keywords: Colonoscopy, endoscopy, sedation, music
INTRODUCTION
Endoscopy and colonoscopy are major diagnostic and therapeutic tools for cancer screening. Fear and anxiety are very common concerns when patients need endo/colonoscopy. Usually sedation is needed for patient comfort and procedural success. In our endoscopy unit, most of the colonoscopies are performed under sedation either by gastroenterologists or by anesthesiologists. Non-pharmacological methods are usually beneficial for anxiolysis and pain reduction. Music, an ancient cure for pain and anxiety, has been used during operations and painful interventions in modern medical practice. There is evidence of increased patient satisfaction and decreased stress, anxiety, and pain with the help of music treatment (1–5). Anesthesiologist-associated sedation is considered time consuming and expensive (6–9). Music therapy can be an easy alternative.
In our endoscopy unit, non-pharmacological methods are not available. Therefore, the aim of the present study was to evaluate the effect of music treatment add-on sedation on drug consumption, anxiety, and pain severity for endo/colonoscopies.
MATERIALS AND METHODS
This was a randomized controlled double-blinded study conducted between June and October 2017 in a hospital gastroenterology unit after obtaining approval from the ethical department (ET: 5.6.2017/261).
Patients who were 18–70 years old, American Anesthesiologist Association (ASA) status I–III, and scheduled for endoscopy/colonoscopy were included in the study after verbal and written approval was obtained. Patients scheduled for endoscopic ultrasound or endoscopic retrograde colangiopancreaticography and having difficulty in communication were excluded from the study. In our endoscopy unit, patients were sedated either by gastroenterologists (conscious sedation) or by anesthesiologists (deep sedation). Music therapy was added to both groups of sedation. Data on age, sex, education level, marital status, and endoscopy type (endoscopy, colonoscopy, or endocolonoscopy) were recorded. Patients were randomized to music treatment or control groups by drawing of lots. An endoscopy personnel applied music administered through headphones so that the investigator and the endoscopist were blinded. All endoscopies were performed by experienced endoscopists.
In the music group, a questionnaire to identify the patient’s favorite music type was applied. The options included classical music, pop music, rap music, Turkish classical music, Turkish folk music, and traditional religious music. In the music group, patients listened to a 30-minute recording of their favorite music. In the control group, the headphone was on without any music.
Patient anxiety was measured by State-Trait Anxiety Inventory (STAI), and pain severity by Numerical Rating Scale (NRS) (0–10). All patients were monitored by electrocardiogram. Nasal O2 4 L/h was administered. Heart rate (HR), mean arterial pressure (MAP), and oxygen saturation were monitored before, during, and after the intervention. At the end of endoscopy, patients were transferred to the recovery room, and recovery was evaluated by Aldrete score (10). When Aldrete score was ≥9, patients were re-evaluated by STAI and NRS. Satisfaction was assessed by Likert scale (1, very satisfied; 2, satisfied; 3, undetermined; and 4, not satisfied). In addition, the patients’ choice to repeat endoscopy using the same protocol was rated by Likert scale (1, wants to repeat; 2, probably keen to repeat; 3, undetermined; and 4, does not want to repeat).
In the conscious sedation groups (Groups 1 and 2), only 2 mg of midazolam was administered. In the deep sedation groups (Groups 3 and 4), patients were administered 1–2 mg of midazolam, 0.1–0.3 mg/kg of ketamine, and 1–3 mg/kg of propofol. Incremental 20 mg of propofol was administered when the patient moved or felt pain. Total drug dose was recorded. Depth of sedation was rated according to the Ramsay Sedation Scale (10). Over sedation due to midazolam was treated by intravenous 0.2 mg of flumazenil.
Statistical analysis
Statistical analysis was performed by Statistical Package for Social Sciences (SPSS) software. Nominal values were evaluated for normality using histogram and Kolmogorov-Smirnov test. Non-parametric tests were used for non-normal distribution. Two group comparisons were made by Mann-Whitney U test, and four group comparisons by Kruskal-Wallis test. Definitive statistics were expressed as mean±standard deviation. Categorical data analysis was made by chi-square test. A p value <0.05 was accepted as statistically significant.
RESULTS
Patients in four groups were classified as Group 1, conscious sedation without music; Group 2, conscious sedation with music; Group 3, deep sedation without music; and Group 4, deep sedation with music. No significant difference was found between patients’ age, sex, marital status, and educational level. There were more women than men in all groups (Table 1). In Groups 2, 3, and 4, HR and MAP values were significantly higher before intervention compared to during and after intervention (Table 2).
Table 1.
Demographic data of patients
| Number of patients Male/Female |
Marital status Married/Single/Widow |
Age Median (min–max) |
p | |
|---|---|---|---|---|
| Group 1 | 25 4/21 |
21/2/2 | 46 (28–69) | NS |
| Group 2 | 33 13/21 |
26/6/1 | 44 (28–65) | NS |
| Group 3 | 55 26/29 |
50/5/0 | 44 (28–60) | NS |
| Group 4 | 41 15/26 |
26/14/1 | 42 (24–65) | NS |
Group 1: conscious sedation without music; Group 2: conscious sedation with music; Group 3: deep sedation without music; Group 4: deep sedation with music
NS: not significant
Table 2.
Comparison of HR and MAP among the groups (mean±SD)
| HR (bpm) MAP(mmHg) | Group 1 | Group 2 | Group 3 | Group 4 | p (in group) |
|---|---|---|---|---|---|
| Before intervention | 117.50±3.53 90.00±0.00 |
110±7.63 95±5.00 |
100±12.31 85±5.45 |
101.50±17.2 95±7.38 |
0.617 0.310 |
| During intervention | 117.50±3.53 90.00±0.00 |
90±12.58 90±2.88 |
95±13.02 85±6.02 |
83±12.70 81±7.69 |
0.0001 0.348 |
| After intervention | 115.00±7.07 90.00±0.00 |
90±2.88 90±2.88 |
95±12.49 85±6.02 |
80±10.44 80±5.60 |
0.0001 0.288 |
Group 1: conscious sedation without music; Group 2: conscious sedation with music; Group 3: deep sedation without music; Group 4: deep sedation with music
HR: heart rate; MAP: mean arterial pressure
Conscious sedation was performed under the supervision of gastroenterologists, and 2 mg of midazolam was administered. In Groups 1 and 2, drug dose was the same. In the deep sedation groups performed by anesthesiologists, drug doses were compared. Midazolam, propofol, and ketamine doses were significantly lower in Group 4 than in Group 3 (Table 3).
Table 3.
Comparison of drug doses among Group 3 and Group 4 (mean±SD)
| Group 3 | Group 4 | p | |
|---|---|---|---|
| Midazolam (mg) | 2±0 | 1.3±0.48 | 0.0001 |
| Ketamine (mg) | 19.63±2.69 | 16.12±4.45 | 0.0001 |
| Propofol (mg) | 204.54±42.24 | 146.34±32.38 | 0.0001 |
Group 3: deep sedation without music; Group 4: deep sedation with music
No patients in Groups 1 and 3 had pain before intervention. In these patients, post-intervention pain was significantly higher than before intervention (p=0.001). In Group 2 and 4 some patients had pain although mild before the procedure and was similar after the procedure (Figure 1).
Figure 1.
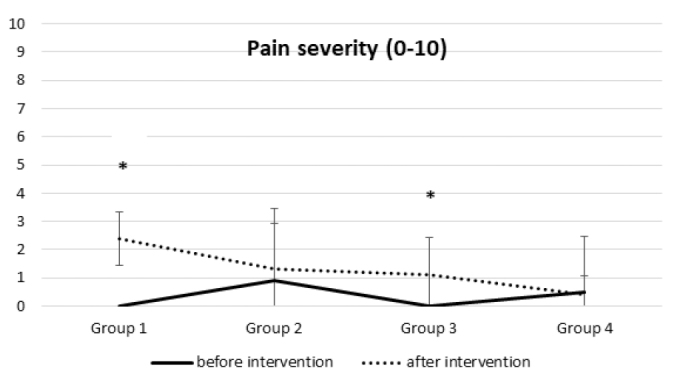
Comparison of pain severity of patients in the groups before and after intervention
Group 1: conscious sedation without music; Group 2: conscious sedation with music; Group 3: deep sedation without music; Group 4: deep sedation with music
*p<0.05
In Groups 2, 3, and 4, anxiety score was significantly lower after the procedure than before the procedure, but not in Group 1 (Table 4).
Table 4.
Comparison of anxiety of patients in the groups before and after intervention (mean±SD)
| Anxiety Score | Before intervention | After intervention | p |
|---|---|---|---|
| Group 1 | 48.88±7.63 | 48.80±7.61 | 0.56 |
| Group 2 | 50.72±9.15 | 46.42±7.15 | 0.0001 |
| Group 3 | 47.94±3.93 | 47.63±3.75 | 0.039 |
| Group 4 | 52.17±10.72 | 45.43±7.30 | 0.0001 |
Group 1: sedation without music; Group 2: sedation with music; Group 3: deep sedation without music; Group 4: deep sedation with music
Flumazenil was never needed in patients to reverse prolonged sedation or respiratory depression. Laryngospasm and respiratory depression were never recorded. No perforation, bleeding, and other complications due to endo/colonoscopy were observed.
In the sedation and music groups, patients were satisfied with their procedure and declared that they would prefer the same method for their next endoscopy. No significant difference was found in patient satisfaction between the groups.
No significant difference was found in patients according to sex for drug dose, anxiety score, and pain severity.
DISCUSSION
The hemodynamic alterations confirmed the benefit of music treatment added to sedation during endoscopy and/or colonoscopy. Pain after the procedure was higher than pain before the procedure in conscious sedation apart from music therapy. In deep sedation, patients’ anxiety score as rated by anesthesiologists was significantly lower after the procedure than before the procedure in the music group. In addition, sedative drug dose was lower in this group than in patients with deep sedation without music.
In the literature, it is common to find that music therapy decreases drug doses for sedation and decreases complications during colonoscopy (5,11). The European gastroenterology guide recommends patients with endoscopy to listen to their favorite music during the procedure and reported that propofol doses are decreased (5). The mechanism of music treatment is related to many stimuli antagonist to each other transferred to the cortex. The thalamus decreases the contaction of the muscles and levels of the adrenocorticotrophic hormone and alters the sympathetic system activation. Music stimulates the hypophysis to secrete more endorphins to help to decrease pain and anxiety. Music decreases pain and discomfort (11).
In studies, music has been used in different ways: one sedative music was administered to all patients or patients were asked to bring their favorite music along (12–15). Music before the intervention decreased pain, anxiety, and need for analgesia (16). In our study, music type was determined by a questionnaire, and patients listened to a 30-minute recording of their choice through headphones. Headphones were preferred to distract patients from environmental noises.
Since 1980, colonoscopy is performed under sedation using opioids and benzodiazepines. Midazolam and fentanyl are the most common drugs used for colonoscopy (17,18). Propofol is the preferred agent alone or combined with opioids. It may only cause an increased side effect due to higher doses (17). In our study, the routine gastroenterologist-controlled conscious sedation in our unit was 2 mg of midazolam for adult patients. There is an option of deep sedation by anesthesiologists when ketamine is added to midazolam, propofol, and fentanyl-based anesthesia. This method has been confirmed for hemodynamic stability, better quality sedation, and decreased propofol dose and recovery time (10,17,19).
It is known that propofol-based sedation increases patient satisfaction and endoscopy quality and shortens recovery. Propofol is not allowed to be used by gastroenterologists in the absence of anesthesiologists; anesthesiologist-controlled sedation increases cost (20,21). In some hospitals, non-anesthetist-administered propofol (NAAP) is common. Non-anesthesiologists must be aware that they must be educated for NAAP and basic and advanced cardiac life support. Naturally, NAAP must only be used for ASA I–II patients with low Mallampati scores (22). The ASA declares more complications with endoscopist-directed sedation; therefore, patients with difficult airway must be treated by anesthesiologists.
In our study, sedation decreased HR and MAP. Anxiety was decreased before and after the intervention in the sedation groups. In music-administered deep sedation patients, MAP and propofol dose was decreased, which is important to show the effect of music. In addition, pain severity was similar before and after the procedure attributed to music therapy, whereas post-procedure pain severity was increased in the groups without music therapy, suggesting the contribution of music. Similarly, decreased pain in music-treated patients are reported in the literature (12–14,23).
In some studies, there are sex-related differences to music therapy, although there are studies proving that sex difference is irrelevant in young population (24,25). Women are inclined to present higher anxiety scores and pain levels than men before the procedure (25,26). Although some authors declare more pain during colonoscopy in women than that in men (26,27), in our study, no difference between the groups due to sex was present. Women pelvic anatomy and longer intestines with loops sometimes cause difficulty during colonoscopy. In addition, gynecological operations and adhesions increase difficulty and decrease tolerance of patients during colonoscopy. After propofol administration for colonoscopy, women recovered faster than men did, although they needed higher a propofol dose (28). In our study, no difference in propofol dose was found between the sexes in the groups.
There are some limitations to the present study. Patients were informed about music therapy on the day of endoscopy, which was stressful. Men were fewer than women in our study, which may have prevented the differences due to sex. In some endoscopy studies, the quality of endoscopy was decided by cecum intubation time, endoscopy time, polyp recognition rate, endoscopist satisfaction, and recovery time (22); however, in our study, these were absent owing to rapid turnover. Aldrete score standardized patient recovery. Children were excluded in the present study, which might have been a valuable data.
In conclusion, gastroendoscopic interventions are mandatory to diagnose and treat various pathologies. Recurrent procedures may be needed during follow-up. Fear and anxiety of patients for these procedures are important factors to maintain comfort. In the present study, music add-on sedation was effective, decreased sedative drug doses, and increased patient satisfaction.
In our gastroenterology unit, music therapy has been used for the first time. We hope many patients can benefit from the encouraging effect of music with or without sedative drugs during endo/colonoscopies. There is a long way for the investigation of music and other non-pharmacological treatments, also in children.
Footnotes
Ethics Committee Approval: Ethics committee approval was received for this study from the Ethics Committee of Gazi University School of Medicine (ET: 5.6.2017/261).
Informed Consent: Written informed consent was obtained from the patients who participated in this study.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - D.A., M.C.; Design - D.C., B.U.Ç.; Supervision - D.A.; Data Collection and/or Processing - M.B.; Analysis and/or Interpretation - A.D.; Literature Search - M.B.; Writing Manuscript - D.A.; Critical Review - D.C.
Conflict of Interest: The authors have no conflicts of interest to declare.
Financial Disclosure: The authors declared that this study has received no financial support.
REFERENCES
- 1.White JM. Music as intervention: a notable endeavor to improve patient outcomes. Nurs Clin North Am. 2001;36:83–92. [PubMed] [Google Scholar]
- 2.Hsu CC, Chen SR, Lee PH, Lin PC. The effect of music listening on pain, heart rate variability, and range of motion in older adults after total knee replacement. Clin Nurs Res. 2017 doi: 10.1177/1054773817749108. https://doi.org/10.1177/1054773817749108 1054773817749108. [DOI] [PubMed] [Google Scholar]
- 3.Bradt J, Norris M, Shim M, Gracely EJ, Gerrity P. Vocal music therapy for chronic pain management in inner-city african americans: a mixed methods feasibility study. J Music Ther. 2016;53:178–206. doi: 10.1093/jmt/thw004. https://doi.org/10.1093/jmt/thw004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chlan L, Evans D, Greenleaf M, Walker J. Effects of a single music therapy intervention on anxiety, discomfort, satisfaction, and compliance with screening guidelines in outpatients undergoing flexible sigmoidoscopy. Gastroenterol Nurs. 2000;23:148–56. doi: 10.1097/00001610-200007000-00003. https://doi.org/10.1097/00001610-200007000-00003 [DOI] [PubMed] [Google Scholar]
- 5.Ovayolu N, Ucan O, Pehlivan S, et al. Listening to Turkish classical music decreases patients’ anxiety, pain, dissatisfaction and the dose of sedative and analgesic drugs during colonoscopy: a prospective randomized controlled trial. World J Gastroenterol. 2006;12:7532–6. doi: 10.3748/wjg.v12.i46.7532. https://doi.org/10.3748/wjg.v12.i46.7532 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lin OS. Sedation for routine gastrointestinal endoscopic procedures: a review on efficacy, safety, efficiency, cost and satisfaction. Intest Res. 2017;15:456–66. doi: 10.5217/ir.2017.15.4.456. https://doi.org/10.5217/ir.2017.15.4.456 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hagan KB, Thirumurthi S, Gottumukkala R, Vargo J. Sedation in the endoscopy suite. Curr Treat Options Gastroenterol. 2016;14(2):194–209. doi: 10.1007/s11938-016-0089-8. https://doi.org/10.1007/s11938-016-0089-8 [DOI] [PubMed] [Google Scholar]
- 8.Cohen LB, Delegge MH, Aisenberg J, et al. AGA Institute review of endoscopic sedation. Gastroenterology. 2007;133:675–701. doi: 10.1053/j.gastro.2007.06.002. https://doi.org/10.1053/j.gastro.2007.06.002 [DOI] [PubMed] [Google Scholar]
- 9.Fleischer D. Monitoring for conscious sedation: perspective of the gastrointestinal endoscopist. Gastrointest Endosc. 1990;36(Suppl 3):S19–22. [PubMed] [Google Scholar]
- 10.Türk HŞ, Aydoğmuş M, Ünsal O, et al. Ketamine versus alfentanil combined with propofol for sedation in colonoscopy procedures: a randomized prospective study. Turk J Gastroenterol. 2014;25:644–9. doi: 10.5152/tjg.2014.7014. https://doi.org/10.5152/tjg.2014.7014 [DOI] [PubMed] [Google Scholar]
- 11.Ko CH, Chen YY, Wu KT, et al. Effect of music on level of anxiety in patients undergoing colonoscopy without sedation. J Chin Med Assoc. 2017;80:154–60. doi: 10.1016/j.jcma.2016.08.010. https://doi.org/10.1016/j.jcma.2016.08.010 [DOI] [PubMed] [Google Scholar]
- 12.Bechtold ML, Puli SR, Othman MO, Bartalos CR, Marshall JB, Roy PK. Effect of music on patients undergoing colonoscopy: a meta-analysis of randomized controlled trials. Dig Dis Sci. 2009;54:19–24. doi: 10.1007/s10620-008-0312-0. https://doi.org/10.1007/s10620-008-0312-0 [DOI] [PubMed] [Google Scholar]
- 13.Nagata K, Iida N, Kanazawa H, et al. Effect of listening to music and essential oil inhalation on patients undergoing screening CT colonography: a randomized controlled trial. Eur J Radiol. 2014;83:2172–6. doi: 10.1016/j.ejrad.2014.09.016. https://doi.org/10.1016/j.ejrad.2014.09.016 [DOI] [PubMed] [Google Scholar]
- 14.Martindale F, Mikocka-Walus AA, Walus BP, Keage H, Andrews JM. The effects of a designer music intervention on patients’ anxiety, pain, and experience of colonoscopy: a short report on a pilot study. Gastroenterol Nurs. 2014;37:338–42. doi: 10.1097/SGA.0000000000000066. https://doi.org/10.1097/SGA.0000000000000066 [DOI] [PubMed] [Google Scholar]
- 15.Harikumar R, Kumar S. Colonoscopy and the role of music therapy: how to go about an ideal protocol? World J Gastroenterol. 2007;13:3272–3. doi: 10.3748/wjg.v13.i23.3272. https://doi.org/10.3748/wjg.v13.i23.3272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hole J, Hirsch M, Ball E, Meads C. Music as an aid for postoperative recovery in adults: a systematic review and meta-analysis. Lancet. 2015;386:1659–71. doi: 10.1016/S0140-6736(15)60169-6. https://doi.org/10.1016/S0140-6736(15)60169-6 [DOI] [PubMed] [Google Scholar]
- 17.das Neves JF, das Neves Araújo MM, de Paiva Araújo F, et al. Colonoscopy sedation: clinical trial comparing propofol and fentanyl with or without midazolam. Braz J Anesthesiol. 2016;66:231–6. doi: 10.1016/j.bjane.2014.09.014. https://doi.org/10.1016/j.bjane.2014.09.014 [DOI] [PubMed] [Google Scholar]
- 18.Trummel JM, Chandrasekhara V, Kochman ML. Anesthesia for colonoscopy and lower endoscopic procedures. Anesthesiol Clin. 2017;35:679–86. doi: 10.1016/j.anclin.2017.08.007. https://doi.org/10.1016/j.anclin.2017.08.007 [DOI] [PubMed] [Google Scholar]
- 19.Tuncali B, Pekcan YO, Celebi A, Zeyneloglu P. Addition of low-dose ketamine to midazolam-fentanyl-propofol-based sedation for colonoscopy: a randomized, double-blind, controlled trial. J Clin Anesth. 2015;27:301–6. doi: 10.1016/j.jclinane.2015.03.017. https://doi.org/10.1016/j.jclinane.2015.03.017 [DOI] [PubMed] [Google Scholar]
- 20.Hassan C, Rex DK, Cooper GS, Benamouzig R. Endoscopist-directed propofol administration versus anesthesiologist assistance for colorectal cancer screening: a cost-effectiveness analysis. Endoscopy. 2012;44:456–64. doi: 10.1055/s-0032-1308936. https://doi.org/10.1055/s-0032-1308936 [DOI] [PubMed] [Google Scholar]
- 21.Padmanabhan A, Frangopoulos C, Shaffer LET. Patient satisfaction with propofol for outpatient colonoscopy: a prospective, randomized, double-blind study. Dis Colon Rectum. 2017;60:1102–8. doi: 10.1097/DCR.0000000000000909. https://doi.org/10.1097/DCR.0000000000000909 [DOI] [PubMed] [Google Scholar]
- 22.Dumonceau JM, Riphaus A, Aparicio JR, et al. European Society of Gastrointestinal Endoscopy, European Society of Gastroenterology and Endoscopy Nurses and Associates, and the European Society of Anaesthesiology Guideline: Non-anaesthesiologist administration of propofol for GI endoscopy. Eur J Anaesthesiol. 2010;27:1016–30. doi: 10.1097/EJA.0b013e32834136bf. https://doi.org/10.1097/EJA.0b013e32834136bf [DOI] [PubMed] [Google Scholar]
- 23.Palakanis KC, DeNobile JW, Sweeney WB, Blankenship CL. Effect of music therapy on state anxiety in patients undergoing flexible sigmoidoscopy. Dis Colon Rectum. 1994;37:478–81. doi: 10.1007/BF02076195. https://doi.org/10.1007/BF02076195 [DOI] [PubMed] [Google Scholar]
- 24.Nater UM, Abbruzzese E, Krebs M, Ehlert U. Sex differences in emotional andpsychophysiological responses to musical stimuli. Int J Psychophysiol. 2006;62:300–8. doi: 10.1016/j.ijpsycho.2006.05.011. https://doi.org/10.1016/j.ijpsycho.2006.05.011 [DOI] [PubMed] [Google Scholar]
- 25.Nilsson U. The anxiety- and pain-reducing effects of music interventions: a systematic review. AORN J. 2008;87:780–807. doi: 10.1016/j.aorn.2007.09.013. https://doi.org/10.1016/j.aorn.2007.09.013 [DOI] [PubMed] [Google Scholar]
- 26.Björkman I, Karlsson F, Lundberg A, Frisman GH. Gender differences when using sedative music during colonoscopy. Gastroenterol Nurs. 2013;36:14–20. doi: 10.1097/SGA.0b013e31827c4c80. https://doi.org/10.1097/SGA.0b013e31827c4c80 [DOI] [PubMed] [Google Scholar]
- 27.Costa A, Montalbano LM, Orlando A, et al. Music for colonoscopy: A single-blind randomized controlled trial. Dig Liver Dis. 2010;42:871–6. doi: 10.1016/j.dld.2010.03.016. https://doi.org/10.1016/j.dld.2010.03.016 [DOI] [PubMed] [Google Scholar]
- 28.Riphaus A, Slottje M, Bulla J, et al. Women awaken faster than men after electroencephalogram-monitored propofol sedation for colonoscopy: A prospective observational study. Eur J Anaesthesiol. 2017;34:681–7. doi: 10.1097/EJA.0000000000000665. https://doi.org/10.1097/EJA.0000000000000665 [DOI] [PubMed] [Google Scholar]


