Abstract
Background/Aims
Good dietary habits, fluid intake, and regular exercise are considered to ease defecation although very few cases of chronic constipation can be managed through these approaches alone. Good defecation habits are recommended to avoid chronic constipation; however, the literature regarding this remains scarce. In this paper, we aimed to assess the association of bad habits concerning defecation, such as postponing, reluctance, or avoiding defecation anywhere but at home, with chronic constipation.
Materials and Methods
This was a cross-sectional observational study including subjects from a tertiary hospital taskforce. In total, 415 of 910 eligible subjects were randomly selected. A cluster of questionnaires easy to understand and fill out was distributed. The questionnaires included queries regarding demographic data; past medical history; the presence of constipation; and dietary, other lifestyle, and defecation habits. The Rome III criteria for chronic constipation were also recorded.
Results
In total, 24.3% of the subjects considered themselves constipated, and 26.5% fulfilled the Rome III criteria for constipation. There were obvious differences in constipation prevalence by sex (men 5% vs. women 31%). Fiber-rich diet, fluid intake, and exercise habits were not related to constipation. Defecation habits significantly correlated with the presence or absence of constipation: regular schedule (OR 0.39; CI 95% 0.23–0.67), persistently postponing defecation (OR 1.94; CI 95% 1.13–3.34), or avoiding defecation anywhere but at home (OR 2.38; CI 95% 1.4–4.1).
Conclusion
Compared with dietary habits, behavioral aspects surrounding defecation are more related to chronic constipation. Our results indicate that the modification of these bad habits may be the first step in chronic constipation treatment.
Keywords: Chronic constipation, Rome III criteria, prevalence, risk factors
INTRODUCTION
Constipation is a functional abnormality of defecation, which often has a multifactorial origin. It may present in different manners and may occult or even trigger important organic conditions, such as colorectal cancer or autoimmune diseases (1–3). Constipation can generate high health care costs: it is associated with a large number of consultations per year and may require multiple diagnostic tests, medications and other products for treatment, and sometimes even surgery (3–6).
However, the epidemiological data available on constipation are limited (3,7,8). Knowledge of its prevalence and risk factors associated with it are essential in attempts to provide adequate treatment resources, in the design of prevention programs, or in activities aimed at controlling the factors that facilitate its onset.
The aim of the present study was to assess the association of bad habits concerning defecation, such as postponing, reluctance, or avoiding defecation anywhere but at home, with chronic constipation.
MATERIALS AND METHODS
Design, subjects, and variables
A survey of the workforce in a tertiary hospital was performed. 910 surveys were randomly distributed among the 4466 working staff according to the needed population calculated for the study. The surveys were anonymous and self-completed. Every question was concrete, easily interpreted, and simple to answer by the general population, particularly the hospital staff. Nonetheless, a telephone number was provided in case any clarification was required.
The questionnaire comprised three parts:
Questions designed to collect data regarding age, sex, occupation, medical and surgical history, obstetric history among female subjects, evacuation characteristics (pain or straining on defecation), the number of bowel movements per day, and the stool size. Subjects were asked whether they felt constipated.
Questions designed to determine whether the Rome III criteria for functional constipation had been met, with the aim of objectively identifying constipated subjects (7).
Questions designed to collect information on hygiene-dietary habits that might influence the onset or persistence of constipation; the need to use laxatives or other aids for evacuation (enemas, suppositories, manual procedures, and the hygiene associated with them); whether daily water intake was >1500 ml; following of fiber-rich diets (25–30 g of fiber intake daily); regularity of exercise; mealtimes and defecation times; whether evacuation was ever postponed for social, work, or environmental reasons; rejection of evacuation outside the home; and the suffering from stress or emotional distress that might influence bowel movements.
An additional annexure was included with some explanations regarding the fiber intake and daily exercise to help participants with their answers. In this annexure, several examples of the fiber content in different types of food were provided. In addition, several definitions of exercise were provided, considering regular exercise to be three or more days a week of any type of aerobic exercise (walking/running, cycling, swimming, or other).
The questionnaires were considered complete when no missing answers were noted.
Consent from the participants regarding the publication of data for scientific purposes was requested. The study was approved by the institutional review board.
Statistical analysis
As the estimated prevalence of chronic constipation in the general population ranges between 2% and 28% (6), a population percentage of approximately 14% with a precision of 3.5% and a confidence interval (CI) of 95% was considered and a sample size of 378 subjects was calculated. Considering a response rate of at least 50%, 910 subjects were considered sufficient for the analysis, and therefore, randomly selected from the whole hospital workforce.
Qualitative results are presented as distribution frequencies. Prevalence was determined with binomial 95% CI. Quantitative results are represented as the mean±standard deviation, or in cases of asymmetry, as the median+interquartile range (IQR).
The association between qualitative variables was examined using the χ2 or Fisher’s exact test, as appropriate.
The association between the quantitative and qualitative variables was determined using the median test.
Univariate and multivariate logistic regression analyses were used to examine the association between explanatory variables and Rome III constipation criteria. Those variables in the univariate analysis with a significance of p<0.1 were included in the multivariate analysis.
Odds ratios (OR) were calculated along with their 95% (CI).
The null hypothesis was rejected when α error was <0.05.
All calculations were performed using the Statistical Package for Social Sciences (SPSS version 15.0.0; SPSS Corp.; Chicago, US).
RESULTS
A total of 426 subjects (46.8%) returned their questionnaires. Of these, 415 (45.6%) had been correctly completed and were usable.
For an estimated prevalence of 14% and a sample of 415 subjects recruited, a precision of 3.3% with a 95% CI was obtained.
In total, 119 (28.7%) subjects were males, and 296 (71.3%) were females. The mean subject age was 43.8±11.9 years. The age group that most commonly responded was 41–50 years (28.2%) followed by 51–60 years group (27.5%); in total 55.7% of the subjects was between 41–60 years age range. No difference was observed between the sexes in terms of age frequencies (p=0.213). Of the subjects, 181 were medical staff members, 78 were nurses, and 64 were auxiliary nurses, together reaching 77.8% of the recruited population.
Thyroid disease was the most common co-morbidity (reported by 8.7% of subjects) (Table 1). The use of medications for chronic diseases was recorded for each subject. Interestingly, only 8 subjects (1.9%) used fecal bolus-forming laxatives.
Table 1.
Description of the study cohort (n=415)
| n | % | ||
|---|---|---|---|
| Age (years) | 20–30 | 90 | 21.7 |
| 31–40 | 67 | 16.1 | |
| 41–50 | 117 | 28.2 | |
| 51–60 | 114 | 27.5 | |
| 61–70 | 27 | 6.5 | |
| Sex | Male | 119 | 28.7 |
| Female | 296 | 71.3 | |
| Professional category | Others | 8 | 1.9 |
| Administrative | 20 | 4.8 | |
| Auxiliary nurse | 64 | 15.4 | |
| Student | 6 | 1.4 | |
| Porter | 40 | 9.6 | |
| Nurse | 78 | 18.8 | |
| Doctor | 181 | 43.6 | |
| Technician | 18 | 4.3 | |
| Diabetes mellitus | 12 | 2.9 | |
| Neuropathy | 16 | 3.9 | |
| Thyroid disease | 36 | 8.7 | |
| Psychological abnormalities | 11 | 2.7 | |
| Women (n=296) | |||
| Previous deliveries | 169 | 56.7 | |
| Vaginal deliveries | 158 | 53.4 | |
| Cesarean section | 26 | 8.8 | |
| Abdominal hysterectomy | 18 | 6.1 | |
| Vaginal hysterectomy | 6 | 2 | |
Data related to previous gynecological/obstetric medical history of the female subjects are summarized in Table 1.
In total, 100 subjects [24.1% (95%CI 19.9–28.3)] reported feeling constipated. No differences were observed in this regard between the age groups although a significantly greater number of females felt constipated than of males (31.8% compared to 5%; p<0.001). The most common reason for reporting this condition was a low frequency of bowel movements (29%) although 63% reported no motive. Approximately 3% of the subjects reported their stools to be hard, and 2% reported the need to strongly strain to achieve evacuation. The mean duration of feeling constipated was 113±66 months.
Table 2 summarizes the data of subjects meeting of the Rome III criteria in the total sample and self-reported constipation.
Table 2.
Frequency of Roma III criteria met by the subjects (n=415)
| n | % | Males (n=6) | Females (n=94) | ||||
|---|---|---|---|---|---|---|---|
|
|
|||||||
| total | total | n | % | n | % | p | |
| a) Straining during at least 25% of defecations | 84 | 20.2 | 11 | 9.2 | 73 | 24.7 | 0.001 |
| b) Lumpy or hard stools in at least 25% of defecations | 124 | 29.9 | 25 | 21 | 99 | 33.4 | 0.012 |
| c) Sensation of incomplete evacuation in at least 25% of defecations | 84 | 20.2 | 12 | 10.1 | 72 | 24.3 | 0.001 |
| d) Sensation of obstruction/blockage in at least 25% of defecations | 46 | 11.1 | 5 | 4.2 | 41 | 13.9 | 0.005 |
| e) Manual maneuvers to facilitate at least 25% of defecations | 30 | 7.2 | 2 | 1.7 | 28 | 9.5 | 0.006 |
| f) Fewer than three defecations per week | 56 | 13.5 | 6 | 5 | 50 | 16.9 | 0.001 |
| Two or more criteria met | 110 | 26.5 | 15 | 12.6 | 95 | 32.1 | <0.001 |
| Loose stools rarely present without the use of laxatives | 123 | 29.6 | |||||
| Symptoms of irritable bowel syndrome | 50 | 12.6 | |||||
Frequency of Roma III criteria met by subjects with self-reported constipation (n=100)
| n | % | Males (n=6) | Females (n=94) | ||||
|---|---|---|---|---|---|---|---|
|
|
|||||||
| total | total | n | % | n | % | p | |
| a) Straining during at least 25% of defecations | 69 | 69 | 4 | 66.6 | 65 | 69.1 | 0.607 |
| b) Lumpy or hard stools in at least 25% of defecations | 76 | 76 | 3 | 50 | 73 | 77.7 | 0.148 |
| c) Sensation of incomplete evacuation in at least 25% of defecations | 58 | 58 | 5 | 83.3 | 53 | 56.4 | 0.195 |
| d) Sensation of obstruction/blockage in at least 25% of defecations | 40 | 40 | 2 | 33.3 | 38 | 40.4 | 0.544 |
| e) Manual maneuvers to facilitate in at least 25% of defecations | 23 | 23 | 0 | 0 | 23 | 24.5 | 0.199 |
| f) Fewer than three defecations per week | 41 | 41 | 1 | 16.6 | 40 | 42.6 | 0.210 |
| Two or more criteria met | 83 | 83 | 5 | 83.3 | 78 | 82.9 | 0.731 |
| Loose stools rarely present without the use of laxatives | 52 | 52 | |||||
| Symptoms of irritable bowel syndrome | 20 | 20 | |||||
Each Rome III criteria was met more often by females than by males, and females more often met two criteria than males (32.1% vs. 12.6%; p<0.001). The meeting of two or more Rome III criteria was related to the sensation of feeling constipated (p<0.001) (Fig. 1). According to the Rome III criteria, the sensibility, specificity, and positive and negative predicting powers of self-reported functional constipation are 0.9, 0.84, 0.83, and 0.91, respectively.
Figure 1.
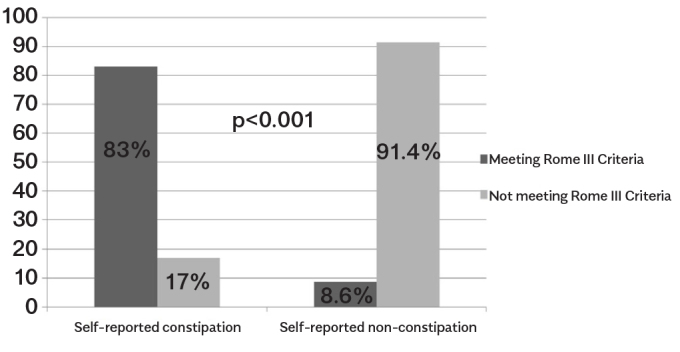
Association between meeting two or more Rome III criteria and “feeling constipated”
Table 3 shows the hygiene-dietary habits of the subjects by sex. Compared with males, females showed a significantly more irregular defecation timetable, were more likely to postpone defecation, to be less comfortable while defecating outside the home, and suffered more stress. All these factors were significantly (p<0.001) associated with meeting two or more Rome III criteria (Table 4).
Table 3.
Hygiene-dietary habits of the study cohort
| Males (n=6) | Females (n=94) | |||||||
|---|---|---|---|---|---|---|---|---|
|
|
||||||||
| n | % | n | % | n | % | p | ||
| Water intake >1500 mL | 241 | 58.1 | 78 | 65.5 | 163 | 55.1 | 0.05 | |
| Keeps regular mealtimes | 310 | 74.7 | 82 | 68.9 | 228 | 77 | 0.085 | |
| Fiber-rich diet | 305 | 73.5 | 82 | 68.9 | 223 | 75.3 | 0.18 | |
| Regular evacuation times | 218 | 52.5 | 75 | 63 | 143 | 48.3 | 0.007 | |
| Delays defecation | 180 | 43.4 | 42 | 35.3 | 138 | 46.6 | 0.035 | |
| Defecation outside the home | 248 | 59.8 | 95 | 79.8 | 153 | 51.7 | <0.001 | |
| Regular exercise | 187 | 45.1 | 60 | 50.4 | 127 | 42.9 | 0.164 | |
| Stress | 205 | 49.4 | 39 | 32.8 | 166 | 56.1 | <0.001 | |
| Type of stress | Work | 152 | 74.1 | 29 | 74.4 | 123 | 74.1 | |
| Family | 44 | 21.5 | 10 | 25.6 | 34 | 20.5 | ||
| Other | 9 | 4.4 | 0 | 0 | 9 | 5.4 | ||
Table 4.
Association between hygiene-dietary habits and the prevalence of meeting two or more Rome III criteria
| N° of Cases | Meeting Two or More Roma III Criteria (%) | p | ||
|---|---|---|---|---|
| Water intake >1500 mL | Yes | 56 | 23.2 | 0.076 |
| No | 54 | 31.0 | ||
| Keeps regular mealtimes | Yes | 78 | 25.2 | 0.286 |
| No | 32 | 30.5 | ||
| Fiber-rich diet | Yes | 77 | 25.2 | 0.333 |
| No | 33 | 30.0 | ||
| Regular defecation times | Yes | 33 | 15.1 | <0.001 |
| No | 77 | 39.1 | ||
| Delays defecation | Yes | 73 | 40.6 | <0.001 |
| No | 37 | 15.7 | ||
| Defecation outside the home | Yes | 43 | 17.3 | <0.001 |
| No | 49 | 41.2 | ||
| Regular exercise | Yes | 43 | 23.0 | 0.142 |
| No | 67 | 29.4 | ||
| Stress | Yes | 77 | 37.6 | <0.001 |
| No | 33 | 15.7 | ||
| Kind of stress | Work | 55 | 36.2 | |
| Family | 19 | 43.2 | ||
| Others | 3 | 33.3 |
Regarding the necessity of any aids for defecation, the use of laxatives was reported by 41 subjects (9.9% of the sample), enemas by 8 (1.9%), suppositories by 22 (5.3%), and manual facilitating maneuvers by 33 (8%). The reported maneuvers performed were vaginal compression (24.2%), perineal compression (51.1%), and fecal digitation (24.2%). All except one of those who needed manual maneuvers were females (10.8 % vs. 0.8%; p=0.001). The use of laxatives was also significantly higher among females than males (12.2% vs. 4.2%; p=0.014); no differences were observed in the use of enemas or suppositories (2% vs. 1.7%; p=0.816 and 6.4% vs. 2.5%; p=0.109, respectively).
Table 5 presents the independent factors associated with the meeting of two or more Rome III criteria, as determined by multivariate logistic regression, reflecting that female sex, postponing defecation, and suffering from any type of stress increase the risk of constipation and that regular defecation times and not avoiding defecation outside the home serve as prevention.
Table 5.
Univariate and multivariate analyses of different factors associated with Rome III criteria for the diagnosis of chronic constipation
| Univariate Analysis | Multivariate Analysis | ||||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| OR | IC95% | p | OR | IC95% | p | ||
| Age (years) | 0.441 | ||||||
| 20–30 | 1 | ||||||
| 31–40 | 1.91 | 0.86 – 4.25 | 0.111 | ||||
| 41–50 | 1.46 | 0.70 – 3.03 | 0.316 | ||||
| 51–60 | 1.87 | 0.89 – 3.92 | 0.099 | ||||
| 61–70 | 2.03 | 0.63 – 6.59 | 0.238 | ||||
| Sex (Female/Male) | 2.07 | 1.04 – 4.12 | 0.038 | 2.03 | 1.04 – 3.98 | 0.039 | |
| Thyroid disease (Yes/No) | 1.13 | 0.48 – 2.64 | 0.784 | ||||
| Regular defecation times | 0.38 | 0.22 – 0.65 | 0.000 | 0.39 | 0.23 – 0.67 | 0.001 | |
| Delays defecation | 2.06 | 1.19 – 3.57 | 0.010 | 1.94 | 1.13 – 3.34 | 0.016 | |
| Defecation outside the home | 0.4 | 0.23 – 0.71 | 0.004 | 0.42 | 0.24 – 0.72 | 0.005 | |
| Stress (Yes/No) | 2.05 | 1.19 – 3.52 | 0.009 | 2.01 | 1.18 – 3.42 | 0.011 | |
DISCUSSION
This study shows that compared with classically considered factors, such as fiber and water intake or regular exercise, defecation-related habits are more important factors associated with chronic constipation.
To the best of our knowledge, this is the first study that focuses on the possible association between defecation-related habits and constipation in the adult population, particularly those concerning postponing, reluctance, or just rejection to defecate anywhere but at home. In our experience, when assessing constipated patients, constipation is often due to defecation-related concerns rather than impaired bowel function or dyssynergic defecation; thus, these factors may be of capital importance.
The respondents reported the presence of a number of chronic health conditions, including high blood pressure, neuropathies, diabetes mellitus, psychological problems, and thyroid disease, and the use of medications to control these. Thyroid disease was the most commonly reported condition. The association between thyroid disease and digestive problems has been widely studied without unanimous conclusions. In the present population, no significant association was observed between thyroid disease and constipation (p=0.784). Moreover, there was no significant association between constipation and gynecological/obstetric history.
Approximately 24.1% of the subjects considered themselves to be constipated; this percentage is higher than that reported in other studies (8,9). No differences were observed between the age groups, but differences were recorded between the sexes (males 5% vs. females 31.8%). This discrepancy is in agreement with the results reported in most other studies (8–17) although this difference is much greater in the present population. The present results indicate that age is not related to a greater prevalence of constipation. Most studies have reported the prevalence of constipation to increase with age (9,12,14–17), while others support the present finding (11,18).
According to the Rome III criteria, 26.5% of the samples were considered constipated [with more female constipated per male (21.1% vs. 12.6%)]. Every single symptom considered in the Rome III criteria was more common in females than in males.
High rates of sensibility, specificity, and positive and negative predictive powers were achieved in the present analysis. Thus, “self-reported constipation” appears to be a sufficiently objective variable to be used in analyses; this is in corroboration with the previous reports (12), but this remains unmentioned in literature. The same results may be obtained by applying the recently published Rome IV criteria (19) because these criteria are superimposable with the previous criteria with the exception of opioid-induced constipation that was not considered in the previous version.
Generally, hygiene and dietary habits are considered to be very important in the onset and development of constipation. Fiber intake has been studied in detail using different methods; thus the obtained results are conflicting (15,20,21). Recently, Lawton (22) has reported a positive association between daily dietary fiber intake and the number of bowel movements, their consistency, and the feeling of well-being. Moreover, although water intake is easier to objectively record, conflicting results have been obtained regarding its effect on the onset of constipation (15,21). Increasing water and fiber intake is systematically recommended as a means of overcoming constipation, yet whether there is any real scientific evidence that water or fiber intake below certain limits is associated with the onset of constipation remains a matter of debate (23). Leung has suggested that these etiological factors may just be a myth and that much more research is required in this area (24). Contrary to previous evidence, in our population fiber or water intake, nor physical activity nor regular mealtimes were related to constipation. Maintaining regular mealtimes is probably the least well-known means of preventing constipation; certainly, little is mentioned in the literature in this regard. In the present study, 74.7% of the subjects claimed to be maintaining regular mealtimes, but this did not appear to affect constipation. Recommendations regarding water and fiber intake or the maintenance of regular mealtimes might help certain individuals, but a failure to do so is hardly exceptional; individualized measures followed by the careful evaluation of their success may provide better outcomes (12,14,16,21,23).
The importance of regular exercise has been previously examined, and the results should be interpreted with caution. Clear definitions of physical exercise are required. Only 45.1% of the subjects in the present population reported regular exercise, but no association of this habit with constipation was observed. Some authors have suggested that regular physical exercise has a beneficial effect on the intestinal transit (8,9,14), but there is no consensus in this regard (15).
Although little studied, it would appear that irregular defecation timetable, postponing defecation, and avoiding defecation outside the home increase the probability of constipation. Heaton et al. (18), who studied the general population via a questionnaire designed to establish the regularity of habits such as mealtimes, physical activity, and defecation timetable, have found that regularity in these factors had a beneficial effect on preventing constipation. The importance of these factors in our work was such that they appeared as risk factors for constipation in subjects with both self-reported and Rome III criteria constipation.
Many people are unable to defecate outside their homes, and thus, postpone evacuation until returning home. However, the need to defecate may not appear when reaching the front door; therefore, people with this problem may have very irregular defecation timetables that may result in constipation. Improving the hygiene conditions of toilets at workplaces might help to reduce the rejection of their use. In the present study, females were more affected by this factor than males, which may help explain the greater percentage of constipated females and those who used laxatives or other evacuation aids. Experimental work has revealed that the voluntarily postponing of defecation can reduce colonic transit speed, leading to fewer evacuation events with smaller/fewer stools (25).
Some authors have suggested that, when symptoms of obstruction to defecation are present, the risk of the slowing of colonic transit speed is 40.2%, while the opposite is almost zero (26). Thus, delays or difficulties in defecation appear to affect the colonic activity. Similar to other studies, the present study reported stress to be an important factor in altering the normal intestinal rhythm; stress was reported by 49.2% of the subjects and more so by females than by males (56.1% vs. 31.9%). The main cause of stress in both sexes was work-related tensions.
The association between psychological factors and intestinal problems has been much studied with respect to irritable bowel syndrome. Chan et al. (27) have suggested that an association exists between psychological or emotional factors and constipation and that the psychological and emotional profile of an individual can predict the physiopathological pattern of constipation and the duration of symptoms.
The reported percentage of subjects with constipation requiring medication differs across studies (16,26). In the present study, 9.9% of the subjects used laxatives, 1.9% used enemas, and 5.3% used suppositories to facilitate defecation. Only 1.9% of the subjects received fecal bolus-forming laxatives; this percentage is low given that nearly 26% of the subjects were constipated. Other studies have reported that 5%–50% of theoretically healthy subjects unnecessarily use laxatives (8,12,14). In addition, other authors have reported a greater use of these medications, probably because these are easily acquired, regarded as safe, and have few adverse effects (23).
In conclusion, approximately 26.5% of study subjects were constipated and 9.9% used laxatives. Constipation appears to be related to defecation-related habits, particularly maintaining the regular defecation times and rejecting the use of toilets in certain situations, which can easily be modified through education. The modification of these factors would have an important benefit for the prevention and treatment of constipation.
Acknowledgements
The authors wish to thank Mr. Adrian Burton for his help with English editing.
Footnotes
Ethics Committee Approval: Ethics committee approval was received for this study from the Local Ethical Committee.
Informed Consent: Written informed consent was obtained from all the patients who participated in this study.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - C.C., M.V., J.C.; Design - C.C., M.O., J.C. Supervision - C.C., M.O., M.V., J.V.; Materials - C.C., M.O.; Data Collection and/or Processingn - C.C., M.V., C.F.; Analysis and/or Interpretation - C.C., M.V., C.F., J.C.; Literature Search - C.C., M.V.; Writing - C.C., J.C.; Critical Reviews - C.F., J.C.
Conflict of Interest: The authors have no conflicts of interest to declare.
Financial Disclosure: The authors declared that this study has received no financial support.
REFERENCES
- 1.Ford AC, Talley NJ, Walker MM, et al. Increased prevalence of autoimmune diseases in functional gastrointestinal disorders: case-control study of 23471 primary care patients. Aliment Pharmacol Ther. 2014;40:827–34. doi: 10.1111/apt.12903. https://doi.org/10.1111/apt.12903 [DOI] [PubMed] [Google Scholar]
- 2.Guerin A, Mody R, Fok B, et al. Risk of developing colorectal cancer and benign colorectal neoplasm in patients with chronic constipation. Aliment Pharmacol Ther. 2014;40:83–92. doi: 10.1111/apt.12789. https://doi.org/10.1111/apt.12789 [DOI] [PubMed] [Google Scholar]
- 3.Gonzalez-Martinez MA, Ortiz-Olvera NX, Mendez-Navarro J. Novel Pharmacological Therapies for Management of Chronic Constipation. J Clin Gastroenterol. 2014;48:21–8. doi: 10.1097/01.mcg.0000436440.05887.02. https://doi.org/10.1097/01.mcg.0000436440.05887.02 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sun SX, DiBonaventura M, Purayidathil FW, et al. Impact of chronic constipation on health-related Quality of Life, Work Productivity, and Healthcare resource use: An analysis of the National Health and Wellness Survey. Dig Dis Sci. 2011;56:2688–95. doi: 10.1007/s10620-011-1639-5. https://doi.org/10.1007/s10620-011-1639-5 [DOI] [PubMed] [Google Scholar]
- 5.Higgins PD, Johanson JF. Epidemiology of constipation in North America: a systematic review. Am J Gastroenterol. 2004;99:750–9. doi: 10.1111/j.1572-0241.2004.04114.x. https://doi.org/10.1111/j.1572-0241.2004.04114.x [DOI] [PubMed] [Google Scholar]
- 6.Cook IJ, Talley NJ, Benninga MA, et al. Chronic constipation: Overview and challenges. Neurogastroenterol Motil. 2009;21(Suppl 2):1–8. doi: 10.1111/j.1365-2982.2009.01399.x. https://doi.org/10.1111/j.1365-2982.2009.01399.x [DOI] [PubMed] [Google Scholar]
- 7.Longstreth GF, Thompson WG, Chey WD, et al. Functional bowel disorders. Gastroenterology. 2006;130:1480–91. doi: 10.1053/j.gastro.2005.11.061. https://doi.org/10.1053/j.gastro.2005.11.061 [DOI] [PubMed] [Google Scholar]
- 8.Wald A, Scarpignato C, Mueller-Lissner S, et al. A multinational survey of prevalence and patterns of laxative use among adults with self-defined constipation. Aliment Pharmacol Ther. 2008;28:917–30. doi: 10.1111/j.1365-2036.2008.03806.x. https://doi.org/10.1111/j.1365-2036.2008.03806.x [DOI] [PubMed] [Google Scholar]
- 9.Sandler RS, Jordan MC, Shelton BJ. Demographic and dietary determinants of constipation in the US population. Am J Public Health. 1990;80:185–9. doi: 10.2105/ajph.80.2.185. https://doi.org/10.2105/AJPH.80.2.185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Garrigues V, Gálvez C, Ortiz V, et al. Prevalence of Constipation: Agreement among several criteria and evaluation of the diagnostic accuracy of qualifying symtoms and self-reported definition in a population-based survey in Spain. Am J Epidemiol. 2004;159:520–6. doi: 10.1093/aje/kwh072. https://doi.org/10.1093/aje/kwh072 [DOI] [PubMed] [Google Scholar]
- 11.Pare P, Ferrazzi S, Thompson WG, et al. An epidemiological Survey of constipation in Canada: Definitions, rates, demographics and predictors of health care seeking. Am J Gastroenterol. 2001;96:3130–7. doi: 10.1111/j.1572-0241.2001.05259.x. https://doi.org/10.1111/j.1572-0241.2001.05259.x [DOI] [PubMed] [Google Scholar]
- 12.Papatheodoridis GV, Vlachogiannakos J, Karaitianos I, et al. A greek survey of community prevalence and characteristics of constipation. Eur J Gastroenterol Hepatol. 2010;22:354–60. doi: 10.1097/MEG.0b013e32832bfdf0. https://doi.org/10.1097/MEG.0b013e32832bfdf0 [DOI] [PubMed] [Google Scholar]
- 13.Sonnenberg A. Physician visits in the United States for constipation: 1958–1986. Dig Dis Sci. 1989;34:606–11. doi: 10.1007/BF01536339. https://doi.org/10.1007/BF01536339 [DOI] [PubMed] [Google Scholar]
- 14.Everhart JE, Go VL, Johannes RS, et al. A longitudinal survey of Self-Reported bowel habits in the United States. Dig Dis Sci. 1989;34:1153–62. doi: 10.1007/BF01537261. https://doi.org/10.1007/BF01537261 [DOI] [PubMed] [Google Scholar]
- 15.Markland AD, Palsson O, Goode PS, et al. Association of Low Dietary Intake of Fiber and Liquids with Constipation: Evidence from the National Health and Nutrition Examination Survey. Am J Gastroenterol. 2013;108:796–803. doi: 10.1038/ajg.2013.73. https://doi.org/10.1038/ajg.2013.73 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Schmulson M, Francisconi C, Olden K, et al. Consenso Latinoamericano de Estreñimiento crónico. Gastroenterol Hepatol. 2008;31:59–74. doi: 10.1157/13116072. https://doi.org/10.1157/13116072 [DOI] [PubMed] [Google Scholar]
- 17.Suares NC, Ford AC. Prevalence of, and risk factors for, chronic idiopathic constipation in the community: Systematic review and Meta-analysis. Am J Gastroenterol. 2011;106:1582–91. doi: 10.1038/ajg.2011.164. https://doi.org/10.1038/ajg.2011.164 [DOI] [PubMed] [Google Scholar]
- 18.Heaton KW, Radvan J, Cripps H, et al. Defecation frecuency and timing, and stool form in the general population: a prospective study. Gut. 1992;33:818–24. doi: 10.1136/gut.33.6.818. https://doi.org/10.1136/gut.33.6.818 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lacy BE, Mearin F, Chang L, et al. Bowel Disorders. Gastroenterology. 2016;150:1393–407. doi: 10.1053/j.gastro.2016.02.031. https://doi.org/10.1053/j.gastro.2016.02.031 [DOI] [PubMed] [Google Scholar]
- 20.Elia M, Engfer MB, Green CJ, et al. Systematic review and meta-analysis: the clinical and physiological effects of fibre-containing enteral formulae. Aliment Pharmacol. 2008;27:120–45. doi: 10.1111/j.1365-2036.2007.03544.x. https://doi.org/10.1111/j.1365-2036.2007.03544.x [DOI] [PubMed] [Google Scholar]
- 21.Murakami K, Sasaki S, Okubo H, et al. Association between dietary fiber, water and magnesium intake and functional constipation among young japanese women. Eur J Clin Nutr. 2007;61:616–22. doi: 10.1038/sj.ejcn.1602573. https://doi.org/10.1038/sj.ejcn.1602573 [DOI] [PubMed] [Google Scholar]
- 22.Lawton CL, Walton J, Hoyland A, et al. Short Term (14 Days) Consumption of Insoluble Wheat Bran Fibre-Containing Breakfast Cereals Improves Subjective Digestive Feelings, General Wellbeing and Bowel Function in a Dose Dependent Manner. Nutrients. 2013;5:1436–55. doi: 10.3390/nu5041436. https://doi.org/10.3390/nu5041436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wald A. Constipation in the primary care setting: Current concepts and misconceptions. Am J Med. 2006;119:736–9. doi: 10.1016/j.amjmed.2006.03.025. https://doi.org/10.1016/j.amjmed.2006.03.025 [DOI] [PubMed] [Google Scholar]
- 24.Leung FW. Etiologic factors of chronic constipation- Review of the Scientific Evidence. Dig Dis Sci. 2007;52:313–6. doi: 10.1007/s10620-006-9298-7. https://doi.org/10.1007/s10620-006-9298-7 [DOI] [PubMed] [Google Scholar]
- 25.Klauser A, Voderholzer WA, Heinrich CA, et al. Behavioral Modification of Colonic Function. Can Constipation be Learned? Dig Dis Sci. 1990;35:1271–5. doi: 10.1007/BF01536418. https://doi.org/10.1007/BF01536418 [DOI] [PubMed] [Google Scholar]
- 26.Ribas Y, Saldaña E, Martí-Ragué J, et al. Prevalence and Pathophysiology of Functional Constipation Among Women in Catalonia, Spain. Dis Colon Rectum. 2011;54:1560–9. doi: 10.1097/DCR.0b013e31822cb5c2. https://doi.org/10.1097/DCR.0b013e31822cb5c2 [DOI] [PubMed] [Google Scholar]
- 27.Chan AOO, Cheng C, Hui WM, et al. Differing coping mechanisms, stress level and anorrectal physiology in patients with functional constipation. World J Gastroenterol. 2005;11:5362–6. doi: 10.3748/wjg.v11.i34.5362. https://doi.org/10.3748/wjg.v11.i34.5362 [DOI] [PMC free article] [PubMed] [Google Scholar]


