Abstract
Esophageal varices are about 10%-15% of UGIB. Over 90% of patients with cirrhosis develop portal hypertension (PHT), but not all patients with PHT and liver cirrhosis have esophageal varices. At the time of diagnosis, only 60% of patients with cirrhosis have esophageal varices. In the case of variceal bleeding suspects, vasoactive drugs should be given as soon as possible and before endoscopy. Balloon tamponade is used to obtain temporary hemostasis by direct compression of hemorrhagic varices. The variceal band ligation is already the first place in the treatment and prevention of variceal bleeding, but also in rebleeding prevention. TIPS is used as a rescue therapy after failure of drug and endoscopic therapy. The mortality assigned to the hemorrhagic episode is substantially, estimated at 13-19% of the overall mortality in hepatic cirrhosis. Current recommendations for the treatment of acute variceal bleeding are the use of combination therapy: vasoactive drugs, balloon tamponade, elastic ligation and TIPS, whose staging is done in various diagnosis and treatment algorithms.
Keywords: variceal bleeding, portal hypertension, endoscopy
Aim
The increased incidence of acute variceal bleeding and the often unpredictable evolution of them, with a high mortality rate has made their management involve the development of diagnostic and therapeutic algorithms. We propose a review of the literature on variceal bleeding in the article below.
Introduction
Esophageal varices are about 10%-15% of UGIB [1]. Upper gastrointestinal bleeding in the patient with cirrhosis is a frequent and dramatic complication [2]. Over 90% of patients with cirrhosis develop portal hypertension (PHT) [3]. Not all patients with PH and liver cirrhosis have esophageal varices. At the time of diagnosis, only 60% of patients with cirrhosis have esophageal varices [4]. The rate of esophageal varices is 6-8% per year, so that 90% of patients with cirrhosis have esophageal varices after 10 years since diagnosis, and after their appearance progress under the influence of increased portal blood pressure and portal blood flow [5].
The etiology is varied, and the frequency of etiology is the following: 60-65% of the hemorrhagic episodes are caused by esophageal varices, approximately 7% of gastric varices [6], 5-8% of hypertensive portal gastropathy [7], and 5-15% of gastric and duodenal ulcers [8]. The mortality attributed to the hemorrhagic episode is substantial, estimated at 13-19% of overall mortality in cirrhosis [9]. The mechanism of increasing portal pressure depends on the location and causes of portal hypertension [10]. Causes of portal hypertension are: portal, splenic and superior mesenteric vein thrombosis, primary biliary cirrhosis, sclerosis cholangitis, cirrhosis, veno-occlusive disease, Budd Chiari syndrome, congestive heart failure, vitamin A toxicity, idiopathic portal hypertension and infiltrative disorders (lymphoproliferative and myeloproliferative diseases) [10].
Physiopathology
Portal hypertension represents a pathological increase in portal vein pressure due to the difference in pressure gradient between the portal vein and the inferior vena cava [11]. This results from changes in portal resistance, along with changes in portal flow [10]. In portal hypertension, porto-systemic collateral decompresses portal circulation and gives rise to esophageal varices [11].
Portal pressure is most frequently determined by the hepatic vein pressure gradient (HVPG), which is defined as the difference between the wedged (WHVP) and the free hepatic venous pressures [12,13]. Esophageal varices develop from the deep vein plexus to the esophagus lumen [14]. The last 5cm of the esophagus is the predilection area of the rupture, and as the varices are larger, the rupture is larger and more severe [15]. Accumulation of 8 endoscopic studies with a total of 3,000 patients with cirrhosis indicated prevalence of variceal veins at 58.7% [16,17,18]. The incidence of variceal veins increase in 10 years from 8% to 58.7% [67]. Extended varices from the esophagus to gastric fornix and the greater curvature have an increased risk of bleeding, especially in patients with Child B and Child C cirrhosis [19,20].
In the production of splanchnic vasodilatation from liver cirrhosis occurs various mediators [21], but the dominant role is played by nitric oxide [22,23]. Increased hepatic venous pressure gradient over 12mm Hg develops esophageal varices and there is a risk of gastroduodenal bleeding [24,25,26] and the pressure over 16mm Hg is the discriminative value at which survival decrease [25]. Varicose rupture occurs most frequently at 2 years after confirmation of the diagnosis of cirrhosis [27,28,29]. In order to quantify the risk of varicose tears, numerous classifications have been proposed, taking into account vein diameter, color and extension in height, presence of the associated "red signs" [15,22,29,30,31,32,33]. Northern Italian Endoscopy Club (NIEC) studies concluded predictability bleeding using endoscopic and Child clinical classification data [29].
Large varices over 5 mm associated with "red signs" presence have increased risk of bleeding, 73% of 7% in small varices [35]. The severity of bleeding produced by variceal veins tear is dependent on hemodynamic factors and hemostatic disorders due cirrhosis [22,30,35,36,37].
It is known that 20% of cirrhotic patients with cataclysmic upper gastrointestinal bleeding die before being admitted to hospital [38]. Bleeding may be severe by the deficient synthesis of coagulation factors by the liver, by decreased platelets secondary to hypersplenism [37]. A predictive factor is the gastric rebleeding present in 50% of bleeding cirrhosis [28,36,39,40,41,42]. The risk of rebleeding in cirrhosis is 70% per year and is associated with a 50% mortality rate for each episode [39]. In the early resumption of hemorrhage, the infection is present in 66% of the cirrhosis patients [29,42,43,44]. The introduction of antibiotic prophylaxis into the therapeutic protocol as soon as hemorrhage was triggered is justified, because infection induces rebleeding and insufficient control of bleeding [43,45,46,47,48].
Positive diagnosis
Patients with UGIB should be promptly and correctly evaluated clinically to provide early key decisions on the initial assessment of the patient with gastrointestinal bleeding. Medical history, physical examination, and initial laboratory values are important in assessing resuscitation, triage, endoscopic exploration, consultation and prognosis requirements [49]. A history of alcoholism increases the risk of cirrhosis, portal hypertension, and bleeding from esophageal varices. In cirrhotic patients, approximately 60% of the initial bleeding is from esophageal varices [50].
Laboratory assessment is necessary for detection of blood count (Hemoglobin, Hematocrit, White bool cells, Platelets-confirms the blood loss, hepatic function (transaminases, bilirubin level, alkaline phosphatase, gamma glutamyl transferase, coagulation times), kidney function (creatinine level, blood urea nitrogen), ionogram for the detection of the hydroelectrolytic imbalance occurring by the hemorrhagic shock, but also for establishing the current biological status under the conditions of a bleeding. All patients with non-variceal upper gastrointestinal bleeding and anticoagulant treatments should be evaluated for coagulopathy (prothrombin index, partial thromboplastin time, platelet count).
A low hematocrit reflects the degree of blood loss after 24 hours or more of a upper gastrointestinal bleeding. The value of hematocrit in dynamics is useful for assessing the degree of severity of an UGIB, but should be combined with hemodynamic assessment because hyperhydration falsely decrease hematocrit. Assessment of central venous pressure or Swan-Ganz catheter reflects volemia rather than physical examination or hematocrit levels [51,52].
Our experience includes a total of 98 cases of acute variceal bleeding representing 21% of the total UGIB hospitalized cases over a 6-year period. The incidence is higher for males (74%) and for rural areas. The average age was around 57, the most common cause of varicella HDS was ethanolic cirrhosis (73%).
Pathological associations have been with cardiovascular diseases that were an aggravating factor in the evolution and prognosis of acute variceal bleeding. Also in 17% of AVB was triggered by antiaggregant and anticoagulant drugs. In establishing the positive diagnosis I took into account clinical manifestations-the exteriorization through hematemesis and/or melena; patient history-liver cirrhosis, history of hemorrhagic episodes due to rupture of esophageal varices or hypertensive portal gastropathy; early or delayed endoscopy.
The form of exteriorization was predominantly hematemesis and melena, and most of the cases were admitted in the first 48 hours with a maximum of 6-24 hours (39%).
Superior endoscopy is the only way to diagnose esophageal varices and is obligatorily when a liver cirrhosis is diagnosticated, considering that esophageal varices are present in 60% of decompensated cirrhosis and 30% of patients with compensated liver cirrhosis [37]. Platelet count decrease, splenomegaly, portal vein dilatation, perisplenic circulation or ultrasound visible collateral, reduced portal flow velocity at Echo-Doppler may be suggestive of portal hypertension [54]. Regarding esophageal varices, regardless of the staging, the endoscopic description of the esophageal varices correlates the increased risk of bleeding with two criterion: the size and the form of the variceal vein. Baveno Consensus since 1996 considers that a classification in large and small varices is a simple and practical classification [54]. Some studies have shown that appearance and size of variceal veins are indicators of the risk of bleeding. Large variceal veins indicate a higher risk of bleeding [55,56].
The endoscopic examination for diagnostic purposes was performed in 23 cases (23.4%) in our study (Fig.1 ).
Figure 1.
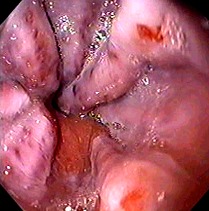
Endoscopic appearance of esophageal varices (Department of Gastroenterology Craiova)
In patients with liver cirrhosis without esophageal varices, superior endoscopy is recommended to be repeated at 2-3 years, but at patients with cirrhosis and small esophageal varices endoscopy will repeat at 1-2 years, to assess varicose progression [54].
Acute variceal bleeding stops spontaneously in about 50% of cases, but after stopping hemorrhage, either spontaneously or by therapeutic means, the risk of rebleeding is increased in the first 10-14 days, and maximum in the first 72 hours after the hemorrhagic event [57].
On our statistics, hemorrhage continued and/or repeated in 38.7% from which the favorable outcome was in 50% of these cases.
Postprandial hyperemia, physical strain, alcohol consumption, or conditions that cause increased intra-abdominal pressure are associated with increased portal pressure, variceal vein dilatation, and increased risk of variceal bleeding, but hemorrhagic episodes are more frequent at night when portal pressure is maximum [54].
Transfusion
Patients with variceal bleeding are conservatively transfused to a hematocrit of only 27% to avoid exacerbation of bleeding by increasing portal pressure [58]. Similarly, in a small, randomized, controlled study, 25 patients with cirrhosis that had been transfused aggressively with transfusion of at least 2 packed red blood cells had a significantly higher risk of bleeding than the 25 patients with hepatic cirrhosis that has been transfused conservatively, with only transfusion for shock or a hemoglobin less than 8g/dl [59]. A 25% and 27% hematocrit is generally appropriate to maintain tissue oxygenation in young healthy patients without comorbidities [60]. Elderly patients, however, have less cardiorespiratory reserves and can’t tolerate mild anemia, e.g. a hematocrit less than 28% was associated with myocardial ischemia in elderly men who had prostatectomy [61].
Blood transfusion was the rule for patients with severe and very severe AVB (63.2% of cases). We did transfuse patients with hemoglobin values less than 8g/dl. The amount of blood transfused ranged from one unit to over 10 units for very severe cases or rebleeding or requiring surgery.
Treatment
Endoscopic therapy
The variceal band ligation already occupied the first place in the treatment and prevention of bleeding variceal veins, but also in resuscitation prevention. This technique is also used in active gastric varices to banding both in retroflexed and non-retroflexed positions, with only four bands sufficient to apply in one session after the results of most studies. [62].
The use of band ligatures in acute bleeding shows a 83-100% hemostasis rate. [63,64,65]. Some authors, after conducted studies on 18 patients, believe that combined therapy, band ligation with sclerotherapy, shows a 100% hemostasis rate. [64,65,66], but this combined therapy presents a high risk of iatrogenic complications, technical skill and increased procedure time.
We applied elastic band ligations to patients with bleeding variceal veins to stop bleeding in 10.7% of cases (Fig.2). Balloon tamponade is used to obtain temporary hemostasis by direct compression of hemorrhagic varices.
Figure 2.
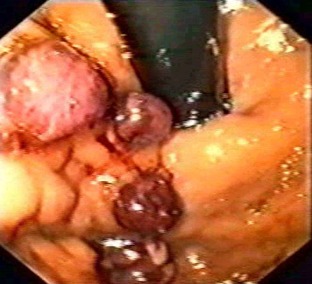
Variceal elastic band ligation (Department of Gastroenterology Craiova)
Endoclips are increasingly used in bleeding from esophageal varices [67], and endoloop has been used in gastric variceal therapy [68]. Histoacryl Injection (N-butyl-2-cyanoacrylate) is used in the treatment of acute variceal bleeding, but may be complicated by arterial emboli and perforations [69,70].
Drug treatment
Octreotide, a somatostatin analogue, is typically used to reduce the risk of bleeding in esophageal varices because it inhibits mesenteric vasodilation induced by glucagon, and in high dose intravenous decrease acid secretion [71]. Octreotide therapy is initiated in patients with acute variceal bleeding, severe hepatic disease, a history of variceal bleeding, history of alcoholism, or modified hepatic biochemical parameters [72]. Octreotide replaced vasopressin as a pharmacotherapy for variceal bleeding due to uncommon and less severe side effects [72].
Glypressin (terlipressin) at doses of 1-2mg intravenous every 4 hours for 5 days produces a fall in intravascular pressure at 2 minutes and controls 80% of hemorrhages at 12 hours [73]. The meta-analysis of randomized trials revealed a significant increase in controlled bleeding and a significant decrease in mortality [5].
Our experience is limited in Glypressin therapy, treating only 7 cases, with favorable responses to lower portal blood pressure, clinically evidenced by stopping bleeding.
PPI adjuvant therapy following variceal endoscopic ligation has a similar effect to beta blockers in hemostasis and rebleeding prevention. Patients with acute variceal bleeding have benefited in over half of cases of PPI antisecretory therapy and sensitive equal doses of monotherapy with H2 antagonists and associated therapy. In patients treated for AVG, bleeding continued or repeated in 39% of cases (Fig.3).
Figure 3.
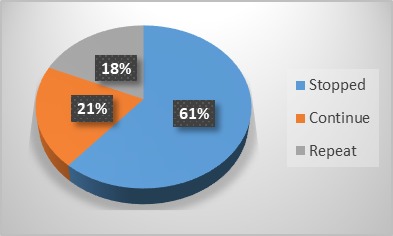
Response to conservative therapy
Surgical treatment was applied only in 6 cases due to the lack of response to medical treatment and the impossibility of performing endoscopic treatment.
Evolution of cases was favorable in 58 cases and unfavorable by repeating bleeding and lack of therapeutic response in 19 cases as well as signs of severe hepatic failure with exitus in 21 cases.
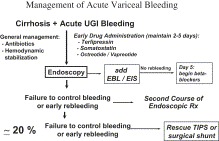
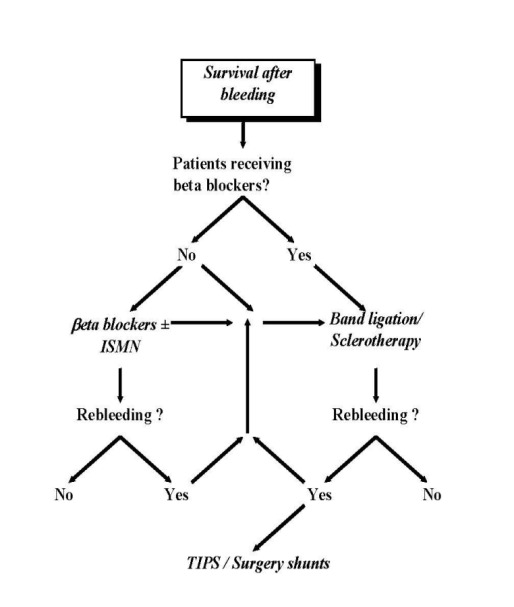
Here are some of the treatment algorithms that we considered most useful in the diagnosis and treatment of acute variceal bleeding (Fig.4,5, 6) [8]:
Figure 4.
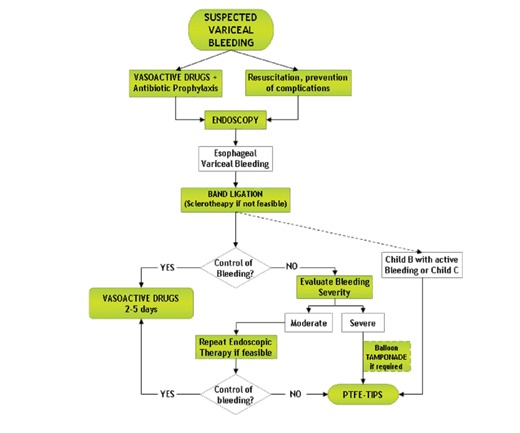
Flow chart showing the management of an AVB episode [75]
Figure 5.
Management of acute variceal bleeding [76]
Figure 6.
Algorithm of management of acute variceal bleeding [8]
Regarding prophylaxis of recurrent bleeding through esophageal varices (after the first hemorrhage), the following treatment algorithm is used in all patients immediately after the acute episode that should be initiated early as soon as possible (Fig.7) [8]:
Figure 7.
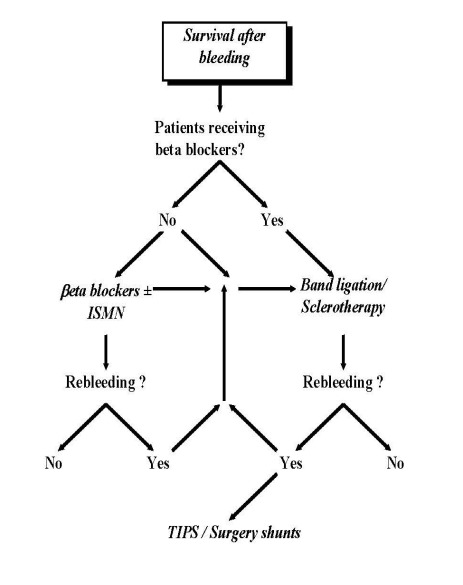
. Algorithm of survival after bleeding [8]
Beta non-selective blockers are elective treatment. Meta-analyzes of randomized trials have shown a significant decrease in rebleeding, first bleeding incidence, near significant mortality, and significant increase in survival [5].
Isosorbide-5-mononitrate has similar efficacy to propranolol [76]. The association of non-selective beta blockers with isosorbide-5-mononitrate has frequent adverse effects and increased noncompliance. And the association of nadolol with isosorbide-5-mononitrate has greater efficacy compared to sclerotherapy [76].
Portal gastropathy
Portal gastropathy is treated by reducing pharmacologic portal hypertension with propranolol, radiologically with TIPS, or surgical with portosystemic shunts [77]. In one study, only 35% of patients treated with propranolol bleed, compared with 62% of the placebo-treated patients [78]. In a study of 40 patients who had mild portal gastropathy, the blood transfusion requirement decreased by 89% after TIPS [79]. Patients with portal gastropathy associated with advanced hepatic insufficiency who have bleeding should undergo a liver transplant [80].
Treatment of portal hypertension includes the prevention of variceal bleeding in non-bleeding patients, the treatment of bleeding episodes and the prevention of resuscitation in patients who have survived an episode of bleeding in esophageal or gastric varices. So far, there is no effective treatment to prevent the development of varices [81].
Screening to prevent first bleeding from esophageal varices
Current guidelines recommend that each patients with cirrhosis diagnosed be endoscopically tested for varices [82], because none of the studies that indicated the use of non-invasive tests (platelet counts and abdominal ultrasound data) can’t have a potential for use in selecting a higher risk group of patients with esophageal varices [4,83,84,85,86].
Two cost-effectiveness analysis have revealed that beta-blockers therapy in all patients with cirrhosis without endoscopic screening is more cost-effective than endoscopic universal screening and therapy use than in patients with large varices. [87,88]
A third study suggested that empiric beta-blockers therapy is more profitable and effective only in patients with decompensated cirrhosis [89].
The recommendation of current guidelines is to repeat endoscopy at 2-3 years after first endoscopy in patients without varices [82]. The expected incidence of large or bleeding varices in these patients is less than 10% at 3 years [56,90,91]. In centers where hemodynamic hepatic studies are available, HVPG is advisable to measure, and values above 10mmHg indicate a more rapid progression to complications of cirrhosis and require shorter surveillance intervals [92].
In patients with small varices at initial endoscopy, the purpose of further exploration is to detect the progression of small varices to large because of prognostic and therapeutic implications. With a variceal progression rate of 10-15% per year, endoscopy should be repeated every 1-2 years in patients with small varices [82]. In patients with advanced cirrhosis, endoscopic red signs or alcoholic etiology of cirrhosis, a 1-year interval for endoscopy is recommended [90,91].
Treatment to prevent first esophageal bleeding
12 trials of beta-adrenergic blocking test were performed to prevent first bleeding and the result of these studies showed that the use of nadolol or propranolol therapy significantly reduces the risk of bleeding from 25% to 15% over a period of 2-year follow-up, and mortality from 27% to 23% [39]. The benefit of treatment has been demonstrated in patients with moderate or large varices (>5mm), with or without ascites or with normal or low liver function [39,93]. Beta blockers reduce the progression of varices from low to high and decrease the incidence of variceal bleeding in patients with small varices [94]. We have administered to all patients with acut variceal bleeding in the absence of hemorrhagic shock, beta-blocker -propranolol treatment in 37 patients (37.7%).
The therapeutic dose of beta-adrenergic blockers is established by the gradual increase of the dose to reaching the maximum tolerated dose, being more effective than titration against cardiac rhythm to achieve a reduction of approximately 25% [95]. Beta-adrenergic blockers therapy should be maintained indefinitely because its discontinuation increases the risk of variceal bleeding as occurs in untreated patients [96].
Adding monosodium isosorbide to beta blocker therapy improves the reduction of portal pressure [97,98]. One study compared nadolol versus nadolol plus isosorbide mononitrate treatment and demonstrated a lower rate of first bleeding in the association group, which was maintained after 55 months of follow-up but without a survival advantage [99]. A randomized trial failed to confirm these results [100], and current guidelines do not recommend combinated therapy in primary prophylaxis [82].
Prevention of rebleeding in esophageal varices
Pharmacological treatment is based on the use of non-selective beta-adrenergic blocker agents [101], and some studies have permanent found benefit of beta-adrenergic blockers regarding re-bleeding (63% to 42%) and mortality (from 27% to 20%) [39]. If there is no reduction in HVPG of more than 20% initial value or below 12 mm Hg, isosorbide mononitrate can be added and a drop in portal pressure results at a third of patients who did not respond to monotherapy with beta-blockers [102].
Endoscopic sclerotherapy of variceal esophagus reduces rebleeding and death [103], but it has been replaced with variceal endoscopic ligation due to the effectiveness of endoscopic ligatures and the prevention of endoscopic postsclerotherapy complications. Recent studies have demonstrated the effectiveness of combining beta blockers with variceal endoscopic ligation, and variceal endoscopic ligation in monotherapy should be used by patients with contraindications to beta adrenergic blockers [104].
We used too propranolol of principle to prevent rebleeding without having the opportunity to monitor the evolution of this treatment over time.
Conclusions
Despite the application of current recommendations of treatments, 10% to 15% of cirrhotic patients still have treatment failure, drugs and endoscopic therapy. It is very important to identify patients with different risks, from the patients with cirrhosis which can developed AVB.
Conflict of interests
The author declares no conflict of interests
Glossary
| Abbreviation | Expansion |
|---|---|
| AVB | acute variceal bleeding |
| UGIB | upper gastrointestinal bleeding |
| EBL | endoscopic band ligation |
| HVPG | hepatic venous pressure gradient |
| PHT | portal hypertension |
| TIPS | transjugular intrahepatic portosystemic shunt |
| NIEC | Northern Italian Endoscopy Club |
References
- 1.Jutabha R, Jensen DM. Management of upper gastrointestinal bleeding in the patient with chronic liver disease. Medical Clinics of North America. 1996;80(5):1035–1068. doi: 10.1016/s0025-7125(05)70479-x. [DOI] [PubMed] [Google Scholar]
- 2.Saftoiu A, Ciurea E. Hemoragiile digestive superioare non-variceale în gastroenterologie și hepatologie. București: Ed Medicală ; 2003. pp. 664–673. [Google Scholar]
- 3.Garcia-Pagan JC, Bosch J. Medical treatment of portal hypertension. Bailliere Gastroenterol. 2000;14(6):895–909. doi: 10.1053/bega.2000.0137. [DOI] [PubMed] [Google Scholar]
- 4.D'Amico G, Garcia-Tsao G, Cales P, Escorsell A, Nevens F, Cestari R. Diagnosis of portal hypertension: how and when . In: Franchis R, editor. Portal Hypertension. 3. Oxford, UK: Blackwell Science; 2001. pp. 36–64. [Google Scholar]
- 5.D'Amico G, Pagliaro L, Bosch J. The treatment of portal hypertension: A meta-analytic review. Hepatology. 1995;22(1):332–354. doi: 10.1002/hep.1840220145. [DOI] [PubMed] [Google Scholar]
- 6.Sarin SK, Lahoti D, Saxena SP, Murthy NS, Makwana UK. Prevalence, classification, and natural history of gastric varices: a long-term follow-up in 568 portal-hypertension patients. Hepatology. 1992;16(6):1343–1349. doi: 10.1002/hep.1840160607. [DOI] [PubMed] [Google Scholar]
- 7.Gostout CJ, Viggiano TR, Balm RK. Acute gastrointestinal bleeding from portal-hypertensive gastropathy: prevalence and clinical features. Am J Gastroenterol. 1993;88(12):2030–2033. [PubMed] [Google Scholar]
- 8.Pagliaro L, D'Amico G, Luca A, Pasta L, Politi F, Aragona E, Malizia G. Portal hypertension: diagnosis and treatment. J Hepatol. 1995;23(Suppl 1):36–44. [PubMed] [Google Scholar]
- 9.Ginés P, Quintero E, Arroyo V, Terés J, Bruguera M, Rimola A, Caballería J, Rodés J, Rozman C. Compensated cirrhosis: natural history and prognostic factors. Hepatology. 1987;7(1):122–128. doi: 10.1002/hep.1840070124. [DOI] [PubMed] [Google Scholar]
- 10.Garcia-Tsao G. Portal hypertension. Curr Opin Gastroenterol. 2006;22(3):254–262. doi: 10.1097/01.mog.0000218962.93806.9a. [DOI] [PubMed] [Google Scholar]
- 11.Toubia N, Sanyal AJ. Portal Hypertension and Variceal Hemorrhage. Med Clin N Am. 2008;92(3):551–574. doi: 10.1016/j.mcna.2007.12.003. [DOI] [PubMed] [Google Scholar]
- 12.Garcia-Pagan JC, Groszmann RJ, Bosch J. Measurement of portal pressure. Clin Gastroenterol Hepatol. 2005:981–981. [Google Scholar]
- 13.Groszmann RJ, Glickman M, Blei AT. Wedged and free hepatic venous pressure measured with a balloon catheter. Gastroenterology. 1979;76(2):253–258. [PubMed] [Google Scholar]
- 14.Kitano S, Terblanche J, Kahn D, Bornman PC. Venous anatomy of the lower esophagus in portal hypertension: practical implication. Br J Surg. 1986;73(7):525–531. doi: 10.1002/bjs.1800730704. [DOI] [PubMed] [Google Scholar]
- 15.Dagradi AE. The natural history of esophageal varices in patients with alcoholic liver cirrhosis. An endoscopic and clinical study. Am J Gastroenterol. 1972;57(6):517–520. [PubMed] [Google Scholar]
- 16.Pascal JP. Histoire naturelle de l'hémorragie digestive chez la maladie cirrhotique. Gastroenterol Clin Biol. 1990;14:B7–B7. [PubMed] [Google Scholar]
- 17.Cales P, Pascal JP. Histoire naturelle des varices oesophagiennes au cours de la cirrhose (de la naissance a la rupture) Gastroenterol Clin Biol. 1988;12:245–254. [PubMed] [Google Scholar]
- 18.Groupe d' Etude de la Prophylaxie Primaire. Cales P. Facteurs prédictifs de la premiere hemorragie digestive et de la mortalite chez les malades cirrhotiques avec varices oesophagiennes. Gastroenterol Clin Biol. 1989;13:54–59. [PubMed] [Google Scholar]
- 19.Sarin SK, Kumar A. Gastric varices: profile, classification and management. Am J Gastroenterol. 1989;84(10):1244–1249. [PubMed] [Google Scholar]
- 20.Zaman A, Hapke R, Folra K, Rosen HH, Benner K. Factors predicting the presence of esophageal or gastric varices in patients with advanced liver disease. Am J Gastroenterol. 1999;94(11):3292–3296. doi: 10.1111/j.1572-0241.1999.01540.x. [DOI] [PubMed] [Google Scholar]
- 21.Erikson AS, Gretzer C, Wallerst DT. Elevation of citokines in peritoneal fluid and blood in patients with liver cirrhosis. Hepatogastroenterology. 2004;51(56):505–509. [PubMed] [Google Scholar]
- 22.Bancu S.> . Tratamentul chirurgical al hipertensiuni portale. 2. București: Ed Universitară "Carol Davila" ; 2003. [Google Scholar]
- 23.Vallace P, Moncada S. Hyperdynamic circulation in cirrhosis: a role for nitric oxid. Lancet. 1991;337(8744):776–778. doi: 10.1016/0140-6736(91)91384-7. [DOI] [PubMed] [Google Scholar]
- 24.Bosch J, Garcia-Pagan JC. Complications of portal hypertension. J Hepatol. 2000;32(1 Suppl):141–156. doi: 10.1016/s0168-8278(00)80422-5. [DOI] [PubMed] [Google Scholar]
- 25.Dittrich S, Alves De Mattos A, Becker M, Goncaves DM, Cheinquer H. Role of hepatic hemodynamic study in the evolution of patients with cirrhosis. Hepatogastroenterology. 2003;50(54):2052–2056. [PubMed] [Google Scholar]
- 26.Garcia-Tsao G, Groszmann RJ, Fisher RL, Conn HO, Atterbury CE, Glickman M. Portal presure, presence of gastroesophageal varices and variceal bleeding. Hepatology. 1985;5(3):419–424. doi: 10.1002/hep.1840050313. [DOI] [PubMed] [Google Scholar]
- 27.Cales P, Pascal JP. Histoire naturelle des varices oesophagiennes au cours de la cirrhose (de la naissance a la rupture) Gastroenterol Clin Biol. 1988;12:245–254. [PubMed] [Google Scholar]
- 28.Jacobs S, Chang RWS, Lee B, Al Rawaf A, Pace NC, Salam I. Prediction of outcome in patients with acute variceal haemorrhage. Br J Surg. 1989;76(2):123–126. doi: 10.1002/bjs.1800760206. [DOI] [PubMed] [Google Scholar]
- 29.NIEC (North Italian Endoscopic Club for study and treatment of Esophageal Varices) Prediction of the first variceal hemorrhage in patients with cirrhosis of the liver and esophageal varices. N Engl J Med. 1988;319(15):983–989. doi: 10.1056/NEJM198810133191505. [DOI] [PubMed] [Google Scholar]
- 30.Popescu I. Chirurgia ficatului. 2. București: Ed Universitarã "Carol Davila" ; 2004. pp. 663–742. [Google Scholar]
- 31.Dagradi AE, Mehler R, Tan ATD, Stempien SJ. Sources of upper gastrointestinal bleeding in patients with liver cirrhosis and large esophago-gastric varices. Am J Gastroenterol. 1970;54(5):458–463. [PubMed] [Google Scholar]
- 32.Jensen DM. Endoscopic screening for varices in cirrhosis: findings, implications and outcomes. Gastro-enterology. 2002;122(6):1620–1630. doi: 10.1053/gast.2002.33419. [DOI] [PubMed] [Google Scholar]
- 33.Madhotra R, Mulcahy HE, Willner I, Reuben A. Prediction of esophageal varices in patients with cirrhosis. J Clin Gastroenterol. 2002;34(1):8185–8185. doi: 10.1097/00004836-200201000-00016. [DOI] [PubMed] [Google Scholar]
- 34.Snady H, Feinman L. Prediction of variceal hemorrhage: A prospective study. Am J Gastroenterol. 1988;83(5):519–525. [PubMed] [Google Scholar]
- 35.Polio J, Groszmann RJ. Haemodynamic factors involved in the development and rupture of esophagial varices: a pathophysiologic approach to treatment. Semin Liver Dis. 1986;6:318–331. doi: 10.1055/s-2008-1040614. [DOI] [PubMed] [Google Scholar]
- 36.Ohmoto K, Yamamoto S. Prevention of variceal recurence, bleeding and death in cirrhosis patients with hipersplenism, especially those with severe trombocytopenia. Hepatogastroenterology. 2003;50(54):1760–1769. [PubMed] [Google Scholar]
- 37.D'Amico G, Morabito A, Pagliaro I, Marubini E. Survival and prognostic indicators in compensated and decompensated cirrhosis. Dig Dis Sci. 1986;31(5):468–475. doi: 10.1007/BF01320309. [DOI] [PubMed] [Google Scholar]
- 38.Bosch J, Abraldes JG, Groszmann R. Current management of portal hypertension. J Hepatol. 2003;suppl1:S54–S54. doi: 10.1016/s0168-8278(02)00430-0. [DOI] [PubMed] [Google Scholar]
- 39.D'Amico G, Pagliaro L, Bosch J. Pharmacological treatment of portal hypertension: an evidence-based approach. Semin Liver Dis. 1999;19(4):475–505. doi: 10.1055/s-2007-1007133. [DOI] [PubMed] [Google Scholar]
- 40.Ben-Ari Z, Cardin F, McCormick AP, Wannamethee G, Burroughs AK. A predictive model for failure to control bleeding during acute variceal hemorrhage. J Hepatol. 1999;31:443–450. doi: 10.1016/s0168-8278(99)80035-x. [DOI] [PubMed] [Google Scholar]
- 41.Infante-Rivard C, Esnaola S, Villeneuve JP. Role of endoscopic variceal sclerotherapy in the long term management of variceal bleeding: a metaanalysis. Gastroenterology. 1989;96:1087–1092. doi: 10.1016/0016-5085(89)91627-2. [DOI] [PubMed] [Google Scholar]
- 42.Deschenes M, Villeneuve JR. Risk factors for the development of bacterial infections in hospitalised patient with cirrhosis. Am J Gastroenterol. 1999;94:2193–2197. doi: 10.1111/j.1572-0241.1999.01293.x. [DOI] [PubMed] [Google Scholar]
- 43.Goulis J, Patch D, Burruoughs AK. Bacterial infection in the pathogenesis of variceal bleeding. Lancet. 1999;353(9147):139–142. doi: 10.1016/S0140-6736(98)06020-6. [DOI] [PubMed] [Google Scholar]
- 44.Vilstrup H. Cirrhosis and bacterial infections. Rom J Gastroenterol. 2003;12(4):297–302. [PubMed] [Google Scholar]
- 45.Bernad B, Cadranel JF, Valla D, Escolano S, Jarlier V, Opolon P. Prognostic significance of bacterial infection in bleeding cirrhotic patients: a prospective study. Gastroenterology. 1995;108(6):1828–1834. doi: 10.1016/0016-5085(95)90146-9. [DOI] [PubMed] [Google Scholar]
- 46.Pohl J, Pollmann K, Sauer P, Ring A, Stremmel W, Schlenker T. Antibiotic prophylaxis after variceal hemorrhage reduces incidence of early rebleeding. Hepatogastroenterology. 2004;51(56):541–546. [PubMed] [Google Scholar]
- 47.Jepsen P, Vilstrup H, Moller JK, Sorensen HT. Prognosis of patients with liver cirrhosis and spontaneus bacterial peritonitis. Hepatogastroenterology. 2003;50(54):2133–2136. [PubMed] [Google Scholar]
- 48.Pauwels A, Mostefa-Kara N, Debenes B, Degoutte E, Levy VG. Systemic antibiotic prophylaxis after gastrointestinal hemorrhage in cirrhotic patients with a high risk of infection. Hepatology. 1996;24(4):802–806. doi: 10.1002/hep.510240408. [DOI] [PubMed] [Google Scholar]
- 49.Kollef MH, O'Brien JD, Zuckerman GR, Shannon W. BLEED: a classification to predict outcome in patients with acute upper and lower gastrointestinal hemorrhage. Crit Care Med. 1997;25(7):1125–1132. doi: 10.1097/00003246-199707000-00011. [DOI] [PubMed] [Google Scholar]
- 50.Sutton FM. Upper gastrointestinal bleeding in patients with esophageal varices: what is the most common source? Am J Med. 1987;83(2):273–275. doi: 10.1016/0002-9343(87)90698-x. [DOI] [PubMed] [Google Scholar]
- 51.Sorensen MB, Christiansen LA, Malmstrom J, Bille-Brahe NE. Central hemodynamics in acute gastrointestinal bleeding. Surg Gynecol Obstet. 1977;145(5):685–690. [PubMed] [Google Scholar]
- 52.Kwan V, Norton ID. Endoscopic management of non-variceal upper gastrointestinal haemorrhage. ANZ J Surg. 2007;77(4):222–230. doi: 10.1111/j.1445-2197.2007.04023.x. [DOI] [PubMed] [Google Scholar]
- 53.Garcia-Tsao G, Escorselle A, Zakko M, Patch D, Matloff D. Predicting the presence of significant portal hypertension and varices in compensated cirrhotic patient (abstract) Hepatol. 1997;26:360 A–360 A. [Google Scholar]
- 54.Săftoiu A, Ciurea T. Gastro-enterologie și Hepatologie. București: Ed Medicală ; 2003. Hemoragiile digestive superioare non-variceale ; pp. 645 –673 . [Google Scholar]
- 55.North Italian Endoscopic Club for the study and treatment Esophageal Varices. Prediction of the first variceal hemorrhage in patient with cirrhosis of the liver and esophageal varices. A prospectiv multicentric study. N Engl J Med. 1998;319(15):983–989. doi: 10.1056/NEJM198810133191505. [DOI] [PubMed] [Google Scholar]
- 56.Pagliaro L, D'Amico G, Pasta L, Politi F, Vizzini G, Traina M, Madonia S, Luca A, Guerrera D, Puleo A, D'Antoni A. Portal hypertension. Pathophysiology and Treatment. Blackwell Science Oxford. 1994:72–92. [Google Scholar]
- 57.Sanyal AJ, Purdum PP III, Luketic VA, Shiffman ML. Bleeding gastroesophageal varices. Sem Liver Dis. 1993;13:328–342. doi: 10.1055/s-2007-1007361. [DOI] [PubMed] [Google Scholar]
- 58.Kravetz D, Bosch J, Arderiu M, Pilar Pizcueta M, Rodés J. Hemodynamic effects of blood volume restitution following a hemorrhage in rats with portal hypertension due to cirrhosis of the liver: influence of the extent of portal-systemic shunting. Hepatology. 1989;9(6):808–814. doi: 10.1002/hep.1840090603. [DOI] [PubMed] [Google Scholar]
- 59.Blair SD, Janvrin SB, McCollum CN, Greenhalgh RM. Effect of early blood transfusion on gastrointestinal haemorrhage. Br J Surg. 1986;73(10):783–785. doi: 10.1002/bjs.1800731007. [DOI] [PubMed] [Google Scholar]
- 60.Klein HG, Spahn DR, Carson JL. Red blood cell transfusion in clinical practice. Lancet. 2007;370(9585):415–426. doi: 10.1016/S0140-6736(07)61197-0. [DOI] [PubMed] [Google Scholar]
- 61.Hogue J, Goodnough LT, Monk TG. Preoperative myocardial ischemic episodes are related to hematocrit levels in patients undergoing radical prostatectomy. Transfusion. 1998;38(10):924–931. doi: 10.1046/j.1537-2995.1998.381098440856.x. [DOI] [PubMed] [Google Scholar]
- 62.Feu F, García-Pagán JC, Bosch J, Luca A, Terés J, Escorsell A, Rodés J. Relation between portal pressure response to pharmacotherapy and risk of recurrent variceal haemorrhage in patients with cirrhosis. Lancet. 1995;346(8982):1056–1059. doi: 10.1016/s0140-6736(95)91740-3. [DOI] [PubMed] [Google Scholar]
- 63.Ramond MJ, Valla D, Mosnier JF, Degott C, Bernuau J, Rueff B, Benhamou JP. Successful endoscopic obturation of gastric varices with butyl cyanoacrylate. Hepatology. 1989;10:488–493. doi: 10.1002/hep.1840100415. [DOI] [PubMed] [Google Scholar]
- 64.Hou MC, Lin HC, Kuo BI, Lee FY, Schmidt CM, Lee SD. Clinical implications of the white nipple sign and its role in the diagnosis of esophageal variceal hemorrhage. Am J Gastroenterol. 1996;91:2103–2109. [PubMed] [Google Scholar]
- 65.Yoshida T, Harada T, Shigemitsu T, Takeo Y, Miyazaki S, Okita K. Endoscopic management of gastric varices using a detachable snare and simultaneous endoscopic sclero-therapy and O-ring ligation. J Gastroenterol Hepatol. 1999;14:730–735. doi: 10.1046/j.1440-1746.1999.01941.x. [DOI] [PubMed] [Google Scholar]
- 66.Arakaki Y, Murakami K, Takahashi K, Sato R, Okimoto T, Ishitobi H, Nasu M, Kagawa J, Kodama M, Fujioka T. Clinical evaluation of combined endoscopic variceal ligation and sclerotherapy of gastric varices in liver cirrhosis. Endoscopy. 2003;35(11):940–945. doi: 10.1055/s-2003-43475. [DOI] [PubMed] [Google Scholar]
- 67.Raju GS, Gajula L. Endoclips for GI endoscopy. Gastrointest Endosc. 2004;59(2):267–279. doi: 10.1016/s0016-5107(03)02110-2. [DOI] [PubMed] [Google Scholar]
- 68.Ljubicic N. Endoscopic detachable mini-loop ligation for treatment of gastroduodenal angiodysplasia: case study of 11 patients with long-term follow-up. Gastrointest Endosc. 2004;59(3):420–423. doi: 10.1016/s0016-5107(03)02718-4. [DOI] [PubMed] [Google Scholar]
- 69.Rollhauser C, Fleischer DE. Nonvariceal upper gastrointestinal bleeding. Endoscopy. 2002;34:111–118. doi: 10.1055/s-2002-19853. [DOI] [PubMed] [Google Scholar]
- 70.Lee KJ, Kim HJ, Hahm KB, Cho SW, Park YS. Randomized trial of N-butyl-2-cyanoacrylate compared with hypertonic saline-epinephrine in the endoscopic treatment of bleeding peptic ulcers. Endoscopy. 2000;32(7):505–511. doi: 10.1055/s-2000-3816. [DOI] [PubMed] [Google Scholar]
- 71.Imperiale TF, Birgisson S. Somatostatin or octreotide compared to H2 antagonist and placebo in the management of acute nonvariceal upper gastrointestinal hemorrhage: a meta-analysis. Ann Intern Med. 1997;127(12):1062–1071. doi: 10.7326/0003-4819-127-12-199712150-00002. [DOI] [PubMed] [Google Scholar]
- 72.Thabut D, Bernard-Chabert B. Management of acute bleeding from portal hypertension. Best Pract Res Clin Gastroenterol. 2007;21(1):19–27. doi: 10.1016/j.bpg.2006.07.010. [DOI] [PubMed] [Google Scholar]
- 73.Levacher S, Letoumelin P, Pateron D, Blaise M, Lapandry C, Pourriat JL. Early administration of terlipressin plus glyceryl trinitrate to control active upper gastrointestinal bleeding in cirrhotic patients. Lancet. 1995;346(8979):865–868. doi: 10.1016/s0140-6736(95)92708-5. [DOI] [PubMed] [Google Scholar]
- 74.Reverter E, García-Pagán JC. Management of an acute variceal bleeding episode. Clinical Liver Disease. 2012;1(5):151–154. doi: 10.1002/cld.82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.D'Amico M, Berzigotti A, Garcia-Pagan JC. Refractory acute variceal bleeding: what to do next? Clinics in liver disease. 2010;14(2):297–305. doi: 10.1016/j.cld.2010.03.012. [DOI] [PubMed] [Google Scholar]
- 76.Angelico M, Carli L, Piat C, Gentile S, Rinaldi V, Bologna E, Capocaccia L. Isosorbide-5-mononitrate versus propranolol in the prevention of first bleeding in cirrhosis. Gastroenterology. 1993;104:1460–1465. doi: 10.1016/0016-5085(93)90356-h. [DOI] [PubMed] [Google Scholar]
- 77.Orloff MJ, Orloff MS, Orloff SL, Haynes KS. Treatment of bleeding from portal hypertensive gastropathy by portacaval shunt. Hepatology. 1995;21(4):1011–1017. [PubMed] [Google Scholar]
- 78.Perez-Ayuso RM, Piqué JM, Bosch J, Panés J, González A, Pérez R, Rigau J, Quintero E, Valderrama R, Viver J. Propranolol in prevention of recurrent bleeding from severe portal hypertensive gastropathy in cirrhosis. Lancet. 1991;337(8755):1431–1434. doi: 10.1016/0140-6736(91)93125-s. [DOI] [PubMed] [Google Scholar]
- 79.Cappell MS. A study of the syndrome of simultaneous acute upper gastrointestinal bleeding and myocardial infarction in 36 patients. Am J Gastroenterol. 1995;90(9):1444–1449. [PubMed] [Google Scholar]
- 80.DeWeert TM, Gostout CJ, Wiesner RH. Congestive gastropathy and other upper endoscopic findings in 81 consecutive patients undergoing orthotopic liver transplantation. Am J Gastroenterol. 1990;85(5):573–576. [PubMed] [Google Scholar]
- 81.Branicki FJ, Boey J, Fok PJ, Pritchett CJ, Fan ST, Lai EC, Mok FP, Wong WS, Lam SK, Hui WM. Bleeding duodenal ulcer: a prospective evaluation of risk factors for rebleeding and death. Ann Surg. 1989;211:411–411. doi: 10.1097/00000658-199004000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.de Franchis R. Updating consensus in portal hypertension: report of the Baveno III Consensus Workshop on definitions, methodology and therapeutic strategies in portal hypertension. J Hepatol. 2000;33(5):846–852. doi: 10.1016/s0168-8278(00)80320-7. [DOI] [PubMed] [Google Scholar]
- 83.Zaman A, Hapke R, Flora K, Rosen HR, Benner K. Factors predicting the presence of esophageal or gastric varices in patients with advanced liver disease. Am J Gastroenterol. 1999;94(11):3292–3296. doi: 10.1111/j.1572-0241.1999.01540.x. [DOI] [PubMed] [Google Scholar]
- 84.Chalasani N, Imperiale TF, Ismail A, Sood G, Carey M, Wilcox CM, Madichetty H, Kwo PY, Boyer TD. Predictors of large esophageal varices in patients with cirrhosis. Am J Gastroenterol. 1999;94(11):3285–3291. doi: 10.1111/j.1572-0241.1999.1539_a.x. [DOI] [PubMed] [Google Scholar]
- 85.Madhotra R, Mulcahy HE, Willner I, Reuben A. Prediction of esophageal varices in patients with cirrhosis. J Clin Gastroenterol. 2002;34(1):81–85. doi: 10.1097/00004836-200201000-00016. [DOI] [PubMed] [Google Scholar]
- 86.Giannini E, Botta F, Borro P, Risso D, Romagnoli P, Fasoli A, Mele MR, Testa E, Mansi C, Savarino V, Testa R. Platelet count/spleen diameter ratio: proposal and validation of a non-invasive parameter to predict the presence of oesophageal varices in patients with liver cirrhosis. Gut. 2003;52(8):1200–1205. doi: 10.1136/gut.52.8.1200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Saab S, DeRosa V, Nieto J, Durazo F, Han S, Roth B. Costs and clinical outcomes of primary prophylaxis of variceal bleeding in patients with hepatic cirrhosis: a decision analytic model. Am J Gastroenterol. 2003;98:763–770. doi: 10.1111/j.1572-0241.2003.07392.x. [DOI] [PubMed] [Google Scholar]
- 88.Spiegel BM, Targownik L, Dulai GS, Karsan HA, Gralnek IM. Endoscopic screening for esophageal varices in cirrhosis: Is it ever cost effective? Hepatology. 2003;37(2):366–377. doi: 10.1053/jhep.2003.50050. [DOI] [PubMed] [Google Scholar]
- 89.Arguedas MR, Heudebert GR, Eloubeidi MA, Abrams GA, Fallon MB. Cost-effectiveness of screening, surveillance, and primary prophylaxis strategies for esophageal varices. Am J Gastroenterol. 2002;97:2441–2452. doi: 10.1111/j.1572-0241.2002.06000.x. [DOI] [PubMed] [Google Scholar]
- 90.Merli M, Nicolini G, Angeloni S, Rinaldi V, De Santis A, Merkel C, Riggio O. Incidence and natural history of small esophageal varices in cirrhotic patients. J Hepatol. 2003;38:266–272. doi: 10.1016/s0168-8278(02)00420-8. [DOI] [PubMed] [Google Scholar]
- 91.de Franchis R. Evaluation and follow-up of patients with cirrhosis and oesophageal varices. J Hepatol. 2003;38:361–363. doi: 10.1016/s0168-8278(03)00011-4. [DOI] [PubMed] [Google Scholar]
- 92.Groszmann RJ, Garcia-Tsao G, Makuch RW, Bosch J, Escorsel A, Garcia-Pagan JC, Patch D. Multicenter randomized placebo-controlled trial of non-selective beta-blockers in the prevention of the complications of portal hypertension: final results and identification of a predictive factor. Hepatology. 2003;38:206A–206A. [Google Scholar]
- 93.Poynard T, Calès P, Pasta L, Ideo G, Pascal JP, Pagliaro L, Lebrec D. Beta-adrenergic-antagonist drugs in the prevention of gastrointestinal bleeding in patients with cirrhosis and esophageal varices. An analysis of data and prognostic factors in 589 patients from four randomized clinical trials. Franco-Italian Multi-center Study Group. N Engl J Med. 1991;324(22):1532–1538. doi: 10.1056/NEJM199105303242202. [DOI] [PubMed] [Google Scholar]
- 94.Merkel C, Marin R, Angeli P, Zanella P, Felder M, Bernardinello E, Cavallarin G, Bolognesi M, Donada C, Bellini B, Torboli P, Gatta A, Gruppo Triveneto per l'Ipertensione Portale. A placebo-controlled clinical trial of nadolol in the prophylaxis of growth of small esophageal varices in cirrhosis. Gastroenterology. 2004;127(2):476–484. doi: 10.1053/j.gastro.2004.05.004. [DOI] [PubMed] [Google Scholar]
- 95.Abraldes JG, Tarantino I, Turnes J, Garcia-Pagan JC, Rodés J, Bosch J. Hemodynamic response to pharmacological treatment of portal hypertension and long-term prognosis of cirrhosis. Hepatology. 2003;37(4):902–908. doi: 10.1053/jhep.2003.50133. [DOI] [PubMed] [Google Scholar]
- 96.Abraczinskas DR, Ookubo R, Grace ND, Groszmann RJ, Bosch J, Garcia-Tsao G, Richardson CR, Matloff DS, Rodés J, Conn HO. Propranolol for the prevention of first esophageal variceal hemorrhage: a lifetime commitment? Hepatology. 2001;34(6):1096–1102. doi: 10.1053/jhep.2001.29305. [DOI] [PubMed] [Google Scholar]
- 97.Garcia-Pagán JC, Feu F, Bosch J, Rodés J. Propranolol compared with propranolol plus isosorbide-5-mononitrate for portal hypertension in cirrhosis. Ann Intern Med. 1991;114:869–873. doi: 10.7326/0003-4819-114-10-869. [DOI] [PubMed] [Google Scholar]
- 98.Merkel C, Sacerdoti D, Bolognesi M, Enzo E, Marin R, Bombonato G. Hemodynamic evaluation of the addition of isosorbide-5-mononitrate to nadolol in cirrhotic patients with insufficient response to the beta-blocker alone. Hepatology. 1997;26:34–39. doi: 10.1053/jhep.1997.v26.pm0009214449. [DOI] [PubMed] [Google Scholar]
- 99.Merkel C, Marin R, Enzo E, Donada C, Cavallarin G, Torboli P. Randomised trial of nadolol alone or with isosorbide mononitrate for primary prophylaxis of variceal bleeding in cirrhosis. Gruppo-Triveneto per L'ipertensione portale (GTIP) Lancet. 1996;348:1677–1681. doi: 10.1016/s0140-6736(96)05406-2. [DOI] [PubMed] [Google Scholar]
- 100.García-Pagán JC, Morillas R, Bañares R, Albillos A, Villanueva C, Vila C, Genescà J, Jimenez M, Rodriguez M, Calleja JL. Propranolol plus placebo versus propranolol plus isosorbide-5-mononitrate in the prevention of a first variceal bleed: a double-blind RCT. Hepatology. 2003;37:1260–1266. doi: 10.1053/jhep.2003.50211. [DOI] [PubMed] [Google Scholar]
- 101.Lebrec D, Nouel O, Bernuau J, Bouygues M, Rueff B, Benhamou JP. Propranolol in prevention of recurrent gastrointestinal bleeding in cirrhotic patients. Lancet. 1981;317(8226):920–921. doi: 10.1016/s0140-6736(81)91617-2. [DOI] [PubMed] [Google Scholar]
- 102.Bureau C, Péron JM, Alric L, Morales J, Sanchez J, Barange K, Payen JL, Vinel JP. “A la carte” treatment of portal hypertension: adapting medical therapy to hemodynamic response for the prevention of bleeding. Hepatology. 2002;36(6):1361–1366. doi: 10.1053/jhep.2002.36945. [DOI] [PubMed] [Google Scholar]
- 103.de Franchis R, Primignani M. Endoscopic treatments for portal hypertension. Semin Liver Dis. 1999;19(4):439–455. doi: 10.1055/s-2007-1007131. [DOI] [PubMed] [Google Scholar]
- 104.de la Pena J, Brullet E, Sanchez-Hernández E, Rivero M, Vergara M, Martin-Lorente JL, Garcia Suárez C. Variceal ligation plus nadolol compared with ligation for prophylaxis of variceal rebleeding. Multi-center trial. Hepatology. 2005;41(3):572–578. doi: 10.1002/hep.20584. [DOI] [PubMed] [Google Scholar]


