Abstract
Objectives:
Burn patients have a highly variable length-of-stay (LOS) due to the complexity of the burn injury itself. The LOS for burn patients is estimated as one day per percent total body surface area (TBSA) burn. To focus care expectation and prognosis we aimed to identify key factors that contribute to prolonged LOS.
Methods:
This was a retrospective cohort-study (2006–2016) in an adult burn-centre that included patients with ≥10% TBSA burn. Patients were stratified into expected-LOS (<2days LOS/%TBSA) and longer-than-expected-LOS (>2days LOS/%TBSA). We assessed demographics, comorbidities, and in-hospital complications. Logistic regression and propensity matching was utilized.
Results:
Of the 583 total patients, 477 had an expected-LOS whereas 106 a longer-than-expected-LOS. Non-modifiable factors such as age, 3rd degree TBSA%, inhalation injuries and comorbidities were greater in the exceeded LOS patients. Subsequent matched analysis revealed factors like number of procedures performed, days ventilated and in-hospital complications (bacteremia, pneumonia, sepsis, graft loss, and respiratory failure) were significantly increased in the longer-than-expected-LOS group.
Conclusions:
Progress has been made to update the conventional one day/%TBSA to better aid health care providers in giving appropriate outcomes for patients and their families and to supply intensive care units with valuable data to assess quality of care and to improve patient prognosis.
Keywords: length of stay, burns, comorbidities, in-hospital complications
INTRODUCTION
Burn patients represent one of the most complex patient groups in hospital care: burn trauma itself leads to the loss of irreplaceable skin and hypermetabolism that dramatically increases the likelihood of in-hospital complications such as infection, sepsis, organ failure, and mortality [1–3]. In addition, the majority of the hospitalized burn patients suffer from pre-existing conditions such as diabetes and mental health issues further complicating discharge and recovery [4, 5]. Greater emphases on the assessment of comorbidities, including psychiatric conditions, are needed to understand their influence on the recovery and LOS of burn patients.
The LOS for burn patients is widely estimated as one day per percent total body surface area (TBSA) burn (LOS/%TBSA) and dates back to 1986 [6], but in 2011 Sahin et al. reported that a mean stay of 2 days/TBSA% is a more conservative goal to obtain [7]. The LOS prediction solely based on the TBSA% has been under heavy critique for inaccuracy, and newer prediction models try to take into account the complexity of burn injury by incorporating variables of inhalation injury and age [8]. It has been postulated that a precise LOS prediction needs to include pre-existing medical conditions, demographics, and directly burn-related variables such as %TBSA and inhalation injury, but also complications that develop during hospitalization [8, 9]. However, it is still unclear to what extent medical conditions contribute to an increase in LOS in burn patients. Identifying which modifiable factors cause an increased LOS will enable teams to appropriately target their care, evaluate its quality, identify areas of improvement, and to help calculate the needed medical resources [8, 10]. Additionally, identification of these factors will also aid in counseling patients and their families to anticipate an appropriate LOS.
To address this, we assessed patient data in a single burn centre in a period between January 2006 and December 2016. Patients were stratified in two different groups: patients that had an average LOS based on the common LOS prediction model (expected-stay group; LOS/%TBSA <2days), and patients that exceeded this time (longer-than-expected-LOS group, >2days LOS/%TBSA). The two groups were then compared using demographic factors, pre-existing medical conditions as well as complications that developed during their hospital stay. We preformed logistic regression and propensity matching to further understand the influence of each variable on the LOS. We hypothesized that pre-existing comorbidities, admittance injury severity, and in-hospital complications will all contribute to an increased LOS in severe burn patients.
METHODS
Study population
This retrospective cohort study is based on a data review of all burn survivors with burns over 10% TBSA, treated at the Ross Tilley Burn Centre in Toronto, Canada, between January 2006 to December 2016. A prospective clinical registry of all patients admitted to our burn centre was utilized to identify patients. After excluding futile cases and patients that died during hospitalization, 583 patients were included in this study.
Demographics and outcome measures
Demographics (date of burn injury, date of admission, age, sex, %TBSA, and presence of an inhalation injury), burn etiology (flame, scald, chemical, contact, radiation, and electrical), pre-existing conditions (depression, alcohol abuse/misuse, tobacco use, and substance abuse/misuse), pre-existing metabolic conditions (diabetes, hypertension, and obesity), LOS, in-hospital complications (bacteremia, sepsis, pneumonia, graft loss, renal failure, and respiratory failure), days of ventilation, and operative procedures conducted during their hospital stay were recorded. The burn team, including the attending burn staff and critical care staff, diagnosed in-hospital complications. Prospective documentation of complications followed the guidelines set by the American Burn Association [11]. Patients were grouped based on their hospital LOS/%TBSA in an expected-LOS group defined as a LOS/%TBSA <2, or a longer-than-expected-LOS group with a LOS/%TBSA ≥2.
Statistical analysis
Categorical data were analyzed using the Fisher’s exact test. Normally distributed continuous variables were analyzed using the Student’s t-test and non-normally distributed variables were analyzed using the Mann-Whitney U test. To examine the association between expected-stay and long-stay patients, and each outcome, individual logistic regression models were developed that included patient age, sex, TBSA%, and inhalation injury. Negative binomial linear regression was employed to model the count nature of LOS. A logistic regression analysis was conducted on the dichotomous outcomes of bacteremia, sepsis, cellulitis, ARDS, and pneumonia. Model calibration was assessed using the Hosmer and Lemeshow test. Propensity scoring was used to match patients based on age, sex, % TBSA burn, % 3rd degree TBSA burn, and inhalation injury. All tests were 2-tailed, with a P value of < 0.05 considered statistically significant. Analyses were performed using SPSS Statistics version 20.0 (IBM Corp., Armonk, NY).
Guidelines and Patient Involvement
The data are reported in accordance with the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement [12]. The study protocol was approved by the research ethics board at our institution (REB# 307–2015). Patients were not directly involved in designing or conducting this research.
RESULTS
Demographics
Of all surviving burn patients with ≥10% TBSA, admitted to the Ross Tilley Burn Centre between January 2006 and December 2016 (n=583), 18% (n=106) exceeded the expected LOS/%TBSA of ≤ 2 days (p<0.0001; Table 1). The longer-than-expected-LOS subset had a significantly higher amount of elderly patients ≥ 65 years (28% vs. 15%, p=0.002), more 3rd degree burns (14±14% vs. 8±13%, p<0.001), and a higher number of patients with inhalation injury (33% vs. 21%, p=0.007). Interestingly, burn injury caused by scalding was significantly less prevalent in the patient group that exceeded the normal LOS (13% vs. 23%, p=0.034). No difference between the two groups could be found regarding gender and total amount of TBSA (p>0.05).
Table 1.
Demographics and outcomes of all patients based on LOS/%TBSA.
| All | LOS/%TBSA < 2.0 (expected-stay) | LOS/%TBSA ≥ 2.0 (long-stay) | p | |
|---|---|---|---|---|
| No. of patients | 583 | 477 | 106 | |
| Age, years, mean ± SD | 47 ± 18 | 45 ± 17 | 56 ± 18 | <0.0001 |
| Age ≥ 65, no. (%) | 100 (17%) | 70 (15%) | 30 (28%) | 0.002 |
| Male, no. (%) | 431 (74%) | 360 (76%) | 71 (67%) | 0.086 |
| TBSA, %, mean ± SD | 21 ± 13 | 21 ± 12 | 21 ± 14 | 0.923 |
| 3rd degree TBSA, %, mean ± SD | 9 ± 13 | 8 ± 13 | 14 ± 14 | <0.001 |
| Inhalation injury, no. (%) | 133 (23%) | 98 (21%) | 35 (33%) | 0.007 |
| Days to admit, mean ± SD | 1 ± 2 | 1 ± 2 | 1 ± 2 | 0.784 |
| Etiology, no. (%) | ||||
| Flame | 421 (72%) | 337 (71%) | 84 (79%) | 0.093 |
| Scald | 123 (21%) | 109 (23%) | 14 (13%) | 0.034 |
| Chemical | 10 (2%) | 9 (2%) | 1 (1%) | 0.699 |
| Radiation | 1 (0.2%) | 1 (0.2%) | 0 | 1.000 |
| Electrical | 26 (5%) | 19 (4%) | 7 (7%) | 0.294 |
| Contact | 2 (0.3%) | 2 (0.4%) | 0 | 1.000 |
| LOS, days, median (IQR) | 20 (15–33) | 18 (13–26) | 45 (31–70) | <0.0001 |
| LOS, days/TBSA, %, median (IQR) | 1.2 (0.9-1.7) | 1.1 (0.8–1.4) | 2.5 (2.2–3.4) | <0.0001 |
| Number of procedures, mean ± SD | 7 ± 8 | 6 ± 6 | 12 ± 11 | <0.0001 |
| Ventilated, no. (%) | 294 (50%) | 217 (46%) | 77 (73%) | <0.0001 |
| Ventilated daysa, mean ± SD | 17 ± 18 | 13 ± 13 | 29 ± 24 | <0.0001 |
Numbers may not add to 100 due to rounding.
LOS, length of stay; TBSA, total body surface area.
Analysis restricted to patients that were on a mechanical ventilator.
Pre-existing medical conditions
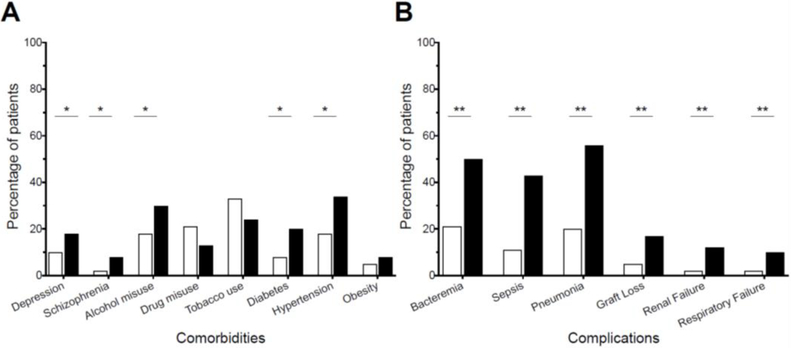
Without adjusting for demographic factors, patients in the longer-than-expected-LOS group showed a significantly higher occurrence in almost all assessed pre-existing medical conditions (Figure 1A): depression (18% vs. 10%, p=0.043), schizophrenia (8% vs. 2%, p=0.008), alcohol misuse (30% vs. 18%, p=0.011), diabetes (20% vs. 8%, p=0.001), and hypertension (34% vs. 18%, p<0.001).
Figure 1.
Proportion of comorbidities (A) and complications (B) present in all patients by length of stay group. *p < 0.05; **p < 0.0001. LOS, length of stay; TBSA, total body surface area.
When adjusted to age, inhalation injury, sex, and %TBSA burn, all comorbid conditions - apart from tobacco use and drug misuse - increased the odds ratio of the burn patient to exceed the average LOS: Depression (OR 1.86, 95%CI 1.01–3.43), schizophrenia (OR 2.93, 95%CI 1.06–8.08), and alcohol misuse (OR 1.82, 95%CI 1.1–3.01). Interestingly, obesity, hypertension, and diabetes, known to affect the LOS in surgical patients, did not increase the odds ratio of burn patients to exceed the LOS.
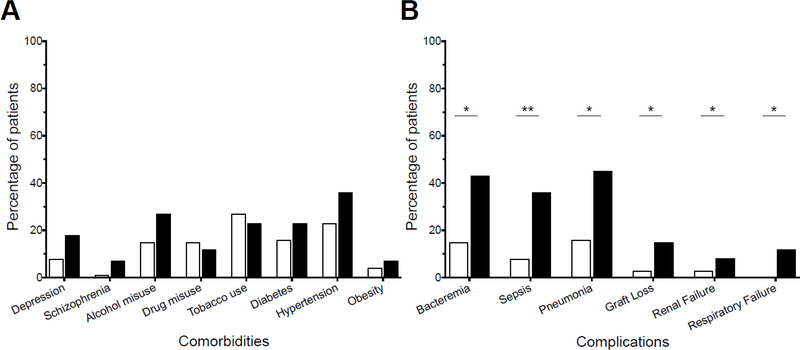
To eliminate the linearity assumption of the logistic regression, we matched patients of the longer-than-expected-LOS and the expected-LOS group based on age, sex, %TBSA 3rd degree burn, and inhalation injury. After matching, comorbidities such as depression (p=0.138), schizophrenia (p=0.209), and alcohol misuse (p=0.105) had a trend of higher prevalence in patients that exceeded the average LOS. Tobacco use (p=0.704) and drug misuse (p=0.810) had did not affect LOS in our patient population. Metabolic conditions like diabetes (p=0.407), hypertension (p=0.146), and obesity (p=0.719) were also more prevalent in the longer-than-expected-LOS group, but without reaching statistical significance (Figure 2A).
Figure 2.
Proportion of comorbidities (A) and complications (B) present in matched patients by length of stay group. *p < 0.05; **p < 0.0001. LOS, length of stay; TBSA, total body surface area.
In-hospital complications
Without adjusting for demographic factors, all in-hospital complications were higher in the longer-than-expected-LOS group (Figure 1B): bacteremia (50% vs. 21%, p<0.0001), sepsis (43% vs. 11%, p<0.0001), pneumonia (56% vs. 20%, p<0.0001), graft loss (17% vs. 5%, p<0.0001), renal failure (12% vs. 2%, p<0.0001), and respiratory failure (10% vs. 2%, p<0.0001). The overall low number of cardiac failures in both groups (1 vs. 2) did not provided enough statistical power for us to draw conclusions. Patients that exceeded the expected LOS also had significantly higher indirect parameters for severe complications such as need for mechanical ventilation (73% vs. 46%, p<0.0001), average days of ventilation (29 vs. 13, p<0.001) and number of surgical procedures (12 vs. 6, p<0.0001).
After adjusting for age, inhalation injury, sex, and %TBSA burn, all assessed complications - apart from cardiac failure - increased the odds of a burn patient to exceed the average LOS (Table 2): bacteremia (OR 7.54, 95%CI 4.03–14.11), pneumonia (OR 6.89, 95%CI 6.24–24.91), graft loss (OR 4.56, 95%CI 2.24–9.3), renal failure (OR 7.7, 95%CI 2.75–21.55), and respiratory failure (OR 7.35, 95%CI 2.63–20.54). Especially sepsis had high odds to prolong the duration of hospitalization: OR 12.47 (6.24–24.91).
Table 2.
Associations between conditions and long-stay in-hospital.
| * Adjusted odds ratio (95% CI) | |
|---|---|
| Pre-existing medical conditions | |
| Depression | 1.86 (1.01, 3.43) |
| Schizophrenia | 2.93 (1.06, 8.08) |
| Alcohol misuse | 1.82 (1.1, 3.01) |
| Drug misuse | 0.72 (0.37, 1.38) |
| Tobacco use | 0.66 (0.4, 1.11) |
| Diabetes | 1.68 (0.91, 3.11) |
| Hypertension | 1.3 (0.74, 2.29) |
| Obesity | 1.55 (0.65, 3.7) |
| In-hospital complications | |
| Bacteremia | 7.54 (4.03, 14.11) |
| Sepsis | 12.47 (6.24, 24.91) |
| Pneumonia | 6.89 (3.93, 12.1) |
| Graft loss | 4.56 (2.24, 9.3) |
| Renal failure | 7.7 (2.75, 21.55) |
| Respiratory failure | 7.35 (2.63, 20.54) |
Adjusted for age, inhalation injury, sex, % TBSA burn, and long-stay. CI, confidence interval; TBSA, total body surface area.
In a matched 1:1 analysis based on patient demographics and injury severity, 73 patients in each group were assessed (Table 3). In-hospital complications were significantly higher in the longer-than-expected-LOS group (Figure 2B): bacteremia (43% vs. 15%, p<0.001), sepsis (36% vs. 8%, p<0.0001), pneumonia (45% vs. 16%, p<0.001), graft loss (15% vs. 3%, p=0.017), and respiratory failure (12% vs. 0%, p=0.003). The number of patients developing renal failure was higher in the longer-than-expected-LOS group, but did not reach statistical significance (8% vs. 3%, p=0.275).
Table 3.
Demographics and outcomes of matched patients based on LOS/%TBSA.
| All | LOS/%TBSA < 2.0 (expected-stay) | LOS/%TBSA ≥ 2.0 (long-stay) | p | |
|---|---|---|---|---|
| No. of patients | 146 | 73 | 73 | |
| Demographics | ||||
| Age, years, mean ± SD | 56 ± 17 | 56 ± 18 | 56 ± 17 | 0.962 |
| Age ≥ 65, no. (%) | 43 (30%) | 23 (32%) | 20 (27%) | 0.717 |
| Male, no. (%) | 104 (71%) | 52 (71%) | 52 (71%) | 1.000 |
| TBSA, %, mean ± SD | 20 ± 12 | 21 ± 11 | 19 ± 12 | 0.545 |
| 3rd degree TBSA, %, mean ± SD | 12 ± 13 | 11 ± 13 | 12 ± 13 | 0.744 |
| Inhalation injury, no. (%) | 30 (21%) | 15 (21%) | 15 (21%) | 1.000 |
| Days to admit, mean ± SD | 1 ± 2 | 1 ± 3 | 1 ± 1 | 0.184 |
| Etiology, no. (%) | ||||
| Flame | 107 (73%) | 51 (70%) | 56 (77%) | 0.455 |
| Scald | 30 (21%) | 20 (27%) | 10 (14%) | 0.064 |
| Chemical | 3 (2%) | 2 (3%) | 1 (1%) | 1.000 |
| Electrical | 6 (4%) | 0 (0%) | 6 (8%) | 0.028 |
| Outcomes | ||||
| LOS, days, median (IQR) | 27 (17–47) | 17 (11–21) | 43 (30–64) | <0.0001 |
| LOS, days/TBSA, %, median (IQR) | 1.9 (0.9-2.5) | 0.9 (0.7–1.2) | 2.5 (2.2–3.2) | <0.0001 |
| Number of procedures, mean ± SD | 8 ± 8 | 5 ± 6 | 11 ± 9 | <0.0001 |
| Ventilated, no. (%) | 77 (53%) | 29 (40%) | 48 (66%) | 0.003 |
| Ventilated daysa, mean ± SD | 14 (4–26) | 8 (2–14) | 17 (11–35) | <0.001 |
Numbers may not add to 100 due to rounding.
LOS, length of stay; TBSA, total body surface area; ns, non-significant
Analysis restricted to patients that were on a mechanical ventilator.
DISCUSSION
Increased LOS in burn patients has poor prognostic factor for patient well-being and overall outcomes. In order to better understand what non-modifiable and modifiable factors could affect LOS, we conducted a retrospective cohort-study in an adult burn center. In this study we used a more conservative threshold [7] of 2 days per percent TBSA to determine LOS, and despite this more generous estimate, we had 18% of patients exceeding the recommendations. We identified admission demographics of age (≥65 years old), 3rd degree burns, and inhalation injury as factors that increased LOS while scald injuries were underrepresented in the exceeding-LOS group. There was no effect of gender or amount of TBSA on LOS in our study. Importantly, complications acquired in-hospital had significant effects on LOS, with sepsis, bacteremia, pneumonia, graft loss, renal failure, and respiratory failure increasing the odds of the patient exceeding the conservative 2day/%TBSA estimates.
We aimed to determine if non-modifiable factors that are beyond critical care management practices had an impact on LOS. In our non-matched analysis, we identified age, 3rd degree TBSA, inhalation injury, scald injury, and pre-existing conditions (depression, schizophrenia, alcohol abuse, diabetes and hypertension) increased LOS. However, when we performed matched analysis based on characteristics such as age, gender, and burn severity, there was a large reduction in these non-modifiable factors’ ability increase in LOS. Electrical burns had a significant increase in LOS and scald injuries approached significance. After matched analysis, it became evident that the majority of factors that increased LOS were a result of care management after the patient was received at the ICU. The number of procedures, percent of patients being ventilated, and mean ventilation days increased LOS, as did in-hospital complications of bacteremia, pneumonia, graft loss, respiratory failure, and sepsis. Only renal failure had no significant increase in LOS. This indicates that proper case management can have consequential effects on patients LOS and overall prognosis.
Burn patients can present with a unique and complex set of pre-existing conditions such as mental health issues that further complicates their treatment and inhibits early recovery and discharge [13, 14]. Our study confirms the data obtained in previous literature associating mental illness and substance misuse with a longer hospital stay and/or prolonged recovery [15–17]. In our matched analysis, patients with pre-existing conditions were not statistically different between expected and exceeding LOS groups. Yet, mental health conditions also occur after burn injury, as those without mental illness pre-injury had three times the number of mental health visits post-injury and a two-fold increase in self-harm injuries [18]. Precautions and monitoring of burn patients after discharge is vital for provide optimal for continued care.
In regard to non-modifiable factors, it is perhaps unsurprising those patients with higher in-hospital complications such as infection (bacteremia, pneumonia, sepsis) and/or renal and respiratory failure had longer than expected LOS. However, it should be noted that when we adjusted to age, inhalation, sex and %TBSA the odds ratio ranged from 4.56 in graft failure to 12.47 in sepsis. Sepsis is particularly troubling because infections are the most common complication in burn patients, and causes high rates of morbidity and mortality [19, 20]. In patients with >40%TBSA, approximately 75% of all deaths are known to be related to sepsis [21], and often is followed by multiple organ dysfunction [22]. Further complicating matters is the fact that antibiotic resistance is directly proportional to LOS [23], with the gram-negative Pseudomonas aeruginosa being the predominant pathogen in increased LOS [23, 24]. Multidrug resistant bacteria are now the leading cause of deaths due to sepsis [25]. Systemic and peri-operative prophylaxis were able to reduce pneumonia and wound infections, respectively [26]. However, until more clinical trials can be conducted, it was recommend that prophylactic treatment with antibiotics should be limited to perioperative severe burn patients alone. Proper wound care and excision performed shortly after injury can contribute to limiting sepsis. Patients who received burn excision within 24 hours after injury has decreased wound colonization and sepsis compared to the conservative treatment of silver sulfadiazine for 5 days prior to excision [27, 28]. Prevention of sepsis should be a major concern in the attempt to decrease LOS in burns patients and improve overall patient outcomes.
Acute respiratory distress syndrome (ARDS) is also common in severe burns patients and leads to increased mortality [29, 30]. ARDS can arise from two mechanisms in a burn patient, either directly through inhalation injury or indirectly through infection and sepsis in these immunocompromised individuals. It has been shown that ARDS only effected LOS in the ICU and not inpatient units [30]. In our initial non-matched analysis, inhalation injury was an associated factor with increased LOS, a finding that parallels the recent large-scale record review of the American Burn Association (ABA) National Burn Repository [8]. However, in our matched analysis that association was lost as the presence of inhalation injury resulted in equal number of patients having expected-LOS and exceeding-LOS. In the ABA study, it was stated that the effect of LOS in record review was “crude” due to the lack of information regarding inhalation injury severity. Our study also lacks the degree of inhalation severity, and therefore we cannot conclude its influence on LOS. Regardless of the cause of ARDS, respiratory distress is exacerbated via ventilator-associated lung damage while under critical care [31]. Respiratory failure was significantly higher in our longer-than-expect LOS groups regardless of matched or non-matching. Of note, in our matched analysis all patients with respiratory failure had a longer-than-expected LOS. In both non-matched and matched analysis, patients that exceeded-LOS where significantly more likely to need mechanical ventilation and had a longer number of days on ventilation. Proper, well organized, and protocol driven respiratory care is critical and is just as important as other components of burn care at decreasing LOS and overall mortality [32, 33].
While this study did encompass a 10-year-period with 583 patients, a limitation is that this was a single-centre study, that could impact its generalizability to other intensive care burn centres and to non-specialized tertiary care hospitals. Additional this was a retrospective cohort-study in has limited causative conclusions and future clinical trials should incorporate LOS into their outcome measurements to properly assess this vital metric of patient prognosis.
In conclusion, our study shows that ICU patient management has a great influence on the LOS of burn patients. We confirm that procedures untaken and in-hospital complications are not only significantly more prevalent in the longer-than-expected-LOS group, but that they also increase the odds for exceeding the average stay of <2 days per TBSA%. Especially sepsis seems to drastically increase the odds ratio of exceeding that timeframe. Despite multiple medical improvements in terms of diagnosing and treating infections and sepsis, they remain one of the biggest issues in burn patient care. Specifically, more attention needs to be paid in early diagnosing and treating infections in burn patients to reduce LOS and ultimately mortality and morbidity.
HIGHLIGHTS.
Critical care patients can have a complex medical history that might interfere with early recovery and discharge.
Events in-hospital had a high influence on longer-than-expected-length of stay per percent burn.
The conventional one day per percent burn should be updated to better evaluate metrics for quality indicators.
ACKNOWLEDGMENTS:
The authors would like to thank the Ross Tilley Burn Centre staff for their support.
Funding/Support: Canadian Institutes of Health Research # 123336, Canada Foundation for Innovation Leader’s Opportunity Fund: Project # 25407, National Institutes of Health 2R01GM087285–05A1.
Abbreviations:
- ABA
American Burn Association
- ARDS
acute respiratory distress syndrome
- ICU
intensive care unit
- LOS
length of stay
- OR
odds ratio
- TBSA
total burn surface area
Footnotes
Competing interests: All authors have completed the ICMJE uniform disclosure and declare: no support from any organisation for the submitted work; no financial relationships with any organisations that might have an interest in the submitted work in the previous three years; no other relationships or activities that could appear to have influenced the submitted work.
Disclosure summary: The authors have no disclosures to report.
This abstract was presented in part at the American Burn Association 50th Annual Meeting and the Shock Society 40th Annual Meeting.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- [1].Tredget EE, Yu YM. The metabolic effects of thermal injury. World J.Surg 1992;1:68–79. [DOI] [PubMed] [Google Scholar]
- [2].Jeschke MG, Klein D, Herndon DN. Insulin treatment improves the systemic inflammatory reaction to severe trauma. Ann.Surg 2004;4:553–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Rowan MP, Cancio LC, Elster EA, Burmeister DM, Rose LF, Natesan S, et al. Burn wound healing and treatment: review and advancements. Crit.Care 2015:243,015–0961-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].McKibben JB, Ekselius L, Girasek DC, Gould NF, Holzer C III, Rosenberg M, et al. Epidemiology of burn injuries II: psychiatric and behavioural perspectives. International Review of Psychiatry 2009;6:512–21. [DOI] [PubMed] [Google Scholar]
- [5].Brusselaers N, Monstrey S, Vogelaers D, Hoste E, Blot S. Severe burn injury in Europe: a systematic review of the incidence, etiology, morbidity, and mortality. Critical care 2010;5:R188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Gillespie R, Carroll W, Dimick AR, Haith L, Heimbach D, Kibbee E, et al. Diagnosis-related groupings (DRGs) and wound closure: roundtable discussion. J.Burn Care Rehabil 1987;3:199–205. [DOI] [PubMed] [Google Scholar]
- [7].Sahin I, Ozturk S, Alhan D, Acikel C, Isik S. Cost analysis of acute burn patients treated in a burn centre: the Gulhane experience. Ann.Burns Fire Disasters 2011;1:9–13. [PMC free article] [PubMed] [Google Scholar]
- [8].Taylor SL, Sen S, Greenhalgh DG, Lawless M, Curri T, Palmieri TL. Not all patients meet the 1day per percent burn rule: A simple method for predicting hospital length of stay in patients with burn. Burns 2017;2:282–9. [DOI] [PubMed] [Google Scholar]
- [9].Taylor SL, Sen S, Greenhalgh DG, Lawless M, Curri T, Palmieri TL. Real-time prediction for burn length of stay via median residual hospital length of stay methodology. Journal of Burn Care & Research 2016;5:e476–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Taylor SL, Sen S, Greenhalgh DG, Lawless M, Curri T, Palmieri TL. A competing risk analysis for hospital length of stay in patients with burns. JAMA surgery 2015;5:450–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Greenhalgh DG, Saffle JR, Holmes JH 4th, Gamelli RL, Palmieri TL, Horton JW, et al. American Burn Association consensus conference to define sepsis and infection in burns. J.Burn Care.Res 2007;6:776–90. [DOI] [PubMed] [Google Scholar]
- [12].von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet 2007;9596:1453–7. [DOI] [PubMed] [Google Scholar]
- [13].MacArthur JD, Moore FD. Epidemiology of burns. The burn-prone patient. JAMA 1975;3:259–63. [PubMed] [Google Scholar]
- [14].Patterson DR, Finch CP, Wiechman SA, Bonsack R, Gibran N, Heimbach D. Premorbid mental health status of adult burn patients: comparison with a normative sample. J.Burn Care Rehabil 2003;5:347–50. [DOI] [PubMed] [Google Scholar]
- [15].Tarrier N, Gregg L, Edwards J, Dunn K. The influence of pre-existing psychiatric illness on recovery in burn injury patients: the impact of psychosis and depression. Burns 2005;1:45–9. [DOI] [PubMed] [Google Scholar]
- [16].Kramer CB, Gibran NS, Heimbach DM, Rivara FP, Klein MB. Assault and substance abuse characterize burn injuries in homeless patients. Journal of Burn care & research 2008;3:461–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Rehou S, Mason S, MacDonald J, Pinto R, Jeschke MG. The influence of substance misuse on clinical outcomes following burn. Burns 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Mason SA, Nathens AB, Byrne JP, Ellis J, Fowler RA, Gonzalez A, et al. Association between burn injury and mental illness among burn survivors: a population-based, self-matched, longitudinal cohort study. J.Am.Coll.Surg 2017;4:516–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Appelgren P, Björnhagen V, Bragderyd K, Jonsson CE, Ransjö U. A prospective study of infections in burn patients. Burns 2002;1:39–46. [DOI] [PubMed] [Google Scholar]
- [20].Coban YK. Infection control in severely burned patients. World J.Crit.Care.Med 2012;4:94–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Church D, Elsayed S, Reid O, Winston B, Lindsay R. Burn wound infections. Clin.Microbiol.Rev 2006;2:403–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Fitzwater J, Purdue GF, Hunt JL, O’Keefe GE. The risk factors and time course of sepsis and organ dysfunction after burn trauma. J.Trauma 2003;5:959–66. [DOI] [PubMed] [Google Scholar]
- [23].Wanis M, Walker SA, Daneman N, Elligsen M, Palmay L, Simor A, et al. Impact of hospital length of stay on the distribution of Gram negative bacteria and likelihood of isolating a resistant organism in a Canadian burn center. Burns 2016;1:104–11. [DOI] [PubMed] [Google Scholar]
- [24].Daneman N, Elligsen M, Walker SA, Simor A. Duration of hospital admission and the need for empirical antipseudomonal therapy. J.Clin.Microbiol 2012;8:2695–701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Williams FN, Herndon DN, Hawkins HK, Lee JO, Cox RA, Kulp GA, et al. The leading causes of death after burn injury in a single pediatric burn center. Critical care 2009;6:R183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Avni T, Levcovich A, Ad-El DD, Leibovici L, Paul M. Prophylactic antibiotics for burns patients: systematic review and meta-analysis. BMJ 2010:c241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Barret JP, Herndon DN. Modulation of inflammatory and catabolic responses in severely burned children by early burn wound excision in the first 24 hours. Archives of surgery 2003;2:127–32. [DOI] [PubMed] [Google Scholar]
- [28].Hart DW, Wolf SE, Chinkes DL, Beauford RB, Mlcak RP, Heggers JP, et al. Effects of early excision and aggressive enteral feeding on hypermetabolism, catabolism, and sepsis after severe burn. Journal of Trauma and Acute Care Surgery 2003;4:755–64. [DOI] [PubMed] [Google Scholar]
- [29].Liffner G, Bak Z, Reske A, Sjöberg F. Inhalation injury assessed by score does not contribute to the development of acute respiratory distress syndrome in burn victims. Burns 2005;3:263–8. [DOI] [PubMed] [Google Scholar]
- [30].Silva L, Garcia L, Oliveira B, Tanita M, Festti J, Cardoso L, et al. Acute respiratory distress syndrome in burn patients: incidence and risk factor analysis. Ann.Burns Fire Disasters 2016;3:178–82. [PMC free article] [PubMed] [Google Scholar]
- [31].Ragaller M, Richter T. Acute lung injury and acute respiratory distress syndrome. J.Emerg.Trauma.Shock 2010;1:43–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Mlcak RP, Suman OE, Herndon DN. Respiratory management of inhalation injury. Burns 2007;1:2–13. [DOI] [PubMed] [Google Scholar]
- [33].McCall JE, Cahill TJ. Respiratory care of the burn patient. J.Burn Care Rehabil 2005;3:200–6. [PubMed] [Google Scholar]