Abstract
Objectives:
Antiretroviral therapy is affording longer lifespans for people living with HIV (PLWH), yet factors such as substance use play an increasing role in morbidity and mortality in this population. Though previous studies have examined substance use differences between age cohorts of PLWH, no study has examined the influence of birth cohort on current substance use patterns. Thus, this study investigated the prevalence of past 12-month self-reported substance use between four birth cohorts, <1970 (M age= 54.1), 1970’s (M age= 41.5), 1980’s (M age= 31.3 years old), & 1990’s (M age=23.2 years old) of PLWH in Florida.
Methods:
PLWH (N = 934) recruited from community health clinics in Florida completed a questionnaire assessing sociodemographics, health status, and substance use. Multivariate logistic regressions utilizing the <1970 cohort as the referent group examined the relationship between birth cohort and substance use.
Results:
The 1980’s cohort had significantly greater odds of marijuana use compared to the oldest cohort (<1970’s), while the three younger cohorts (1970’s, 1980’s, & 1990’s) evidenced a significantly greater odds of ecstasy use compared to the oldest group. Contrastingly, the three younger birth cohorts reported significantly less crack use than the oldest cohort, while the youngest group (1990’s) also demonstrated an 80% reduction in injection drug use compared to the oldest group.
Conclusion:
The older cohort evidenced significantly greater crack and injection drug use, while the younger cohorts evidenced greater marijuana and ecstasy use. Therefore, it is important to develop age-specific substance use interventions among PLWH.
Keywords: HIV, substance use, aging, interventions, health policy
INTRODUCTION
An estimated 1.2 million adolescents and adults are living with HIV in the United States, and 37,600 new cases of HIV are diagnosed per year (Centers for Disease Control and Prevention, 2016). Though the incidence of HIV has remained relatively steady and has evidenced decline in several locales, previous work has elucidated the disproportionate rates of HIV incidence in the southern United States, such that 49–52% of all new HIV diagnoses occur in this region (Reif et al., 2014; Swan & Evans, 2017). The HIV burden is particularly relevant within the state of Florida, which has shown a steady increase in HIV incidence since 2013 (CDC, 2016; Florida Department of Health, 2017). Persons aged 50 and older evidence an increased susceptibility to HIV infection, accounting for 17% of new cases nationally, and 21% of all new HIV infections within Florida (CDC, 2016; Florida Department of Health, 2017). Further, the population of people living with HIV (PLWH) is aging. Older PLWH report lower ratings of psychosocial functioning and physical health and may be particularly susceptible to the harmful effects of substance use (Group, 2003; Piette, Wachtel, Mor, & Mayer, 1995; Rueda, Law, & Rourke, 2014; Vance, 2010).
Comorbidities such as substance use disorders are becoming increasingly relevant to morbidity and mortality in this population. In a seven site study examining alcohol consumption within the past year among 8,567 PLWH, 68% reported any alcohol use, 34% reported binge drinking and 27% reported current hazardous alcohol use (Crane et al., 2017). Furthermore, a meta-analysis found that 34% of PLWH use illicit substances (Nduka, Uthman, Kimani, & Stranges, 2015). Specifically, injection drug use is a particular concern, as it is a direct vector for HIV transmission (Mathers et al., 2008; Nduka et al., 2015). Additionally, non-injection drug use is a documented indirect vector of HIV transmission, due to the association of non-injection drug use with high risk sexual behavior (Baum et al., 2009; Brewer, Zhao, Metsch, Coltes, & Zenilman, 2007; Carey et al., 2009). Specifically, crack use is associated with a greater likelihood of engaging in unprotected sex and having a greater number of sexual partners and thus, may increase the risk of HIV transmission to uninfected adults (Azevedo, Botega, & Guimarães, 2007; Harzke, Williams, & Bowen, 2009). Illicit drug use is also associated with non-adherence to antiretroviral (ART) treatment, which results in increased levels of HIV viral load and transmissibility, as well as disease progression (Arnsten et al., 2002; Baum et al., 2009; Friedland & Vlahov, 2011; Lucas et al., 2006; Wood et al., 2004). Previous research has also indicated that both occasional and daily marijuana use may not be associated with suboptimal antiretroviral adherence or poor HIV-related health outcomes such as detectable viral load, though further study is needed to investigate these relationships (Bonn-Miller, Oser, Bucossi, & Trafton, 2014; Chander, 2010; Okafor et al., 2017; Slawson et al., 2015).
Substance use typically begins in early adolescence and may attenuate with age (Substance Abuse and Mental Health Service Administration, 2011; Trenz et al., 2012). However, findings from The Veterans Aging Cohort Study (VACS) virtual cohort, which examined 33,420 HIV-infected veterans, suggested that the 40–49 year old cohort had the highest rate of any substance use disorder relative to any of the other age groups (Goulet et al., 2007). Additionally, Vance and colleagues (2011) noted that a cohort of 50–59 year-olds had the highest prevalence of alcohol abuse, while 40–49 year olds evidenced higher rates of illicit drug abuse compared to other cohorts among 1,478 adults living with HIV grouped across decades of life (i.e., 18–29, 30–39, 40–49, 50–59, 60+). With ART medications mitigating disparities in life expectancies for PLWH, continued examination of health behaviors, such as substance use, is required to promote optimal health outcomes among PLWH (Mahy, Autenrieth, Stanecki, & Wynd, 2014)
Differences in substance use prevalence among age cohorts of PLWH may be partly explained by the historical factors which shaped these behaviors, as different birth cohorts were exposed to unique sociopolitical environments surrounding the HIV epidemic (i.e., 1981–1996). For example, people born before 1970 experienced the sexual revolution and gay rights movement, during which time period there was also a significant increase in the number of young people experimenting with marijuana, psychedelics, and other illicit substances (Allyn, 2001; Poindexter, 1997). Individuals born prior to 1970 may have also been exposed to the “crack epidemic” of the 1980’s during their formative years. Additionally, people born in the 1970’s and 1980’s experienced the brunt of the HIV epidemic during their early teens and 20’s, an age when substance use onset most commonly occurs, and during a period in history when use of crack/cocaine and injection drugs was more prevalent (Cohler, 2007). This period resulted in an increase in AIDS-related deaths, along with heightened distress, fear, and worry associated with gay related stigma, risk factors for engaging in substance use (Rosenfeld, Bartlam, & Smith, 2012). Individuals born after 1990 developed during a period where HIV became a more manageable chronic illness, marked by decreased AIDS-related deaths along with substantial social changes such as the legalization of gay marriage, which has been shown to have a positive impact on psychological functioning among PLWH (Hatzenbuehler et al., 2012; McDonald et al., 2016). However, there is growing concern that individuals who matured during this period may now be engaging in riskier behavior due to optimism associated with advancements in medical treatment related to HIV-health (Callander & Senn, 2013; Mackellar et al., 2011). Additionally, younger HIV+ adults are growing up in a time when there has been a legislative shift more in favor of marijuana use for both medicinal and recreational purposes (Berg et al., 2015). More recent studies have demonstrated the phenomena of birth cohort effects, as Whitehead and colleagues (2014), found that HIV+ adults 45 and older, who were born before 1970, had significantly higher odds of recent crack use compared to younger HIV+ adults, while the younger group evidenced a greater likelihood of recent marijuana use.
Though birth cohort differences can be influential in explaining current substance use patterns among PLWH, no studies to date have examined current substance use differences by birth cohort among PLWH. Given the implications related to the effects of substance use on HIV transmission and hastened disease progression, along with lower quality of life, the current study sought to assess the prevalence and trends of past 12-month self-reported substance use and misuse among four different birth cohorts based on time of birth relative to the HIV epidemic. These birth cohorts included adults born before 1970, in the 1970’s, 1980’s, and 1990’s of a demographically heterogeneous sample of HIV-positive adults living in Florida. We hypothesized that there would be no significant differences in the prevalence of cigarette smoking and binge alcohol consumption, as there are generally no observed age differences in the prevalence of use (Substance Abuse and Mental Health Service Administration, 2011; Rahmanian et al., 2011). We further hypothesized that the two oldest cohorts (i.e. <1970 and 1970’s) would report significantly greater use of illicit substances other than marijuana compared to youngest cohort (1990’s), while the two older groups would report significantly less marijuana use compared to the two most recent birth cohorts (1980’s and 1990’s) based on previous findings (Whitehead et al., 2014).
METHODS
Participants and Procedures
The sample (N = 934) consisted of participants from the Florida Cohort, an ongoing National Institute on Alcohol Abuse and Alcoholism (NIAAA) funded study examining the determinants of health outcomes among PLWH receiving care within the state of Florida. Participants were recruited through county health departments and community clinics throughout Florida (i.e., Gainesville, Ft. Lauderdale, Lake City, Miami, Orlando, Sanford, & Tampa Bay). Participants were informed about the study by clinic staff members and after expressing initial interest, were provided with detailed information and screened for enrollment eligibility including a literacy assessment. Upon execution of informed consent, participants completed a self-administered 45-minute questionnaire on paper or via secured laptop computer. Information regarding demographics, HIV clinical outcomes, and substance use and misuse was collected. Participants received $25.00 for completion of the study. Survey information was then linked to surveillance databases maintained by the Florida Department of Health and the participant’s electronic medical record maintained by the study clinics. The Institutional Review Boards of the University of Florida, Florida International University, and the Florida Department of Health approved this study.
Measures:
Cigarette Smoking:
Participants were dichotomized based on whether or not they endorsed a single item asking, “Do you currently smoke cigarettes?”
Binge Drinking:
Binge drinking was defined as consuming 5 or more alcoholic drinks on the same occasion on at least 1 day in the past 30 days for men, and 4 or more alcoholic drinks for women, consistent with the Centers for Disease Control and Prevention Behavioral Risk Factor Surveillance System and the Substance Abuse and Mental Health Services Administration (SAMHSA) criteria. Participants were dichotomized based on their responses to this item (SAMHSA, 2017).
Drug Use:
Participants answered a dichotomous yes/no question pertaining to their use of substances use over the past 12 months. For analytic purposes, we examined the most prevalently reported substances, such as self-reported marijuana, crack, cocaine, ecstasy, sedatives, opioids, and injection drug use (i.e., intravenous heroin and/or stimulant use).
Birth Cohort:
Previous investigations examining cohort differences among HIV-positive adults have dichotomized older and younger adults (Johnson, Striley, & Cottler, 2007; Whitehead et al., 2014; Zanjani, Saboe, & Oslin, 2007), limiting potential variability between more distinct groups. Nelson and colleagues (2016) previously examined the effect of birth cohort on sexual risk-taking among men who have sex with men, demonstrating that decade of birth relative to the HIV epidemic was significantly associated with risky sexual behavior. In line with their stratification, participants were categorized into four birth cohorts based on the decade in which they were born, resulting in a group of individuals born in the 1990’s, 1980’s, 1970’s, and adults born before the 1970’s. As mentioned, these decades signify important sociopolitical changes within the context of substance use and the HIV epidemic during the formative years of these adults’ lives.
Covariates:
Demographics (i.e., race/ethnicity, sex, employment status, housing status, educational attainment, and sexual identity) were collected. Race/ethnicity categories were Black, White, Hispanic, and Other (i.e., Native American, Asian, Multi-Racial, and Unknown). Participants were categorized as male or female depending on their assigned sex at birth. Employment status was categorized as currently employed or not employed. Educational attainment was divided into the categories of less than high school, high school, and more than high school. Housing status was categorized into stable (own, rented, or stayed in house or apartment with family or friends), unstable (treatment facility, emergency shelter, motel, church), or homeless (car, street, or abandoned building) in the past 12 months. Sexual identity was categorized into heterosexual, homosexual, and bisexual. Years since diagnosis was a continuous variable assessing the number of years since participants received an HIV-positive diagnosis from a healthcare provider.
Statistical Analyses
Authors first calculated the prevalence of use of each substance by dividing the number of users over the total number of participants in each age group. Bivariate analyses were conducted using chi-square and one-way ANOVA analyses to assess differences in demographics, HIV health variables, and substance use between birth cohorts. To further assess the association between the primary independent variable, birth cohort, and dichotomous substance use outcome variables, we conducted multivariate logistic regression analyses controlling for potential confounding variables associated with birth cohort and substance use in bivariate analysis (p<0.10; i.e., sex, race, employment, education, housing, and sexual identity), and presented adjusted odds ratios with 95% confidence intervals. Individual models were created for substances significantly associated with birth cohort, as well as substances trending towards significance at the bivariate level (p<.10; i.e., binge drinking, cigarettes, marijuana, crack, ecstasy, and injection drug use). All multivariate analyses investigating the relationship between birth cohort and substance use utilized the <1970 group as the referent group, as this was the largest birth cohort of the four. All statistical analyses were conducted using SPSS Version 22 (SPSS, Version 22; IBM, Armonk, NY).
Sample Description
The sample (N = 934) had a mean age of 46.64 years (SD = 11.24). The mean age of each birth cohort was 54.1 (SD=5.9; <1970’s), 41.5 (SD=3.1; 1970’s), 31.3 (SD=3.1; 1980’s), and 23.2 (SD=1.7; 1990’s). The mean age between birth cohorts was significantly different (F (3,933) = 1273.48, p<.001). The racial/ethnic breakdown was as follows: Black (55.4%), White (20.8%), Hispanic (20.1%), and Other (3.7%). The majority of participants (66.4%) were men. Nearly an equivalent number of participants reported obtaining less than a high school degree and a degree beyond high school, 34.5% vs. 35.8% respectively. The majority of participants (80.9%) reported being currently single, widowed, divorced, or separated. The majority (53.1%) of participants identified as heterosexual, while 36.7% identified as gay, and 10.2% were bisexual. Mean years since HIV diagnosis was 11.43 years (SD = 7.66). Approximately, 30% of the sample reported less than 95% ART adherence. For additional sample information, please refer to Table 1.
Table I:
Sociodemographics and treatment adherence by birth cohort (N=934)
| Variable | Category | <1970 Mean (SD) or N (%) |
1970–1979 Mean (SD) or N (%) |
1980–1989 Mean (SD) or N (%) |
1990–1999 Mean (SD) or N (%) |
Total Mean (SD) or N (%) |
Chi-Square Value (d.f.) or ANOVA F-Value (d.f.) |
P-Value |
|---|---|---|---|---|---|---|---|---|
| Age | 54.1 (5.9) | 41.5 (3.1) | 31.3 (3.1) | 23.2 (1.7) | 46.64 (11.2) | 1273.48 (933) | <.001 | |
| Sex | Male | 359 (64.5) | 118 (61.5) | 102 (74.5) | 41 (85.4) | 620 (66.4) | 14.80 (3) | .002 |
| Female | 198 (35.5) | 74 (38.5) | 35 (25.5) | 7 (14.6) | 314 (33.6) | |||
| Race | Hispanic | 111 (19.9) | 35 (18.2) | 34 (24.8) | 8 (16.7) | 188 (20.1) | 30.65 (9) | <.001 |
| Not Hispanic, White | 127 (22.8) | 38 (19.8) | 17 (12.4) | 12 (25) | 194 (20.8) | |||
| Not Hispanic, Black | 308 (55.3) | 112 (58.3) | 75 (54.7) | 22 (45.8) | 517 (55.4) | |||
| Not Hispanic, Other | 11 (2) | 7 (3.6) | 11 (8) | 6 (12.5) | 35 (3.7) | |||
| Education | <High School | 206 (37.2) | 71 (37.2) | 37 (27) | 7 (14.6) | 321 (34.5) | 15.10 (6) | .019 |
| High School diploma or equivalent | 163 (29.4) | 53 (27.7) | 42 (30.7) | 18 (37.5) | 276 (29.7) | |||
| >High School | 185 (33.4) | 67 (35.1) | 58 (42.3) | 23 (47.9) | 333 (35.8) | |||
| Marital Status | Married/Living with a long-term partner | 95 (17.1) | 42 (22) | 31 (22.6) | 10 (20.8) | 178 (19.1) | 3.58 (3) | .309 |
| Divorced/Widowed/Separated/Single | 459 (82.9) | 149 (78) | 106 (77.4) | 38 (79.2) | 752 (80.9) | |||
| Employment | Unemployed | 446 (82.4) | 133 (72.3) | 85 (62.5) | 23 (47.9) | 687 (75.6) | 47.38 (3) | <.0001 |
| Employed | 95 (17.6) | 51 (27.7) | 51 (37.5) | 25 (52.1) | 222 (24.4) | |||
| Housing | Stable | 351 (64.1) | 99 (52.3) | 61 (45.1) | 18 (37.5) | 529 (57.5) | 42.22 (6) | <.001 |
| Unstable | 110 (20.1) | 55 (29.1) | 45 (33.3) | 26 (54.1) | 236 (25.6) | |||
| Homeless | 86 (15.8) | 35 (18.5) | 29 (21.4) | 4 (8.3) | 154 (16.8) | |||
| Sexual Identity | Heterosexual | 311 (59.6) | 96 (53.6) | 44 (33.1) | 17 (35.4) | 468 (53.1) | 39.34 (6) | <.0001 |
| Homosexual | 160 (30.7) | 65 (36.3) | 72 (54.1) | 27 (56.3) | 324 (36.7) | |||
| Bisexual | 51 (9.8) | 18 (10.1) | 17 (12.8) | 4 (8.3) | 90 (10.2) | |||
| ART Adherence | <=95% | 136 (24.7) | 58 (37.9) | 36 (33.6) | 14 (37.8) | 244 (30.7) | 7.55 (3) | .056 |
| >95% | 360 (75.3) | 95 (62.1) | 71 (66.4) | 23 (62.2) | 549 (69.3) |
Note. The number of participants per birth cohort was as follows:
<1970’s (n=557), 1970–1979 (n=192), 1980–1989 (n=137), 1990–1999 (n=48), total (N=934). N may vary slightly according to missing data.
RESULTS
Substance Use Prevalence
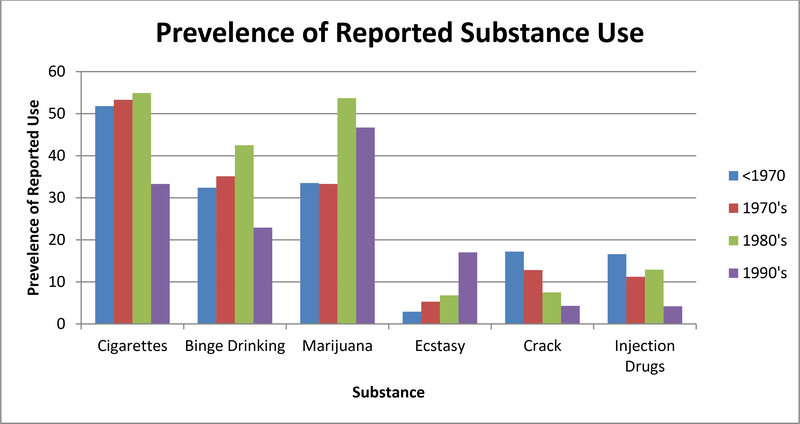
Regarding substance use, 34.0% of participants reported at least one binge drinking episode during the past month, and 51.6% reported currently smoking cigarettes. Approximately 37% of participants reported using marijuana in the past 12 months, while 36.1% reported using an illicit substance other than marijuana. The most commonly reported illicit substances used during the past 12 months were injection drugs (14.3%), crack (14.1%), opioids (10.7%), sedatives (10.9%), cocaine (9.9%), and ecstasy (4.7%) (Figure 1).
Figure I.
Prevalence of Past 12 Month Self-Reported Substance Use by Birth Cohort
Current cigarette smoking was the least prevalent in the youngest (e.g., 1990’s) group with only 33% reporting current use, while over 50% of adults in the other birth cohorts reported current cigarette use. Binge drinking was also least likely to be reported by the youngest group compared to all other birth cohorts; 22% versus >32% for all other groups. Approximately 46.7% and 53.7% of the 1990’s and 1980’s cohorts reported marijuana use respectively. Additionally, 17.2% and 16.6% of the <1970’s birth cohort reported using crack and injection drugs respectively, the highest reported use compared to the other birth cohorts See Table 2.
Table II:
Substance Use by birth cohort (N=934)
| Variable | Category | <1970 N (%) |
1970–1979 N (%) |
1980–1989 N (%) |
1990–1999 N (%) |
Total N (%) |
Chi-Square Value (d.f.) |
P-value |
|---|---|---|---|---|---|---|---|---|
| Cigarettes | No | 256 (48.2) | 85 (46.7) | 60 (45.1) | 32 (66.7) | 433 (48.4) | 7.20 (3) | .065 |
| Yes | 275 (51.8) | 97 (53.3) | 73 (54.9) | 16 (33.3) | 461 (51.6) | |||
| Binge Drinking | No | 355 (67.6) | 122 (64.9) | 77 (57.5) | 37 (77.1) | 591 (66) | 7.69 (3) | .053 |
| Yes | 170 (32.4) | 66 (35.1) | 57 (42.5) | 11 (22.9) | 304 (34) | |||
| Marijuana | No | 325 (66.5) | 114 (66.7) | 57 (46.3) | 24 (53.3) | 520 (62.8) | 19.89 (3) | <.001 |
| Yes | 164 (33.5) | 57 (33.3) | 66 (53.7) | 21 (46.7) | 308 (37.2) | |||
| Crack | No | 434 (82.8) | 164 (87.2) | 123 (92.5) | 45 (95.7) | 766 (85.9) | 12.86 (3) | .004 |
| Yes | 90 (17.2) | 24 (12.8) | 10 (7.5) | 2 (4.3) | 126 (14.1) | |||
| Cocaine | No | 479 (91.6) | 168 (89.4) | 118 (88.7) | 38 (80.9) | 803 (90.1) | 6.21 (3) | .10 |
| Yes | 44 (8.4) | 20 (10.6) | 15 (11.3) | 9 (19.1) | 88 (9.9) | |||
| Opioids | No | 457 (87.7) | 170 (90.4) | 125 (94) | 42 (89.4) | 794 (89.3) | 4.67 (3) | .197 |
| Yes | 64 (12.3) | 18 (9.6) | 8 (6) | 5 (10.6) | 95 (10.7) | |||
| Sedatives | No | 464 (89.1) | 171 (91) | 116 (87.2) | 41 (87.2) | 792 (89.1) | 1.32 (3) | .724 |
| Yes | 57 (10.9) | 17 (9) | 17 (12.8) | 6 (12.8) | 97 (10.9) | |||
| Ecstasy | No | 506 (97.1) | 178 (94.7) | 124 (93.2) | 39 (83) | 847 (95.3) | 21.11 (3) | <.001 |
| Yes | 15 (2.9) | 10 (5.3) | 9 (6.8) | 8 (17) | 42 (4.7) | |||
| Injection Drugs | No | 431 (83.4) | 165 (88.8) | 114 (87.1) | 45 (95.8) | 755 (85.7) | 7.72 (3) | .052 |
| Yes | 86 (16.6) | 21 (11.2) | 17 (12.9) | 2 (4.2) | 126 (14.3) |
Note. The number of participants per birth cohort was as follows:
<1970’s (n=557), 1970–1979 (n=192), 1980–1989 (n=137), 1990–1999 (n=48), total (N=934). N may vary slightly according to missing data.
Self-Reported Substance Use Differences between Birth Cohorts
Substances (i.e., cigarettes, binge drinking, marijuana, ecstasy, non-injection crack, & injection drugs) evidencing significant group differences or trending towards significance (p <.10) were further examined utilizing adjusted binary logistic regressions with the oldest birth cohort (i.e., <1970) as the referent group.
After adjusting for the covariates of sex, race, employment, education, housing status, and sexual identity, the relationship between birth cohort and self-reported substance use was re-examined for each substance. Marijuana use was significant, with the 1980’s group reporting significantly greater use (AOR=2.37, 95% CI=1.51–3.69, p<.001) than the oldest group. Adjusted analysis of ecstasy use revealed that the 1970’s group (AOR=2.71, 95% CI=1.05–7.00, p=.039), 1980’s group (AOR=3.22, 95% CI=1.21–8.59, p=.019), and 1990’s group (AOR=10.32, 95% CI=3.41–31.23, p<.001) all had a significantly greater odds of use compared the oldest group. The opposite relationship was seen with crack use, as adjusted analysis showed that the 1970’s group (AOR=0.55, 95% CI=0.32–0.94, p=.032), 1980’s group (AOR=0.34, 95% CI=0.16–0.72, p=.004), and 1990’s group (AOR=0.21, 95% CI=0.04–0.93, p=.041) all used significantly less than the oldest birth cohort. The most recent birth cohort (1990’s) also demonstrated an 80% reduction in injection drug use (AOR=0.20, 95% CI=0.04–0.89, p=.036) compared with the <1970’s group. For additional results regarding birth cohorts and covariates, please refer to Table 3.
Table III:
Adjusted Odds ratios and 95% CI’s for Birth Cohorts and Past 12 Month Substance Use (N=934)
| Variable | Cigarettes (CI) | p | Binge Drinking AOR (CI) |
p | Marijuana AOR (CI) |
p | Ecstasy AOR (CI) |
p | Crack AOR (CI) |
p | Injection Drugs, AOR (CI) | p |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Birth Cohort | ||||||||||||
| <1970’s (Referent) |
||||||||||||
| 1970’s | 1.09 (0.74–1.58) |
.652 | 1.03 (0.71–1.50) |
.869 | 0.98 (0.66–1.46) |
.944 |
2.71 (1.05–7.00) |
.039 |
0.55 (0.32–0.94) |
.032 | 0.71 (0.41–1.23) |
.229 |
| 1980’s | 1.43 (0.93–2.22) |
.102 | 1.44 (0.95–2.20) |
.084 |
2.37 (1.51–3.69) |
<.001 |
3.22 (1.21–8.59) |
.019 |
0.34 (0.16–0.72) |
.005 | 0.78 (0.42–1.45) |
.440 |
| 1990’s | 0.60 (0.30–1.20) |
.151 | 0.53 (0.25–1.11) |
.096 | 1.61 (0.83–3.13) |
.152 |
10.32 (3.41–31.23) |
<.001 |
0.21 (0.04–0.93) |
.041 |
0.20 (0.04–0.89) |
.036 |
| Sexual Identity | ||||||||||||
| Heterosexual (Referent) |
||||||||||||
| Gay | 0.74 (0.50–1.10) |
.140 | 0.98 (0.66–1.46) |
.957 | 1.10 (0.73–1.66) |
.627 | 1.24 (0.51–2.97) |
.629 | 0.92 (0.52–1.62) |
.781 | 0.88 (0.52–1.49) |
.658 |
| Bisexual | 1.18 (0.71–1.97) |
.505 | 1.12 (0.67–1.85) |
.656 | 1.39 (0.82–2.34) |
.216 | 0.73 (0.19–2.78) |
.648 | 1.43 (0.75–2.71) |
.271 | 0.78 (0.37–1.62) |
.513 |
| Sex | ||||||||||||
| Male (Referent) |
||||||||||||
| Female | 0.76 (0.52–1.09) |
.141 | 0.86 (0.59–1.25) |
.439 | 0.70 (0.47–1.05) |
.090 | 0.36 (0.11–1.19) |
.095 | 1.21 (0.73–1.99) |
.477 |
0.51 (0.29–0.90) |
.022 |
| Race | ||||||||||||
| White (Referent) |
||||||||||||
| Black | 1.35 (0.86–2.13) |
.199 | 1.30 (0.82–2.05) |
.263 |
2.00 (1.23–3.25) |
.005 | 1.28 (0.45–3.59) |
.639 |
2.65 (1.16–6.00) |
.020 | 1.55 (0.89–2.69) |
.116 |
| Hispanic | 1.33 (0.86–2.13) |
.147 | 1.20 (0.80–1.79) |
.371 |
1.80 (1.17–2.76) |
.007 | 0.82 (0.32–2.10) |
.688 |
3.28 (1.56–6.88) |
.002 |
0.47 (0.27–0.81) |
.007 |
| Other | 1.71 (0.73–3.99) |
.209 | 1.46 (0.64–3.32) |
.367 |
2.38 (1.01–5.58) |
.045 | 0.45 (0.05–4.14) |
.484 | 1.33 (0.26–6.89) |
.727 | 0.56 (0.15–2.07) |
.516 |
| Employment Status | ||||||||||||
| Unemployed (Referent) |
||||||||||||
| Employed |
0.55 (0.39–0.79) |
.001 | 1.27 (0.89–1.81) |
.186 | 0.99 (0.68–1.44) |
.989 | 1.33 (0.59–2.99) |
.486 | 0.90 (0.51–1.57) |
.712 |
0.51 (0.29–0.88) |
.017 |
| Education | ||||||||||||
| < High school (Referent) |
||||||||||||
| High school | 0.85 (0.59–1.23) |
.410 | 0.74 (0.52–1.07) |
.115 | 1.20 (0.82–1.76) |
.335 | 1.33 (0.55–3.22) |
.522 | 0.65 (0.39–1.08) |
.098 | 1.08 (0.63–1.84) |
.777 |
| >High school |
0.43 (0.30–0.63) |
<.001 |
0.53 (0.36–0.77) |
.001 | 0.76 (0.51–1.13) |
.187 | 0.71 (0.26–1.90) |
.500 | 0.70 (0.41–1.18) |
.185 | 1.31 (0.78–2.22) |
.302 |
| Housing Status | ||||||||||||
| Stable (Referent) |
||||||||||||
| Unstable | 1.12 (0.79–1.59) |
.507 | 1.29 (0.91–1.85) |
.149 | 1.01 (0.69–1.47) |
.953 | 1.21 (0.45–3.21) |
.695 |
2.30 (1.37–3.86) |
.001 | 1.54 (0.92–2.55) |
.094 |
| Homeless |
2.22 (1.45–3.41) |
<.001 |
1.72 (1.16–2.59) |
.007 |
1.75 (1.15–2.65) |
.009 |
5.33 (2.25–12.62) |
<.001 |
4.70 (2.82–7.86) |
<.001 |
2.57 (1.52–4.33) |
<.001 |
Note. Controlled for sexual identity, sex, race, employment status, education & housing status
DISCUSSION
The results of the present study suggest significant differences in self-reported substance use behavior between four distinct birth cohorts of PLWH in Florida. The study population was recruited from a number of unique sites around the state, thereby providing a sample of the epidemic across Florida. Our findings highlight the importance of addressing substance use among older (e.g., <1970) adults living with HIV, an ongoing and understudied issue that has implications for increasing HIV incidence and contributing to poorer health outcomes in this population. Our results evidenced greater marijuana use among the most recent birth cohorts, while older adults reported a higher prevalence of crack and injection drug use. Our findings are in line with previous investigations suggesting a higher prevalence of marijuana use and ecstasy use in younger HIV-positive adults, and more prevalent stimulant use in HIV-positive older adults (Pappas & Halkitis, 2011; Whitehead et al., 2014). Our findings regarding prevalence of cigarette use (51.6%) and binge drinking (34.0%) are consistent with previous literature suggesting that up to 50% of PLWH report current use (Rahmanian et al., 2011). Self-reported prevalence of alcohol use and cigarettes use, in addition to cocaine, sedative, and opioid use did not differ significantly by birth cohort. Consistent with a robust literature regarding health disparities, homeless adults had significantly greater odds of using any of the substances examined in multivariable analyses, while racial/ethnic minorities (i.e., Blacks and Hispanics) had greater odds of reported marijuana and crack use. These findings speak to a need to continue to address the implications of health disparities and substance use among underserved and underrepresented populations.
Of note, the <1970 birth cohort group reported a significantly higher prevalence of current crack use relative to the younger groups, and this group also evidenced a significantly higher prevalence of injection drug use relative to the youngest group. Stress, anxiety, and loneliness are prevalent among HIV-positive older adults, while depression has been shown to be associated with younger age in PLWH, and as such, we hypothesize that such factors in our sample may have contributed to higher rates of associated substance use between birth cohorts (Bhatia & Munjal, 2014; Kalichman, Heckman, Kochman, Sikkema, & Bergholte, 2000; Eller et al., 2013; Mannes et al., 2016; Rueda et al., 2014).
We hypothesize that findings among the older birth cohorts are a contemporary manifestation of the crack epidemic of the mid 1980’s and early 1990’s (Chiasson et al., 1991; Edlin et al., 1994). Individuals who first began to use crack during this period have aged and may continue to use crack (Johnson & Sterk, 2003). Younger individuals in our sample reported a lower prevalence of crack use, as their onset of substance use occurred after this period when the perception of crack use became decidedly more negative and less socially acceptable. Alternatively, “late-onset” users may also be driving our findings (Johnson & Sterk, 2003).
Our findings regarding the higher prevalence of crack and injection drug use among the older adult cohort are particularly relevant to the HIV epidemic in Florida. First, crack use is a well-documented risk factor of HIV-transmission due to its association with engaging in risky sexual behavior, including greater number of sexual partners, overlapping sexual network members, and unprotected sex (Azevedo, Botega, & Guimarães, 2007; Chiasson et al., 1991; Harzke, Williams, & Bowen, 2009). Additionally, the higher prevalence of injection drug use among older HIV-positive adults in our sample is similar to trends observed in HIV-negative adults (Armstrong, 2007). Though there were no significant age differences in opioid use in our sample, previous findings have indicated that opioids were most commonly prescribed for non-cancer related pain in HIV-positive older adults compared to uninfected individuals from 1999–2010 (Becker et al., 2016). Given the findings of Becker and colleagues, along with results from our study evidencing increased injection drug use among the older groups, alternative pain management strategies may be helpful in reducing opioid use and injection drug use in this population. For example, cognitive behavioral therapies may provide an effective alternative to managing longstanding pain commonly experienced by HIV-positive adults.
Over half (51.7%) of the two most recent birth cohorts reported recently using marijuana. These findings are largely consistent with those suggesting a rise in drug use since 2002 driven largely by marijuana use in younger adults (Carliner et al., 2017). Previous research suggests that marijuana use may be more acceptable than tobacco use in younger people due to lower perceived harm (Berg et al., 2015). This finding was relevant to our sample, as a larger proportion of younger adults reported smoking marijuana versus smoking cigarettes, while older adults were more likely to report current use of cigarettes. Alternatively, our observed differences in marijuana and/or ecstasy use may be more related to increased propensity toward sensation-seeking behaviors, as the literature suggests this characteristic is more common in younger individuals (Steinberg et al., 2008).
Despite the high prevalence of crack and injection drug use among HIV-positive older adults observed in this study, previous investigations have evidenced a lack of treatment seeking related to substance misuse in this population. Ompad and colleagues (2016) noted that 27.3% of individuals in this population who currently met criteria for substance dependence had never been in treatment, with an additional 34.8% not currently in treatment. Our results emphasize the importance of continued examination and treatment of substance use and misuse among HIV-positive older adults, specifically interventions related to treatment of crack and injection drug use, substances that have been implicated as both direct and indirect vectors of HIV transmission. Though healthcare utilization was not assessed in our current study, the observed high prevalence of crack and injection drug use among HIV-positive older adults in our sample support calls for integrated mental health and primary care services for identifying, intervening, and referring substance misusers to appropriate treatment programs. Specifically, Screening, Brief Intervention, and Referral to Treatment (SBIRT) interventions may be modifiable to address the needs of this population (Ondersma, Martino, Svikis, & Yonkers, 2017). Additionally, in regard to injection drug use, distribution of clean needles through needle exchange programs has been previously shown to be successful at promoting safer practices and reducing HIV transmission, while access to opiate replacement programs (e.g., methadone maintenance) may also reduce the use of injection drugs in our adult sample (Adamson, Jackson, & Gahagan, 2017; De Maeyer et al., 2011; Kerr et al., 2010; Parker, Jackson, Dykeman, Gahagan, & Karabanow, 2012).
Future studies should explore longitudinal trends of drug use trajectories, specifically the relationship between drug use in early adulthood and crack and injection drug use in late adulthood. In doing so, studies should seek to assess the determinants of drug use relapse should adults report ceasing use at any point during this period. In a cross sectional latent class analyses conducted by Green and colleagues (2010), current injection drug users and multidrug users reported the highest prevalence of AIDS associated illness and psychiatric distress compared to the other classified groups. Authors also noted that a proportion of HIV-positive adults transitioned from injection to non-injection drug use (Green et al., 2010). Further exploration of the transitions from lower-risk substance use to higher-risk substance use, and vice versa, would help to provide appropriate substance use treatment for HIV-positive individuals at critical age junctures.
Our study has several strengths and limitations. This study did not examine the exact quantity and frequency of drug use among participants, as we exclusively analyzed dichotomous self-report data. Secondly, our study utilized a cross-sectional design, thus we cannot determine the temporality of the observed relationships. Consequently, authors cannot untangle the unique influences of age, cohort effects, and influential historical periods on current substance use, as we did not examine substance use trajectories across time. Additionally, all participants were HIV-positive adults enrolled in care within the state of Florida, and thus our findings may not generalize to all PLWH in other geographical regions. However, previous research has highlighted similar trends in adults living with HIV to those observed in our study (Pappas & Halkitis, 2011; Vance et al., 2011; Whitehead et al., 2014). Lastly, all injection drug users were categorized together due to the increased risk of HIV transmission as compared to alternative routes of drug administration. This limited our ability to assess differences in the prevalence of distinct classifications of injection drugs (e.g., heroin, methamphetamines, and crack) and assess whether there were differences across birth cohorts. Despite these limitations, this study elucidated significant differences in the prevalence rates of substance use among birth cohorts of adults living with HIV, while controlling for significant confounding variables. Moreover, our sample was geographically heterogeneous and contained high levels of racial and ethnic diversity. Therefore, we believe our findings constitute a substantial and relevant contribution to the literature regarding the differences in substance use and misuse between birth cohorts of adults living with HIV.
CONCLUSIONS
These findings compare the prevalence of substance use among PLWH by birth cohort, resulting in significant differences in current substance use between cohorts. Younger adults evidenced significantly greater self-reported prevalence of marijuana and ecstasy use, while older adults had a significantly greater likelihood of reporting use of crack and injection drugs. This work has direct implications for clinicians serving this population. An understanding of current age differences in substance use among PLWH is necessary so that healthcare professionals can provide more effective interventions, thereby improving health outcomes among this population. Improvement of health outcomes among PLWH continues to be a priority, as maintenance of optimal health among PLWH will reduce the risk of HIV transmission among same age counterparts not currently infected with HIV, as well as provide improved longstanding quality of life for individuals living with HIV. Knowledge of current substance use and misuse patterns will continue to be important for appropriate screening and referral to substance abuse treatments in this population.
Acknowledgements:
This study was funded by the National Institute on Alcohol Abuse and Alcoholism (NIAAA) under grant number U24AA022002, the National Institute on Drug Abuse (NIDA) under grant number 1K23DA039769–01 and NIDA UF Substance Abuse Training Center under grant number T32DA035167.
Footnotes
Disclosure statement
The authors report no conflicts of interest.
REFERENCES
- Abuse S (2011). Results from the 2010 National Survey on Drug Use and Health: Summary OfNational Findings. [Google Scholar]
- Adamson K, Jackson L, & Gahagan J (2017). Young people and injection drug use: Is there a need to expand harm reduction services and support? International Journal of Drug Policy, 39, 14–20. [DOI] [PubMed] [Google Scholar]
- Allyn D (2001). Make love, not war: The sexual revolution: An unfettered history. New York: Routledge. [Google Scholar]
- Armstrong GL (2007). Injection drug users in the United States, 1979–2002: an aging population. Archives of internal medicine, 167(2), 166–173. [DOI] [PubMed] [Google Scholar]
- Arnsten JH, Demas PA, Grant RW, Gourevitch MN, Farzadegan H, Howard AA, & Schoenbaum EE (2002). Impact of Active Drug Use on Antiretroviral Therapy Adherence and Viral Suppression in HIV‐infected Drug Users. Journal of general internal medicine, 17(5), 377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Azevedo R. C. S. d., Botega NJ, & Guimarães LAM (2007). Crack users, sexual behavior and risk of HIV infection. Revista Brasileira de Psiquiatria, 29(1), 26–30. [PubMed] [Google Scholar]
- Baum MK, Rafie C, Lai S, Sales S, Page B, & Campa A (2009). Crack-cocaine use accelerates HIV disease progression in a cohort of HIV-positive drug users. JAIDS Journal of Acquired Immune Deficiency Syndromes, 50(1), 93–99. [DOI] [PubMed] [Google Scholar]
- Becker WC, Gordon K, Edelman EJ, Kerns RD, Crystal S, Dziura JD, . . . Justice AC (2016). Trends in any and high-dose opioid analgesic receipt among aging patients with and without HIV. AIDS and Behavior, 20(3), 679–686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berg CJ, Stratton E, Schauer GL, Lewis M, Wang Y, Windle M, & Kegler M (2015). Perceived Harm, Addictiveness, and Social Acceptability of Tobacco Products and Marijuana Among Young Adults: Marijuana, Hookah, and Electronic Cigarettes Win. Substance Use & Misuse, 50(1), 79–89. doi: 10.3109/10826084.2014.958857 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhatia M, & Munjal S (2014). Prevalence of Depression in People Living with HIV/AIDS Undergoing ART and Factors Associated with it. Journal of clinical and diagnostic research: JCDR, 8(10), WC01–04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonn-Miller MO, Oser ML, Bucossi MM, & Trafton JA (2014). Cannabis use and HIV antiretroviral therapy adherence and HIV-related symptoms. Journal of behavioral medicine, 37(1), 1–10. [DOI] [PubMed] [Google Scholar]
- Brewer TH, Zhao W, Metsch LR, Coltes A, & Zenilman J (2007). High-risk behaviors in women who use crack: Knowledge of HIV serostatus and risk behavior. Annals of epidemiology, 17(7), 533–539. [DOI] [PubMed] [Google Scholar]
- Callander D, & Senn C (2013). Examining the Role of Relationships, Body Image, Closeness to HIV/AIDS, and HIV Optimism in the Sexual Risks of Young Men Who Have Sex With Men. Journal of HIV/AIDS & Social Services, 12(2), 205–223. doi: 10.1080/15381501.2013.790869 [DOI] [Google Scholar]
- Carey JW, Mejia R, Bingham T, Ciesielski C, Gelaude D, Herbst JH, . . . Jenkins RA. (2009). Drug use, high-risk sex behaviors, and increased risk for recent HIV infection among men who have sex with men in Chicago and Los Angeles. AIDS and Behavior, 13(6), 1084. [DOI] [PubMed] [Google Scholar]
- Carliner H, Mauro PM, Brown QL, Shmulewitz D, Rahim-Juwel R, Sarvet AL, . . . Hasin DS. (2017). The widening gender gap in marijuana use prevalence in the US during a period of economic change, 2002–2014. Drug and alcohol dependence, 170, 51–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2016). Diagnoses of HIV infection in the United States and dependent areas, 2015. HIV Surveillance Report, 27, 1–114. [Google Scholar]
- Chander G (2010). Assessing substance use among patients living with HIV/AIDS: the role of harm reduction and treatment. Paper presented at the Proceedings. [Google Scholar]
- Chiasson MA, Stoneburner RL, Hildebrandt DS, Ewing WE, Telzak EE, & Jaffe HW (1991). Heterosexual transmission of HIV-1 associated with the use of smokable freebase cocaine (crack). Aids, 5(9), 1121–1126. [DOI] [PubMed] [Google Scholar]
- Cohler B (2007). Writing Desire: Sixty years of gay autobiography. Madison, WI: University of Wisconsin Press. [Google Scholar]
- Crane HM, McCaul ME, Chander G, Hutton H, Nance RM, Delaney JA, . . . Mugavero MJ(2017). Prevalence and Factors Associated with Hazardous Alcohol Use Among Persons Living with HIV Across the US in the Current Era of Antiretroviral Treatment. AIDS and Behavior, 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Maeyer J, Vanderplasschen W, Camfield L, Vanheule S, Sabbe B, & Broekaert E (2011). A good quality of life under the influence of methadone: A qualitative study among opiate-dependent individuals. International journal of nursing studies, 48(10), 1244–1257. [DOI] [PubMed] [Google Scholar]
- Edlin BR, Irwin KL, Faruque S, McCoy CB, Word C, Serrano Y, . . . Holmberg SD (1994). Intersecting epidemics--crack cocaine use and HIV infection among inner-city young adults. New England Journal of Medicine, 331(21), 1422–1427. [DOI] [PubMed] [Google Scholar]
- Eller LS, Bunch EH, Wantland DJ, Portillo CJ, Reynolds NR, Nokes KM, ... & Hamilton MJ. (2010). Prevalence, correlates, and self-management of HIV-related depressive symptoms. AIDS care, 22(9), 1159–1170. [DOI] [PubMed] [Google Scholar]
- Florida Department of Health (FL DOH). (2017). Florida HIV/AIDS Surveillance Program. Retrieved from http://www.floridahealth.gov/diseases-and-conditions/aids/surveillance/index.html
- Friedland G, & Vlahov D (2011). Integration of buprenorphine for substance-abuse treatment by HIV care providers: LWW. [DOI] [PubMed] [Google Scholar]
- Goulet JL, Fultz SL, Rimland D, Butt A, Gibert C, Rodriguez-Barradas M, . . . Justice AC. (2007). Aging and infectious diseases: do patterns of comorbidity vary by HIV status, age, and HIV severity? [Research Support, N.I.H., Extramural [DOI] [PMC free article] [PubMed] [Google Scholar]
- Research Support, Non-U.S. Gov’t]. Clin Infect Dis, 45(12), 1593–1601. doi: 10.1086/523577 [DOI] [Google Scholar]
- Green TC, Kershaw T, Lin H, Heimer R, Goulet JL, Kraemer KL, . . . Bryant K. (2010). Patterns of drug use and abuse among aging adults with and without HIV: a latent class analysis of a US Veteran cohort. Drug and alcohol dependence, 110(3), 208–220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Group W-H (2003). Preliminary development of the World Health Organsiation’s Quality of Life HIV instrument (WHOQOL-HIV): analysis of the pilot version. Social Science & Medicine, 57(7), 1259–1275. [DOI] [PubMed] [Google Scholar]
- Han B, Gfroerer JC, Colliver JD, & Penne MA (2009). Substance use disorder among older adults in the United States in 2020. Addiction, 104(1), 88–96. [DOI] [PubMed] [Google Scholar]
- Harzke AJ, Williams ML, & Bowen AM (2009). Binge use of crack cocaine and sexual risk behaviors among African-American, HIV-positive users. AIDS and Behavior, 13(6), 1106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatzenbuehler ML, O’Cleirigh C, Grasso C, Mayer K, Safren S, & Bradford J (2012). Effect of same-sex marriage laws on health care use and expenditures in sexual minority men: a quasi-natural experiment. [Research Support, N.I.H., Extramural [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson SD, Striley C, & Cottler LB (2007). Comorbid substance use and HIV risk in older African American drug users. Journal of aging and health, 19(4), 646–658. [DOI] [PubMed] [Google Scholar]
- Johnson WA, & Sterk CE (2003). Late-onset crack users: an emergent HIV risk group. JAIDS Journal of Acquired Immune Deficiency Syndromes, 33, S229–S232. [PubMed] [Google Scholar]
- Kalichman SC, Heckman T, Kochman A, Sikkema K, & Bergholte J (2000). Depression and thoughts of suicide among middle-aged and older persons living with HIV-AIDS. Psychiatric Services, 51(7), 903–907. [DOI] [PubMed] [Google Scholar]
- Kerr T, Small W, Buchner C, Zhang R, Li K, Montaner J, & Wood E (2010). Syringe sharing and HIV incidence among injection drug users and increased access to sterile syringes. American journal of public health, 100(8), 1449–1453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lucas GM, Griswold M, Gebo KA, Keruly J, Chaisson RE, & Moore RD (2006). Illicit drug use and HIV-1 disease progression: a longitudinal study in the era of highly active antiretroviral therapy. American Journal of Epidemiology, 163(5), 412–420. [DOI] [PubMed] [Google Scholar]
- Mackellar DA, Hou SI, Whalen CC, Samuelsen K, Valleroy LA, Secura GM, . . . Torian LV. (2011). A plausible causal model of HAART-efficacy beliefs, HIV/AIDS complacency, and HIV-acquisition risk behavior among young men who have sex with men. AIDS Behav, 15(4), 788–804. doi: 10.1007/s10461-010-9813-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magodoro IM, Esterhuizen TM, & Chivese T (2016). A cross-sectional, facility based study of comorbid non-communicable diseases among adults living with HIV infection in Zimbabwe. BMC Research Notes, 9(1), 379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahy M, Autenrieth CS, Stanecki K, & Wynd S (2014). Increasing trends in HIV prevalence among people aged 50 years and older: evidence from estimates and survey data. Aids, 28, S453–S459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mannes ZL, Burrell LE, Bryant VE, Dunne EM, Hearn LE, & Whitehead NE (2016). Loneliness and substance use: the influence of gender among HIV+ Black/African American adults 50+. AIDS care, 28(5), 598–602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mathers BM, Degenhardt L, Phillips B, Wiessing L, Hickman M, Strathdee SA, . . . Toufik A (2008). Global epidemiology of injecting drug use and HIV among people who inject drugs: a systematic review. The Lancet, 372(9651), 1733–1745. [DOI] [PubMed] [Google Scholar]
- McDonald K, Slavin S, Pitts MK, Elliott JH, & HealthMap Project, T. (2016). Chronic Disease Self-Management by People With HIV. [Research Support, Non-U.S. Gov’t]. Qual Health Res, 26(6), 863–870. doi: 10.1177/1049732315600415 [DOI] [PubMed] [Google Scholar]
- Nachega JB, Hislop M, Dowdy DW, Lo M, Omer SB, Regensberg L, . . . Maartens G. (2006). Adherence to highly active antiretroviral therapy assessed by pharmacy claims predicts survival in HIV-infected South African adults. JAIDS Journal of Acquired Immune Deficiency Syndromes, 43(1), 78–84. [DOI] [PubMed] [Google Scholar]
- Nduka C, Uthman O, Kimani P, & Stranges S (2015). Drug Abuse in People Living with HIV in the Era of Highly Active Antiretroviral Therapy: A Systematic Review and Meta-Analysis. J Addict Res Ther, 6(255), 2. [Google Scholar]
- Nelson KM, Gamarel KE, Pantalone DW, Carey MP, & Simoni JM (2016). Sexual debut and HIV-related sexual risk-taking by birth cohort among men who have sex with men in the United States. AIDS and Behavior, 20(10), 2286–2295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okafor CN, Zhou Z, Burrell LE, Kelso NE, Whitehead NE, Harman JS, ... & Cook RL. (2017). Marijuana use and viral suppression in persons receiving medical care for HIV-infection. The American journal of drug and alcohol abuse, 43(1), 103–110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ompad DC, Giobazolia TT, Barton SC, Halkitis SN, Boone CA, Halkitis PN, . . . Urbina A. (2016). Drug use among HIV+ adults aged 50 and older: findings from the GOLD II study. AIDS care, 28(11), 1373–1377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ondersma SJ, Martino S, Svikis DS, & Yonkers KA (2017). Commentary on Kim et al.(2017): Staying focused on non‐treatment seekers. Addiction, 112(5), 828–829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pappas MK, & Halkitis PN (2011). Sexual risk taking and club drug use across three age cohorts of HIV-positive gay and bisexual men in New York City. AIDS care, 23(11), 1410–1416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parker J, Jackson L, Dykeman M, Gahagan J, & Karabanow J (2012). Access to harm reduction services in Atlantic Canada: Implications for non-urban residents who inject drugs. Health & place, 18(2), 152–162. [DOI] [PubMed] [Google Scholar]
- Piette J, Wachtel TJ, Mor V, & Mayer K (1995). The impact of age on the quality of life in persons with HIV infection. Journal of Aging and Health, 7(2), 163–178. [DOI] [PubMed] [Google Scholar]
- Poindexter CC (1997). Sociopolitical antecedents to Stonewall: analysis of the origins of the gay rights movement in the United States. [Historical Article]. Soc Work, 42(6), 607–615. [DOI] [PubMed] [Google Scholar]
- Rahmanian S, Wewers ME, Koletar S, Reynolds N, Ferketich A, & Diaz P (2011). Cigarette smoking in the HIV-infected population. Proceedings of the American Thoracic Society, 8(3), 313–319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reif SS, Whetten K, Wilson ER, McAllaster C, Pence BW, Legrand S, & Gong W (2014). HIV/AIDS in the Southern USA: a disproportionate epidemic. AIDS care, 26(3), 351–359. [DOI] [PubMed] [Google Scholar]
- Robinson WT, Risser JM, McGoy S, Becker AB, Rehman H, Jefferson M, . . . Tortu S. (2006). Recruiting injection drug users: a three-site comparison of results and experiences with respondent-driven and targeted sampling procedures. Journal of Urban Health, 83(1), 29–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenfeld D, Bartlam B, & Smith RD (2012). Out of the closet and into the trenches: gay male Baby Boomers, aging, and HIV/AIDS. Gerontologist, 52(2), 255–264. doi: 10.1093/geront/gnr138 [DOI] [PubMed] [Google Scholar]
- Rueda S, Law S, & Rourke SB (2014). Psychosocial, mental health, and behavioral issues of aging with HIV. Current Opinion in HIV and AIDS, 9(4), 325–331. [DOI] [PubMed] [Google Scholar]
- Slawson G, Milloy M, Balneaves L, Simo A, Guillemi S, Hogg R, . . . Kerr, T. (2015). High-intensity cannabis use and adherence to antiretroviral therapy among people who use illicit drugs in a Canadian setting. AIDS and Behavior, 19(1), 120–127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinberg L, Albert D, Cauffman E, Banich M, Graham S, & Woolard J (2008). Age differences in sensation seeking and impulsivity as indexed by behavior and self-report: evidence for a dual systems model. Developmental psychology, 44(6), 1764. [DOI] [PubMed] [Google Scholar]
- Swan J, & Evans N (2017). HIV/AIDS for Florida Healthcare Professionals.
- Trenz RC, Scherer M, Harrell P, Zur J, Sinha A, & Latimer W (2012). Early onset of drug and polysubstance use as predictors of injection drug use among adult drug users. Addictive Behaviors, 37(4), 367–372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruce RD, Merlin J, Lum PJ, Ahmed E, Alexander C, Corbett AH, Foley K, Leonard K, Treisman GJ, & Selwyn P (2017). 2017 HIVMA of IDSA Clinical Practice Guideline for the Management of Chronic Pain in Patients Living With HIV. Clin Infect Dis, 65(10), e1–e37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vance DE (2010). Aging with HIV: Clinical considerations on an emerging population. The American journal of nursing, 110(3), 42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vance DE, Mugavero M, Willig J, Raper JL, & Saag MS (2011). Aging with HIV: a cross-sectional study of comorbidity prevalence and clinical characteristics across decades of life. Journal of the Association of Nurses in AIDS Care, 22(1), 17–25. [DOI] [PubMed] [Google Scholar]
- Webster LR, & Grabois M (2015). Current regulations related to opioid prescribing. PM&R, 7(11), S236–S247. [DOI] [PubMed] [Google Scholar]
- Whitehead NE, Trenz RC, Keen L, Rose J, & Latimer WW (2014). Younger versus older African Americans: Patterns and prevalence of recent illicit drug use. Journal of ethnicity in substance abuse, 13(2), 126–138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wood E, Montaner J, Yip B, Tyndall MW, Schechter MT, O’Shaughnessy MV, & Hogg RS (2004). Adherence to antiretroviral therapy and CD4 T-cell count responses among HIV-infected injection drug users. Antiviral therapy, 9(2), 229–235. [PubMed] [Google Scholar]
- Zanjani F, Saboe K, & Oslin D (2007). Age difference in rates of mental health/substance abuse and behavioral care in HIV-positive adults. AIDS patient care and STDs, 21(5), 347–355. [DOI] [PubMed] [Google Scholar]