Abstract
Purpose:
To investigate tibial tunnel widening in ACL reconstruction patients over 7-years to establish the effects of initial graft tension on tibial widening and clinical outcomes when using both patellar tendon (BTB) and hamstring tendon (HS) grafts.
Methods:
Ninety patients were reconstructed with BTB or HS autografts were randomized using one of two initial graft tension protocols; 1) tensioned to restore normal anteroposterior laxity (“low-tension”; n=46) and 2) tensioned to over-constrain AP laxity by 2 mm (“high-tension”; n=44). 70 patients had post-surgical data with 45 available for review at 7 years. Tunnel widening was assessed via radiographs at 1, 3, and 7-year follow-up. Patient reported outcomes were compared.
Results:
The mean±95% confidence intervals of the initial diameters for the BTB autografts were 10.3±0.5mm (Low-tension) and 10.2±0.6mm (High-tension) with final diameters of 10.8±0.6mm (Low-tension) and 9.9±0.6mm (High-tension). The initial diameters for HS autografts were 8.1±0.9mm (Low-tension) and 8.4±0.7mm (High-tension) with final diameters of 11.5±1.1mm (Low-tension) and 11.1±0.9mm (High-tension). For subjects with HS autografts, mean tunnel diameters significantly changed over time (p <.001); no significant changes were observed in BTB autografts (p=.29). Change in diameter of the HS autograft group remained significantly greater than the BTB group at all time points for both tension groups (p<.05). No differences in patient reported outcomes were found between tension groups or graft types.
Conclusions:
Patients who undergo ACL-R with HS autograft undergo tibial tunnel widening over 7 years. Patients with BTB autografts did not experience widening, regardless of initial graft tension. Patient reported outcomes were equivalent.
Keywords: ACL, tunnel widening, graft selection, graft tensioning
1.0. Introduction
Anterior cruciate ligament reconstruction (ACL-R) relies on adequate fixation and healing of the graft within the tibial and femoral bone tunnels.[1] However, there is a balance between allowing adequate time for bone healing to occur at the graft-tunnel interface and mobilizing the patient for early rehabilitation following ACL-R. While Rodeo et al showed that early graft tunnel widening may lead to osteoclast mediated tunnel resorption[1], the utility of early postoperative rehabilitation has been well documented with regards to patient reported outcomes.[2–8] Additionally, while tunnel widening is an accepted phenomenon following ACL-R, little is known about the mechanisms and its clinical ramifications. There is disagreement between studies regarding the effects of tunnel expansion on clinical, functional, and patient reported outcomes.[9–15]
Tunnel widening is thought to occur due to biological and mechanical factors related to graft healing.[16,17] Biological factors include host-derived immune response in reaction to foreign bodies such as allograft, or cell death due to heat necrosis from drilling of the tunnels.[16] Mechanical factors may be related to graft selection (autograft versus allograft, bone-patellar tendon-bone (BTB) versus hamstring (HS)), tunnel position, fixation method, graft motion (via early rehabilitation), or the initial tension placed on the graft during fixation.[14–19] Weber et al prospectively examined tunnel widening and suggested that the a decreased distance between graft fixation and tunnel aperture (more stiff graft) results in less widening.[14]
The initial graft tension is also thought to be a potential contributor to tunnel motion and widening.[14,16,20] Taketomi et al reported greater femoral tunnel widening when BTB autografts were tensioned with a manual maximum pull as compared to those tensioned to 80 N (78.6% versus 27.7%, respectively) one year post-operatively, though the clinical outcomes were similar between the two groups. The effect across graft types and the degree of tunnel widening over the long-term was not assessed.
While several studies have evaluated tunnel widening following ACL-R, none compared tunnel widening between graft types under low and high graft tensioning conditions over a 7 year time period.[9,10,25,11–14,21–24] Our objective was to evaluate the progression of tibial tunnel widening over a seven-year post-operative period following ACL-R using BTB or HS autografts fixed under a high or low-initial graft tension. We hypothesized: 1) that patients who underwent ACL-R with HS autografts would exhibit more tibial tunnel widening than those with BTB autografts and 2) that patients with high-tension autografts would undergo greater tibial tunnel widening compared to those with low-tension autografts over a 7-year follow-up period.
2.0. Methods
2.1. Patients
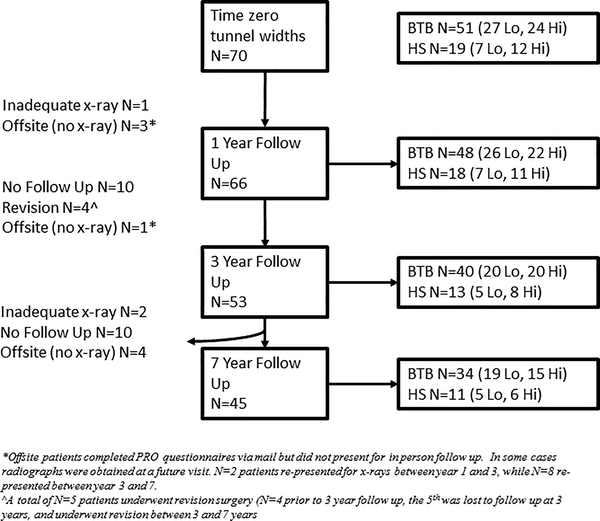
Following Institutional Review Board approval, we retrospectively reviewed the data of 90 patients who underwent ACL-R as part of a previously published prospective, double-blind, randomized controlled trial to assess of the effects of ACL graft tensioning (NCT00434837).[26,27] The analysis presented here is unique and addressed different hypotheses than the original study. The trial was performed at a large tertiary academic center comparing two laxity-based initial graft tension protocols. While the patients were randomized to the two initial graft tension groups, graft type (BTB or HS autografts) was selected by the surgeon and/or patient. Three fellowship trained senior sports surgeons performed the surgeries (PDF, MJH, RMS). Patients were included if they were between the ages 15 and 50, had no history of a previous knee injury, and were undergoing ACL reconstruction using either BTB or HS autografts. The exclusion criteria included allograft, previous or chronic knee injury (greater than 12 months old), presence of concomitant or contralateral knee injuries, partial ACL tears, or a meniscal tear involving greater than one-third of the meniscus. Ninety patients were ultimately included with 46 randomized to the low-tension group and 44 to the high-tension group. For the tunnel widening assessment, 14 patients were excluded as the initial tunnel widths were not dictated in the operative notes, 6 patients did not return for at-least one year of radiographic follow-up, leaving 70 patients available for analysis (Figure 1).
Figure 1.
CONSORT diagram depicting patient participation in the tunnel widening analysis.
2.2. Graft Tensioning Protocol
All autografts were obtained from either the central third of the ipsilateral patellar tendon or a quadruple stranded autograft created from the semitendinosus and gracilis tendons. The three surgeons followed the same operative procedures using the same transtibial drill guide system (Smith & Nephew, Andover, Massachusetts) and anatomic landmarks to select graft insertion sites at the center of the native ACL insertions. All autografts were preconditioned with 20 manual tension cycles before insertion into the joint. For the BTB autografts, the bone blocks were secured using titanium interference screws (7×20, 8×20, or 9×20 mm) (Arthrex, Naples, Florida). The HS autografts were fixed using a button at the outside of the femur (Endobutton, Smith & Nephew) and a biodegradable 8- to 9-mm tapered interference screw on the tibia (Biointrafix, Depuy Mitek, Raynham, Massachusetts) backed up at the surgeon’s discretion with a screw and spiked soft tissue washer. After the femoral end of the graft was fixed, the tension was applied to the graft prior to tibial fixation. For the low-tension assignment, the grafts were firmly tensioned with the knee at 0° of knee flexion. For the high-tension assignment, the grafts were firmly tensioned with the knee at 30° of knee flexion. Tibial fixation was then partially engaged, and the anteroposterior (AP) knee laxity at 20° of flexion was checked using the KT-1000S arthrometer (MEDmetric Corp, San Diego, California) and compared with that of the contralateral knee under anesthesia. Knee angles were confirmed using a sterile goniometer intraoperatively. If the desired laxity value was not achieved to <1 mm of the desired value [0 mm and – 2 mm difference between knees (surgical – control) in the low-tension and high-tension groups, respectively], the fixation was released and the tensioning procedure repeated. A standardized rehabilitation program was followed post-operatively with a goal of return to full activity at 6 months.
2.3. Tunnel Measurements
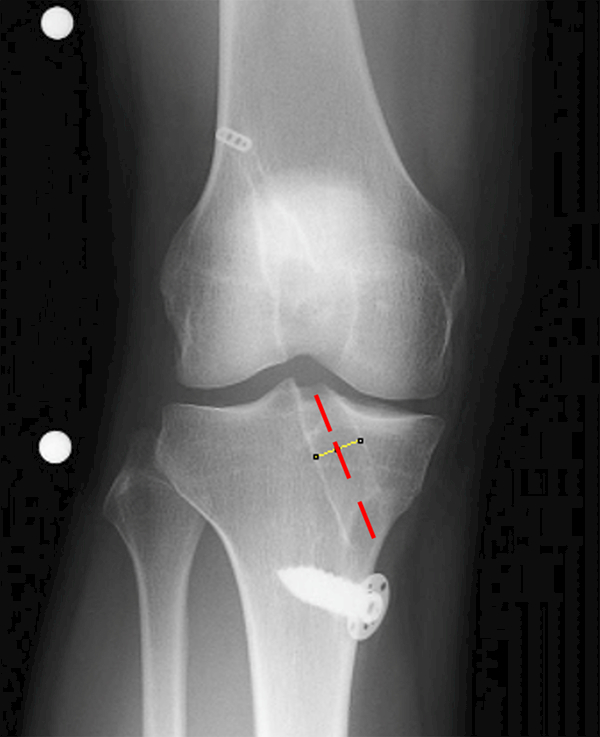
Baseline tibial tunnel diameters were obtained from the operative reports for each patient under the assumption that the initial tibial tunnel diameter was equal to the diameter of the reamer. Serial radiographs were obtained at the 1, 3, and 7-year follow-up visits. Anterior-posterior (AP) radiographs were reviewed and the maximum tunnel diameter along the length of the tibial tunnel was recorded perpendicular to the longitudinal axis of the tunnel (Figure 2). All radiographs where taken with two marker balls fixed 10 cm apart placed in the field of view. The marker-to-marker distance was measured and the ratio of that distance to 10 cm was used to determine the magnification factor for each image. Images were measured using imaging analysis software (ImageJ, U. S. National Institutes of Health, Bethesda, Maryland), and performed by a single observer (SFD) (Figure 2).
Figure 2.
Demonstration of sample image with marker balls to adjust for parallax and the location of the tunnel diameter measurement (yellow line). Longitudinal axis of tibial tunnel (dashed red line).
2.4. Patient Reported Outcomes
Patient reported outcomes, the Knee Osteoarthritis Outcome Score (KOOS)[28] and SF-36v2,[29] were evaluated between graft types and tension groups to determine if tunnel widening influenced them at 7-year follow-up. There are 5 domains associated with the KOOS: (1) quality of life (KOOS-QOL), (2) sports and recreation (KOOS-sport), (3) activities of daily living (KOOS-ADL), (4) symptoms (KOOS-symptoms), and (5) pain (KOOS-pain). The SF-36 is comprised of 8 domains evaluating health status related to physical functioning, role limitations, bodily pain, vitality, social functioning, emotional role, mental health, and general health.
2.5. Statistical Analyses
Pre-operative age, weight, and AP knee laxity were compared between the four groups (BTB High-tension, BTB Low-tension, HS High-tension, vs HS Low-tension) using two-way analyses of variance (ANOVA). Similarly, a nonparametric ANOVA was used to compare groups on days from injury to surgery, which was not normally distributed. Chi square tests were used to compare the proportion of males and females across groups. A three-way mixed model repeated measures analysis was used to compare mean tunnel widths between tension groups (High vs Low-tension), graft types (BTB vs HS), and across time (0, 1, 3 vs 7 years). A similar analysis was also performed on tunnel width change scores. The mean tunnel widths and associated 95% confidence intervals presented are least square means which adjust for incomplete follow-up. Lastly, the patient reported outcomes (KOOS and SF-36 scores) at 7 years were compared between groups using two-way ANOVA. All analyses were performed using SAS Statistical Software (SAS Institute, Cary, NC) with statistical significance based on α=.05.
3.0. Results
There were no significant differences in age, time between injury and surgery, or pre-operative AP knee laxity among the four treatment groups (Table 1). However, there were differences in the distributions of males and females among the four groups (p=.025) with a greater percentage of females in the HS autograft groups (74% vs 64%, p=.010). Additionally, the mean weight of the patients receiving HS autografts was significantly lower than those receiving BTB autografts (66±12Kg vs 75±16Kg, p=.049). The mean differences (±95% CI) for the intra-operative AP knee laxity values were −2.0±0.3mm, 0.0±0.4mm, −2.1±0.4mm, −0.2±0.8mm for the BTB High-tension, BTB Low-tension, HS High-tension and HS Low-tension groups, respectively, demonstrating that the target tension conditions were achieved.
Table 1.
Pre-operative variables between groups (means±SD). * indicates a significant difference (p<.05) between graft types (HS vs BTB) based on two-way ANOVA.
| Pre-op Demographic |
BTB Low | BTB High |
HS Low |
HS High |
|---|---|---|---|---|
| Age | 24±9.6 | 21±6.6 | 20±3.4 | 26±7.3 |
| Weight* | 76±17 | 72±15 | 63±7 | 68±15 |
| Sex* | 19M/8F | 12M/12F | 1M/6F | 4M/8F |
| Time to Surgery | 98±61 | 109±64 | 135±97 | 111±81 |
| KT-10001 | 4.4±2.0 | 4.3±2.6 | 5.2±1.5 | 4.1±3.3 |
Surgical – Contralateral control (mm)
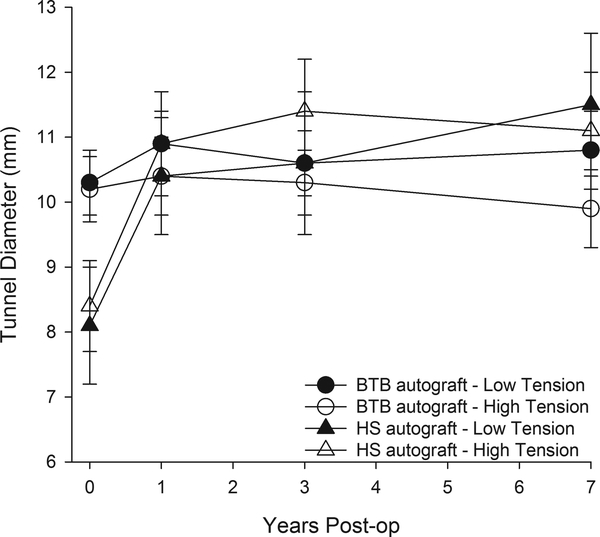
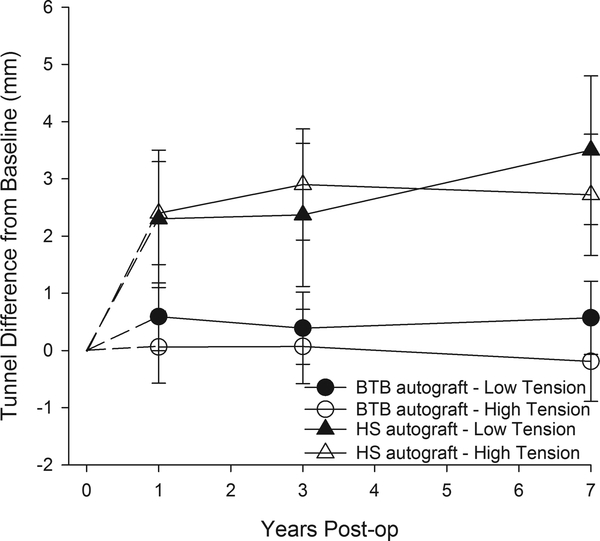
At the time of surgery, the mean (±95% CI) tunnel diameters for the BTB and HS autograft groups were 10.3±0.5mm (Low-tension), 10.2±0.6mm (High-tension), 8.1±0.9mm (Low-tension), and 8.4±0.7mm (High-tension), respectively. Mean tunnel diameters at surgery were significantly greater for BTB than the HS autografts (p<.001) while there were no differences between high- and low-tension groups (p=.85). Final mean (±95% CI) tunnel diameters for BTB autograft patients were 10.8±0.6mm (Low-tension) and 9.9±0.6mm (High-tension). While the final diameters of HS autograft patients were 11.5±1.1mm (Low-tension) and 11.1±0.9mm (High-tension). When temporal changes were examined post-surgery, there was a significant time by graft type interaction (p<.001) indicating that the changes in diameter over time were different between graft types (Figure 3). For subjects with HS autografts, mean tunnel diameters significantly changed over time (p <.001), while no significant changes were observed in subjects with BTB autografts (p=.29). Within the HS autograft group, tunnel diameters significantly increased in the first year (p<.001) with relative increases of 28% and 30% for the low-tension and high-tension groups, respectively. After the first year, subjects with HS autografts showed a small (~6%) but significant increase (p=.029). The change in diameter of the HS autograft groups remained significantly greater than that of the BTB group at all time points for both tension groups (p<.05; Figure 4). There was no evidence that differences in temporal changes between graft types were dependent on tension group (time x graft type x tension group, p=.77), nor was there evidence of a time by tension group interaction (p=.32).
Figure 3.
Mean tibial tunnel diameters versus time between graft type and initial graft tension groups. BTB – bone patellar tendon bone. The error bars represent the 95% confidence intervals.
Figure 4.
Mean changes in tunnel widening relative to time of surgery (0). The error bars represent the 95% confidence intervals.
At 7-year follow-up, there were no significant differences between graft types (p>.16), tension groups (p>.18) or evidence of interactions (p>.56) in patient reported outcomes (Table 2).
Table 2.
Patient reported outcomes at 7-year follow-up (means±95% confidence intervals). No significant differences were detected.
| Outcome | BTB Low | BTB High | HS Low |
HS High |
|---|---|---|---|---|
| KOOS pain | 89±9 | 90±10 | 96±3 | 98±2 |
| KOOS ADL | 94±5 | 95±6 | 89±2 | 99±1 |
| KOOS QOL | 77±11 | 83±11 | 76±11 | 76±20 |
| KOOS S/R | 78±9 | 87±9 | 84±14 | 91±11 |
| KOOS Sym | 81±7 | 83±8 | 82±17 | 89±9 |
| SF-36 BP | 80±6 | 83±9 | 83±10 | 90±6 |
| SF-36 GH | 79±7 | 85±8 | 86±10 | 87±8 |
| SF-36 MH | 83±6 | 86±7 | 79±17 | 86±6 |
| SF-36 PF | 93±5 | 94±5 | 94±6 | 97±5 |
| SF-36 RE | 96±4 | 94±87 | 96±7 | 96±8 |
| SF-36 RP | 95±5 | 96±6 | 96±7 | 100±0 |
| SF-36 SF | 95±4 | 96±6 | 94±11 | 99±3 |
| SF-36 V | 71±8 | 74±8 | 69±17 | 72±11 |
4.0. Discussion
The most important finding of this study is that tunnel widening was dictated by graft type but not the initial graft tension applied at the time of fixation. Patients who underwent ACL reconstruction with HS autograft had significantly more tunnel widening than those with BTB autograft regardless of the initial graft tension condition. These results provide evidence to support our hypothesis relating to graft selection, but disproved our hypothesis that high-tension grafts would have greater tunnel widening than the low-tension grafts within either graft type. We also found that the patient reported outcomes were not significantly different between graft types or tension groups at 7 years.
We found that in patients with HS autografts, significant tunnel widening occurs in the first postoperative year with a small but statistically significant increase continuing out to 7 years. With regards to BTB autografts there was no significant tunnel widening at any time point. Weber et al previously evaluated tunnel widening in 18 patients (14 BTB autograft, 3 HS autograft, 1 Achilles allograft). Patients exhibited widening for the initial 24 weeks of the study, with subsequent tunnel contraction for the remainder of the two-year follow-up.[14] The aforementioned study did not find a difference in tunnel widening between graft types, however it was likely underpowered to do so.[14] This study is also in contrast to our study with regards to how long tunnel widening was observed. The aforementioned study did not observe any widening after 24 weeks, while we observed a small but statistically significant widening from 1 to 7 years with HS autograft. No tunnel contraction was seen in our study.
HS showed significant change in tunnel diameter that was time dependent when compared to the initial tunnel diameter, regardless of initial tension. BTB autografts however, did not exhibit tunnel widening at any time point. Clatworthy et al reported similar results in a study comparing tunnel widening between BTB and HS autografts.[23] Tibial tunnel diameters in patients with HS autografts increased an average of 73.9% at 12 months, compared to a decrease of 2.1% in BTB.[23] In our study, patients with HS in low-tension experienced an increase in tunnel width of 28% at 12 months, while the high-tension group experienced an increase of 30% at 12 months. In both the aforementioned study as well as in our study, this increase in tunnel widening did not correlate with any difference in functional outcomes.[23,26,27] More importantly, both the study by Clatworthy et al as well as our own showed a significant increase in tibial tunnel widening within 12 months of surgery. Also, our study continued to show significant widening for up to 7 years postoperatively in the HS autograft group.
Graft-tunnel motion is a theorized cause of tunnel widening for both BTB and HS reconstruction. Because BTB grafts are typically fixed flush against the intra-articular side of the femur, graft-tunnel motion is greater at the tibial tunnel-graft interface.[16] Specifically for BTB grafts, the bone plug is often located in the distal part of the tunnel, causing dead space where the graft plugs into the tibial footprint, due to the diameter of the tendinous portion of the graft being smaller than the bone block.[30] L’Insalata et al termed this motion in the transverse plane “the windshield wiper effect”, and reported a greater increase in tibial tunnel size compared to femoral tunnel size in BTB autografts due to the translational movement of the tendon within the tibial tunnel compared to the femoral side.[31] HS autografts are also subject to this type of motion. The authors reported greater tibial tunnel widening in HS compared to BTB patients, due to the increased distance of graft fixation from the anatomic ACL insertion. This creates a larger moment arm for HS compared to BTB autografts, allowing for more motion during within the tunnel during cyclic loading.[31] HS autografts are also subject to longitudinal displacement within the tibial tunnel via the “bungee effect”.[18] While this phenomenon is not specific to HS grafts, it is primarily associated with soft tissue grafts with longer tibial tunnel lengths.[16,18] Because BTB grafts are typically rigidly fixed with interference screws and bone plugs, these grafts are less susceptible to this type of graft-tunnel motion.[18] However, the results of the current study suggest that the phenomenon of tunnel widening is only relevant to the HS autografts for the initial tension conditions evaluated in the current study.
Other studies have shown that tunnel expansion may be associated with increases in ACL graft tensioning.[20]. This led us to hypothesize that increased graft tensioning would result in greater tibial tunnel widening. This was proven to be unlikely in our study as we found that initial graft tension did not affect tunnel widening within both graft types. This is in contrast to the study by Taketomi et al which examined the effect of tensioning on femoral tunnel widening following BTB ACL-R.[20] In their study, 18 patients were reconstructed with maximal tension (a high-tension condition) while 25 patients were fixed with 80 N of tension (a low-tension condition). When measured at one year, the tunnel sizes of the high-tension group had a 78.6% increase compared to a 27.7% increase in the low-tension group. Of note there was no differences in clinical outcomes between the two groups.[20] The tension conditions evaluated in our study were different as the grafts were tensioned to restore AP laxity or to constrain AP laxity relative to the uninjured knee. Thus, these two tension conditions span the range of conditions that would be acceptable in the OR as it is unlikely that surgeons would set laxity more lax than the contralateral knee or to over-constrain the knee by more than 2 mm. While our study did not show a difference in tunnel widening between these two high and low tension groups, the Taketomi study also focused on the femoral tunnel compared to the tibial tunnel of our study.[20]
When examining clinical outcomes, Jarvela et al found a significant correlation between anterior and rotational laxity and tunnel widening.[32] Additionally, our prior long-term follow-up study using the same patient cohort examined here found that the amount of initial tension of the graft has a significant effect on patient reported outcome, specifically the KOOS “sports and recreation” subscale at 84 months follow-up.[26] However, when patients meeting the criteria for the present study were extracted from this larger cohort, no differences in patient reported outcomes via KOOS were seen at 7 years. The findings of this study, and the potential functional improvements in high tension patients in a prior study,[26] we conclude that in order to optimize outcomes while minimizing tibial tunnel expansion (from least to most) surgeons should use the following: BTB with high-tension, BTB with low-tension, hamstring with high-tension, hamstring with low-tension. However, due to inconclusive evidence with regards to improved clinical outcomes as a result of decreased tunnel widening over time in our study, we cannot recommend that BTB autograft be used in all clinical scenarios. The authors acknowledge that BTB can be technically demanding and should only be performed by surgeons who are comfortable with this technique.
4.1. Limitations
There were several limitations to our study. First, graft choice was not randomized and was at the discretion of the surgeon and/or patient, which could introduce selection bias.[9–11] There were differences in the proportions of males and females who received BTB versus HS graft. Second, the loss to follow-up could introduce transfer bias. For this analysis, we acquired 7-year radiographic follow up for 64.3% of the 70 eligible patients. Also, several patients were only able to complete PRO questionnaires via mail, as they were unable to present for radiographs at certain time points. Several of these patients re-entered the study by presenting for radiographs at a later date (N=2 re-presentations at year 3, and N=7 at year 7). Patients with inadequate x-rays were those who did not have marker balls placed at the time of imaging, thus no standardized measurement of the tunnel could be made. Third, with regards to tunnel expansion, either the tibia or femur could be implicated. However, Weber et al examined tunnel widening over a two year period and found that tibial tunnel was impacted more than the femoral tunnel[14]. Thus, we focused on tibial tunnel widening in our study.
Another limitation is that we assumed that the initial tibial tunnel size was equal to that of the reamer used to drill the tunnels. It is likely that the tunnel was slightly larger than that of the drill diameter. Given the magnitude of the increases seen for the HS autografts measured, the impact of this assumption would be relatively minor. This assumption has been widely accepted within the literature.[10,13,15,16,18,19,23,32,33] Additionally, we used plain radiographs to assess changes in tunnel diameter, while other studies have used MRI and CT imaging to obtain 3-D models of the tunnel.[14] However, tunnel measurements from plain radiographs have been shown to correlate well with those obtained from CT and MRI.[34,35] In our study, only AP radiographs were available for all patients, leading to this view being used for analysis. It is possible that differences would have been greater in the sagittal plane possibly due to the windshield wiper effect. In attempt to minimize any error associated with measuring tunnel widths on the radiographs, all measurements were made by one researcher (SFD). Lastly, the effect of tunnel position on tunnel widening was not considered in this study. This is a potential source of inherent bias as 3 different surgeons performed the surgeries. To minimize any bias, the same drill guide system and anatomical landmarks were used by the surgeons. Ultimately, research is required to determine the causes of tibial tunnel widening and its effect on clinical and functional outcomes.
5.0. Conclusion
Patients who underwent ACL-R with HS autograft experienced significant tunnel widening over the first year from surgery when placed in either low- and high-initial graft tension. A small but statistically significant widening persisted out to 7 years in the HS patients. In contrast, patients with BTB grafts did not experience any significant widening at any time point, regardless of initial graft tension. Additionally, we did not demonstrate any significant differences in patient reported outcomes in either group, despite tunnel widening.
Acknowledgements
The authors have no relevant financial disclosures or conflicts to report that are directly related to the study. Dr. Owens is a consultant for Mitek and MTF/CONMED. Dr. Fleming is a cofounder of Miach Orthopaedics, LLC, a consultant for New York R&D Center for Translational Medicine and Therapeutics, Inc, has received travel support to attend a workshop by Smith & Nephew, and is an associate editor for the American Journal of Sports Medicine. Dr. Hulstyn has received hospitality payment from Arthrex. Dr. Bokshan has received educational support from Stryker.
The research reported in this publication was supported by the National Institute of Health (2R01-AR047910 & 2P20 GM104937), the Lucy Lippitt Endowment, and the RIH Orthopaedic Foundation. The contents of this article are solely the responsibility of the authors and do not necessarily represent the official views of the National Institutes of Health.
References
- [1].Rodeo SA, Kawamura S, Kim H-J, Dynybil C, Ying L. Tendon Healing in a Bone Tunnel Differs at the Tunnel Entrance versus the Tunnel Exit. Am J Sports Med 2006;34:1790–800. doi:10.1177/0363546506290059. [DOI] [PubMed] [Google Scholar]
- [2].Makhni EC, Crump EK, Steinhaus ME, Verma NN, Ahmad CS, Cole BJ, et al. Quality and Variability of Online Available Physical Therapy Protocols From Academic Orthopaedic Surgery Programs for Anterior Cruciate Ligament Reconstruction. Arthrosc J Arthrosc Relat Surg 2016;32:1612–21. doi:10.1016/j.arthro.2016.01.033. [DOI] [PubMed] [Google Scholar]
- [3].Albright JC, Crepeau AE. Functional Bracing and Return to Play After Anterior Cruciate Ligament Reconstruction in the Pediatric and Adolescent Patient. Clin Sports Med 2011;30:811–5. doi:10.1016/j.csm.2011.06.001. [DOI] [PubMed] [Google Scholar]
- [4].Alshewaier S, Yeowell G, Fatoye F. The effectiveness of pre-operative exercise physiotherapy rehabilitation on the outcomes of treatment following anterior cruciate ligament injury: a systematic review. Clin Rehabil 2017;31:34–44. doi:10.1177/0269215516628617. [DOI] [PubMed] [Google Scholar]
- [5].Failla MJ, Logerstedt DS, Grindem H, Axe MJ, Risberg MA, Engebretsen L, et al. Does Extended Preoperative Rehabilitation Influence Outcomes 2 Years After ACL Reconstruction?: A Comparative Effectiveness Study Between the MOON and Delaware-Oslo ACL Cohorts. Am J Sports Med 2016;44:2608–14. doi:10.1177/0363546516652594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Moksnes H, Engebretsen L, Eitzen I, Risberg MA. Functional outcomes following a non-operative treatment algorithm for anterior cruciate ligament injuries in skeletally immature children 12 years and younger. A prospective cohort with 2 years follow-up. Br J Sports Med 2013;47:488–94. doi:10.1136/bjsports-2012-092066. [DOI] [PubMed] [Google Scholar]
- [7].van Grinsven S, van Cingel REH, Holla CJM, van Loon CJM. Evidence-based rehabilitation following anterior cruciate ligament reconstruction. Knee Surgery, Sport Traumatol Arthrosc 2010;18:1128–44. doi:10.1007/s00167-009-1027-2. [DOI] [PubMed] [Google Scholar]
- [8].DeFroda SF, Hiller K, Cruz AI. Pediatric Anterior Cruciate Ligament Rehabilitation: A Review. R I Med J (2013) 2017;100:26–30. [PubMed] [Google Scholar]
- [9].Robinson J, Huber C, Jaraj P, Colombet P, Allard M, Meyer P. Reduced bone tunnel enlargement post hamstring ACL reconstruction with poly-l-lactic acid/hydroxyapatite bioabsorbable screws. Knee 2006;13:127–31. doi:10.1016/j.knee.2005.09.002. [DOI] [PubMed] [Google Scholar]
- [10].Lind M, Feller J, Webster KE. Tibial bone tunnel widening is reduced by polylactate/hydroxyapatite interference screws compared to metal screws after ACL reconstruction with hamstring grafts. Knee 2009;16:447–51. doi:10.1016/j.knee.2009.04.003. [DOI] [PubMed] [Google Scholar]
- [11].Lind M, Feller J, Webster KE. Bone Tunnel Widening After Anterior Cruciate Ligament Reconstruction Using EndoButton or EndoButton Continuous Loop. Arthrosc J Arthrosc Relat Surg 2009;25:1275–80. doi:10.1016/j.arthro.2009.06.003. [DOI] [PubMed] [Google Scholar]
- [12].Sabat D, Kundu K, Arora S, Kumar V. Tunnel Widening After Anterior Cruciate Ligament Reconstruction: A Prospective Randomized Computed Tomography–Based Study Comparing 2 Different Femoral Fixation Methods for Hamstring Graft. Arthrosc J Arthrosc Relat Surg 2011;27:776–83. doi:10.1016/j.arthro.2011.02.009. [DOI] [PubMed] [Google Scholar]
- [13].Aga C, Wilson KJ, Johansen S, Dornan G, La Prade RF, Engebretsen L. Tunnel widening in single- versus double-bundle anterior cruciate ligament reconstructed knees. Knee Surgery, Sport Traumatol Arthrosc 2017;25:1316–27. doi:10.1007/s00167-016-4204-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Weber AE, Delos D, Oltean HN, Vadasdi K, Cavanaugh J, Potter HG, et al. Tibial and Femoral Tunnel Changes After ACL Reconstruction. Am J Sports Med 2015;43:1147–56. doi:10.1177/0363546515570461. [DOI] [PubMed] [Google Scholar]
- [15].Baumfeld JA, Diduch DR, Rubino LJ, Hart JA, Miller MD, Barr MS, et al. Tunnel widening following anterior cruciate ligament reconstruction using hamstring autograft: a comparison between double cross-pin and suspensory graft fixation. Knee Surg Sports Traumatol Arthrosc 2008;16:1108–13. doi:10.1007/s00167-008-0606-y. [DOI] [PubMed] [Google Scholar]
- [16].Höher J, Möller HD, Fu FH. Bone tunnel enlargement after anterior cruciate ligament reconstruction: fact or fiction? Knee Surgery, Sport Traumatol Arthrosc 1998;6:231–40. doi:10.1007/s001670050105. [DOI] [PubMed] [Google Scholar]
- [17].Amiel D, Kleiner JB, Akeson WH. The natural history of the anterior cruciate ligament autograft of patellar tendon origin. Am J Sports Med 1986;14:449–62. doi:10.1177/036354658601400603. [DOI] [PubMed] [Google Scholar]
- [18].Höher J, Livesay GA, Ma CB, Withrow JD, Fu FH, Woo SL. Hamstring graft motion in the femoral bone tunnel when using titanium button/polyester tape fixation. Knee Surg Sports Traumatol Arthrosc 1999;7:215–9. doi:10.1007/s001670050151. [DOI] [PubMed] [Google Scholar]
- [19].Hantes ME, Mastrokalos DS, Yu J, Paessler HH. The effect of early motion on tibial tunnel widening after anterior cruciate ligament replacement using hamstring tendon grafts. Arthroscopy 2004;20:572–80. [DOI] [PubMed] [Google Scholar]
- [20].Taketomi S, Inui H, Tahara K, Shirakawa N, Tanaka S, Nakagawa T. Effects of initial graft tension on femoral tunnel widening after anatomic anterior cruciate ligament reconstruction using a bone–patellar tendon–bone graft. Arch Orthop Trauma Surg 2017;137:1285–91. doi:10.1007/s00402-017-2728-5. [DOI] [PubMed] [Google Scholar]
- [21].Wang JH, Lee ES, Lee BH. Paradoxical tunnel enlargement after ACL reconstruction with hamstring autografts when using β-TCP containing interference screws for tibial aperture fixation- prospectively comparative study. BMC Musculoskelet Disord 2017;18:398. doi:10.1186/s12891-017-1757-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Hwang D-H, Shetty GM, Kim JI, Kwon JH, Song J-K, Muñoz M, et al. Does press-fit technique reduce tunnel volume enlargement after anterior cruciate ligament reconstruction with autologous hamstring tendons? A prospective randomized computed tomography study. Arthroscopy 2013;29:83–8. doi:10.1016/j.arthro.2012.07.007. [DOI] [PubMed] [Google Scholar]
- [23].Clatworthy MG, Annear P, Bulow J-U, Bartlett RJ. Tunnel widening in anterior cruciate ligament reconstruction: a prospective evaluation of hamstring and patella tendon grafts. Knee Surgery, Sport Traumatol Arthrosc 1999;7:138–45. doi:10.1007/s001670050138. [DOI] [PubMed] [Google Scholar]
- [24].Choi N-H, Oh J-S, Jung S-H, Victoroff BN. Correlation between endobutton loop length and tunnel widening after hamstring anterior cruciate ligament reconstruction. Am J Sports Med 2013;41:101–6. doi:10.1177/0363546512466384. [DOI] [PubMed] [Google Scholar]
- [25].Struewer J, Efe T, Frangen TM, Schwarting T, Buecking B, Ruchholtz S, et al. Prevalence and influence of tibial tunnel widening after isolated anterior cruciate ligament reconstruction using patella-bone-tendon-bone-graft: long-term follow-up. Orthop Rev (Pavia) 2012;4:e21. doi:10.4081/or.2012.e21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Akelman MR, Fadale PD, Hulstyn MJ, Shalvoy RM, Garcia A, Chin KE, et al. Effect of Matching or Overconstraining Knee Laxity During Anterior Cruciate Ligament Reconstruction on Knee Osteoarthritis and Clinical Outcomes. Am J Sports Med 2016;44:1660–70. doi:10.1177/0363546516638387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Fleming BC, Fadale PD, Hulstyn MJ, Shalvoy RM, Oksendahl HL, Badger GJ, et al. The Effect of Initial Graft Tension After Anterior Cruciate Ligament Reconstruction. Am J Sports Med 2013;41:25–34. doi:10.1177/0363546512464200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Roos EM, Roos HP, Lohmander LS, Ekdahl C, Beynnon BD. Knee Injury and Osteoarthritis Outcome Score (KOOS)—Development of a Self-Administered Outcome Measure. J Orthop Sport Phys Ther 1998;28:88–96. doi:10.2519/jospt.1998.28.2.88. [DOI] [PubMed] [Google Scholar]
- [29].Ware JE, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care 1992;30:473–83. [PubMed] [Google Scholar]
- [30].Kurzweil PR. The “N + 7 rule” for tibial tunnel placement in endoscopic anterior cruciate ligament reconstruction. Arthroscopy 1996;12:392–4. [DOI] [PubMed] [Google Scholar]
- [31].L’Insalata JC, Klatt B, Fu FH, Harner CD. Tunnel expansion following anterior cruciate ligament reconstruction: a comparison of hamstring and patellar tendon autografts. Knee Surg Sports Traumatol Arthrosc 1997;5:234–8. doi:10.1007/s001670050056. [DOI] [PubMed] [Google Scholar]
- [32].Järvelä T, Moisala A-S, Paakkala T, Paakkala A. Tunnel Enlargement After Double-Bundle Anterior Cruciate Ligament Reconstruction: A Prospective, Randomized Study. Arthrosc J Arthrosc Relat Surg 2008;24:1349–57. doi:10.1016/j.arthro.2008.07.018. [DOI] [PubMed] [Google Scholar]
- [33].Fink C, Zapp M, Benedetto KP, Hackl W, Hoser C, Rieger M. Tibial tunnel enlargement following anterior cruciate ligament reconstruction with patellar tendon autograft. Arthrosc J Arthrosc Relat Surg 2001;17:138–43. doi:10.1053/jars.2001.21509. [DOI] [PubMed] [Google Scholar]
- [34].Webster KE, Feller JA, Elliott J, Hutchison A, Payne R. A comparison of bone tunnel measurements made using computed tomography and digital plain radiography after anterior cruciate ligament reconstruction. Arthrosc J Arthrosc Relat Surg 2004;20:946–50. doi:10.1016/j.arthro.2004.06.037. [DOI] [PubMed] [Google Scholar]
- [35].Jansson KA, Harilainen A, Sandelin J, Karjalainen PT, Aronen HJ, Tallroth K. Bone tunnel enlargement after anterior cruciate ligament reconstruction with the hamstring autograft and endobutton fixation technique. A clinical, radiographic and magnetic resonance imaging study with 2 years follow-up. Knee Surg Sports Traumatol Arthrosc 1999;7:290–5. doi:10.1007/s001670050166. [DOI] [PubMed] [Google Scholar]