Abstract
Introduction
Racial disparities in cancer treatment contribute to racial disparities in mortality rates. The quality of patient–physician communication during clinical interactions with black patients and non-black physicians (racially discordant) is poorer than communication quality with white patients (racially concordant). Patient and physician race-related attitudes affect the quality of this communication. These attitudes are likely expressed through subtle non-verbal behaviours, but prior research has not examined these behaviours. Nonverbal synchrony, the coordination of physical movement, reflects the preinteraction attitudes of participants in interactions and predicts their postinteraction perceptions of and affect towards one another. In this study, peer reviewed and funded by the National Institute of Minority Health and Health Disparities (R21MD011766), we will investigate non-verbal synchrony in racially concordant and discordant interactions to better understand racial disparities in clinical communication.
Methods and analysis
This secondary analysis includes racially concordant (n=163) and racially discordant (n=68) video-recorded oncology interactions, patient and oncologist self-reported race-related attitudes, perceptions of the interaction and observer ratings of physician patient-centred communication and patient and physician affect and rapport. In aim 1, we will assess and compare non-verbal synchrony between physicians and patients in racially concordant and discordant interactions. In aim 2, we will determine the influence of non-verbal synchrony on patient and physician affect and communication. In aim 3, we will examine possible causes (ie, race-related attitudes) and consequences (ie, negative perceptions) of non-verbal synchrony in racially discordant interactions. In aim 4, we will develop and test a mediational model linking physician and patient race-related attitudes to non-verbal synchrony and, in turn, interaction outcomes.
Ethics and dissemination
The parent and current studies were approved by the Wayne State University Institutional Review Board. Since only archival data will be used, ethical or safety risks are low. We will disseminate our findings to relevant conferences and journals.
Keywords: disparities, cancer, racial discordance, nonverbal synchrony, race-related attitudes
Strengths and limitations of this study.
This study explores non-verbal synchrony, a channel of communication that has not been previously examined in medical interactions.
This study uses video-recorded cancer treatment discussions of black and white patients with cancer, recorded with state-of-art recording equipment.
This study uses automated behavioural coding software, which introduces less error than traditional methods using human coders.
This study takes advantage of existing datasets, but the video-recorded and self-report data were not collected with the current hypotheses in mind.
The data are not evenly distributed by sex and race.
Introduction
Racial disparities in cancer mortality and treatment are well documented. In the USA, deaths due to cancer are approximately 20% higher for black patients than for white patients.1 This mortality disparity remains even after controlling for stage at diagnosis, disease aggressiveness, obesity, comorbidities, physician access, insurance status and referrals.2–6 Importantly, this disparity is greatest for the most treatable cancers.7 This strongly suggests treatment disparities may contribute to mortality disparities.8–14 For example, black patients with cancer are less likely to receive chemotherapy for leukaemia, breast, lung and colorectal cancers. If they do receive treatment, it is more likely to be delayed or not adherent to the treatment guidelines set by the National Comprehensive Cancer Network.2 8 15–23 Multiple causes of these treatment disparities exist including tumour biology, socioeconomic status, environment and access to care.6 However, research clearly shows that even when these factors are controlled, racial disparities in treatment remain. We focus on two other contributors to racial disparities in cancer treatments: (1) poor patient–physician communication during oncology interactions24–30 and (2) race-related attitudes and perceptions of physicians and patients.31–42 We are investigating these factors because they account for unique variance in racial treatment disparities.
Black patients experience poorer quality communication during oncology interactions compared with similar interactions with white patients. Due to the small number of black physicians, especially black oncologists,43 about 80% of black patients’ clinical interactions are racially discordant (black patients, non-black physicians).44 Patient–physician communication is often of poorer quality in racially discordant clinical interactions than racially concordant ones. Patients in racially discordant interactions tend to ask fewer questions25 and are less likely to participate in decision-making45; whereas physicians tend to be less patient centred,46 47 more verbally dominant,47 more contentious,48 exhibit fewer rapport building non-verbal behaviours49 and provide less information.27 Physicians and patients show fewer expressions of positive affect47 and relationship-building attempts.29
Patient and physician race-related attitudes and perceptions affect interaction outcomes via communication behaviours. Prior research, including our own, suggests that race-related attitudes and perceptions (eg, physician implicit bias against black people, patient suspicion of medical care black people receive) affect communication in clinical interactions and perceptions physicians and patients have of each other during racially discordant clinical interactions.31–33 37 38 For example, physicians with higher levels of implicit (unconscious) bias against black people are perceived as less patient centred and less trustworthy by their black patients than physicians with lower levels of implicit bias against black people.31 40 41 50 Our prior research suggests such perceptions and behaviours are associated with less positive patient expectations about recommended treatments.51 We have also found that black patients with higher levels of suspicion of medical care are less optimistic about outcomes of recommended treatments and are perceived by their physicians to be less educated.52 This, in turn, is associated with less positive physician expectations about how their black patients will do on a treatment protocol, such as their adherence and/or ability to tolerate treatment. Given that these attitudes and perceptions are not directly observable, the only possible way in which they can affect perceptions and expectations is through their influence on communication behaviours.
Relatively little is known about how race-related attitudes and perceptions are manifested in communication behaviours during oncology interactions or the effects of communication on interaction outcomes. Our own and others’ research has shown that non-black physicians’ unconscious race-related attitudes (ie, implicit racial bias) influence their communication with black patients.51 53 54 Studies of non-medical interracial interactions find that implicit bias is more likely to be expressed through less deliberate non-verbal communication (eg, facial expressions, posture) than through more deliberate verbal communication (eg, spoken words).55–58 Black patients’ communication may be driven more by explicit than implicit race-related attitudes and perceptions,59 but its expression may also be subtle and involve less deliberate communication (eg, non-verbal behaviours).54 The behavioural channels through which these race-related attitudes and perceptions are expressed are not known, but non-verbal synchrony is a promising candidate as one of them.
Non-verbal synchrony is the coordination of physical movement that occurs between two individuals during an interaction.60 The construct of synchrony was first introduced more than 50 years ago and has sparked many related areas of study.61 Here, we consider non-verbal synchrony as a dynamic and jointly determined phenomenon, not focused on any particular behaviour (eg, posture, eye contact). Rather, we consider non-verbal synchrony as a form of behavioural matching between two individuals. This matching does not have to occur at the same time (as it would for two people dancing), but it must involve similar kinds of motion and exhibit some sort of coordinated back and forth between individuals.62–64 As an example, an individual shaking his or her head while another individual waves his or her hand would exhibit non-verbal synchrony but they are not mirroring one another nor are they perfectly in time.63
Considerable prior laboratory-based research shows that non-verbal synchrony is often unconscious, unintentional and effortless.65–67 However, non-verbal synchrony can be predicted by preinteraction attitudes68 and has postinteraction consequences.69 People synchronise more with others with whom they have positive relationships,70 those with whom they want to develop positive relationships71 and others whom they trust.68 In a recent experimental laboratory-based study, individuals with higher implicit bias favouring their own race synchronised more with an avatar of their own race than with an avatar of a different race.72 In terms of non-verbal synchrony’s role as a predictor, non-verbal synchrony reflects more subsequent positive affect and liking,69 perceptions of similarity, closeness, rapport with the interaction partner and collaborative problem solving.68 73–75 More relevant to clinical communication, non-verbal synchrony has been found to positively influence therapeutic processes,76 cooperation,77 obedience74 and memory for information provided by the interaction partner.78 79 It is because of this previous research that we will investigate general non-verbal synchrony in this study, rather than, for example, vocal synchrony or synchrony of more precise behaviours such as eye gaze.
To summarise, current evidence indicates that black patients and non-black physicians have negative reactions to each other’s race-related attitudes and perceptions. Also, evidence indicates that these attitudes and perceptions are subtly manifested in communication. Little is known, however, about the channels through which these attitudes and perceptions are communicated. Because non-verbal synchrony is subtle, unintentional, automatic and affect-laden, it may likely serve as a behavioural marker of race-related attitudes and perceptions. Here, we describe the protocol for a study that will help fill this gap in understanding by examining the role of non-verbal synchrony in racially concordant and racially discordant oncology interactions.
The study was designed to achieve the following aims and hypotheses, which are based on the research reviewed:
Aim 1: Assess and compare non-verbal synchrony between physicians and patients in racially concordant and racially discordant oncology interactions.
Hypothesis 1: Non-verbal synchrony will be greater in racially concordant than in racially discordant oncology interactions.
Aim 2: Determine the influence of non-verbal synchrony on physician communication (eg, level of patient-centredness) and patient and physician affect in racially concordant and racially discordant oncology interactions.
Hypothesis 2: Non-verbal synchrony will positively influence physician patient-centred communication, patient and physician affect, and relational rapport in racially concordant and racially discordant clinical interactions.
Aim 3: Examine the antecedents and outcomes of non-verbal synchrony in racially discordant oncology interactions.
Hypothesis 3: In racially discordant oncology interactions, non-verbal synchrony will significantly negatively covary with patient postinteraction distress and positively covary with (1) patient postinteraction perceptions of physicians’ patient-centred communication and treatment expectations; (2) physicians’ postinteraction perceptions of patient personal characteristics (eg, understanding of treatment options) and their responses to treatment (eg, willingness to follow treatment regimen) and (3) observers’ ratings of physician patient-centred communication, patient and physician affect, and relational rapport.
Hypothesis 4: Non-verbal synchrony will significantly covary with preinteraction race-related attitudes and perceptions of the patient and physicians (eg, physician implicit bias; patient suspicion).
Aim 4: Develop and test a mediational model that links physician and patient race-related attitudes and perceptions to non-verbal synchrony and, in turn, outcomes of racially discordant oncology interactions.
Hypothesis 5: Non-verbal synchrony will mediate the relationship between preinteraction race-related attitudes and perceptions and postinteraction perceptions of the patients and physicians.
Methods and analysis
Overview of proposed study
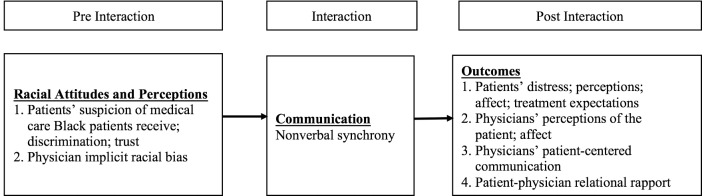
Our goals are to: (1) compare the extent to which physicians and patients synchronise their behaviour in racially concordant and racially discordant oncology interactions; (2) compare the associations between non-verbal synchrony and self-report and observational measures of patient and physician affect and physicians’ patient-centred communication in racially concordant and racially discordant oncology interactions; (3) investigate how race-related attitudes and perceptions (eg, physician implicit bias, patient suspicion) affect non-verbal synchrony in racially discordant oncology interactions; (4) investigate how non-verbal synchrony affects the outcomes of racially discordant clinical interactions and (5) test the conceptual model in figure 1, which predicts that race-related attitudes and perceptions will be associated with patient and physician perceptions and treatment-related outcomes of racially discordant oncology interactions, through their influence on non-verbal synchrony. To achieve these goals, we will conduct a secondary analysis of data from two studies conducted by members of our study team. This secondary analysis was officially funded in September 2017. Thus, it is ongoing and will be completed by August 2019. Study 1, which was funded by the National Cancer Institute (NCI), was conducted at two NCI-designated comprehensive cancer centres between April 2002 and March 2006 (R01CA75003),80 was an investigation of how patient–oncologist communication influences patients’ decision-making about treatment including clinical trials. Study 2 (also funded by the NCI) was conducted at one of the study 1 NCI-designated centres plus another large urban cancer clinic in the same city between April 2012 and December 2014. Study 2 investigated associations between communication and outcomes during racially discordant oncology interactions (U54CA153606-04).81 Only patients and oncologists from these studies who agreed on their consent forms to allow their video-recorded and self-reported data to be used in secondary analyses will be used in the current study. Comparisons of groups did not find any sociodemographic or attitudinal differences between patients/oncologists who did and did not agree to be in secondary analyses.
Figure 1.
Conceptual model.
Data sources
Participants, procedures and measures in study 1
Patients from study 1 who are in the current study include 163 self-identified White (92 male; 71 female) patients who were meeting with a white medical oncologist for the first time to discuss treatment for their cancer. On consent, which occurred immediately prior to meeting their oncologist, patients completed a survey assessing their sociodemographic characteristics. Oncologists were 22 white male medical oncologists (no female oncologists participated in study 1) who saw at least one participating patient (M=7.4, SD=7.0). On consent, oncologists completed a demographic survey. Examination rooms were equipped with unobtrusive digital audio and video recording devices. Studies have demonstrated the non-reactance to the recording process,82 and enhanced validity compared with audio recording alone.83
Participants, procedures and measures in study 2
Patients from study 2 who are in the current study include 68 black female patients who were meeting with a non-black medical oncologist for the time to discuss treatment for their cancer. While patients were recruited for study Two irrespective of sex, only six of the patients who enrolled were males. A meaningful statistical comparison on the variables of interest by patient sex cannot be conducted with so few male participants. Thus, we are excluding them from further analyses. On consent, patients provided sociodemographic information and completed measures of suspicion of medical care black patients receive34 and trust in medical institutions.84 There were 16 medical oncologists (7 females; 9 males; 8 white; 6 Asian/Pacific Islander; 2 Arab/Middle Eastern) who saw at least one participating patient (M=5.2, SD=6.4). On consent, oncologists completed a demographic survey and the implicit association test, which assesses implicit racial bias against black people.85 Just as in study 1, examination rooms in study 2 were equipped with unobtrusive digital audio and video recording devices.
In study 2, oncologists were consented on enrolment, and the video-recorded clinical interactions took place within 2 weeks after patients consented. Immediately after the interactions, patients completed measures of distress,86 perception of the physicians’ patient-centred communication87 and expectations about recommended treatment. Also, immediately after interactions, oncologists completed measures of perceptions of the patient and how well the patient would do in treatment. One week later, patients reported their level of trust in their oncologist84 in a telephone survey. Trained observers later observed and rated video-recorded interactions to assess physicians’ patient-centred communication.48 To do this, coders applied a global scale of physicians’ patient-centred communication which assessed physicians’ informativeness (eg, ‘the doctor thoroughly explained everything to the patient’); supportiveness (eg, ‘the doctor made the patient feel completely at ease during the consultation’) and partnership building (eg, ‘the doctor encouraged the patient to express concerns and worries’).48 At least two observers rated physicians’ patient-centred communication (three observers rated 15% of interactions to ensure continued reliability); inter-rater reliability was acceptable (intraclass correlation coefficient=0.57–0.74, p<0.05). Each physician’s patient-centred communication score was the average of observer ratings.
Five 1 min video slices were created from each of the recordings from the two studies (n=340 slices) by dividing each video recording into five equal segments and selecting the first minute from each segment.55 88–90 The slices were observed and rated by naïve observers who had no training other than instructions to provide their ratings for patient and physician affect (eg, warm/friendly) and relational rapport (eg, attentive). The use of naïve observers is consistent with this type of methodology.55 88
Hypotheses and data analysis
Aim 1: assess and compare non-verbal synchrony between physicians and patients in racially concordant and racially discordant oncology interactions
We will achieve this aim by first matching video recordings from study 1 and study 2 on patient and physician sex and other sociodemographics. Although our focus is on racial concordance/discordance, prior research suggests that patient and physician sex affects communication in medical interactions.91–95 However, as described above, matching on sex is constrained by the distributions in the original recordings. Thus, from study 1, we will use 71 white female patients and 92 white male patients who interacted with White male physicians. From study 2, we will use the 34 black female patient/non-black male physician dyads and 34 black female patient/non-black female physician dyads. Thus, within race concordant and race discordant interactions, we will examine the effects of sex concordance and discordance. We acknowledge that this is not a full factorial design, but it will permit us to examine the influence of race concordance/discordance on non-verbal synchrony and, also partially examine whether the influence of race on non-verbal synchrony is moderated by patient and physician sex. To minimise any other differences between black patients and white patients, we will also do block matching of patients from study 1 with patients from study 2 on characteristics that might affect non-verbal communication (eg, age, type of cancer). We expect this matching will reduce the number of patients available from study 1 by 20%–30%, but sufficient cases will be available for well-powered analyses of racial concordance/discordance. We will then further the equivalence of patients with advanced methods of propensity scoring.96–98
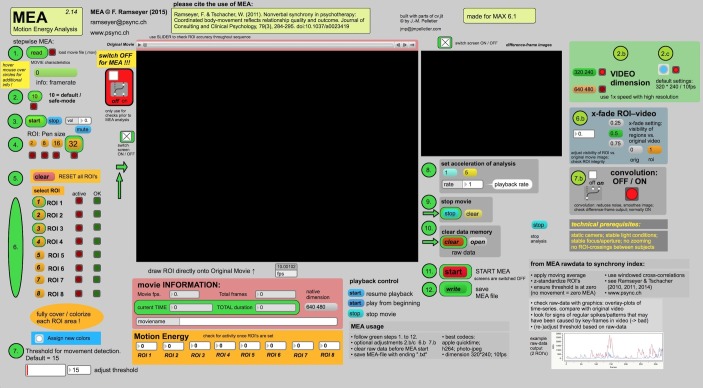
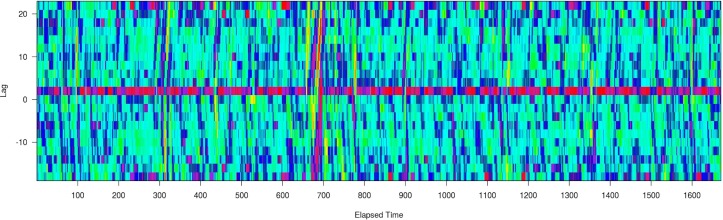
We will assess non-verbal synchrony in all matched interactions using customised Motion Energy Analysis (http://psync.ch/?p=9)76 99 software to obtain synchrony scores for each interaction. Figure 2 is a screenshot of the Motion Energy Analysis software. Motion Energy Analysis is an objective automated method that continuously monitors the amount of movement occurring in predefined regions of interest.62 76 100 Motion Energy Analysis captures frame-by-frame movement and provides quantification of change in movement in the ‘regions of interest’. In this study, we consider each individual as one ‘region of interest,’ allowing us to capture full body movement. Motion Energy Analysis uses pixel-differencing methods to measure total amount of movement. We will quantify non-verbal synchrony by deriving scores using windowed cross-correlation matrices to obtain synchrony scores for each interaction.101 Non-verbal synchrony tends to ebb and flow during conversations.91 Windowed cross-correlation accounts for the possibility of changing synchronisation by comparing small sections of time at different time lags. By looking at multiple smaller sections at multiple different lags, windowed cross-correlation is able to estimate synchronisation between systems which do not have a constant lag. Figure 3 is windowed cross-correlation output displayed as a heat map with warmer colours representing strong positive correlations between the two individuals’ behaviour (eg, positive non-verbal synchrony) and cooler colours representing strong negative correlations (eg, negative non-verbal synchrony). These synchrony scores are dyadic attributes that represent amounts and relationships of synchronous movement within dyads. Once we have obtained these scores, we will compare (1) effects of race concordance versus discordance on non-verbal synchrony and (2) effects of sex concordance versus discordance on non-verbal synchrony and (3) determine the relative impact of race concordance/discordance versus sex concordance/discordance on non-verbal synchrony.
Figure 2.
Motion Energy Analysis software.
Figure 3.
Window cross-correlation output.
Hypothesis 1: Non-verbal synchrony will be greater in racially concordant than in racially discordant oncology interactions. To obtain time-varying synchrony scores, we will block each interaction into five equal segments and obtain synchrony scores for each segment using Motion Energy Analysis. This procedure also allows us to adjust for patients and physicians moving outside of the regions of interest set at the beginning of each segment and maximises the likelihood that we capture all patient and physician movement. For example, this strategy will help us capture continuous movement even if a patient or physician gets up from a seated position and walks outside of the predetermined region of interest. To model changes in dynamic and overall levels of synchrony, we will use structural equation modelling (SEM) methods, latent differential equations (LDE) and multilevel modelling (MLM) methods. LDE is a special case of SEM that allows for estimation of parameters of a proposed underlying dynamical system. LDE models contain parameters pertaining to the dynamics of a given system (eg, ‘eta’ and ‘zeta’ parameters of a latent harmonic oscillator model). We will use multigroup SEM modelling to test for differences in these parameters between racially concordant and racially discordant interactions. By using a likelihood ratio test comparing two models where (1) these dynamic parameters are free to vary and (2) where these parameters are constrained to be equal across models, we will be able to determine if the motion dynamics differ between racially concordant and racially discordant interactions. Using a three-level HLM model with time segments (level 1) nested within patient (level 2) and patient nested within physician (level 3), we will model changes in non-verbal synchrony based on a categorical variable modelling either racially concordant or racially discordant interactions. Assuming 168 dyads, an alpha of 0.05, a correlation coefficient of 0.1 and a linear time effect, we have a power of 0.8 to detect an effect size of 0.50.
Aim 2: determine the influence of non-verbal synchrony on physician communication and patient and physician affect in racially concordant and racially discordant oncology interactions
We will first collect the same observational measures for study 1 as in study 2, including physician patient-centred communication and patient and physician affect, and rapport. Trained research assistants will rate each of the racially concordant interactions on physicians’ patient-centred communication.48 Next, we will create thin slices of the interactions from study 1 and naïve observers will rate the slices using the same measures of physician–patient affect and rapport as in study 2. Then we will use the synchrony scores from aim 1 to compare the relationship between non-verbal synchrony and patient–physician affect and rapport in racially concordant and discordant interactions.
Hypothesis 2: Non-verbal synchrony will influence physician patient-centred communication, patient and physician affect, and relational rapport in racially concordant and racially discordant clinical interactions. We will use MLM and multigroup SEM to create a mediation model where non-verbal synchrony will predict level 2 (patient) and level 3 (physician) outcomes. Assuming 168 dyads, an alpha of 0.05 and a correlation coefficient of 0.1, we have power of 0.8 to detect an effect size of 0.48.
Aim 3: examine the antecedents and outcomes of non-verbal synchrony in racially discordant oncology interactions
We will achieve this aim using the synchrony scores from the racially discordant interactions in study 2. We will examine the relationships between non-verbal synchrony and (1) interaction outcomes collected in the parent study including: patient satisfaction, distress, perception of physicians’ patient-centred communication and treatment expectations, and physician perceptions of the patient (eg, willingness to follow treatment regimen) and (2) preinteraction physician and patient race-related attitudes and perceptions (eg, implicit bias; suspicion), also collected in the parent study.
Hypothesis 3: In the racially discordant oncology interactions, non-verbal synchrony will significantly negatively covary with patient postinteraction distress and positively covary with (1) patient postinteraction perceptions of physicians’ patient-centred communication and treatment expectations; (2) physicians’ postinteraction perceptions of patient personal characteristics (eg, understanding of treatment options) and their responses to treatment (eg, willingness to follow treatment regimen) and (3) observers’ ratings of physician patient-centred communication, patient and physician affect, and relational rapport. Using LDE, we will model dynamic parameter values of the fluctuations in non-verbal synchrony over the course of each interaction. These values will then be used as first-level predictors in an MLM model. The second-level predictors for this model will be values associated with physician and patient postinteraction perceptions of the interaction and of each other. Assuming 68 dyads, an alpha of 0.05 and a correlation coefficient of 0.1, we have a power of 0.9 to detect an effect size of 0.56.
Hypothesis 4: Non-verbal synchrony will significantly covary with preinteraction race-related attitudes and perceptions of the patient and physicians (eg, physician implicit bias, patient suspicion). We will create a three-level MLM. We will model synchrony assessed over five time segments nested within each patient and each patient nested within physician. Each patient–physician dyad will have its own average synchrony score.
Aim 4: Develop and test a mediational model that links physician and patient race-related attitudes and perceptions to non-verbal synchrony and, in turn, outcomes of race-related discordant oncology interactions.
Hypothesis 5: Non-verbal synchrony will mediate the relationship between preinteraction race-related attitudes and perceptions and postinteraction perceptions of the patients and physicians. To examine the proposed mediations in a multilevel context, we will use multilevel SEM, as described by Preacher et al.102 103 These models address potential conflated estimates of mediated effects that can arise when using multilevel data. Time segments will be nested within each patient and each patient will be nested within physician, with synchrony varying at each time point. We will use a single mediation model to assess how physician and patient race-related attitudes and perceptions influence interaction outcomes via their influence on non-verbal synchrony.
Patient and public involvement
Cancer survivors were heavily involved with both study 1 and study 2. Investigators had extensive conversations with survivors about their experiences as patients and survivors, which helped guide the research questions, measured outcomes and design of both studies.
Patients were not directly involved with developing the research questions and outcomes for this secondary analysis. However, this work extends naturally from the considerable previous work we have done focused on understanding and improving patient–oncologist communication for all patients, with special attention to patients more vulnerable to cancer treatment and mortality disparities. This secondary analysis will investigate another important aspect of patient–physician communication that our patient and physician partners have agreed needs research attention.
Recruitment to both study 1 and study 2 was done by the investigators and their research and clinic staff. As principal investigator, LMH, will disseminate results from this investigation through the Karmanos Cancer Institutes’ Department of Community Outreach and Education, which has regularly scheduled meetings with cancer survivors, caretakers and community stakeholders.
Ethics and dissemination
Only patients and physicians from the previous studies who provided their consent for secondary analyses of their data were included in the current study. The nature of the data makes it unlikely we will encounter ethical or safety issues.
We will submit our ongoing findings to relevant communication, social psychology and oncology conferences. Similarly, we plan to submit the final manuscripts to high-impact communication, social psychology and oncology peer-reviewed journals.
Strengths and limitations
This secondary analysis is innovative in its focus and method. This study explores non-verbal synchrony, a channel of communication that has not been previously examined in medical interactions. It takes advantage of existing datasets, which include video-recorded cancer treatment discussions of black and white patients with cancer, recorded with state-of-art recording equipment. It also applies automated behavioural coding software, thus introducing less error than traditional methods using human coders.
However, this study is not without limitations. First, this study takes advantage of existing datasets, but the video-recorded and self-report data were not collected with the current hypotheses in mind. Second, the data are not evenly distributed by sex and race. As is often the case with medical research involving actual patients, the distributions of study patient characteristics are constrained by the distributions of patient demographic and medical characteristics of the patients who are treated at the participating hospitals. This reality precludes us from fully examining all combinations of race and sex. However, there are advantages to the fact that this research is conducted in a real-world, rather than a laboratory setting; also, we are able to account for some variability in our models by treating certain factors (eg, cancer type) as random effects. Last, although given a design that is adequately powered to make both between-subject and within-subject comparisons, it is still possible we may find no significant findings regarding non-verbal synchrony. Of course, this finding would be interesting in and of itself and would direct research attention to other avenues of investigation.
Supplementary Material
Footnotes
Contributors: All authors meet criteria for authorship. LMH: principal investigator, involved in all aspects of conceptualisation and study design. RM: research assistant, involved in the study design and responsible for design and implementation of statistical anlayses. TLA: coinvestigator, involved in all aspects of conceptualisation and study design. SB: coinvestigator, involved in all aspects of conceptualisation and study design and responsible for design and implementation of statistical analyses. SE: coinvestigator, involved in all aspects of conceptualisation and study design. LAP: coinvestigator, involved in all aspects of conceptualisation and study design.
Funding: This work was supported by the National Institutes of Health/National Institute on Minority Health and Health Disparities 1R21MD011766-01A1 (LMH, PI).
Competing interests: None declared.
Patient consent: Not required.
Ethics approval: Studies 1 (069003B3D), 2 (125211B3E) and the current study (044716B3E) are all approved by the Wayne State University Institutional Review Board.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. National Center for Health Statistics. Health, United States, 2015: with special feature on racial and ethnic health disparities. Hyattsville, MD: National Center for Health Statistics, 2016. [PubMed] [Google Scholar]
- 2. Murphy CC, Harlan LC, Warren JL, et al. Race and insurance differences in the receipt of adjuvant chemotherapy among patients with stage III colon cancer. J Clin Oncol 2015;33:2530–6. 10.1200/JCO.2015.61.3026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Bach PB, Schrag D, Brawley OW, et al. Survival of blacks and whites after a cancer diagnosis. JAMA 2002;287:2106–13. 10.1001/jama.287.16.2106 [DOI] [PubMed] [Google Scholar]
- 4. Greenwald HP, Polissar NL, Borgatta EF, et al. Social factors, treatment, and survival in early-stage non-small cell lung cancer. Am J Public Health 1998;88:1681–4. 10.2105/AJPH.88.11.1681 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ramsey SD, Howlader N, Etzioni RD, et al. Chemotherapy use, outcomes, and costs for older persons with advanced non-small-cell lung cancer: evidence from surveillance, epidemiology and end results-Medicare. J Clin Oncol 2004;22:4971–8. 10.1200/JCO.2004.05.031 [DOI] [PubMed] [Google Scholar]
- 6. Smedley BD, Stith AY, Nelson AR. Unequal treatment: confronting racial and ethnic disparities in health care: Institute of Medicine, 2003. [PubMed] [Google Scholar]
- 7. Tehranifar P, Neugut AI, Phelan JC, et al. Medical advances and racial/ethnic disparities in cancer survival. Cancer Epidemiol Biomarkers Prev 2009;18:2701–8. 10.1158/1055-9965.EPI-09-0305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Patel MI, Ma Y, Mitchell B, et al. How do differences in treatment impact racial and ethnic disparities in acute myeloid leukemia? Cancer Epidemiol Biomarkers Prev 2015;24:344–9. 10.1158/1055-9965.EPI-14-0963 [DOI] [PubMed] [Google Scholar]
- 9. Ward E, Jemal A, Cokkinides V, et al. Cancer disparities by race/ethnicity and socioeconomic Status. CA: A Cancer J Clin 2004;54:78–93. 10.3322/canjclin.54.2.78 [DOI] [PubMed] [Google Scholar]
- 10. Ghafoor A, Jemal A, Ward E, et al. Trends in breast cancer by race and ethnicity. CA Cancer J Clin 2003;53:342–55. 10.3322/canjclin.53.6.342 [DOI] [PubMed] [Google Scholar]
- 11. Jemal A, Siegel R, Ward E, et al. Cancer statistics, 2006. CA Cancer J Clin 2006;56:106–30. 10.3322/canjclin.56.2.106 [DOI] [PubMed] [Google Scholar]
- 12. Siegel R, Ma J, Zou Z, et al. Cancer statistics, 2014. CA Cancer J Clin 2014;64:9–29. 10.3322/caac.21208 [DOI] [PubMed] [Google Scholar]
- 13. Hardy D, Liu CC, Xia R, et al. Racial disparities and treatment trends in a large cohort of elderly black and white patients with nonsmall cell lung cancer. Cancer 2009;115:2199–211. 10.1002/cncr.24248 [DOI] [PubMed] [Google Scholar]
- 14. Agency for Healthcare Research and Quality. 2014 National healthcare quality and disparities report. Rockville, MD: Agency for Healthcare Research and Quality, 2015. [Google Scholar]
- 15. Griggs JJ, Sorbero ME, Stark AT, et al. Racial disparity in the dose and dose intensity of breast cancer adjuvant chemotherapy. Breast Cancer Res Treat 2003;81:21–31. 10.1023/A:1025481505537 [DOI] [PubMed] [Google Scholar]
- 16. Morris AM, Billingsley KG, Hayanga AJ, et al. Residual treatment disparities after oncology referral for rectal cancer. J Natl Cancer Inst 2008;100:738–44. 10.1093/jnci/djn145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Berger M, Lund MJ, Brawley OW. Racial disparities in lung cancer. Curr Probl Cancer 2007;31:202–10. 10.1016/j.currproblcancer.2007.02.002 [DOI] [PubMed] [Google Scholar]
- 18. Daly B, Olopade OI. A perfect storm: How tumor biology, genomics, and health care delivery patterns collide to create a racial survival disparity in breast cancer and proposed interventions for change. CA Cancer J Clin 2015;65:221–38. 10.3322/caac.21271 [DOI] [PubMed] [Google Scholar]
- 19. Hayn MH, Orom H, Shavers VL, et al. Racial/ethnic differences in receipt of pelvic lymph node dissection among men with localized/regional prostate cancer. Cancer 2011;117:4651–8. 10.1002/cncr.26103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Penner LA, Eggly S, Griggs JJ, et al. Life-threatening disparities: the treatment of black and white cancer patients. J Soc Issues 2012;68:328–57. 10.1111/j.1540-4560.2012.01751.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Meghani SH, Kang Y, Chittams J, et al. African Americans with cancer pain are more likely to receive an analgesic with toxic metabolite despite clinical risks: a mediation analysis study. J Clin Oncol 2014;32:2773–9. 10.1200/JCO.2013.54.7992 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Hassett MJ, Schymura MJ, Chen K, et al. Variation in breast cancer care quality in New York and California based on race/ethnicity and Medicaid enrollment. Cancer 2016;122 10.1002/cncr.29777 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Phelan JC, Link BG. Is Racism a fundamental cause of inequalities in health? Annu Rev Sociol 2015;41:311–30. 10.1146/annurev-soc-073014-112305 [DOI] [Google Scholar]
- 24. Jean-Pierre P, Fiscella K, Griggs J, et al. Race/ethnicity-based concerns over understanding cancer diagnosis and treatment plan. J Natl Med Assoc 2010;102:184–9. 10.1016/S0027-9684(15)30524-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Eggly S, Harper FW, Penner LA, et al. Variation in question asking during cancer clinical interactions: a potential source of disparities in access to information. Patient Educ Couns 2011;82:63–8. 10.1016/j.pec.2010.04.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Eggly S, Barton E, Winckles A, et al. A disparity of words: racial differences in oncologist-patient communication about clinical trials. Health Expect 2015;18:1316–26. 10.1111/hex.12108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Gordon HS, Street RL, Sharf BF, et al. Racial differences in doctors’ information-giving and patients’ participation. Cancer 2006;107:1313–20. 10.1002/cncr.22122 [DOI] [PubMed] [Google Scholar]
- 28. Gordon HS, Street RL, Sharf BF, et al. Racial differences in trust and lung cancer patients’ perceptions of physician communication. J Clin Oncol 2006;24:904–9. 10.1200/JCO.2005.03.1955 [DOI] [PubMed] [Google Scholar]
- 29. Siminoff LA, Graham GC, Gordon NH. Cancer communication patterns and the influence of patient characteristics: disparities in information-giving and affective behaviors. Patient Educ Couns 2006;62:355–60. 10.1016/j.pec.2006.06.011 [DOI] [PubMed] [Google Scholar]
- 30. Song L, Hamilton JB, Moore AD. Patient-healthcare provider communication: perspectives of African American cancer patients. Health Psychol 2012;31:539–47. 10.1037/a0025334 [DOI] [PubMed] [Google Scholar]
- 31. Penner LA, Dovidio JF, West TV, et al. Aversive racism and medical interactions with Black patients: A field study. J Exp Soc Psychol 2010;46:436–40. 10.1016/j.jesp.2009.11.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Boulware LE, Cooper LA, Ratner LE, et al. Race and trust in the health care system. Public Health Rep 2003;118:358–65. 10.1016/S0033-3549(04)50262-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Nguyen GC, LaVeist TA, Harris ML, et al. Patient trust-in-physician and race are predictors of adherence to medical management in inflammatory bowel disease. Inflamm Bowel Dis 2009;15:1233–9. 10.1002/ibd.20883 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Thompson HS, Valdimarsdottir HB, Winkel G, et al. The Group-Based Medical Mistrust Scale: psychometric properties and association with breast cancer screening. Prev Med 2004;38:209–18. 10.1016/j.ypmed.2003.09.041 [DOI] [PubMed] [Google Scholar]
- 35. Bird ST, Bogart LM. Perceived race-based and socioeconomic status(SES)-based discrimination in interactions with health care providers. Ethn Dis 2001;11:554–63. [PubMed] [Google Scholar]
- 36. Bird ST, Bogart LM, Delahanty DL. Health-related correlates of perceived discrimination in HIV care. AIDS Patient Care STDS 2004;18:19–26. 10.1089/108729104322740884 [DOI] [PubMed] [Google Scholar]
- 37. O’Malley AS, Sheppard VB, Schwartz M, et al. The role of trust in use of preventive services among low-income African-American women. Prev Med 2004;38:777–85. 10.1016/j.ypmed.2004.01.018 [DOI] [PubMed] [Google Scholar]
- 38. Green AR, Carney DR, Pallin DJ, et al. Implicit bias among physicians and its prediction of thrombolysis decisions for black and white patients. J Gen Intern Med 2007;22:1231–8. 10.1007/s11606-007-0258-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Hagiwara N, Penner LA, Gonzalez R, et al. Racial attitudes, physician-patient talk time ratio, and adherence in racially discordant medical interactions. Soc Sci Med 2013;87:123–31. 10.1016/j.socscimed.2013.03.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Cooper LA, Roter DL, Carson KA, et al. The associations of clinicians’ implicit attitudes about race with medical visit communication and patient ratings of interpersonal care. Am J Public Health 2012;102:979–87. 10.2105/AJPH.2011.300558 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Blair IV, Steiner JF, Fairclough DL, et al. Clinicians’ implicit ethnic /racial bias and perceptions of care among Black and Latino patients. Ann Fam Med 2013;11:43–52. 10.1370/afm.1442 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Hausmann LR, Myaskovsky L, Niyonkuru C, et al. Examining implicit bias of physicians who care for individuals with spinal cord injury: A pilot study and future directions. J Spinal Cord Med 2015;38:102–10. 10.1179/2045772313Y.0000000184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Hamel LM, Chapman R, Malloy M, et al. Critical shortage of African American Medical Oncologists in the United States. J Clin Oncol 2015;33:3697–700. 10.1200/JCO.2014.59.2493 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Kirkwood MK, Kosty MP, Bajorin DF, et al. Tracking the workforce: the American Society of Clinical Oncology workforce information system. J Oncol Pract 2013;9:3–8. 10.1200/JOP.2012.000827 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Cooper-Patrick L, Gallo JJ, Gonzales JJ, et al. Race, gender, and partnership in the patient-physician relationship. JAMA 1999;282:583–9. 10.1001/jama.282.6.583 [DOI] [PubMed] [Google Scholar]
- 46. Cooper LA, Roter DL, Johnson RL, et al. Patient-centered communication, ratings of care, and concordance of patient and physician race. Ann Intern Med 2003;139:907–15. 10.7326/0003-4819-139-11-200312020-00009 [DOI] [PubMed] [Google Scholar]
- 47. Johnson RL, Roter D, Powe NR, et al. Patient race/ethnicity and quality of patient-physician communication during medical visits. Am J Public Health 2004;94:2084–90. 10.2105/AJPH.94.12.2084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Street RL, Gordon H, Haidet P. Physicians’ communication and perceptions of patients: is it how they look, how they talk, or is it just the doctor? Soc Sci Med 2007;65:586–98. 10.1016/j.socscimed.2007.03.036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Elliott AM, Alexander SC, Mescher CA, et al. Differences in physicians’ verbal and nonverbal communication with black and white patients at the end of life. J Pain Symptom Manage 2016;51:1–8. 10.1016/j.jpainsymman.2015.07.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Penner LA, Gaertner S, Dovidio JF, et al. A social psychological approach to improving the outcomes of racially discordant medical interactions. J Gen Intern Med 2013;28:1143–9. 10.1007/s11606-013-2339-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Penner LA, Dovidio JF, Gonzalez R, et al. The effects of oncologist implicit racial bias in racially discordant oncology interactions. J Clin Oncol 2016;34:2874–80. 10.1200/JCO.2015.66.3658 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Penner LA, Harper FWK, Dovidio JF, et al. The impact of Black cancer patients’ race-related beliefs and attitudes on racially-discordant oncology interactions: A field study. Soc Sci Med 2017;191:99–108. 10.1016/j.socscimed.2017.08.034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Penner LA, Blair IV, Albrecht TL, et al. Reducing racial health care disparities: a social psychological analysis. Policy Insights Behav Brain Sci 2014;1:204–12. 10.1177/2372732214548430 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Hamel LM, Manning MA, Penner LA, et al. Racial attitudes and nonverbal convergence of patients and physicians in oncology interactions. Published Abstract, Annals Behav Med 2017;51:S1742 10.1080/10410236.2013.783773 [DOI] [Google Scholar]
- 55. Richeson JA, Shelton JN. Brief report: thin slices of racial bias. J Nonverbal Behav 2005;29:75–86. 10.1007/s10919-004-0890-2 [DOI] [Google Scholar]
- 56. Dovidio JF, Kawakami K, Gaertner SL. Implicit and explicit prejudice and interracial interaction. J Pers Soc Psychol 2002;82:62–8. 10.1037/0022-3514.82.1.62 [DOI] [PubMed] [Google Scholar]
- 57. Dovidio JF, Kawakami K, Johnson C, et al. On the nature of prejudice: automatic and controlled processes. J Exp Soc Psychol 1997;33:510–40. 10.1006/jesp.1997.1331 [DOI] [Google Scholar]
- 58. Dovidio JF, LaFrance M. Race, ethnicity, and nonverbal behavior : Hall JA, Knapp M, Nonverbal communication. The Hague, The Netherlands: DeGruyter-Mouton, 2013:671–96. [Google Scholar]
- 59. Penner LA, Hagiwara N, Eggly S, et al. Racial healthcare disparities: a social psychological analysis. Eur Rev Soc Psychol 2013;24:70–122. 10.1080/10463283.2013.840973 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Kimura M, Daibo I. Interactional synchrony in conversations about emotional episodes: a measurement by “the Between-Participants Pseudosynchrony Experimental Paradigm”. J Nonverbal Behav 2006;30:115–26. 10.1007/s10919-006-0011-5 [DOI] [Google Scholar]
- 61. Condon WS, Ogston WD. Sound film analysis of normal and pathological behavior patterns. J Nerv Ment Dis 1966;143:338–47. 10.1097/00005053-196610000-00005 [DOI] [PubMed] [Google Scholar]
- 62. Ramseyer F, Tschacher W. Nonverbal synchrony or random coincidence? How to tell the difference. Development of Multimodal Interfaces: Active Listing and Synchrony 2010;5967:182–96. [Google Scholar]
- 63. Moulder RG, Boker SM, Ramseyer F, et al. Determining synchrony between behavioral time series: An application of surrogate data generation for establishing falsifiable null-hypotheses. Psychol Methods 2018. 10.1037/met0000172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Ramseyer F, Tschacher W. Synchrony: a core concept for a constructivist approach to psychotherapy. Constructivism in the Human Sciences 2006;11:150–71. [Google Scholar]
- 65. Chartrand TL, Lakin JL. The antecedents and consequences of human behavioral mimicry. Annu Rev Psychol 2013;64:285–308. 10.1146/annurev-psych-113011-143754 [DOI] [PubMed] [Google Scholar]
- 66. White K, Argo JJ. When imitation doesn’t flatter: the role of consumer distinctiveness in responses to mimicry. J Consum Res 2011;38:667–80. 10.1086/660187 [DOI] [Google Scholar]
- 67. Chartrand TL, Maddux WW, Lakin JL. Beyond the perception-behavior link: the ubiquitous utility and motivational moderators of nonconscious mimicry : Hassin RR, Uleman JS, Bargh JA, The new unconscious: Oxford University Press, 2005:334–61. [Google Scholar]
- 68. Vacharkulksemsuk T, Fredrickson BL. Strangers in sync: achieving embodied rapport through shared movements. J Exp Soc Psychol 2012;48:399–402. 10.1016/j.jesp.2011.07.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Hove MJ, Risen JL. It’s all in the timing: interpersonal synchrony increases affiliation. Soc Cogn 2009;27:949–60. 10.1521/soco.2009.27.6.949 [DOI] [Google Scholar]
- 70. Miles LK, Griffiths JL, Richardson MJ, et al. Too late to coordinate: contextual influences on behavioral synchrony. Eur J Soc Psychol 2010;40:52–60. [Google Scholar]
- 71. Miles LK, Lumsden J, Richardson MJ, et al. Do birds of a feather move together? Group membership and behavioral synchrony. Exp Brain Res 2011;211:495–503. 10.1007/s00221-011-2641-z [DOI] [PubMed] [Google Scholar]
- 72. Sacheli LM, Christensen A, Giese MA, et al. Prejudiced interactions: implicit racial bias reduces predictive simulation during joint action with an out-group avatar. Sci Rep 2015;5:8507 10.1038/srep08507 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Paladino MP, Mazzurega M, Pavani F, et al. Synchronous multisensory stimulation blurs self-other boundaries. Psychol Sci 2010;21:1202–7. 10.1177/0956797610379234 [DOI] [PubMed] [Google Scholar]
- 74. Wiltermuth S. Synchrony and destructive obedience. Soc Influ 2012;7:78–89. 10.1080/15534510.2012.658653 [DOI] [Google Scholar]
- 75. Wiltshire TJ, Steffensen SV, Fiore SM. Multiscale movement coordination dynamics in collaborative team problem solving. Appl Ergon 2018. doi: 10.1016/j.apergo.2018.07.007 [Epub ahead of print 10 Aug 2018]. 10.1016/j.apergo.2018.07.007 [DOI] [PubMed] [Google Scholar]
- 76. Ramseyer F, Tschacher W. Nonverbal synchrony in psychotherapy: coordinated body movement reflects relationship quality and outcome. J Consult Clin Psychol 2011;79:284–95. 10.1037/a0023419 [DOI] [PubMed] [Google Scholar]
- 77. Valdesolo P, Ouyang J, DeSteno D. The rhythm of joint action: synchrony promotes cooperative ability. J Exp Soc Psychol 2010;46:693–5. 10.1016/j.jesp.2010.03.004 [DOI] [Google Scholar]
- 78. Macrae CN, Duffy OK, Miles LK, et al. A case of hand waving: Action synchrony and person perception. Cognition 2008;109:152–6. 10.1016/j.cognition.2008.07.007 [DOI] [PubMed] [Google Scholar]
- 79. Miles LK, Nind LK, Henderson Z, et al. Moving memories: Behavioral synchrony and memory for self and others. J Exp Soc Psychol 2010;46:457–60. 10.1016/j.jesp.2009.12.006 [DOI] [Google Scholar]
- 80. Albrecht TL, Eggly SS, Gleason ME, et al. Influence of clinical communication on patients’ decision making on participation in clinical trials. J Clin Oncol 2008;26:2666–73. 10.1200/JCO.2007.14.8114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Eggly S, Hamel LM, Foster TS, et al. Randomized trial of a question prompt list to increase patient active participation during interactions with black patients and their oncologists. Patient Educ Couns 2017;100:818–26. 10.1016/j.pec.2016.12.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Penner LA, Orom H, Albrecht TL, et al. Camera-related behaviors during video recorded medical interactions. J Nonverbal Behav 2007;31:99–117. 10.1007/s10919-007-0024-8 [DOI] [Google Scholar]
- 83. Riddle DL, Albrecht TL, Coovert MD, et al. Differences in audiotaped versus videotaped physician-patient interactions. J Nonverbal Behav 2002;26:219–39. 10.1023/A:1022160117278 [DOI] [Google Scholar]
- 84. Dugan E, Trachtenberg F, Hall MA. Development of abbreviated measures to assess patient trust in a physician, a health insurer, and the medical profession. BMC Health Serv Res 2005;5:64 10.1186/1472-6963-5-64 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Greenwald AG, Nosek BA, Banaji MR. Understanding and using the implicit association test: I. An improved scoring algorithm. J Pers Soc Psychol 2003;85:197–216. 10.1037/0022-3514.85.2.197 [DOI] [PubMed] [Google Scholar]
- 86. Jacobsen PB. Screening for psychological distress in cancer patients: challenges and opportunities. J Clin Oncol 2007;25:4526–7. 10.1200/JCO.2007.13.1367 [DOI] [PubMed] [Google Scholar]
- 87. Stewart M, Brown JB, Donner A, et al. The impact of patient-centered care on outcomes. J Fam Pract 2000;49:796–804. [PubMed] [Google Scholar]
- 88. Ambady N, Rosenthal R. Thin slices of expressive behavior as predictors of interpersonal consequences: a meta-analysis. Psychol Bull 1992;111:256–74. 10.1037/0033-2909.111.2.256 [DOI] [Google Scholar]
- 89. Murphy NA. Using thin slices for behavioral coding. J Nonverbal Behav 2005;29:235–46. 10.1007/s10919-005-7722-x [DOI] [Google Scholar]
- 90. Roter DL, Hall JA, Blanch-Hartigan D, et al. Slicing it thin: new methods for brief sampling analysis using RIAS-coded medical dialogue. Patient Educ Couns 2011;82:410–9. 10.1016/j.pec.2010.11.019 [DOI] [PubMed] [Google Scholar]
- 91. Roter DL, Hall JA, Aoki Y. Physician gender effects in medical communication: a meta-analytic review. JAMA 2002;288:756–64. [DOI] [PubMed] [Google Scholar]
- 92. Janssen SM, Lagro-Janssen AL. Physician’s gender, communication style, patient preferences and patient satisfaction in gynecology and obstetrics: a systematic review. Patient Educ Couns 2012;89:221–6. 10.1016/j.pec.2012.06.034 [DOI] [PubMed] [Google Scholar]
- 93. Schieber AC, Delpierre C, Lepage B, et al. Do gender differences affect the doctor-patient interaction during consultations in general practice? Results from the INTERMEDE study. Fam Pract 2014;31:706–13. 10.1093/fampra/cmu057 [DOI] [PubMed] [Google Scholar]
- 94. Inglehart MR. Interactions between patients and dental care providers: does gender matter? Dent Clin North Am 2013;57:357–70. 10.1016/j.cden.2013.02.003 [DOI] [PubMed] [Google Scholar]
- 95. Bertakis KD, Azari R. Patient-centered care: the influence of patient and resident physician gender and gender concordance in primary care. J Womens Health 2012;21:326–33. 10.1089/jwh.2011.2903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Iacus SM, King G, Porro G. Causal inference without balance checking: coarsened exact matching. Political Analysis 2012;20:1–24. 10.1093/pan/mpr013 [DOI] [Google Scholar]
- 97. King GN R. Why propensity scores should not be used for matching, 2016. Working Paper. [Google Scholar]
- 98. Austin PC. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivariate Behav Res 2011;46:399–424. 10.1080/00273171.2011.568786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Motion Energy Analysis (MEA). http://www.psync.ch2016
- 100. Ramseyer F, Tschacher W. Nonverbal synchrony in psychotherapy: Coordinated movement, the therapeutic relationship and outcome. Internat J Psychol 2008;43:59. [DOI] [PubMed] [Google Scholar]
- 101. Boker SM, Xu M, Rotondo JL, et al. Windowed cross-correlation and peak picking for the analysis of variability in the association between behavioral time series. Psychol Methods 2002;7:338–55. 10.1037/1082-989X.7.3.338 [DOI] [PubMed] [Google Scholar]
- 102. Preacher KJ, Zyphur MJ, Zhang Z. A general multilevel SEM framework for assessing multilevel mediation. Psychol Methods 2010;15:209–33. 10.1037/a0020141 [DOI] [PubMed] [Google Scholar]
- 103. Preacher KJ, Zhang Z, Zyphur MJ. Alternative methods for assessing mediation in multilevel data: the advantages of multilevel SEM. Structural Equation Modeling: A Multidisciplinary Journal 2011;18:161–82. 10.1080/10705511.2011.557329 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.