Abstract
Background
Atypical BCR-ABL1 transcripts are detected in less than 5% of patients diagnosed with chronic myeloid leukaemia (CML), of which e19a2 is the most frequently observed, with breakpoints in the micro breakpoint cluster region (μ-BCR) and coding for the p230 BCR-ABL1 protein. p230 CML is associated with various clinical presentations and courses with variable responses to first-line imatinib.
Case presentation
Here we report a case of imatinib resistance due to an E255V mutation, followed by early post-transplant relapse with a T315I mutation that achieved a persistent negative deep molecular response (MR5.0) after treatment with single-agent ponatinib. Using CastPCR, we could trace back the presence of the T315I mutation to all the RNA samples up to the detection of T315 mutation by Sanger sequencing shortly after allogeneic hematopoietic stem cell transplantation (HSCT).
Conclusion
This case illustrates the major interest of ponatinib as a valid treatment option for e19a2 CML patients who present a T315I mutation following relapse after HSCT.
Electronic supplementary material
The online version of this article (10.1186/s12885-018-5100-4) contains supplementary material, which is available to authorized users.
Keywords: CML, T315I, Relapse, HSCT, Ponatinib
Background
Chronic myeloid leukaemia (CML) is a myeloproliferative neoplasia caused by the fusion of the BCR and ABL1 genes, usually as the result of the reciprocal translocation t(9;22)(q34;q11.2). The exact breakpoint of the translocation and the molecular weight of the resulting fusion gene protein are variable, with most of the breakpoints on chromosome 22 falling in the major breakpoint cluster region (M-BCR), between exons 13 and 14 of the BCR gene, leading to a BCR–ABL1 mRNA with e13a2 or e14a2 junctions encoding for a p210 fusion protein [1]. Less than 5% of patients express atypical transcript types, of which e19a2, with breakpoints in the micro breakpoint cluster region (μ-BCR) and coding for the p230 BCR-ABL1 protein, is the most frequently encountered with a frequency of 0.7–2.7% of the cases [2, 3]. p230 CML has been associated with various clinical presentations and courses with variable responses to first-line imatinib, possibly confounded due to reporting bias in favour of cases with atypical features and/or responses [4–7]. The present study reports the case of a patient with p230 CML that was successfully treated with the third-generation tyrosine kinase inhibitor (TKI) ponatinib, following an early relapse with a T315I mutation after allogeneic stem cell transplantation.
Case presentation
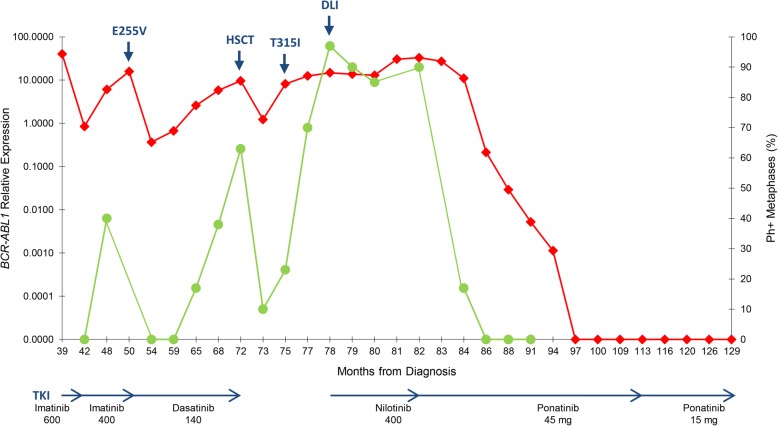
In November 2007, a 51 year-old man was admitted to the Centre Hospitalier Universitaire Vaudois in Switzerland for observation due to leucocytosis. His white blood cell (WBC) count was 232,000/μL, with 130,000/μL neutrophils (69.8%), 2300/μL basophils (1%), 7000/μL eosinophils (3%), 140 × 109/L platelets, 9.5 g/dL hemoglobin, and 2% peripheral blood blasts. He had no liver or spleen enlargement. The calculated Sokal, EUTOS and ELTS scores were low (0.64), low (7), and intermediate (1.639), respectively. A bone marrow aspirate showed marked hypercellularity and myelogenous hyperplasia without an increase in the blast ratio. Cytogenetic analysis showed the presence of a 46,XY,t(9;22)(q34;q11.2),+der(22)t(9;22) karyotype in 25 metaphases, and the presence of a BCR-ABL1 gene fusion was confirmed by FISH analysis. Molecular analysis revealed the presence of an e19a2 BCR-ABL1 transcript and the patient was diagnosed with an e19a2-positive chronic phase CML. The detection of an additional Ph+, a major route abnormality that has been reported as an adverse prognostic factor, does not mandate in daily practice a different initial treatment approach [8], therefore imatinib 400 mg QD was started. The patient rapidly achieved an haematological response and, after 3 months of treatment, a partial cytogenetic response (PCyR) was observed (28% Ph + metaphases), corresponding to an optimal response according to the ELN guidelines [8]. After 6 months of imatinib therapy, he lost his cytogenetic response (CyR), with all the metaphases analysed showing the same karyotype detected at diagnosis, which suggested treatment failure [8]. At this point, the patient interrupted the treatment and was lost to follow-up. In May 2010, the patient presented with hyperleukocytosis (300,000/μL), left abdominal pain and malaise. A CT scan revealed a splenomegaly of 20 cm and karyotype analysis showed the presence in 25 metaphases of the same karyotype observed at diagnosis. In view of the patient’s previous history, it was decided to initiate treatment with imatinib 600 mg QD. After 4 months of therapy, he was in haematological remission, but karyotype analysis showed only a minimal cytogenetic response (75% Ph + metaphases). In December 2010, 6 months after starting therapy, his cytogenetic response improved to a minor response (45% Ph + metaphases), corresponding to a sub-optimal response [8]. In February 2011, by decision of the patient, he was transferred to our institute (Additional file 1: Table S1). At the time of admission, he was in complete haematological response. Molecular analysis showed the presence of an e19a2 BCR-ABL1 transcript, but no cytogenetic analysis was performed. In order to quantitate the e19a2 BCR-ABL1 transcript and monitor response to treatment, a BCR exon 19 forward primer was designed (ENF007; 5′- CACTGAAGGCAGCCTTCGA-3′) and used with reverse primer ENR561 and probe ENP541 (7). A standard curve was established by tenfold dilutions of patient cDNA. Control ABL1 transcripts were detected as previously described [9]. At this point, 9 months after restarting imatinib therapy, the BCR-ABL1/ABL1 ratio was 40.258% (Fig. 1). Three months later, at the 12-month evaluation, the patient finally achieved a complete cytogenetic response (CCyR), with a BCR-ABL1 level of 0.846% (Fig. 1). At this point, and taking into account the good response to treatment, the patient was switched to imatinib 400 QD. However, 6 months later, karyotype analysis showed loss of CCyR (40% Ph + metaphases; minor CyR), with a concomitant rise in BCR-ABL1 levels (6.070%). Two months later, an additional rise in BCR-ABL1 levels to 15.820%, confirmed loss of molecular response and prompted search for mutations in the ABL1 kinase domain as previously reported [10]. Sanger sequencing allowed identification of an E255V mutation (Fig. 1), leading to start of second line dasatinib therapy (140 mg QD), and prompting search for an unrelated stem cell donor. Three months after start of dasatinib therapy, the patient achieved a CCyR with a BCR-ABL1 level of 0.365% and 5 months later, the patient maintained a CCyR, with a BCR-ABL1 level of 0.671%. However, in the following months, the patient showed a progressive loss of cytogenetic response: PCyR (17% Ph + metaphases), minor CyR (38% Ph + metaphases), and minor CyR (63% Ph + metaphases), 14 months, 17 months and 21 months after starting second-line dasatinib therapy, respectively. At this time, dasatinib therapy was stopped and the patient underwent allogeneic haematopoietic stem cell transplant (HSCT) from a 9/10 matched HLA unrelated donor (one HLA-B mismatch), after a non-myeloablative reduced-intensity conditioning (RIC) regimen that included busulfan, fludarabine and antithymocyte globulin (ATG). The graft-versus host disease (GVHD) prophylaxis consisted of the association of tacrolimus with mycophenolate mofetil (MMF). Neither acute GVHD nor other significant clinical complications were observed. One month after transplant, cytogenetic analysis showed persistence of disease (10% Ph + metaphases; PCyR), with a BCR-ABL1 level of 1.229%, which prompted start of nilotinib therapy (400 mg BID). Two months later, his BCR-ABL1 level rose to 8.132% with 23% Ph + metaphases (PCyR), suggesting resistant disease. Mutational analysis by Sanger sequencing revealed the presence of a T315I mutation, which led to the interruption of both nilotinib therapy and immunosuppression. Four months after transplant the patient lost his PCyR (70% Ph + metaphases; minor CyR) and his BCR-ABL1 levels increased to 12.477%. The patient showed mixed chimerism predominantly donor-derived. Since ponatinib was not available at the time at our institution and approval was pending, nilotinib therapy (400 mg BID) was restarted. One month later, karyotype analysis showed a minimal CyR (97% Ph + metaphases) and the patient was submitted to donor lymphocyte infusion (DLI), which resulted only in a minor CyR (90% Ph + metaphases) that nevertheless was maintained in the following months. This was, however, accompanied by increasing BCR-ABL1 levels to a maximum of 32.879%, 10 months after HSCT. The patient also showed progressive loss of donor chimerism (mixed chimerism with < 5% donor cells). At this point ponatinib approval was granted, nilotinib therapy was interrupted and ponatinib was started at the standard dose of 45 mg QD. Before ponatinib initiation, and considering its well-known cardiovascular toxicity profile, a comprehensive cardiologic and metabolic evaluation was performed. The only cardiovascular risk-factors identified were dyslipidaemia and arterial hypertension (AHT), which were already present since the beginning of the disease and were easily manageable with lifestyle modifications and therapy (enalapril/hydrochlorothiazide 20/12.5 mg, ½ tablet QD), respectively. Two months later, karyotype analysis showed a PCyR (17% Ph + metaphases) and a reduction of BCR-ABL1 levels (10.940%) was observed. Subsequently, four months later, the patient achieved a CCyR associated with a BCR-ABL1 level of 0.213%. In the following months a progressive decline in BCR-ABL1 levels was documented: 0.029% at 6 months (equivalent to a Major Molecular Response; MMR), 0.005% at 9 months (equivalent to a MR4.0), 0.001% at 12 months (equivalent to a MR4.5), and 0.000% at 15 months (equivalent to a MR5.0). The patient maintained ponatinib 45 mg QD treatment during an additional 16 months and, since a persistent and sustained MR5.0 with no detectable disease was documented, dosage was reduced to 15 mg QD. Treatment with ponatinib was well tolerated since the beginning of therapy with no evidence of toxicity. At the time of the last evaluation, 15 months after ponatinib dose reduction, the patient maintained a sustained MR5.0 with no detectable disease. No evidence of cardiovascular toxicity was observed at the last observation. Under ponatinib treatment, the patient maintained a mixed chimerism with < 5% donor cells. To evaluate if the T315I clone was present at low-levels in the earlier phases of the disease, we used CastPCR (Competitive Allele-Specific TaqMan PCR™, Applied Biosystems) specific for the T315I mutation in all the available RNA patient samples collected since he was admitted to our institution. For the T315I mutation detection, each sample was run in real-time PCR with the assay targeting both the mutation and the corresponding reference gene, according to the manufacturer’s instructions. After amplification, data files containing the samples Ct values were imported into Life Technologies Mutation Detector™ Software for post-PCR data analysis. CastPCR is highly specific and sensitive and can detect and quantitate rare amounts of mutated DNA/cDNA in a sample that contains large amounts of normal, i.e., non-mutated, DNA/cDNA, with a sensibility up to 0.1%. Using this approach, we could trace back the presence of the T315I mutation to all the RNA samples up to the detection of T315 mutation by Sanger sequencing shortly after HSCT.
Fig. 1.
Monitoring of BCR-ABL1 levels (red) and cytogenetic response (green) during the different treatments of the patient. HSCT, haematopoietic stem cell transplant; DLI, donor lymphocyte infusion
Discussion and conclusions
p230 CML has been associated with various clinical presentations and courses [4, 5] with recent data suggesting that these patients have a poor response to front-line imatinib therapy, but better responses to second-line nilotinib and dasatinib [6, 7]. Point mutations in the kinase domain (KD) of the ABL1 gene represent the most common resistance mechanism to TKI therapy in CML, occurring in 30–90% of patients who develop resistance to imatinib [11], with more than 100 different mutations reported, although many are only rarely detected clinically [11]. The relative in vitro sensitivity of different mutants to the various available TKI varies considerably and correlates well with the outcome after subsequent therapy with a different TKI [12]. Similarly, mutants that are less likely to be inhibited by a given TKI are more likely to emerge clinically during therapy with such inhibitors [13].
Here we report a case of imatinib resistance due to an E255V mutation, followed by early post-transplant relapse with a T315I mutation that achieved a persistent negative deep molecular response (MR5.0) after treatment with single-agent ponatinib. Recently, patients with E255K/V mutations have been described as having a particularly poor prognosis, regardless of the stage of the disease at detection, with a higher risk of transformation to advanced/blast phase, and a short survival [14]. Indeed, this mutation shows a high IC50 to all available TKIs, including third-generation ponatinb [15]. In this case, dasatinib has been suggested as the most likely option in terms of probability of response among all available TKIs [14]. Therefore, dasatinib treatment was initiated as a bridge to HSCT, and a CCyR was quickly achieved. However, in the following months, the patient lost CCyR and at the time of HSCT showed only a minor CyR. The best response achieved after HSCT was a PCyR, that was nevertheless quickly lost with mutation analysis revealing the presence of a T315I. Since the T315 mutation was retrospectively detected even before the detection of the E255V mutation, this suggests that at least two distinct BCR-ABL1 sub-clones were present at the start of therapy. This observation can be explained by differences in competitive advantage between mutant clones. Indeed, in vitro cell assays showed that selected mutant clones (for example, P-loop mutations Y253F, E255K) have higher transformation potency and proliferation rate compared with T315I, even in the absence of BCR-ABL1 inhibitors [16]. Assuming that imatinib has lower activity against these mutant clones with P-loop mutations, they may expand more rapidly than clones with the T315I mutation when exposed to imatinib [13]. On the other hand, it has been shown that dasatinib suppresses P-loop mutations to a greater extent than T315I [17], therefore a T315I positive clone may be able to increase its size during dasatinib treatment with relatively little competition from rapidly proliferating clones [13]. This hypothesis is supported by the observation that dasatinib treated patients seem to more frequently show T315I mutations [13]. This is in agreement with the model in which evolution of BCR-ABL1–positive cells is mainly shaped by TKI-selective pressure and the fitness of each ABL1 KD mutated population is the net result of the ability to survive treatment depending on the intrinsic sensitivity to the specific TKI administered and of the ability to survive the competition with all other coexisting populations [18].
Although our patient did not develop adverse events related to ponatinib therapy, its expected benefits must be balanced against the potential risks, including arterial hypertension, and serious arterial occlusive and venous thromboembolic events, reported in the PACE trial in 19 and 5% of patients, respectively. Published data support the observation that adverse events appear to be related to certain pre-existing cardiovascular risk factors, ponatinib dose, or both [19]. For this reason, and since our patient was in sustained MR5.0 with no detectable disease after 27 months of ponatinib therapy, the dose was reduced to 15 mg OD. Fifteen months later, the patient maintains a sustained MR5.0 with no detectable disease. Ponatinib efficacy was previously observed in a CML e19a2 patient refractory to both imatinib and dasatinib therapy due to the presence of a T315I mutation [20]. These results suggest that ponatinib could be an excellent therapeutic option in the treatment of e19a2 CML harbouring the T315I mutation refractory to previous therapies including HSCT, although more studies are necessary to draw a definitive conclusion.
Additional file
Table S1. Clinical and laboratory data of the patient. (DOCX 17 kb)
Acknowledgements
Not applicable.
Funding
This work was supported in part by an unrestricted grant from Incyte Corp.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AHT
Arterial hypertension
- ATG
Antithymocyte globulin
- CastPCR
Competitive Allele-Specific TaqMan PCR
- CCyR
Complete cytogenetic response
- CML
Chronic myeloid leukaemia
- CyR
Cytogenetic response
- DLI
Donor lymphocyte infusion
- GVHD
Graft-versus host disease
- HSCT
Haematopoietic stem cell transplant
- M-BCR
Major breakpoint cluster region
- MMF
Mycophenolate mofetil
- MMR
Major molecular response
- PCyR
Partial cytogenetic response
- RIC
Reduced-intensity conditioning
- TKI
Tyrosine kinase inhibitor
- WBC
White blood cell
- μ-BCR
Micro breakpoint cluster region
Authors’ contributions
NC, RBF, MRT, and AC designed the study. RS was responsible for sample processing. NC and SB performed the molecular studies. CC, LT, SL and JV performed the cytogenetic analysis. RBF, FC, CPV, LL, and AC provided patient samples and clinical data. NC and RBF were responsible for the collection, analysis and interpretation of data. NC, RBF, MRT, and AC were involved in drafting the manuscript. All authors contributed to revisions, read, and approved the final version of this manuscript.
Ethics approval and consent to participate
This study is in accordance with the ethical standards of the Ethics Committee of the Portuguese Oncology Institute of Porto (approval number 38.010) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Consent for publication
Written informed consent was obtained from the patient.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Nuno Cerveira, Email: nuno.cerveira@ipoporto.min-saude.pt.
Rosa Branca Ferreira, Email: r.branca.s.ferreira@gmail.com.
Susana Bizarro, Email: susana.bizarro@ipoporto.min-saude.pt.
Cecília Correia, Email: ceciliacorreia@ipoporto.min-saude.pt.
Lurdes Torres, Email: mlurdes.torres@ipoporto.min-saude.pt.
Susana Lisboa, Email: susanalisboa@ipoporto.min-saude.pt.
Joana Vieira, Email: joana.vieira@ipoporto.min-saude.pt.
Rui Santos, Email: ruimssantos89@gmail.com.
Fernando Campilho, Email: campilho@ipoporto.min-saude.pt.
Carlos Pinho Vaz, Email: cpvaz@ipoporto.min-saude.pt.
Luís Leite, Email: luisclaudioleite@gmail.com.
Manuel R. Teixeira, Email: manuel.teixeira@ipoporto.min-saude.pt
António Campos, Email: acampos@ipoporto.min-saude.pt.
References
- 1.Goldman JM, Melo JV. Chronic myeloid leukemia: advances in biology and new approaches to treatment. N Engl J Med. 2003;349(15):1451–1464. doi: 10.1056/NEJMra020777. [DOI] [PubMed] [Google Scholar]
- 2.Saglio G, Guerrasio A, Rosso C, Zaccaria A, Tassinari A, Serra A, et al. New type of Bcr/Abl junction in Philadelphia chromosome-positive chronic myelogenous leukemia. Blood. 1990;76(9):1819–1824. [PubMed] [Google Scholar]
- 3.Wilson GA, Vandenberghe EA, Pollitt RC, Rees DC, Goodeve AC, Peake IR, et al. Are aberrant BCR-ABL transcripts more common than previously thought? Br J Haematol. 2000;111(4):1109–1111. doi: 10.1046/j.1365-2141.2000.02471.x. [DOI] [PubMed] [Google Scholar]
- 4.Crampe M, Garry J, Langabeer SE, Murphy PT. Sustained molecular response with nilotinib in imatinib-intolerant chronic myeloid leukaemia with an e19a2 BCR-ABL1 fusion. Hematol Oncol Stem Cell Ther. 2016;9(4):168–169. doi: 10.1016/j.hemonc.2016.05.007. [DOI] [PubMed] [Google Scholar]
- 5.How GF, Tan LT, Lim LC. Chronic myeloid leukemia with e19a2 (c3a2) BCR/ABL fusion junction: is it truly a benign disease? Leukemia. 1998;12(7):1166–1167. doi: 10.1038/sj.leu.2401055. [DOI] [PubMed] [Google Scholar]
- 6.Andrikovics H, Nahajevszky S, Szilvási A, Bors A, Adám E, Kozma A, et al. First and second line imatinib treatment in chronic myelogenous leukemia patients expressing rare e1a2 or e19a2 BCR-ABL transcripts. Hematol Oncol. 2007;25(3):143–147. doi: 10.1002/hon.822. [DOI] [PubMed] [Google Scholar]
- 7.Qin YZ, Jiang Q, Jiang H, Lai YY, Shi HX, Chen WM, et al. Prevalence and outcomes of uncommon BCR-ABL1 fusion transcripts in patients with chronic myeloid leukaemia: data from a single Centre. Br J Haematol. 2018;182(5):693–700. doi: 10.1111/bjh.15453. [DOI] [PubMed] [Google Scholar]
- 8.Baccarani M, Deininger MW, Rosti G, Hochhaus A, Soverini S, Apperley JF, et al. European LeukemiaNet recommendations for the management of chronic myeloid leukemia: 2013. Blood. 2013;122(6):872–884. doi: 10.1182/blood-2013-05-501569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gabert J, Beillard E, van der Velden VH, Bi W, Grimwade D, Pallisgaard N, et al. Standardization and quality control studies of ‘real-time’ quantitative reverse transcriptase polymerase chain reaction of fusion gene transcripts for residual disease detection in leukemia - a Europe against Cancer program. Leukemia. 2003;17(12):2318–2357. doi: 10.1038/sj.leu.2403135. [DOI] [PubMed] [Google Scholar]
- 10.Branford S, Rudzki Z, Walsh S, Parkinson I, Grigg A, Szer J, et al. Detection of BCR-ABL mutations in patients with CML treated with imatinib is virtually always accompanied by clinical resistance, and mutations in the ATP phosphate-binding loop (P-loop) are associated with a poor prognosis. Blood. 2003;102(1):276–283. doi: 10.1182/blood-2002-09-2896. [DOI] [PubMed] [Google Scholar]
- 11.Jabbour E, Kantarjian H, Jones D, Talpaz M, Bekele N, O'Brien S, et al. Frequency and clinical significance of BCR-ABL mutations in patients with chronic myeloid leukemia treated with imatinib mesylate. Leukemia. 2006;20(10):1767–1773. doi: 10.1038/sj.leu.2404318. [DOI] [PubMed] [Google Scholar]
- 12.Jabbour E, Jones D, Kantarjian HM, O'Brien S, Tam C, Koller C, et al. Long-term outcome of patients with chronic myeloid leukemia treated with second-generation tyrosine kinase inhibitors after imatinib failure is predicted by the in vitro sensitivity of BCR-ABL kinase domain mutations. Blood. 2009;114(10):2037–2043. doi: 10.1182/blood-2009-01-197715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hughes TP, Saglio G, Quintás-Cardama A, Mauro MJ, Kim DW, Lipton JH, et al. BCR-ABL1 mutation development during first-line treatment with dasatinib or imatinib for chronic myeloid leukemia in chronic phase. Leukemia. 2015;29(9):1832–1838. doi: 10.1038/leu.2015.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Naqvi K, Cortes JE, Luthra R, O'Brien S, Wierda W, Borthakur G, et al. Characteristics and outcome of chronic myeloid leukemia patients with E255K/V BCR-ABL kinase domain mutations. Int J Hematol. 2018;107(6):689–695. doi: 10.1007/s12185-018-2422-6. [DOI] [PubMed] [Google Scholar]
- 15.Redaelli S, Mologni L, Rostagno R, Piazza R, Magistroni V, Ceccon M, et al. Three novel patient-derived BCR/ABL mutants show different sensitivity to second and third generation tyrosine kinase inhibitors. Am J Hematol. 2012;87(11):E125–E128. doi: 10.1002/ajh.23338. [DOI] [PubMed] [Google Scholar]
- 16.Griswold IJ, MacPartlin M, Bumm T, Goss VL, O'Hare T, Lee KA, et al. Kinase domain mutants of Bcr-Abl exhibit altered transformation potency, kinase activity, and substrate utilization, irrespective of sensitivity to imatinib. Mol Cell Biol. 2006;26(16):6082–6093. doi: 10.1128/MCB.02202-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gruber FX, Ernst T, Porkka K, Engh RA, Mikkola I, Maier J, et al. Dynamics of the emergence of dasatinib and nilotinib resistance in imatinib-resistant CML patients. Leukemia. 2012;26(1):172–177. doi: 10.1038/leu.2011.187. [DOI] [PubMed] [Google Scholar]
- 18.Soverini S, De Benedittis C, Machova Polakova K, Brouckova A, Horner D, Iacono M, et al. Unraveling the complexity of tyrosine kinase inhibitor-resistant populations by ultra-deep sequencing of the BCR-ABL kinase domain. Blood. 2013;122(9):1634–1648. doi: 10.1182/blood-2013-03-487728. [DOI] [PubMed] [Google Scholar]
- 19.Iclusig (summary of product characteristics) ARIAD Pharma Ltd. UK: Leatherhead; 2017. [Google Scholar]
- 20.Ferri CA, Bianchini M, Bengió RM, Moiraghi EB, Gonzalez MS, Noriega MF, et al. Clinical activity of ponatinib in one patient with chronic myeloid leukemia in chronic phase with e19a2 transcript and T315I mutation. Eur J Haematol. 2015;94(3):270–272. doi: 10.1111/ejh.12358. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Clinical and laboratory data of the patient. (DOCX 17 kb)
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.