Abstract
Background
Colorectal cancer remains a serious public health problem due to the poor prognosis. In the present study, we attempted to develop and validate a prognostic signature to predict the individual mortality risk in colorectal cancer patients.
Materials and Methods
The original study datasets were downloaded from The Cancer Genome Atlas database. The present study finally included 424 colorectal cancer patients with wholly gene expression information and overall survival information.
Results
A nine-lncRNA prognostic signature was built through univariate and multivariate Cox proportional regression model. Time-dependent receiver operating characteristic curves in model cohort demonstrated that the Harrell’s concordance indexes of nine-lncRNA prognostic signature were 0.768 (95% CI [0.717–0.819]), 0.778 (95% CI [0.727–0.829]) and 0.870 (95% CI [0.819–0.921]) for 1-year, 3-year and 5-year overall survival respectively. In validation cohort, the Harrell’s concordance indexes of nine-lncRNA prognostic signature were 0.761 (95% CI [0.710–0.812]), 0.801 (95% CI [0.750–0.852]) and 0.883 (95% CI [0.832–0.934]) for 1-year, 3-year and 5-year overall survival respectively. According to the median of nine-lncRNA prognostic signature score in model cohort, 424 CRC patients could be stratified into high risk group (n = 212) and low risk group (n = 212). Kaplan–Meier survival curves showed that the overall survival rate of high risk group was significantly lower than that of low risk group (P < 0.001).
Discussion
The present study developed and validated a nine-lncRNA prognostic signature for individual mortality risk assessment in colorectal cancer patients. This nine-lncRNA prognostic signature is helpful to evaluate the individual mortality risk and to improve the decision making of individualized treatments in colorectal cancer patients.
Keywords: Overall survival, Prognosis, LncRNA, Colorectal cancer, Prediction
Introduction
Colorectal cancer (CRC) is one of the most common malignant tumors and one of the leading causes of cancer-related death, resulting in 135,430 estimated new cases and 50,260 estimated deaths in the United States in 2017 (Siegel et al., 2017; Siegel, Miller & Jemal, 2016). The 5-year survival rates of CRC patients varied dramatically in patients with different tumor stages (Ferlay et al., 2010). The 5-year survival rate of localized CRC patients was 90%, whereas it was 71% and 14% for CRC patients with regional metastasis and distant metastasis respectively (Siegel et al., 2017). It was reported that the 5-year survival rate was approximately 10% in stage IV CRC patients (Sanoff et al., 2008). Therefore, it is of great importance to develop a reliable prognostic biomarker to predict the prognosis and optimize the clinical therapy decision.
Long non-coding RNAs (lncRNAs) are a class of non-coding RNAs more than 200 nucleotides in length (McFadden & Hargrove, 2016). The lncRNAs have been reported to be correlated with overall survival and might serve as prognostic biomarkers for CRC patients (Kita et al., 2017; Weng et al., 2017; Xie et al., 2016). Recently, several studies constructed lncRNAs-based prognostic signatures to predict the overall survival of CRC patients by using Cox proportional regression model (Fan & Liu, 2018; Xing et al., 2018; Xue et al., 2017; Zeng et al., 2017). However, these prognostic signatures have three limitations for clinical application. First, these prognostic signatures are too difficult to calculate for clinical application due to the complex formulas. For example, the prognostic signature constructed by Xing et al. (2018) did not provide detailed formula of random forest model and therefore was unrepeatable for clinical application. The study performed by Xue et al. calculated the prognostic risk score by using reads per kilobase per million mapped reads (RPKM) method. However, as the original gene expression read counts were not available for most studies, RPKM method was difficult to perform for clinical application in different population (Xue et al., 2017). Second, the clinical significances of prognostic risk scores in theses previous studies were difficult to understand for patients without medical knowledge. Third, these prognostic signatures provided merely the prediction of overall survival for a special subgroup, but not the individual risk prediction of overall survival. Therefore, an ideal individual risk predictive model should be easy to obtain, calculate and understand for clinical application.
Several studies have used nomogram method to predict the prognosis of different cancers (Li et al., 2015; Tian et al., 2017). This method has two advantages in predicting the prognosis. Firstly, the nomogram is convenient to calculate and evaluate the individual probability of disease without complex formula. Secondly, this method provides a straightforward individual risk and the result is easy to understand for patients. Therefore, the nomogram method is suitable for prediction of prognosis. To the best of our knowledge, the present study is the first to develop a prognostic nomogram by using the lncRNA expression data for overall survival of CRC patients.
In the present study, our objective was to develop and validate a lncRNA-based prognostic signature to predict the overall survival of CRC patients. To improve the quality of prognostic model, the development and validation of the prognostic model in the present study were performed in accordance with the guidelines of Transparent Reporting of a multivariable prediction model for Individual Prognosis Or Diagnosis (TRIPOD) (Collins et al., 2015).
Materials and Methods
Study protocol approval
The data download and analyses were performed according to the policies of The Cancer Genome Atlas (TCGA) database. Since the study datasets in the present study were all downloaded from TCGA database, additional ethics approval was not needed. All data collections and analyses were in accordance with the principles of Declaration of Helsinki.
The gene expression dataset
The original RNA sequencing dataset was obtained from GDC Data Portal (https://portal.gdc.cancer.gov/exploration). The dataset was downloaded in May 31, 2018. The RNA sequencing data were generated on the Illumina HiSeq 2000 RNA Sequencing platform. The downloaded RNA sequencing data contained the original gene read counts of 60,483 genes from 458 CRC tumor tissues and 41 non-tumor normal tissues. The duplicated samples were removed from the present study (n = 22). In the present study, the lncRNAs ID were downloaded from GENCODE Version 7 (Derrien et al., 2012). Finally the extracted gene expression data of 14,449 lncRNAs from 458 CRC tissues and 41 non-tumor normal tissues were selected for differentially expressed lncRNAs.
Differential expression analyses
The “edgeR” package was applied for the differential expression analyses and the original gene expression read counts was normalized by the Trimmed Mean of M (TMM) method (Robinson & Oshlack, 2010). The genes whose average expression read counts lower than 1 were filtered out from the present study. The F-tests was used for assessments of quasi-likelihood. Thresholds of differentially expressed lncRNAs were P adj <0.05 and —log2 fold change— >2.
Heat map and volcano map
The heat map and volcano map were drawn according to the normalized gene expression values of differentially expressed lncRNAs. The darker color represented higher expression level of differentially expressed lncRNA.
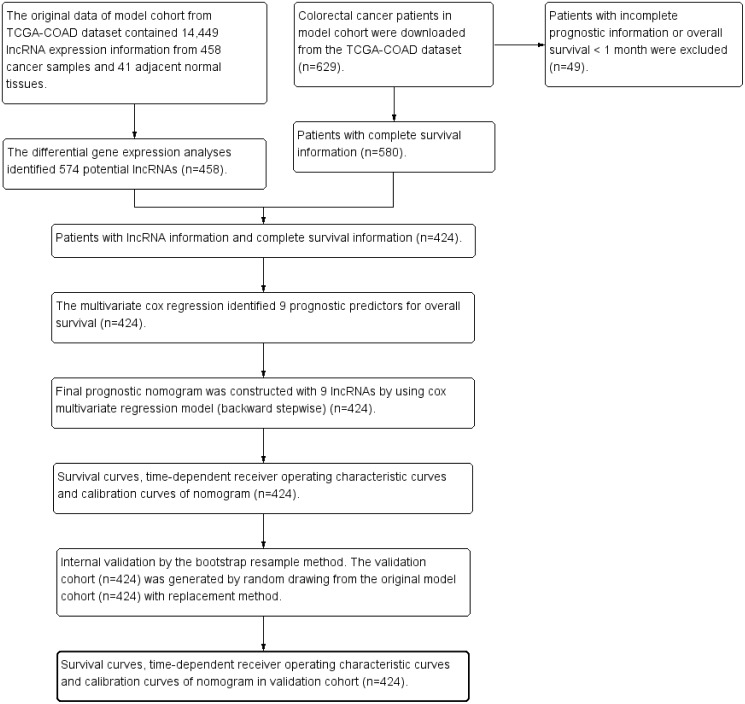
The model cohort
The clinical dataset of 629 CRC patients were downloaded from cBioPortal database (May 31, 2018, http://www.cbioportal.org/datasets). The patients with overall survival time less than one month were excluded from the present study to avoid the impact of unrelated causes of death (n = 49). The clinical dataset was matched to the gene expression dataset. The patients without gene expression information were excluded from the present study (n = 156). Finally 424 CRC patients were enrolled for further survival analysis. Figure 1 was the study flowchart for patient selection in the present study. The end-point in the present study was overall survival (OS). The average follow-up time was 30.0 ± 25.5 months. Overall survival time was calculated from initial diagnosis time to death time or the last follow-up time. The maximum value and the minimum value of overall survival time were 140.9 months and 1.0 month. The study time was from May 18, 2010 to January 27, 2015. The missing data in the present study were coded as “NA” in all tables and analyses.
Figure 1. Study flowchart in the present study.
TCGA, The Cancer Genome Atlas
Assessment of predictive performance
The Harrell’s concordance index (C-index), calibration plot and time-dependent receiver operating characteristic (ROC) curves were used to assess the predictive performance of prognostic signatures. The predictive performance of prognostic signature in the current study was compared with two previous prognostic signatures (named RS lncRNA score and Risk score). The formulas of the RS lncRNA score and the Risk score were as follows:
RS lncRNA score = (0. 1337 × expression value of RP1-170O19.17) + (0. 0633 × expression value of RP11-785D18.3) + (0. 8131 × expression value of RP11-798K3.2) + (−1.5194 × expression value of XXbac-B476C20.9) + (4. 3132 × expression value of RP11-481J13.1) + (0. 4497 × expression value of RP11-167H9.4) (Fan & Liu, 2018). In the formula of RS lncRNA score, the lncRNA expression values were normalized by “DEseq” packages.
Risk score =expLINC01555∗(−.191) + expRP11−108K3.1∗(0.318) + expLINC01207∗(−0.191) + expRP11−610P16.1∗(−0.163) (Zeng et al., 2017). In the formula of Risk score, the lncRNA expression values were log2-transformed.
Internal validation by using bootstrap resampling method
The bootstrap resampling method has been recommended for internal validation of the predictive model (Blackstone, 2001; Grunkemeier & Wu, 2004). The validation cohort in the present study was constructed by drawing 424 CRC patients with replacements from the original model cohort.
Statistical analysis
The statistical analyses were carried out by using the R software (version 3.4.1) and SPSS Statistics 19.0 (SPSS Inc., Armonk, NY, USA). The following R packages were carried out as needed in the current study: “survival”, “rms” , “pROC”, “plyr”, “glmnet”, and “timeROC”. Continuous variables in the present study were presented as mean ± standard deviation. Continuous variables were compared by t-test or Mann–Whitney U test. Categorical variables were compared by chi-squared test or Fisher’s exact test. A 2-tail P < 0.05 was defined as statistically significant in the present study.
Results
Study cohorts
The present study finally included 424 CRC patients with total lncRNA expression information and overall survival information. The average age was 66.7 ± 13.0 years and the average overall survival time was 30.0 ± 25.5 months in model cohort. There were 102 (24.0%) patients died during the follow-up period in model cohort, whereas there were 108 (25.5%) patients died during the follow-up period in validation cohort. The clinical characteristics of CRC patients in model cohort and validation cohort were summarized in Table 1. There were no significant differences in terms of clinical characteristics and lncRNA expression between model cohort and validation cohort. There were no missing data in terms of survival status, survival time and lncRNA expression value.
Table 1. The clinical features of colorectal cancer patients in model cohort and validation cohort.
| Model cohort (n = 424) | Validation cohort (n = 424) | P value | |
|---|---|---|---|
| Death (n(%)) | 102(24.0) | 108(25.5) | 0.633 |
| Survival time (mean ± SD, month) | 30.0 ± 25.5 | 28.6 ± 25.4 | 0.163 |
| Age (mean ± SD, year) | 66.7 ± 13.0 | 67.1 ± 12.4 | 0.612 |
| Gender (Male/Female) | 230/194 | 224/200 | 0.680 |
| Tumor site | |||
| Colon | 361(85.1) | 351(82.8) | 0.363 |
| Rectum | 58(13.7) | 69(16.3) | |
| NR | 5(1.2) | 4(0.9) | |
| AJCC Stage (IV/III/II/I/NA) | 59∕124∕162∕68∕11 | 58∕145∕143∕68∕10 | 0.578 |
| AJCC PT (T4/T3/T2/T1/NA) | 51∕292∕70∕11∕0 | 54∕286∕73∕11∕0 | 0.976 |
| AJCC PN (N2/N1/N0/NA) | 77∕102∕245∕0 | 88∕105∕231∕0 | 0.756 |
| AJCC PM (MX/M1/M0/NA) | 47∕59∕312∕6 | 46∕58∕314∕6 | 0.998 |
| Radiation treatment adjuvant (Yes/No /NA) | 0∕33∕391 | 0∕42∕382 | 0.553 |
| Pharmaceutical adjuvant (Yes/No /NA) | 18∕15∕391 | 22∕20∕382 | 0.608 |
| History other malignance (Yes/No /NA) | 56∕368∕0 | 50∕374∕0 | 0.533 |
| AC005256.1 (High/Low) | 212/212 | 212/212 | 1.0 |
| RP11_815M8.1 (High/Low) | 212/212 | 219/205 | 0.631 |
| RP11_342A23.2 (High/Low) | 212/212 | 212/212 | 1.0 |
| RP11_264B14.1 (High/Low) | 212/212 | 196/228 | 0.272 |
| AC064834.1 (High/Low) | 212/212 | 215/209 | 0.837 |
| RP11_108K3.2 (High/Low) | 212/212 | 207/217 | 0.731 |
| LINC01571 (High/Low) | 212/212 | 206/218 | 0.680 |
| RP11_383I23.2 (High/Low) | 212/212 | 206/218 | 0.680 |
| AC079612.1 (High/Low) | 212/212 | 237/187 | 0.085 |
Notes.
Continuous variables were compared by t-test or Mann–Whitney U test as appropriate. Categorical variables were compared by chi-squared test or Fisher’s exact test as appropriate.
- NA
- missing data
- NR
- not reported
Differentially expressed analyses
We performed differential expression analyses by comparing all gene expression values between 458 tumor tissues and 41 normal colon tissues. The “edgeR” package identified 574 differentially expressed genes for overall survival. The heat map and volcano map of differential expression genes were presented in Figs. S1 and S2, respectively.
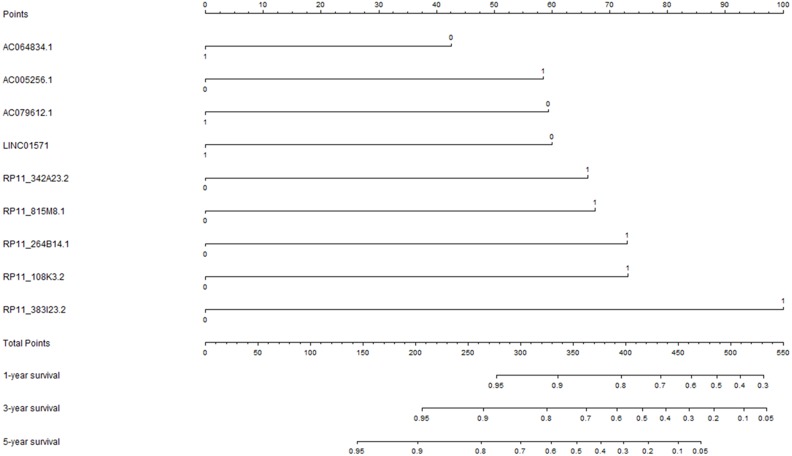
Construction of prognostic signature for overall survival
The univariate Cox regression analysis was performed to explore the potential prognostic lncRNAs for overall survival. The univariate Cox proportional regression analysis identified 33 potential lncRNA predictors for overall survival. Using multivariate Cox proportional regression analysis, a nine-lncRNA prognostic signature (Fig. 2) was constructed based on the potential prognostic lncRNA predictors determined by Cox regression analysis. The overall information of nine prognostic lncRNA predictors were summarized in Table 2. The formula of nine-lncRNA prognostic signature was as follows: nine-lncRNA prognostic signature score = (0.837* RP11_815M8.1) + (0.822* RP11_342A23.2) + (0.905* RP11_264B14.1) + (−0.529* AC064834.1) + (0.907* RP11_108K3.2) + (−0.745* LINC01571) + (1.241* RP11_383I23.2) + (−0.737* AC079612.1) + (0.725* AC005256.1).
Figure 2. The nine-lncRNA prognostic signature to predict the overall survival of colorectal cancer patients.
Table 2. The overall information of nine prognostic lncRNA predictors in univariate and multivariable Cox regression analyses.
| Univariate analysis | Multivariate analysis | ||||||
|---|---|---|---|---|---|---|---|
| HR | 95% CI | P-value | Coefficient | HR | 95% CI | P-value | |
| RP11_815M8.1 (High/Low) | 1.842 | 1.232–2.754 | 0.003 | 0.837 | 2.310 | 1.473–3.623 | <0.001 |
| RP11_342A23.2 (High/Low) | 1.580 | 1.063–2.347 | 0.024 | 0.822 | 2.276 | 1.490–3.477 | <0.001 |
| RP11_264B14.1 (High/Low) | 1.510 | 1.015–2.246 | 0.042 | 0.905 | 2.471 | 1.582–3.857 | <0.001 |
| AC064834.1 (High/Low) | 0.590 | 0.396–0.880 | 0.010 | −0.529 | 0.589 | 0.391–0.889 | 0.012 |
| RP11_108K3.2 (High/Low) | 2.552 | 1.659–3.927 | <0.001 | 0.907 | 2.478 | 1.592–3.855 | <0.001 |
| LINC01571 (High/Low) | 0.661 | 0.446–0.981 | 0.040 | −0.745 | 0.475 | 0.307–0.733 | <0.001 |
| RP11_383I23.2 (High/Low) | 1.667 | 1.117–2.487 | 0.012 | 1.241 | 3.459 | 2.143–5.583 | <0.001 |
| AC079612.1 (High/Low) | 0.450 | 0.297–0.681 | <0.001 | −0.737 | 0.479 | 0.314–0.731 | <0.001 |
| AC005256.1 (High/Low) | 1.606 | 1.080–2.387 | 0.019 | 0.725 | 2.065 | 1.352–3.155 | <0.001 |
Notes.
- HR
- hazard ratio
- CI
- confidence interval
The medians of lncRNA expression values were used as cutoff values to stratify lncRNA expression values into high expression group (as value 1) and low expression group (as value 0).
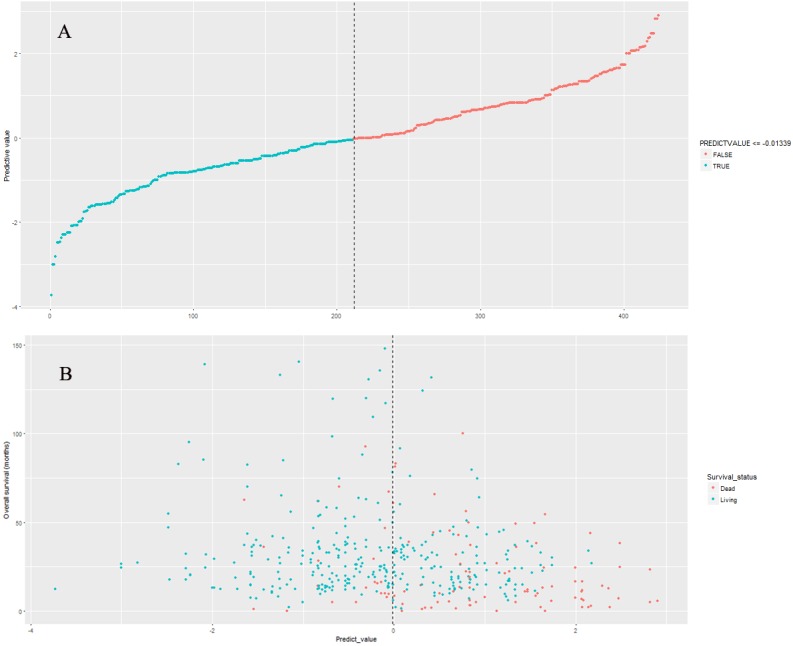
Performance of nine-lncRNA prognostic signature in model cohort
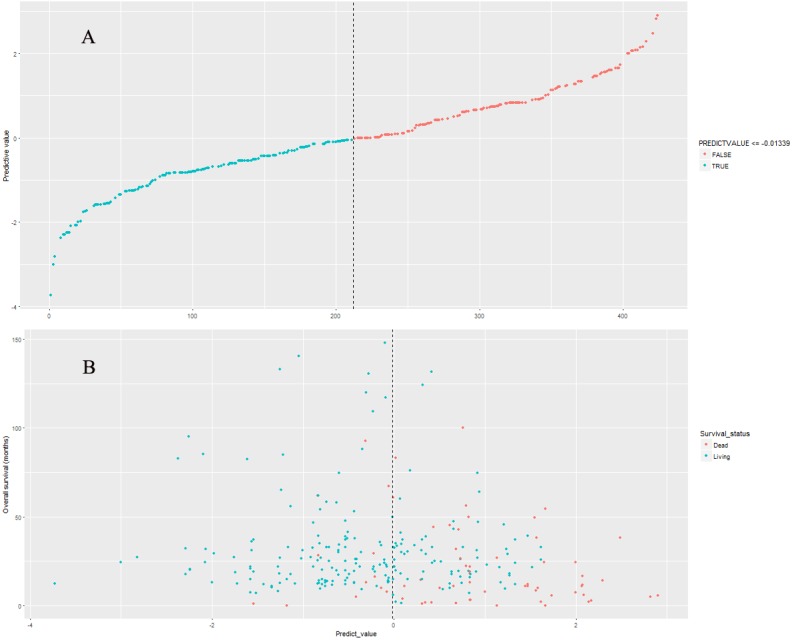
The nine-lncRNA prognostic signature score were generated according to the previous formula. The distributions of nine-lncRNA prognostic signature score (Fig. 3A), overall survival status and overall survival time (Fig. 3B) in model cohort were shown in Fig. 3. In model cohort, the Harrell’s concordance-index (C-index) of nine-lncRNA prognostic signature was 0.757 (95% CI [0.706–0.808]).
Figure 3. The distributions of nine-lncRNA prognostic signature (A), overall survival status and overall survival time (B) in model cohort.
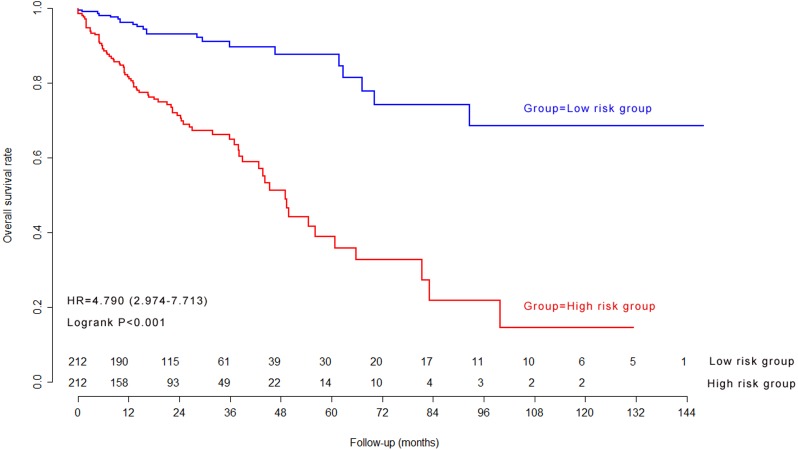
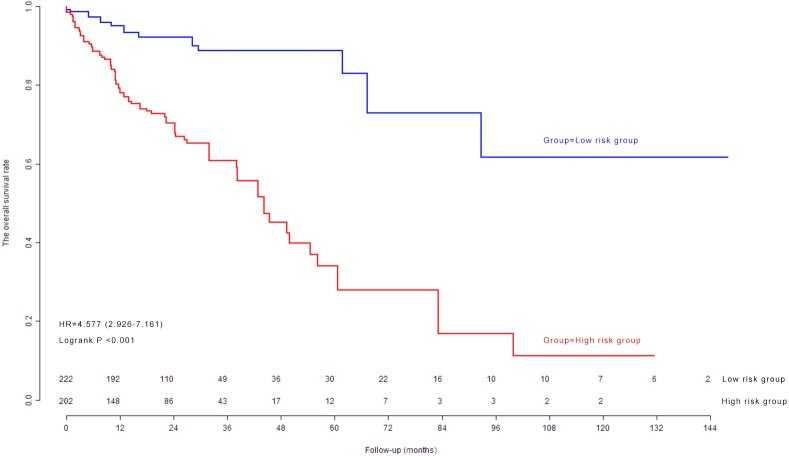
Kaplan–Meier survival curves and log-rank test in model cohort
The median of nine-lncRNA prognostic signature score was used as cutoff value to stratify CRC patients into high risk group and low risk group. Kaplan–Meier survival curves (Fig. 4) and log-rank test were used to compare the difference of overall survival rate between high risk group and low risk group. As shown in Fig. 4, patients with high nine-lncRNA prognostic signature score had poorer overall survival rate than patients with low nine-lncRNA prognostic signature score (P < 0.001).
Figure 4. The Kaplan–Meier survival curves in model cohort.
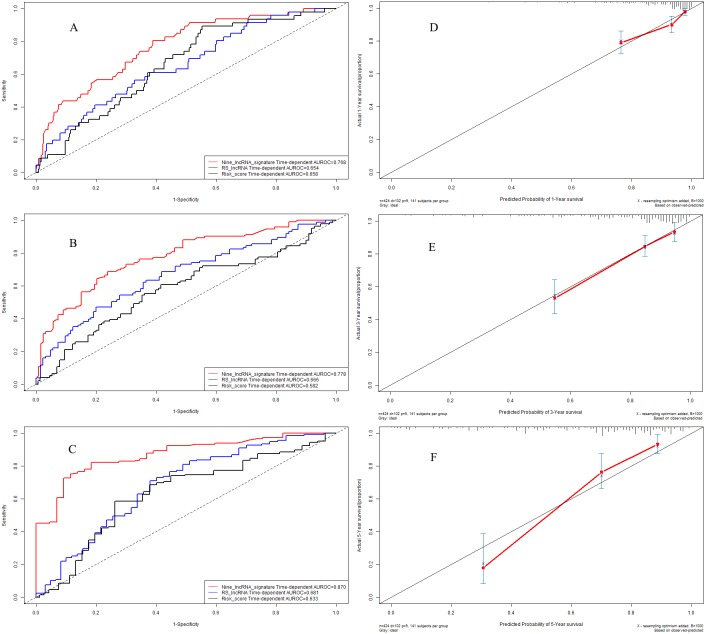
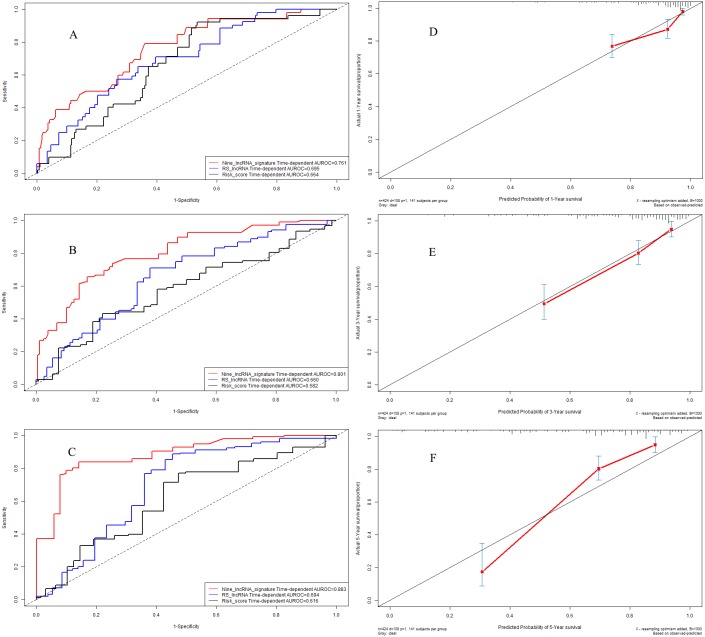
Time-dependent receiver operating characteristic curves in model cohort
We further explored the predictive accuracy of nine-lncRNA prognostic signature score compared with two previous prognostic signatures by using time-dependent receiver operating characteristic curves (Fig. 5). The C-indexes of nine-lncRNA prognostic signature, RS lncRNA score and Risk score were 0.768, 0.654 and 0.658 for 1-year overall survival (Fig. 5A) respectively, whereas it were 0.778, 0.666 and 0.582 for 3-year overall survival (Fig. 5B). For 5-year overall survival (Fig. 5C), the C-indexes of nine-lncRNA prognostic signature, RS lncRNA score and Risk score were 0.870,0.681 and 0.633, respectively.
Figure 5. Performance of nine-lncRNA prognostic signature in model cohort: Time-dependent receiver operating characteristic curves of three prognostic models according to 1-year (A), 3-year (B) and 5-year (C) overall survival. (D) Calibration curve for 1-year overall survival; (E) Calibration curve for 3-year overall survival; (F) Calibration curve for 5-year overall survival.
Calibration curves in model cohort
The calibration curves were used to assess the predictive performance of nine-lncRNA prognostic signature. The calibration curves for 1-year (Fig. 5D), 3-year (Fig. 5E) and 5-year (Fig. 5F) overall survival demonstrated that there were a good agreement between the predictive probability and the actual overall survival in model cohort.
Internal validation of nine-lncRNA prognostic signature
The validation cohort (n = 424) was generated by random drawing from the model cohort with replacement method. The nine-lncRNA prognostic signature score were generated according to the previous formula for patients in validation cohort. The distributions of nine-lncRNA prognostic signature score (Fig. 6A), overall survival status and overall survival time (Fig. 6B) in validation cohort were shown in Fig. 6. The C-index of nine-lncRNA prognostic signature was 0.751 95% CI [0.700–0.802]) in validation cohort.
Figure 6. The distributions of nine-lncRNA prognostic signature (A), overall survival status and overall survival time (B) in validation cohort.
Kaplan–Meier survival curves and log-rank test in validation cohort
The previous cutoff value of nine-lncRNA prognostic signature score in model cohort was used as the cutoff value to stratify CRC patients into high risk group and low risk group in validation cohort. As shown in Fig. 7, the log-rank test indicated that the overall survival rate in high risk group was significantly lower than that in low risk group (P < 0.001).
Figure 7. The Kaplan–Meier survival curves in validation cohort.
Time-dependent receiver operating characteristic curves in validation cohort
In validation cohort, the C-indexes of nine-lncRNA prognostic signature, RS lncRNA score and Risk score were 0.761, 0.695 and 0.664 for 1-year overall survival (Fig. 8A) respectively, whereas it were 0.801, 0.660 and 0.582 for 3-year overall survival (Fig. 8B). For 5-year overall survival (Fig. 8C), the C-indexes of nine-lncRNA prognostic signature, RS lncRNA score and Risk score were 0.883,0.694 and 0.616 respectively.
Figure 8. Performance of nine-lncRNA prognostic signature in validation cohort: Time-dependent receiver operating characteristic curves of three prognostic models according to 1-year (A), 3-year (B) and 5-year (C) overall survival. (D) Calibration curve for 1-year overall survival; (E) Calibration curve for 3-year overall survival; (F) Calibration curve for 5-year overall survival.
Calibration curves in validation cohort
The calibration curves for 1-year (Fig. 8D), 3-year (Fig. 8E) and 5-year (Fig. 8F) overall survival indicated a good agreement between the predictive probability of overall survival and the actual overall survival in validation cohort.
Independence of nine-lncRNA prognostic signature for overall survival
We further carried out multivariate Cox regression analyses to explore whether nine-lncRNA prognostic signature was an independent influence factor for overall survival in model cohort and validation cohort. After adjustment of other clinical variables, including age, gender, the American Joint Committee on Cancer (AJCC) PT, AJCC PN, AJCC PM and AJCC stage (Table 3), the results of multivariate Cox regression analysis indicated that the nine-lncRNA prognostic signature was an independent influence factor for overall survival of CRC patients.
Table 3. Univariate and multivariable Cox regression analyses.
| Univariate analysis | Multivariate analysis | |||||||
|---|---|---|---|---|---|---|---|---|
| n | HR | 95% CI | P-value | Coefficient | HR | 95% CI | P-value | |
| Model cohort (n = 424) | ||||||||
| Age(year) | 424 | 1.022 | 1.005–1.038 | 0.010 | 0.025 | 1.025 | 1.007–1.044 | 0.007 |
| Gender (Male/Female) | 424 | 1.112 | 0.752–1.645 | 0.595 | −0.101 | 0.904 | 0.595–1.373 | 0.636 |
| AJCC PT (T4,T3/T2,T1) | 424 | 2.926 | 1.356–6.318 | 0.006 | 1.161 | 3.193 | 1.248–8.165 | 0.015 |
| AJCC PN (N2,N1/N0) | 424 | 2.506 | 1.683–3.733 | <0.001 | −0.551 | 0.576 | 0.218–1.524 | 0.267 |
| AJCC PM (MX,M1/M0) | 418 | 2.962 | 1.985–4.419 | <0.001 | 0.707 | 2.029 | 1.284–3.205 | 0.002 |
| AJCC stage (IV,III/II,I) | 413 | 2.841 | 1.869–4.317 | <0.001 | 1.233 | 3.433 | 1.157–10.187 | 0.026 |
| Nine-lncRNA prognostic signature (High/Low) | 424 | 4.790 | 2.974–7.713 | <0.001 | 1.513 | 4.539 | 2.722–7.571 | <0.001 |
| Validation cohort (n = 424) | ||||||||
| Age(year) | 424 | 1.017 | 1.002–1.033 | 0.032 | 0.031 | 1.031 | 1.012–1.050 | 0.001 |
| Gender (Male/Female) | 424 | 1.051 | 0.720–1.535 | 0.797 | −0.213 | 0.808 | 0.538–1.214 | 0.306 |
| AJCC PT (T4,T3/T2,T1) | 424 | 8.353 | 2.646-26.368 | <0.001 | 3.079 | 21.729 | 2.988–158.025 | 0.002 |
| AJCC PN (N2,N1/N0) | 424 | 2.253 | 1.528–3.323 | <0.001 | −0.526 | 0.591 | 0.260–1.346 | 0.211 |
| AJCC PM (MX,M1/M0) | 418 | 2.347 | 1.577–3.493 | <0.001 | 0.570 | 1.769 | 1.107–2.827 | 0.017 |
| AJCC stage (IV,III/II,I) | 414 | 2.741 | 1.817–4.134 | <0.001 | 1.231 | 3.425 | 1.317–8.905 | 0.012 |
| Nine-lncRNA prognostic signature (High/Low) | 424 | 4.577 | 2.926–7.161 | <0.001 | 1.515 | 4.551 | 2.806–7.383 | <0.001 |
Notes.
- AJCC
- the American Joint Committee on Cancer
- HR
- hazard ratio
- CI
- confidence interval
The median of nine-lncRNA prognostic signature score was used as the cutoff value to stratify colorectal patients into high risk group and low risk group.
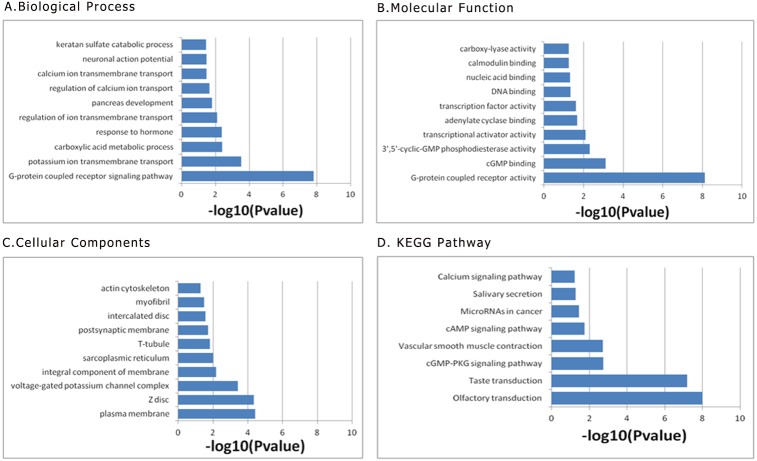
Functional enrichment analysis of prognostic signature
We performed functional enrichment analysis to explore the biological pathway and process correlated with this nine-lncRNA prognostic signature. At first, the pearson correlation coefficients between these prognostic lncRNA expression values and the mRNA expression values were calculated in the TCGA dataset. Then the genes correlated with at least one of these prognostic lncRNAs (defined as —Pearson correlation coefficient— >0.5) were included into the following functional enrichment analysis. The gene ontology (GO) biological process enrichment analysis and the Kyoto Encyclopedia of Genes and Genomes (KEGG) signaling pathway analysis were presented in Fig. 9 by using the above identified genes in the Database for Annotation, Visualization, and Integrated Discovery (DAVID) (https://david.ncifcrf.gov/) Bioinformatics Resources. The results of functional enrichment analysis demonstrated that the co-expressed genes were mainly enriched in G-protein coupled receptor signaling pathway, potassium ion transmembrane transport, carboxylic acid metabolic process response to hormone, regulation of ion transmembrane transport (Fig. 9).
Figure 9. Functional enrichment analysis of prognostic signature: (A) Biological Process; (B) Moleccular Function; (C) Cellular Component; (D) KEGG Pathway.
KEGG, Kyoto Encyclopedia of Genes and Genomes.
Discussion
In the present study, we developed and validated a nine-lncRNA prognostic signature that was helpful for individual mortality risk prediction and survival stratification of CRC patients. This nine-lncRNA prognostic signature was helpful for patients to ascertain their individual mortality risk and optimize their personalized treatment strategies. Time-dependent receiver operating characteristic curves demonstrated that this nine-lncRNA prognostic signature was superior to other two previous prognostic signatures for prediction of overall survival.
This nine-lncRNA prognostic signature without pathological parameters provided a noninvasive preoperative prediction method for overall survival of CRC patients. Firstly, this nine-lncRNA prognostic signature could provide a preoperative individual mortality risk prediction, which was helpful for patients without medical knowledge to understand the actual individual mortality risk in different clinical endpoints. Secondly, the median of nine-lncRNA prognostic signature score was used as the cutoff value to stratify colorectal patients into high risk group and low risk group. The Kaplan–Meier survival curves demonstrated that the overall survival rate in high risk group was significantly lower than that in low risk group. Therefore, this nine-lncRNA prognostic signature was helpful for patients with high mortality risk to make clinical decision of receiving active individualized treatment.
As reported in the original article, the AUROCs of Risk score for 5-year overall survival were 0.706 and 0.619 in model group and validation group respectively (Zeng et al., 2017). The AUROCs of RS lncRNA score were 0.731 and 0.727 in training dataset and testing dataset (Fan & Liu, 2018). The AUROCs of Risk score and RS lncRNA score in the present study were lower than that in original articles. The differences of AUROC might be caused by the following reasons: firstly, the sample size in the present study was 424, whereas it were 371 for Risk score and 568 for RS lncRNA score. The difference of sample size would result in an influence to the predictive accuracy of prognostic models. Secondly, the numbers of selected lncRNAs were different in three prognostic signatures. The number of selected lncRNAs in nine-lncRNA prognostic signature was nine, whereas it was four for the Risk score and six for the RS lncRNA score. Thirdly, the Risk score was calculated by using the lncRNA expression values which have been log2-transformed. The RS lncRNA score was calculated by using the lncRNA expression values which have been normalized by the “DEseq” package. In order to improve the universal applicability of the research results, the medians of original lncRNA expression values were used as cutoff values to stratify lncRNA expression values into high expression group (as value 1) and low expression group (as value 0) in the present study. The nine-lncRNA prognostic signature score were calculated by using the binary lncRNA expression values according to the medians of original lncRNA expression values. This adjustment was helpful to improve the clinical application of prognostic model in other study population.
The present study has the following advantages: first, this nine-lncRNA prognostic signature can be used to assess the individual mortality risk through simple chart by patients. Second, this nine-lncRNA prognostic signature can provide an individual mortality risk assessment for 1-year, 3-year and 5-year overall survival. Individual mortality risk prediction at different time points is of great significance to persuade CRC patients receive a timely differentiated intensive treatment. Third, this nine-lncRNA prognostic signature provides individual mortality risk probability and the result is easy to understand for patients without medical knowledge. Fourth, this nine-lncRNA prognostic signature can serve as a preoperative non-invasive prediction method for overall survival of CRC patients. Therefore, this nine-lncRNA prognostic signature is suitable for preoperative prediction of overall survival, especially for advanced CRC patients who can’t tolerate surgery.
The current study has two shortcomings which must be considered for interpreting the clinical significance of the results. First, the current study constructed a prognostic signature by using nine lncRNA predictors. However, due to the different gene detection platforms and different lncRNA name, we could not obtain second independent dataset containing these nine lncRNA predictors in other databases including Gene Expression Omnibus (GEO) database, ArrayExpress database, and The Atlas of Noncoding RNAs in Cancer (TANRIC). We performed an internal validation by using bootstrap resampling method but not external validation by using independent data. Therefore, this nine-lncRNA prognostic signature in the current study need further external validation through external independent dataset. Second, we searched TCGA database and ascertained nine lncRNAs as prognostic predictors for overall survival in CRC patients. The relationship between these lncRNA predictors and the prognosis of CRC patients was not clear. Third, the average follow-up time was 30.0 ± 25.5 months and there were only 102 (24.0%) patients died during the follow-up period in model cohort. Taking into account the limited follow-up time and relatively small event size, the association between these lncRNA predictors and the prognosis of CRC patients should be validated in an additional cohort with longer follow-up period and larger event size. Therefore, large prospective clinical studies are needed to clarify the relationship between these lncRNA predictors and the prognosis of CRC patients.
Conclusions
In summary, the present study developed and validated a nine-lncRNA prognostic signature for individual mortality risk assessment in colorectal cancer patients. This nine-lncRNA prognostic signature is helpful to determine the individual mortality risk of overall survival and to improve the decision making of individualized treatments in colorectal cancer patients.
Supplemental Information
Abbreviations
- CRC
Colorectal cancer
- AUC
Area under the ROC curve
- OS
Overall survival
- ROC
Receiver operating characteristic curve
- LncRNA
Long non-coding RNA
- TCGA
The Cancer Genome Atlas
- RPKM
Reads per kilobase per million mapped reads
- TMM
Trimmed Mean of M
- AJCC
American Joint Committee on Cancer
- HR
Hazard ratio
- CI
Confidence interval
- GO
gene ontology
- KEGG
Kyoto Encyclopedia of Genes and Genomes
- DAVID
Database for Annotation, Visualization, and Integrated Discovery
Funding Statement
This study was supported by the Guangdong Provincial Health Department and the Guangdong Provincial Financial Department. The grant numbers were: B2018237 (grant recipient: Zhiqiao Zhang) and A2016450 (grant recipient: Zhiqiao Zhang). The total capital was RMB 15000. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Additional Information and Declarations
Competing Interests
The authors declare there are no competing interests.
Author Contributions
Zhiqiao Zhang conceived and designed the experiments, performed the experiments, analyzed the data, contributed reagents/materials/analysis tools, prepared figures and/or tables, authored or reviewed drafts of the paper, approved the final draft.
Qingbo Liu conceived and designed the experiments, performed the experiments, analyzed the data, prepared figures and/or tables, authored or reviewed drafts of the paper, approved the final draft.
Peng Wang conceived and designed the experiments, prepared figures and/or tables, authored or reviewed drafts of the paper, approved the final draft.
Jing Li contributed reagents/materials/analysis tools, authored or reviewed drafts of the paper, approved the final draft.
Tingshan He approved the final draft.
Yanling Ouyang and Weidong Wang performed the experiments, analyzed the data, approved the final draft.
Yiyan Huang contributed reagents/materials/analysis tools, approved the final draft.
Human Ethics
The following information was supplied relating to ethical approvals (i.e., approving body and any reference numbers):
The data download and analyses were performed according to the policies of The Cancer Genome Atlas (TCGA) database. Since the study datasets in the present study were all downloaded from TCGA database, additional ethics approval was not needed. All data collections and analyses were in accordance with the principles of Declaration of Helsinki.
Data Availability
The following information was supplied regarding data availability:
All relevant data have been provided in the Supplemental Files.
References
- Blackstone (2001).Blackstone EH. Breaking down barriers: helpful breakthrough statistical methods you need to understand better. Journal of Thoracic and Cardiovascular Surgery. 2001;122:430–439. doi: 10.1067/mtc.2001.117536. [DOI] [PubMed] [Google Scholar]
- Collins et al. (2015).Collins GS, Reitsma JB, Altman DG, Moons KG. Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): the TRIPOD statement. British Journal of Surgery. 2015;102:148–158. doi: 10.1002/bjs.9736. [DOI] [PubMed] [Google Scholar]
- Derrien et al. (2012).Derrien T, Johnson R, Bussotti G, Tanzer A, Djebali S, Tilgner H, Guernec G, Martin D, Merkel A, Knowles DG, Lagarde J, Veeravalli L, Ruan X, Ruan Y, Lassmann T, Carninci P, Brown JB, Lipovich L, Gonzalez JM, Thomas M, Davis CA, Shiekhattar R, Gingeras TR, Hubbard TJ, Notredame C, Harrow J, Guigo R. The GENCODE v7 catalog of human long noncoding RNAs: analysis of their gene structure, evolution, and expression. Genome Research. 2012;22:1775–1789. doi: 10.1101/gr.132159.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fan & Liu (2018).Fan Q, Liu B. Discovery of a novel six-long non-coding RNA signature predicting survival of colorectal cancer patients. Journal of Cellular Biochemistry. 2018;119:3574–3585. doi: 10.1002/jcb.26548. [DOI] [PubMed] [Google Scholar]
- Ferlay et al. (2010).Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. International Journal of Cancer. 2010;127:2893–2917. doi: 10.1002/ijc.25516. [DOI] [PubMed] [Google Scholar]
- Grunkemeier & Wu (2004).Grunkemeier GL, Wu Y. Bootstrap resampling methods: something for nothing? Annals of Thoracic Surgery. 2004;77:1142–1144. doi: 10.1016/j.athoracsur.2004.01.005. [DOI] [PubMed] [Google Scholar]
- Kita et al. (2017).Kita Y, Yonemori K, Osako Y, Baba K, Mori S, Maemura K, Natsugoe S. Noncoding RNA and colorectal cancer: its epigenetic role. Journal of Human Genetics. 2017;62:41–47. doi: 10.1038/jhg.2016.66. [DOI] [PubMed] [Google Scholar]
- Li et al. (2015).Li Y, Xia Y, Li J, Wu D, Wan X, Wang K, Wu M, Liu J, Lau WY, Shen F. Prognostic nomograms for pre- and postoperative predictions of long-term survival for patients who underwent liver resection for huge hepatocellular carcinoma. Journal of the American College of Surgeons. 2015;221:962–974. doi: 10.1016/j.jamcollsurg.2015.08.003. [DOI] [PubMed] [Google Scholar]
- McFadden & Hargrove (2016).McFadden EJ, Hargrove AE. Biochemical methods to investigate lncRNA and the influence of lncRNA: protein complexes on chromatin. Biochemistry. 2016;55:1615–1630. doi: 10.1021/acs.biochem.5b01141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson & Oshlack (2010).Robinson MD, Oshlack A. A scaling normalization method for differential expression analysis of RNA-seq data. Genome Biology. 2010;11:R25. doi: 10.1186/gb-2010-11-3-r25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanoff et al. (2008).Sanoff HK, Sargent DJ, Campbell ME, Morton RF, Fuchs CS, Ramanathan RK, Williamson SK, Findlay BP, Pitot HC, Goldberg RM. Five-year data and prognostic factor analysis of oxaliplatin and irinotecan combinations for advanced colorectal cancer: N9741. Journal of Clinical Oncology. 2008;26:5721–5727. doi: 10.1200/jco.2008.17.7147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siegel et al. (2017).Siegel RL, Miller KD, Fedewa SA, Ahnen DJ, Meester RGS, Barzi A, Jemal A. Colorectal cancer statistics, 2017. CA: A Cancer Journal for Clinicians. 2017;67:177–193. doi: 10.3322/caac.21395. [DOI] [PubMed] [Google Scholar]
- Siegel, Miller & Jemal (2016).Siegel RL, Miller KD, Jemal A. Cancer statistics, 2016. CA: A Cancer Journal for Clinicians. 2016;66:7–30. doi: 10.3322/caac.21332. [DOI] [PubMed] [Google Scholar]
- Tian et al. (2017).Tian X, Zhu X, Yan T, Yu C, Shen C, Hong J, Chen H, Fang JY. Differentially expressed lncRNAs in gastric cancer patients: a potential biomarker for gastric cancer prognosis. Journal of Cancer. 2017;8:2575–2586. doi: 10.7150/jca.19980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weng et al. (2017).Weng M, Wu D, Yang C, Peng H, Wang G, Wang T, Li X. Noncoding RNAs in the development, diagnosis, and prognosis of colorectal cancer. Translational Research. 2017;181:108–120. doi: 10.1016/j.trsl.2016.10.001. [DOI] [PubMed] [Google Scholar]
- Xie et al. (2016).Xie X, Tang B, Xiao YF, Xie R, Li BS, Dong H, Zhou JY, Yang SM. Long non-coding RNAs in colorectal cancer. Oncotarget. 2016;7:5226–5239. doi: 10.18632/oncotarget.6446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xing et al. (2018).Xing Y, Zhao Z, Zhu Y, Zhao L, Zhu A, Piao D. Comprehensive analysis of differential expression profiles of mRNAs and lncRNAs and identification of a 14-lncRNA prognostic signature for patients with colon adenocarcinoma. Oncology Reports. 2018;39:2365–2375. doi: 10.3892/or.2018.6324. [DOI] [PubMed] [Google Scholar]
- Xue et al. (2017).Xue W, Li J, Wang F, Han P, Liu Y, Cui B. A long non-coding RNA expression signature to predict survival of patients with colon adenocarcinoma. Oncotarget. 2017;8:101298–101308. doi: 10.18632/oncotarget.21064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeng et al. (2017).Zeng JH, Liang L, He RQ, Tang RX, Cai XY, Chen JQ, Luo DZ, Chen G. Comprehensive investigation of a novel differentially expressed lncRNA expression profile signature to assess the survival of patients with colorectal adenocarcinoma. Oncotarget. 2017;8:16811–16828. doi: 10.18632/oncotarget.15161. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The following information was supplied regarding data availability:
All relevant data have been provided in the Supplemental Files.