Abstract
Introduction:
Multiple cadaver and radiographic analyses have been performed to define the surgical anatomy of the sacrum and pelvis. We provide a comprehensive review of this information, creating an accurate anatomic guide for practice and research.
Methods:
A systematic review was performed to identify publications citing sacral or iliac morphometric parameters based on cadaver or radiographic anatomy.
Results:
A total of 780 abstracts were evaluated. Fifty-six articles were included for final review and grouped into four sections: (1) bone density, (2) bony corridors, (3) screw length and trajectory, and (4) neurovascular and alimentary anatomy.
Conclusion:
A systematic analysis of the radiographic and gross anatomic features of the sacrum has yet to be published. This review includes details on the spatial arrangement of the S1 and S2 pedicle screws, sacroiliac screws, iliac screws, S2 alar iliac screws, and pelvic neurovascular anatomy. The study can be referenced by clinicians for sacral dissection, implant application, and ongoing advances in orthopaedic research.
Study Design:
Systematic review
Level of Evidence:
Level IV
The sacral bone is an inverted triangle that sits obliquely between the two innominate bones of the pelvis at the distal aspect of the spinal column. It functions mechanically to convey axial load from the lumbar spine into the lower extremities for balanced locomotion. The ventral sacral body is concave and derived from five vertebrae. The transverse processes of the sacral vertebrae coalesce to form the sacral ala, which projects laterally from the upper sacral promontory.
The dorsal surface of the sacral bone is formed from the coalescence of the spinous processes, zygapophyseal joints, and the laminae of the sacral vertebrae. The sacral body serves as a protective conduit for the cauda equina, which typically ends at the S2 vertebrae. Between the central sacral body and the lateral sacral lamina are the four ventral and dorsal foramina that transmit the sacral nerve roots out of the sacral canal. A rich network of neurovascular structures surrounds the sacrum and poses intraoperative dangers during sacropelvic osteosynthesis.
Increasingly sophisticated techniques for sacral instrumentation require a detailed surgical knowledge to maintain patient safety. A concise anatomic review of surgically relevant data has yet to be published; our goal was to collate morphometric references for surgical instrumentation.
Methods
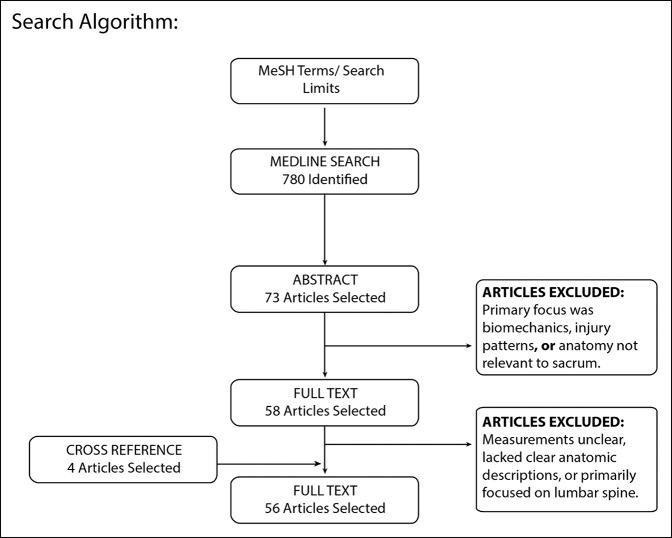
Our methods were developed following the Cochrane Collaboration guidelines. In August 2016, we performed a search using Medical Subject Headings terms and Boolean operators to identify English language publications in the PubMed database referencing sacral or iliac anatomic parameters based on cadaver or radiographic anatomy (Figure 1, Supplemental Digital Content 1, http://links.lww.com/JG9/A23). Two independent investigators reviewed and classified study titles, abstracts, and full-text articles based on inclusion and exclusion criteria (Supplemental Digital Content 1, http://links.lww.com/JG9/A23). Full-length studies were analyzed according to the anatomic area (eg, S1 pedicle), and numerical morphometric measurements were documented and rounded to the nearest whole number. A manual cross-reference review was performed on bibliographies of all selected articles to further identify sources. Articles were included based on a consensus between reviewers, and disagreements were resolved by a third party with ultimate jurisdiction on inclusion. Articles were grouped categorically into bone density, screw length and trajectory, bony corridors, or neurovascular/alimentary anatomy.
Figure 1.
Flowchart showing the search algorithm. MeSH = Medical Subject Headings
Results
Our search yielded 780 relevant abstracts, 58 of which were selected for full review. Fifty-two publications met final inclusion criteria with four additional publications included based on the citations of the fully reviewed articles.
Bone Density
Investigators have studied the internal architecture of the sacrum to identify areas of increased bone density for improved screw purchase. Ebraheim and colleagues1,2 revealed that the anterior aspect of the S1 body possessed better bone stock than the caudal areas of the sacrum or ala. Moreover, analysis of Hounsfield units on separate CT study revealed that the S1 segment has greater density than the S2 segment (A difference on average of 89 HU).3 In general, bone density decreases at successive levels of the sacrum, and thicker cortices tend to be anteromedial. Thus, the best fixation bone stock for screw thread purchase is likely at the anteromedial aspect of the S1 segment.
Screw Length and Trajectory
The following is a summary of available data averages to guide sacral screw insertion from several entry points. Patients may have variable anatomy that is not reflected accurately in population averages, making preoperative and intraoperative imaging crucial for safety.
S1 Pedicle Screw
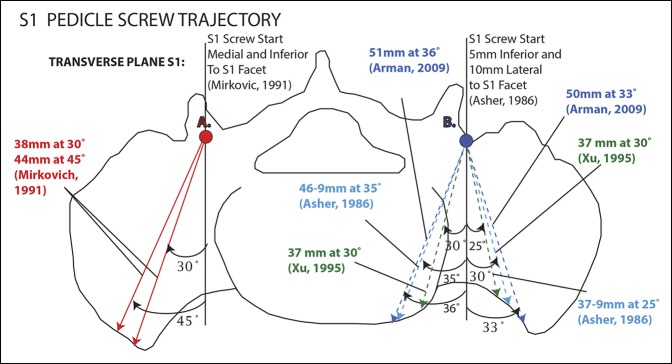
The S1 pedicle screw has three potential trajectories: (1) anterolateral into the ala, (2) anterior into the junction of the sacral ala and vertebral body, or (3) anteromedial into the promontory.4,5 Distinct from the thoracolumbar pedicles, the sacral pedicle has no well-defined cortical ring.5 The trajectories of the anteromedial and anterolateral S1 screws have been reported as either 30° medial into the pedicle or 45° to 50° lateral into the sacral ala. All trajectories use a 10°- to 20°-caudal tilt in the sagittal plane.6 The anterior trajectory is reportedly least desirable because this path provides the shortest length of the three options, at an average measurement of 30 mm.
The anteromedial trajectory generally starts 5 to 10 mm caudal and 10 mm lateral to the superior articular facet of S1. The angulation may be from 10° to 20° cephalad in reference to the sacral lamina and 23° to 35° medial from the sagittal plane. The average screw length using this trajectory is 37 to 51 mm.4,7-9 The surgical approach may determine the insertional angle; wide lateral approaches may afford longer trajectories.10 Overall, the anteromedial trajectory is preferred because of increased biomechanical strength from convergence of the screws and better bony support.10-12
The anterolateral trajectory entry starts from the same point as the anteromedial screw but may be more medial, and it is directed 25° to 53° laterally from the sagittal plane. The anterolateral trajectory screw lengths, on average, are reported to range from 37 to 46 mm4,7,8,9,10 (Figure 2, Supplemental Digital Content 2, http://links.lww.com/JG9/A23).
Figure 2.
Illustration showing S1 pedicle screw trajectories.
S2 Pedicle Screw
Similar to the S1 screw trajectory, the S2 pedicle screw has two main paths: anteromedial and anterolateral. A straight anterior approach, to our knowledge, has not been studied anatomically. The starting point is generally in a trough between the sacral lamina and the lateral sacral ala. The point is located at the junction of the proximal and middle one-third of the distance between the S1 and S2 dorsal foramina. This screw is directed either 30° medially or 30° laterally and parallel to the S1 end plate. The average length of either trajectory was 30 to 34 mm.7,8,13 (Supplemental Digital Content 2, http://links.lww.com/JG9/A23).
Iliac Screw
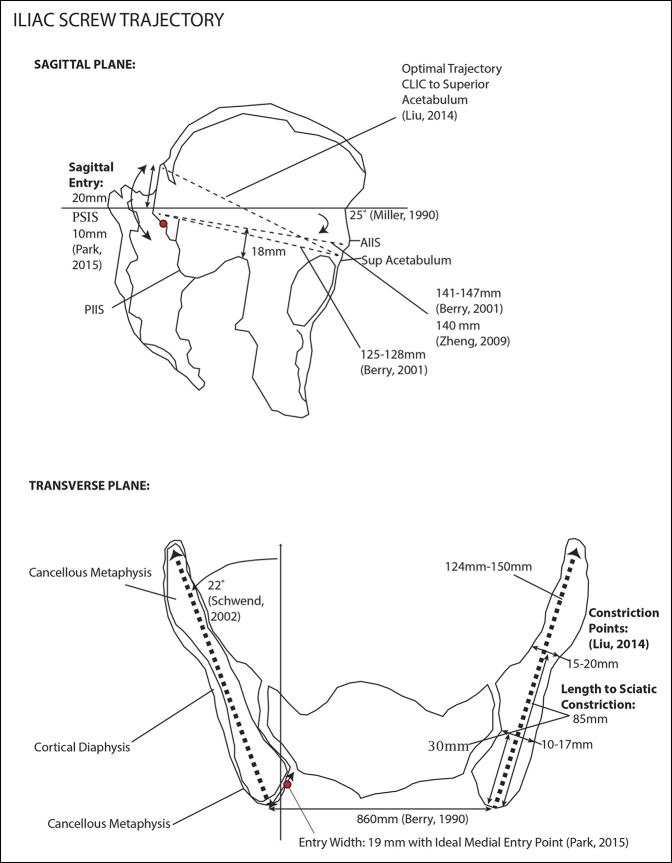
Iliac fixation (ie, iliac screw and iliac bolt) was the original lumbopelvic fixation technique to support S1-L5 instrumentation. It was first proposed by Allen and Ferguson14 in the form of the Galveston supra-acetabular intrailiac implant—a contoured rod directly inserted into the pelvis. Modern techniques use large-diameter screws that connect to a cranial rod construct. The main advantages of this technique over S2 alar iliac (S2AI) screws (described below) are that iliac screws are contained within the ilium and avoid violation of the sacroiliac (SI) joint. Iliac screws are typically directed from the posterior superior iliac spine (PSIS) to the anterior inferior iliac spine (AIIS), which has been shown to maximize the length.15,16
CT studies show the ideal entry point of the iliac screw, to obtain the most length and to minimize perforations, should be within the medial portion of a zone 20 mm cranial and 10 mm caudal of the PSIS.17,18 The trajectory is 22° lateral in the transverse plane and 25° caudal in the sagittal plane.16,18,19 The average length of this screw has been reported as 124 to 150 mm.15,18,19,20,21
The risks of using the iliac screw technique include violation of the greater sciatic notch and the acetabulum through inferior penetration. Caudal start points put the acetabulum at a greater risk, whereas caudal end points put the sciatic notch at a greater risk.15,20 In the transverse section of the screw path, there are two narrow constriction points where the screw may breach21 (Figure 3, Supplemental Digital Content 3, http://links.lww.com/JG9/A23).
Figure 3.
Illustration showing the iliac screw passage. AIIS = anterior inferior iliac spine, PSIS = posterior superior iliac spine
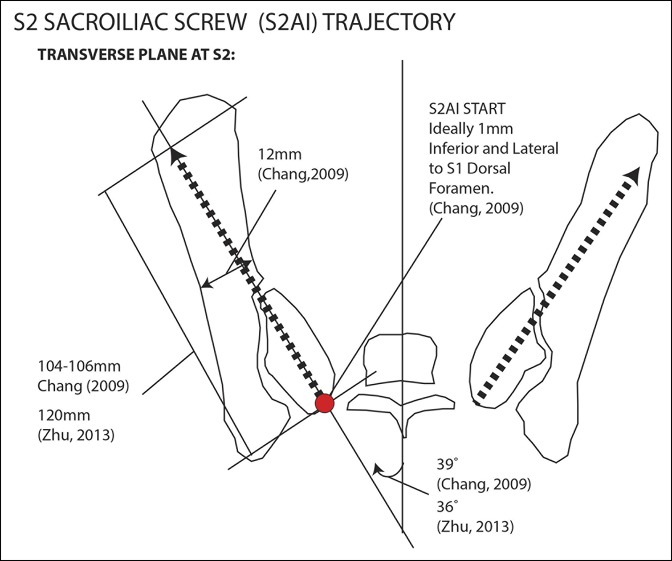
S2 Alar Iliac Screw
The S2 alar screw (S2AI or S2 Iliac technique) is a lumbopelvic fixation technique that uses a lateral S2 pedicle screw trajectory through the sacrum and into the ilium. Initially proposed by Chang et al,22 the S2AI technique has several advantages over pure iliac screw fixation. Compared with iliac screws, it is less prominent, requires less soft-tissue dissection, and is in line with cranial anchor points. In addition, this technique does not disrupt the posterior iliac crest, which may be used for bone grafting.
The starting point for the S2AI screw is 1 mm lateral and inferior to the S1 dorsal foramen. The trajectory is 36° to 40° lateral and 26° to 38° caudal from horizontal.22,23 The average length for this screw was 104 to 120 mm22,23 (Figure 4, Supplemental Digital Content 4, http://links.lww.com/JG9/A23). The screw passes through the SI joint, typically at 35 mm of the total insertional length. It also passes through a constriction point in the ilium, which measures on average 12 mm in diameter.22 Ethnicity of the patient may influence the trajectories and screw lengths.23 Ideally, the S2AI screw passes through a nonarticular portion of the SI joint, but in clinical practice, many S2AI screws will traverse the articular cartilage. In addition, the screw may breach the posterior iliac cortex, but generally, without complication24 (Figure 4, Supplemental Digital Content 3, http://links.lww.com/JG9/A23).
Figure 4.
Illustration showing the S2AI screw. S2AI = S2 alar iliac
Sacroiliac Screw
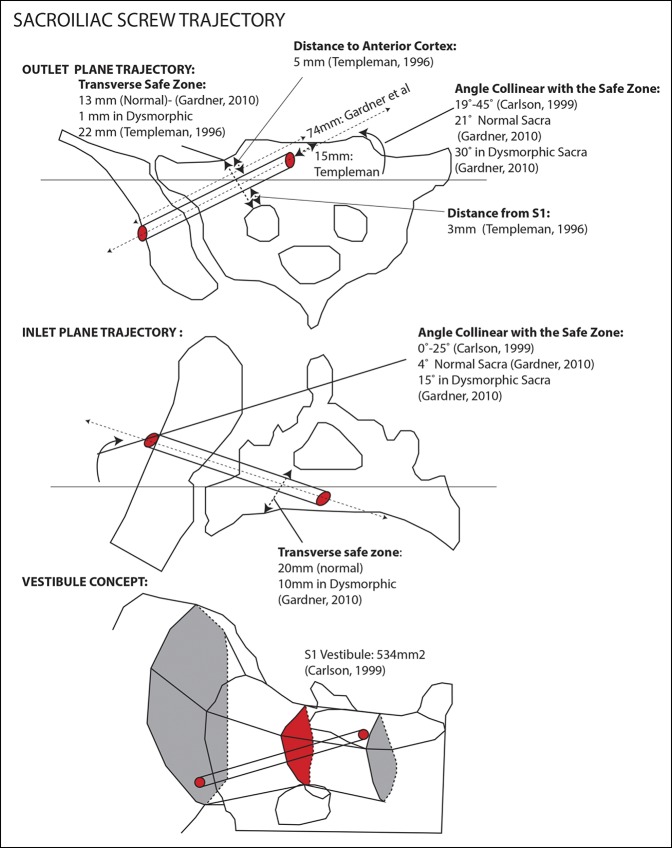
Iliosacral screws are used in the stabilization of pelvic ring injuries and use a corridor of bone through the ilium, SI joint, sacral ala, and into the sacral promontory.25 Carlson et al27 described the “sacral vestibule,” which is the key concept for appropriate iliosacral screw placement. It denotes the smallest corridor of alar bone through which an iliosacral screw passes as it transverses from the lateral ilium into the sacral body. The vestibule is ovoid in shape, approximately 5.34 cm2 in diameter, and perpendicular to an axis in the anterior superior plane.25-27 The vestibule is bounded by the sacral foramen (S1 nerve root) inferiorly and the alar slope (L5 nerve root) superiorly, and thus, represents the entrance into the S1 vertebral body. Expanding from the vestibule are two cones of bone—the vertebral body toward the midline and the ala and ilium laterally.26,28
The starting point for the SI screw, originally defined by Matta and Saucedo,29 is 15 mm anterior to the crista glutes at a point 50% of the distance between the greater sciatic notch and the iliac crest. Other authors have described the starting point on the outer table of the ilium 3 cm anterior to the PSIS and 4 cm cephalad to the greater sciatic notch.30 Radiographically, the starting point is located at the inferior aspect of S1 foramen and posterior to iliac cortical density, which represents the anterior-most aspect of the sacral ala.26,31 The screw length on average is 75 to 90 mm.26,27,30
The anatomy of SI screw placement is complicated by a spectrum of dysmorphic features, which occur at a relatively high incidence of 20% to 40%. Sacral dysmorphism is defined by variations in the normal sacral anatomy such as angulated upsloping ala and incomplete upper sacral segment disc space.27 A dysmorphic sacrum has surgical implications for SI screw placement. Gardner et al27 reported that the dysmorphic sacrum has a vestibule 36% smaller than normal (222 versus 346 mm2). The authors concluded that the SI screw trajectory in the dysmorphic sacrum was more oblique. The trajectory angle collinear with the safe zone measured on a coronal outlet reformat CT as 21° from horizontal in normal sacra and 30° in dysmorphic sacra. In the inlet plane, the angle collinear with the safe zone was 4° in normal sacra and 15° in dysmorphic sacra. Careful study of preoperative CT scans is imperative for safe placement of SI screws in patients with a dysmorphic sacrum.
Neurovascular structures are at risk with placement of SI screws. This includes the L5 nerve root crossing over the sacral ala and the S1 nerve root passing through the S1 foramen. Templeman et al32 found that the average distance of intraoperative screw placement from the S1 foramen was 3 mm with five screws appearing to enter the S1 foramen. The average distance from the sacral alar cortex to the screw was 5 mm with one screw penetrating the anterior cortex and reentering the sacral body. The superior gluteal neurovascular bundle, on the outer face of the ilium, may also be injured with percutaneous inserted SI screws and may be impaled in <18% of cases33 (Figures 5 and 6, Supplemental Digital Content 6, http://links.lww.com/JG9/A23).
Figure 5.
Illustration showing the sacroiliac screw trajectory.
Figure 6.
Illustration showing anatomic measurements of bony corridors within the sacrum.
Bony Corridors
Iliac Column
The iliac column is a corridor of bone bounded anteriorly by the AIIS and posteriorly by the PSIS. Inferiorly, it is limited by the sciatic notch and the acetabulum. Superiorly, it is bounded by the iliac wing and the iliac fossa.19
The iliac column is composed of a diaphyseal cortical center and metaphyseal cancellous bone at the anterior and posterior projections (AIIS and PSIS). There are two constriction points in the iliac column for iliac screw passage occurring on average at 30 and 85 mm from posterior to anterior.34 The first constriction point occurs above the SI joint and is 15 to 23 mm wide and 32 mm in height.15,19,20 The second constriction point occurs 22 mm above the sciatic notch15 and is 19 to 22 mm wide15,20 (Figure 3).
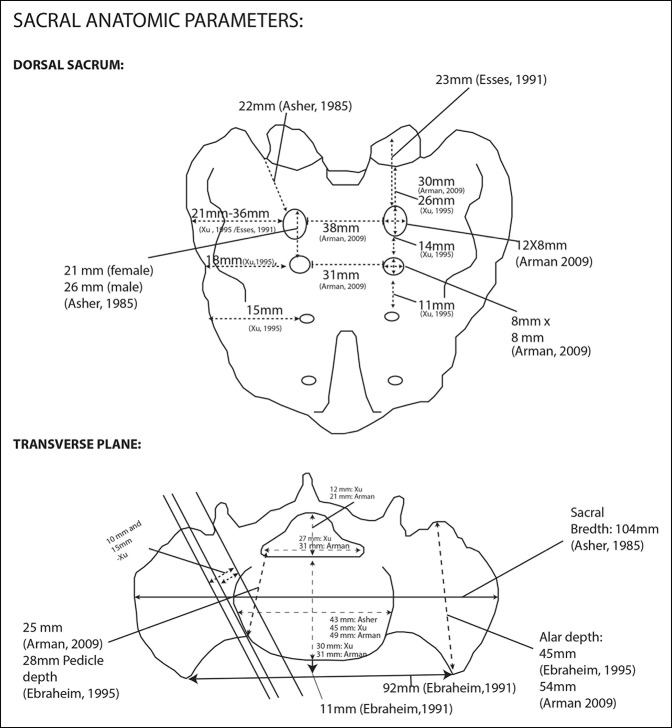
Sacral Pedicles
The sacral pedicles are defined as the area between the lateral edge of the sacral foramina and the lateral edge of the superior articular facet.8 Several authors have measured the height of the S1 sacral pedicle (interforaminal distance); it averages from 21 to 26 mm.4,30 The heights of the S2 and S3 pedicles are, on average, 14 and 11 mm, respectively.8 The width from the lateral edge of the facet to the lateral edge of the vertebral body averages 10 mm.35
Sacral Ala
The sacral ala is defined as the bone lateral to the sacral pedicle and averages 21, 18, and 15 mm wide on the dorsal surface of S1, S2, and S3, respectively.8 At the midpoint of the bone on the axial plane from anterior to posterior, the sacral ala measures 27 to 29 mm from medial to lateral.36
S1 Vertebral Body
The S1 segment is unique in that it has a large central anterior convex border known as the sacral promontory.37 The S1 vertebral body measures 30 to 31 mm in the AP dimension and 43 to 49 mm in the transverse dimension.4,7,35
S1 Sacral Canal
At the S1 level, the sacral canal is triangular in shape.37 It is connected through intervertebral foramina to both the ventral and dorsal foramina. The sacral canal width is 27 to 31 mm, and the AP distance is 12 to 21 mm.4,35
Dorsal Sacrum
The dorsal surface of the sacrum is convex and consists of a raised sacral crest formed in an interrupted fashion from the fusion of the spinous processes. Most commonly, flanking the crest are four pairs of sacral tubercles, which lead down to the caudal opening, the sacral hiatus.37 Lateral to the sacral crest are the fused sacral laminae, which form a plate medial to the dorsal foramina. They are the insertion point for the SI ligaments. Lateral to the sacral foramina are the intermediate sacral crests and sacral ala, which are formed from the fusion of the transverse processes. The sacrum generally contains four dorsal foramina.37 The dorsal foramina contain cutaneous nerves and are much smaller than the ventral foramina.37 Compared with the ventral foramina, dorsal foramina are more medial and course from central to lateral and open dorsally.38 The first sacral foramina are located 22 to 23 mm from the cranial limit of the sacrum and 37 mm from the lateral limit.7,38 They are 12 mm in height and 8 mm in width. The transverse diameter between the S1 foramina averages 38 mm.4
Ventral Sacrum
The ventral surface of the sacrum is concave. Four corresponding sacral foramina serve as conduits for the ventral sacral rami, which carry both motor and sensory function. The foramina run in a posteromedial-to-anterolateral and a superior-to-inferior direction to exit the ventral sacral surface 10 to 15 mm from their origin.37 Between each ventral foramen is a transverse ridge remnant of the fused intervertebral disc.38 The first ventral sacral foramina are located 23 mm from the superior aspect and 23 mm from the lateral aspect of the sacrum.38 (Figure 6, Supplemental Digital Content 7, http://links.lww.com/JG9/A23).
Neurovascular and Alimentary Anatomy
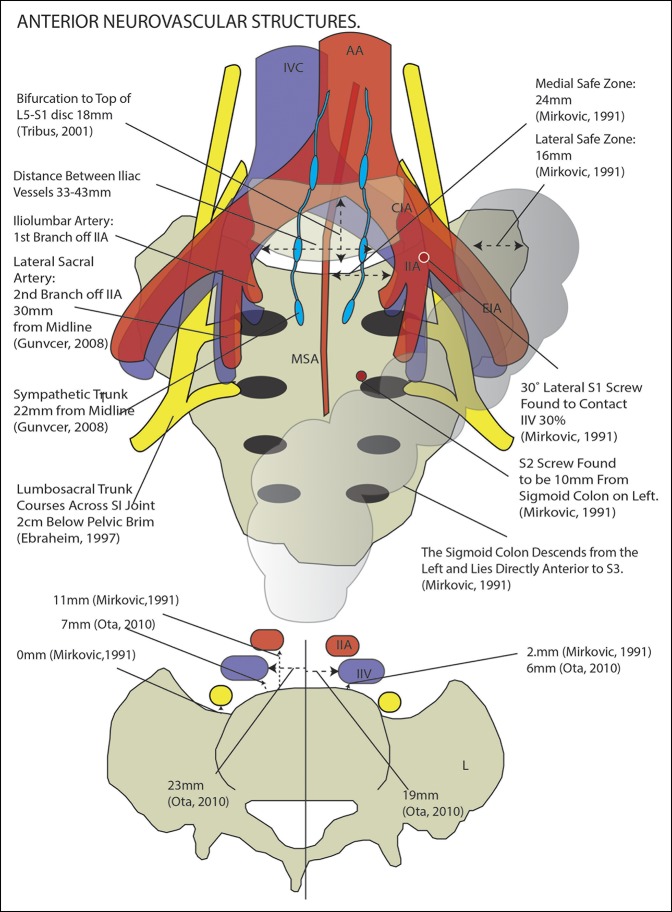
Instrumentation of the sacrum is challenging because of the irregular bony morphology and the proximity to neurovascular structures responsible for normal bowel, bladder, and sexual function. When approaching the sacrum posteriorly, screw fixation places anatomic structures in the retroperitoneum at risk. This area contains the internal iliac vessels, lateral sacral artery, middle sacral artery (MSA), hypogastric plexus, and sympathetic trunk. Inadvertent anterior cortical penetration by orthopaedic implants can cause notable morbidity.
Vascular Structures
Aortic bifurcation into the common iliac arteries occurs left of the midline at the lower level of the L4 vertebrae.38-40 The average distance of the bifurcation from the L5/S1 disc is 18 mm.41 The angle subtended by the bifurcation is 46°, with the left common iliac being 10° more vertical than the right. At the level of S1, the two vessels average 43 mm apart.41
The MSA is 2 to 3 mm in diameter. It originates 4 cm proximal to the aortic bifurcation and travels inferiorly, remaining near the midline.38,41 The MSA terminates into an anastomosis with the lateral sacral arteries, ultimately providing arterial branches to the ventral sacral foramina. Although consistently present, its course relative to the midline is highly variable. The MSA may be to the right or to the left of the midline by <3 cm and thus is a poor anatomic landmark.38,42,43
Distal to the aortic bifurcation, the right and left common iliac arteries travel in an inferolateral direction and branch into the internal and external iliac arteries.38 The right common iliac artery is 22 mm in diameter. It crosses the right common iliac vein and bifurcates anterior and lateral to the vein at the level of the L5-S1 disc.38 The left common iliac artery travels anterior and lateral but parallel to the vein.38 The distance from the anterior sacrum to the internal iliac artery averages 11 mm.13
Other smaller arterial branches include the iliolumbar artery and the lateral sacral artery. The iliolumbar artery is the first branch of the internal iliac artery and travels cranially, posteriorly, and laterally across the superior aspect of the SI joint.38 The lateral sacral artery is the second branch of the internal iliac artery at the level of S1-2 and is approximately 30 mm from the midline.43
The iliac vein confluence occurs slightly right of the midline at the upper end of the L5 vertebral body, forming the inferior vena cava from the two common iliac veins.13,40,41 The right common iliac vein is slightly shorter, more vertical, and travels farther from the midline than the left common iliac vein (23 versus 19 mm).11 The confluence angle of the common iliac veins is 63°.41 The total width of the so-called “safe zone” between the right common iliac artery and the left common iliac vein has been reported as 35 to 43 mm at the L5-S1 disc space.10,13,40,41 The average angle subtended by the right common iliac artery and the left common iliac vein is 77°.41 There is variability in the position of the left common iliac vein, and it may occur at the midline.38 The surgeon must be prepared to mobilize the left common iliac vein for access to the L5-S1 disc space.38,40 The common iliac veins are immediately in front of the sacral bone by 2 to 7 mm, unlike the common iliac arteries that are more anterior.11,14 The iliolumbar vein empties into the left common iliac vein posteriorly at the level of the L5 segment, and it may require ligation during the anterior approach. The venous anatomy may be abnormal in the presence of transitional vertebrae such that the venous confluence lies directly over the L5-S1 disc space.44
Neurologic Structures
The five sacral nerve roots, the lumbosacral plexus, and the sympathetic trunk are at risk with instrumentation of the sacrum. Five sacral nerve roots exist, which descend from the conus medullaris. The first four exit through the foramina, and the fifth exits between the sacrum and the coccyx.37 These spinal nerves course from the dorsal root ganglia and branch into the ventral and dorsal rami. All major motor nerve roots exit ventrally with only sensory cutaneous nerves exiting dorsally.38
The lumbosacral trunk (L4-L5) joins the sacral plexus anterior to the piriformis muscle to form the sciatic nerve. The fourth lumbar nerve root courses medial to the psoas muscle and crosses just superior to the first sacral foramen to join the fifth lumbar nerve root, which traverses laterally to join it. The location of the fifth lumbar nerve root can be variable and occurs either laterally on the ala near the SI joint or medially over the S1 pedicle. It is typically lateral to the internal iliac vein.13,38 The lumbosacral trunk is the closest anatomic structure to the sacrum, passing just 0.1 mm off of the anterior surface periosteum.14
Ebraheim et al1 analyzed the relationship of the lumbosacral plexus (L4-S3) to the sacrum and SI joint and provided measurements on the nerve size and position. The lengths of the L4 and L5 nerve roots are 102 and 75 mm, respectively, from the intervertebral foramina to the lumbosacral trunk. Similarly, the lengths of the S1, S2, and S3 are 58, 51, and 47 mm, respectively, from the anterior sacral foramina to the formation of the sciatic nerve. The angle formed by the nerve in relation to the sagittal plane decreases from distal (55° at S3) to proximal (15° at L4). On average, S1 has the thickest contribution to the lumbosacral plexus and courses just under the SI joint. The L4 nerve root is round, mobile, and located anterior to the L5 nerve root. It generally does not contact the sacrum or sacral ala. The L5 nerve root exits inferior to the lumbosacral ligament and is fixed in position by connective tissue to the anterior superior sacral ala. It has the longest course across the SI joint. The L4 and L5 nerve roots join to form the lumbosacral trunk, which traverses across the SI joint 2 cm below the pelvic brim. The S1 nerve courses along the inferior border of the SI joint. The S2 and S3 nerve roots generally do not have contact with the SI joint.45
The sympathetic trunk is derived from the anterior sacral nerve roots and is medial to the lateral sacral artery and approximately 22 mm from the midline.43 Mirkovic et al13 defined critical surgical parameters by identifying the medial and lateral safe zones on the anterior sacrum. The lateral safe zone is 16 mm wide and is bordered by the SI joint laterally and the lumbosacral trunk medially. The medial zone is 24 mm wide safe zone and is bordered by the sacral promontory medially and the internal iliac vein laterally29 (Figure 7, Supplemental Digital Content 8, http://links.lww.com/JG9/A23).
Figure 7.
Illustration showing the neurovascular anatomy surrounding the sacrum. IVC = inferior vena cava, AA = abdominal aorta, CIA = common iliac artery, EIA = external iliac artery, IIA = internal iliac artery, MSA = middle sacral artery.
Bowel
The sigmoid colon descends into the pelvis on the left side and becomes more posterior as it moves distally to a point where it lies directly on the sacral bone at S3. Mirkovic noted that S2 screws were closer to the sigmoid colon on the left side than the right (10 versus 15 mm).13
Conclusion
A systematic literature analysis and comprehensive report on the radiographic and gross anatomic features of sacral surgical instrumentation have yet to be performed. This review includes studies on the spatial arrangement of the S1 and S2 pedicle screws, SI screws, iliac screws, S2AI, pelvic neurovascular anatomy, and the sacral bony dimensions. This anatomically detailed data can be referenced by clinicians for sacral dissection and implant application. The data may also be useful for ongoing innovation in orthopaedic instrumentation technology.
Footnotes
Dr. Doty or an immediate family member is a member of a speakers' bureau or has made paid presentations on behalf of Arthrex, Globus Medical, and Wright Medical Technology; serves as a paid consultant to Arthrex, Globus Medical, and Wright Medical Technology; has stock or stock options held in Globus Medical; and has received research or institutional support from Wright Medical Technology. None of the following authors or any immediate family member has received anything of value from or has stock or stock options held in a commercial company or institution related directly or indirectly to the subject of this article: Dr. Katsuura, Mr. Chang, Dr. Sabri, and Dr. Gardner.
References
- 1.Ebraheim NA, Lin D, Xu R, Stanescu S, Yeasting RA: Computed tomographic evaluation of the internal structure of the lateral sacral mass in the upper sacra. Orthopedics 1999;22:1137-1140. [DOI] [PubMed] [Google Scholar]
- 2.Ebraheim N, Sabry FF, Nadim Y, Xu R, Yeasting RA: Internal architecture of the sacrum in the elderly: An anatomic and radiographic study. Spine (Phila Pa 1976) 2000;25:292-297. [DOI] [PubMed] [Google Scholar]
- 3.Salazar D, Lannon S, Pasternak O, Schiff A, Lomasney L, Mitchell E, et al. : Investigation of bone quality of the first and second sacral segments amongst trauma patients: concerns about iliosacral screw fixation. J Orthop Traumatol 2015;16:301-308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Arman C, Naderi S, Kiray A, et al. : The human sacrum and safe approaches for screw placement. J Clin Neurosci 2009;16:1046-1049. [DOI] [PubMed] [Google Scholar]
- 5.Robertson PA, Plank LD: Pedicle screw placement at the sacrum: Anatomical characterization and limitations at S1. J Spinal Disord 1999;12:227-233. [PubMed] [Google Scholar]
- 6.de Peretti F, Argenson C, Bourgeon A, Omar F, Eude P, Aboulker C: Anatomic and experimental basis for the insertion of a screw at the first sacral vertebra. Surg Radiol Anat 1991;13:133-137. [DOI] [PubMed] [Google Scholar]
- 7.Asher MA, Strippgen WE: Anthropometric studies of the human sacrum relating to dorsal transsacral implant designs. Clin Orthop Relat Res 1986;203:58-62. [PubMed] [Google Scholar]
- 8.Xu R, Ebraheim NA, Mohamed A, el-Gamal H, Yeasting RA: Anatomic considerations for dorsal sacral plate-screw fixation. J Spinal Disord 1995;8:352-356. [PubMed] [Google Scholar]
- 9.Morse BJ, Ebraheim NA, Jackson WT: Preoperative CT determination of angles for sacral screw placement. Spine (Phila Pa 1976) 1994;19:604-607. [DOI] [PubMed] [Google Scholar]
- 10.Ota M, Neo M, Fujibayashi S, Takemoto M, Nakamura T: Advantages of the paraspinal muscle splitting approach in comparison with conventional midline approach for s1 pedicle screw placement. Spine (Phila Pa 1976) 2010;35:E452–E457. [DOI] [PubMed] [Google Scholar]
- 11.Smith SA, Abitbol JJ, Carlson GD, Anderson DR, Taggart KW, Garfin SR: The effects of depth of penetration, screw orientation, and bone density on sacral screw fixation. Spine (Phila Pa 1976) 1993;18:1006-1010. [DOI] [PubMed] [Google Scholar]
- 12.Barber J, Boden S, Ganey T: Biomechanical study of lumbar pedicle screws: Does convergence affect axial pullout strength? J Spinal Disord 1998;11:215-220. [PubMed] [Google Scholar]
- 13.Mirkovic S, Abitbol JJ, Steinman J, et al. : Anatomic consideration for sacral screw placement. Spine (Phila Pa 1976) 1991;16(suppl 6):S289-S294. [PubMed] [Google Scholar]
- 14.Allen BL, Ferguson RL: The Galveston technique for L rod instrumentation of the scoliotic spine. Spine (Phila Pa 1976) 1982;7:276-284. [DOI] [PubMed] [Google Scholar]
- 15.Berry JL, Stahurski T, Asher MA, et al. : Morphometry of the supra sciatic notch intrailiac implant anchor passage. Spine (Phila Pa 1976) 2001;26:E143–E148. [DOI] [PubMed] [Google Scholar]
- 16.Tian X, Li J, Sheng W, et al. : Morphometry of iliac anchorage for transiliac screws: A cadaver and CT study of the Eastern population. Surg Radiol Anat 2010;32:455-462. [DOI] [PubMed] [Google Scholar]
- 17.Park SA, Kwak DS, You SL: Entry zone of iliac screw fixation to maintain proper entry width and screw length. Eur Spine J 2015;24:2573-2579. [DOI] [PubMed] [Google Scholar]
- 18.Schwend RM, Sluyters R, Najdzionek J: The pylon concept of pelvic anchorage for spinal instrumentation in the human cadaver. Spine (Phila Pa 1976) 2003;28:542-547. [DOI] [PubMed] [Google Scholar]
- 19.Miller F, Moseley C, Koreska J: Pelvic anatomy relative to lumbosacral instrumentation. J Spinal Disord 1990;3:169-173. [PubMed] [Google Scholar]
- 20.Zheng ZM, Yu BS, Chen H, et al. : Effect of iliac screw insertion depth on the stability and strength of lumbo-iliac fixation constructs: An anatomical and biomechanical study. Spine (Phila Pa 1976) 2009;34:E565–E572. [DOI] [PubMed] [Google Scholar]
- 21.Liu B, Wang J, Zhang L, Gan W: Radiographic study of iliac screw passages. J Orthop Surg 2014;9:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chang T-L, Sponseller PD, Kebaish KM, Fishman EK: Low profile pelvic fixation: Anatomic parameters for sacral alar-iliac fixation versus traditional iliac fixation. Spine (Phila Pa 1976) 2009;34:436-440. [DOI] [PubMed] [Google Scholar]
- 23.Zhu F, Bao HD, Yuan S, et al. : Posterior second sacral alar iliac screw insertion: Anatomic study in a Chinese population. Eur Spine J 2013;22:1683-1689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.O'Brien JR, Warren DY, Bhatnagar R, Sponseller P, Kebaish KM: An anatomic study of the S2 iliac technique for lumbopelvic screw placement. Spine (Phila Pa 1976) 2009;34:E439-E442. [DOI] [PubMed] [Google Scholar]
- 25.Noojin FK, Malkani AL, Haikal L, Lundquist C, Voor MJ: Cross-sectional geometry of the sacral ala for safe insertion of iliosacral lag screws: A computed tomography model. J Orthop Trauma 2000;14:31-35. [DOI] [PubMed] [Google Scholar]
- 26.Carlson DA, Scheid DK, Maar DC, Baele JR, Kaehr DM: Safe placement of S1 and S2 iliosacral screws: The “vestibule” concept. J Orthop Trauma 2000;14:264-269. [DOI] [PubMed] [Google Scholar]
- 27.Gardner MJ, Morshed S, Nork SE, Ricci WM, Routt MLC, Jr: Quantification of the upper and second sacral segment safe zones in normal and dysmorphic sacra. J Orthop Trauma 2010;24:622-629. [DOI] [PubMed] [Google Scholar]
- 28.Gardner MJ, Farrell ED, Nork SE, Segina DN, Chip Routt ML., Jr Percutaneous placement of iliosacral screws without electrodiagnostic monitoring. J Trauma 2009;66:1411-1415. [DOI] [PubMed] [Google Scholar]
- 29.Matta JM, Saucedo T: Internal fixation of pelvic ring fractures. Clin Orthop 1989;242:83-97. [PubMed] [Google Scholar]
- 30.Ebraheim NA, Xu R, Biyani A, Nadaud MC: Morphologic considerations of the first sacral pedicle for iliosacral screw placement. Spine (Phila Pa 1976) 1997;22:841-846. [DOI] [PubMed] [Google Scholar]
- 31.Routt ML, Simonian PT, Agnew SG, Mann FA: Radiographic recognition of the sacral alar slope for optimal placement of iliosacral screws: A cadaveric and clinical study. J Orthop Trauma 1996;10:171-177. [DOI] [PubMed] [Google Scholar]
- 32.Templeman D, Schmidt A, Freese J, Weisman I: Proximity of iliosacral screws to neurovascular structures after internal fixation. Clin Orthop Relat Res 1996:194-198. [DOI] [PubMed] [Google Scholar]
- 33.Collinge C, Coons D, Aschenbrenner J: Risks to the superior gluteal neurovascular bundle during percutaneous iliosacral screw insertion: An anatomical cadaver study. J Orthop Trauma 2005;19:96-101. [DOI] [PubMed] [Google Scholar]
- 34.Schildhauer TA, McCulloch P, Chapman JR, Mann FA: Anatomic and radiographic considerations for placement of transiliac screws in lumbopelvic fixations. J Spinal Disord Tech 2002;15:199-205. [DOI] [PubMed] [Google Scholar]
- 35.Xu R, Ebraheim NA, Yeasting RA, Wong FY, Jackson WT: Morphometric evaluation of the first sacral vertebra and the projection of its pedicle on the posterior aspect of the sacrum. Spine (Phila Pa 1976) 1995;20:936-940. [DOI] [PubMed] [Google Scholar]
- 36.Jackson RP, McManus AC: The iliac buttress: A computed tomographic study of sacral anatomy. Spine (Phila Pa 1976) 1993;18:1318-1328. [PubMed] [Google Scholar]
- 37.Whelan MA, Gold RP: Computed tomography of the sacrum: 1. Normal anatomy. AJR Am J Roentgenol 1982;139:1183-1190. [DOI] [PubMed] [Google Scholar]
- 38.Esses SI, Botsford DJ, Huler RJ, Rauschning W: Surgical anatomy of the sacrum: A guide for rational screw fixation. Spine (Phila Pa 1976) 1991;16(6 suppl):S283-S288. [DOI] [PubMed] [Google Scholar]
- 39.Datta JC, Janssen ME, Beckham R, Ponce C: The use of computed tomography angiography to define the prevertebral vascular anatomy prior to anterior lumbar procedures. Spine (Phila Pa 1976) 2007;32:113-119. [DOI] [PubMed] [Google Scholar]
- 40.Liu LH, Liang Y, Zhou Q, et al. : Study on the anatomy of the lumbosacral anterior great vessels pertinent to L5/S1 anterior interbody surgery with computer tomography angiography. Acta Orthop Belg 2014;80:537-543. [PubMed] [Google Scholar]
- 41.Tribus CB, Belanger T: The vascular anatomy anterior to the L5-S1 disk space. Spine (Phila Pa 1976) 2001;26:1205-1208. [DOI] [PubMed] [Google Scholar]
- 42.Sae-Jung S, Khamanarong K, Woraputtaporn W, Amarttayakong P: Awareness of the median sacral artery during lumbosacral spinal surgery: An anatomic cadaveric study of its relationship to the lumbosacral spine. Eur Spine J 2015;24:2520-2524. [DOI] [PubMed] [Google Scholar]
- 43.Güvençer M, Dalbayrak S, Tayefi H, et al. : Surgical anatomy of the presacral area. Surg Radiol Anat 2009;31:251-257. [DOI] [PubMed] [Google Scholar]
- 44.Weiner BK, Walker M, Fraser RD: Vascular anatomy anterior to lumbosacral transitional vertebrae and implications for anterior lumbar interbody fusion. Spine J 2001;1:442-444. [DOI] [PubMed] [Google Scholar]
- 45.Ebraheim NA, Lu J, Biyani A, Huntoon M, Yeasting RA: The relationship of lumbosacral plexus to the sacrum and the sacroiliac joint. Am J Orthop (Belle Mead NJ) 1997;26:105-110. [PubMed] [Google Scholar]