Abstract
Background:
Achilles tendon rupture (ATR) is a common injury with increasing incidence. Several risk factors have been identified; however, little is known about seasonal variations in injury prevalence. Previous reports have generated mixed results, with no clear consensus in the literature. The purpose of this investigation was to retrospectively review ATRs seen at a major academic orthopaedic surgery department in New York City to determine whether a statistically significant seasonal pattern of ATRs exists.
Methods:
A retrospective chart review was conducted, identifying patients with an acute ATR. Patients were excluded if they had a chronic rupture, laceration, débridement for tendinitis, Haglund deformity, or other nonacute indications for surgery. Date and mechanism of injury were determined from the clinical record.
Results:
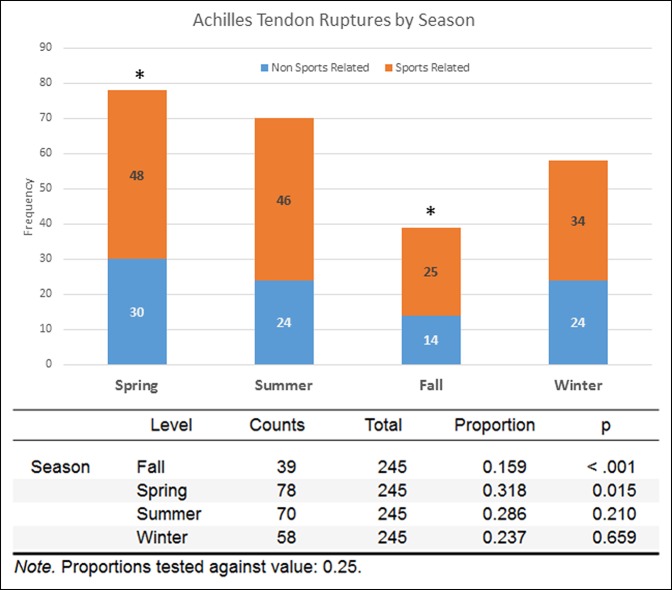
The highest rate of injury was seen in spring (P = 0.015) and the lowest in fall (P < 0.001), both of which were statistically significant. Overall, no statistically significant difference was noted in summer or winter, although more injuries were seen in summer. When only sports-related injuries are considered, a similar trend is seen, with most injuries occurring in spring (n = 48, P = 0.076) and fewest in fall (n = 25, P = 0.012); however, only the lower number in fall reaches statistical significance. No statistically significant difference was noted between seasons when only non–sports-related injuries were considered.
Conclusion:
A statistically significant increase was noted in the incidence of ATRs in spring and a statistically significant decrease in fall. The need for recognition of risk factors and preventive education is increasingly important in the orthopaedic surgery community and for primary care physicians, athletic trainers, coaches, and athletes.
Level of Evidence:
Prognostic level IV
Achilles tendon rupture (ATR) is a common injury with an incidence of 37:100,000 per year,1 and the incidence seems to be increasing.2 This injury generally requires two things to be present: (1) a focus of degeneration, or tendinosis, in the tendon, and (2) an eccentric contracture of the tendon of sufficient force to tear the tendon apart. Several known risk factors for ATR, including male sex, age between 30 and 40 years, episodic athletic activity (the so-called weekend warrior), fluoroquinolone antibiotics, and steroid injections, exist.3,4 However, little is reported on the seasonal variance of the incidence of these injuries. In the clinical experience of our group, the incidence of this injury tends to increase in early spring and remains high through the summer months. Of the few studies in the literature that address this question, the results are varied.5,6,7,8 The only statistically significant results were reported in a retrospective review of 23 years of experience treating ATRs at an academic teaching hospital in Vancouver, Canada. The authors found signficantly more ATRs occurred during the spring season.7 The purpose of this investigation was to retrospectively review ATRs seen at a major academic orthopaedic surgery department to determine whether a statistically significant seasonal pattern of ATRs exits. Finding such a seasonal variation in risk would provide evidence-based guidance for patient education and community counseling with the goal of injury prevention.
Methods
This project was conducted with the approval of the institutional review board. We queried all available billing records for Current Procedural Terminology codes 27650, 27652, and 27654 and International Classification of Disease diagnosis codes 727.67, 845.09, and S86.01x pertaining to Achilles tendon injury, repair, and reconstruction. Charts were then manually screened and included if (1) the patient had an acute ATR and (2) the date of the injury could be determined from the records (expressly stated in the office or surgical notes). Charts were excluded if (1) the patient had a chronic Achilles tear where the date of injury could not be determined, (2) underwent reconstruction or débridement for tendinitis, Haglund deformity, tendon laceration, or any other indications other than acute rupture, or (3) did not have sufficient detailed information on the record to determine the date of injury. If information was not clear on the mechanism of injury, the case was considered non–sports related. Included charts were also reviewed for patient demographics, comorbidities, mechanism of injury (sports related or non–sports related), and any history of previous Achilles ruptures or symptoms. Seasons were defined in the same manner as in the study by Scott et al,7 with spring: March 21 to June 20, summer: June 21 to September 20, fall: September 21 to December 20, and winter: December 21 to March 20. Our database search yielded a total of 499 patients between July 1, 2003, and April 7, 2017. After chart review, 251 acute ATRs were identified. Six cases were excluded because of inadequate information on the record, leaving a total of 245 records for analysis.
Data were analyzed using a chi-squared test for categoric variables, binomial test for probability determination, and appropriate Student t-tests for continuous variables. For continuous variables, normality and variance were tested using a Shapiro-Wilk test and Levene test, respectively. A nonparametric Mann-Whitney U t-test was selected for data sets without a normal distribution and equal variance, and a Welch t-test was used for normally distributed data sets without equal variance. Significance was determined by P < 0.05. Statistical analysis was conducted using JASP statistical software (version 0.8.1.1; JASP Team, 2017).
Results
Overall, the average age of the patient at the time of injury was 43.6 years (range, 17 to 90 years), with statistically significantly more men than women (86% versus 14%, respectively; P < 0.001) and no difference in laterality (50% left versus 50% right; P = 0.95). Sixty-six percent of injuries were identified as sports related, whereas 34% were identified as non–sports related. A previous Achilles rupture was reported in 11% of patients overall, with no difference between the sports and nonsports groups (P = 0.77). Of those patients with previous ruptures (n = 25), 72% involved the contralateral side (P = 0.043; 95% CI, 0.506 to 0.879).
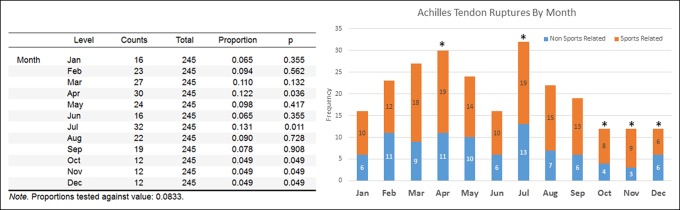
When stratified by month (Figure 1), statistically significant peaks occurred in April and July (P = 0.036 and P = 0.011, respectively), with statistically significantly fewer injuries occurring in October through December (P = 0.049). Regarding seasons (Figure 2), the highest rate of injury was seen in spring (P = 0.015) and the lowest in fall (P < 0.001), both of which were statistically significant. Overall, no statistically significant difference was noted in summer or winter, although more injuries were seen in summer. When only sports-related injuries are considered, a similar trend is seen, with most injuries occurring in spring (n = 48; P = 0.076) and fewest in fall (n = 25; P = 0.012); however, only the lower number in fall reaches statistical significance. No statistically significant difference was noted between seasons when only the non–sports-related injuries were considered.
Figure 1.
Graph showing Achilles tendon ruptures by season. Significantly more ruptures were seen in spring (P = 0.015), and statistically significantly fewer ruptures were seen in fall (P < 0.001). The incidence of sports-related and non–sports-related injuries followed a similar trend.
Figure 2.
Graph showing Achilles tendon ruptures by month. Significantly more ruptures were seen in April and July (*P = 0.036 and P = 0.011, respectively), and statistically significantly fewer ruptures were seen from October to December (P = 0.049). Sports-related and non–sports-related injury incidence followed a similar trend.
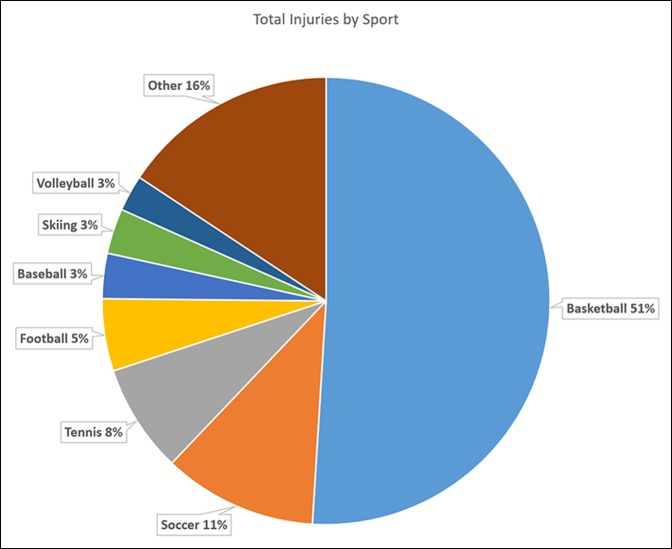
The average age of patients with sports-related injuries was 37.5 years at the time of injury; this was statistically significantly lower than that of patients with non–sports-related injuries who averaged 56.2 years (P < 0.001). Similarly, the average body mass index of patients with sports-related injuries was statistically significantly lower than those with non–sports-related injuries (26.8 versus 28.7; P = 0.009). No statistically significant difference in sex or laterality of injury was noted between sports-related and non–sports-related injuries (P = 0.06 and P = 0.43, respectively). Of sports-related injuries (Figure 3), basketball was the most common sport involved (n = 78), which accounted for 51% of injuries included in this study, a statistically significant majority (P < 0.001). The next most common sports were soccer and tennis, which accounted for only 11% (n = 17) and 8% (n = 12), respectively. No statistically significant variation was noted between seasons in any particular sport. Overall, Most patients (87.6%) did not have any symptoms of pain before their rupture; however, patients with sports-related injuries were statistically significantly less likely to have preceding pain than those with non–sports-related injuries (5.4% versus 25.6%, respectively; P < 0.001).
Figure 3.
Pie chart showing total injuries by sport. Basketball was the most common sport (n = 78), followed by soccer (n = 17), tennis (n = 12), and football (n = 8). Less common sports included baseball (n = 5), skiing (n = 5), volleyball (n = 4), climbing (n = 2), handball (n = 2), kickboxing (n = 2), lacrosse (n = 2), racquetball (n = 2), skateboarding (n = 2), snowboarding (n = 2), softball (n = 2), table tennis (n = 2), dance (n = 1), dodgeball (n = 1), parkour (n = 1), pickleball (n = 1), running (n = 1), and squash (n = 1).
Discussion
Our results suggest a statistically significant seasonal variation in the incidence of ATRs in the population served by our physicians. Both sports-related and non–sports-related injuries followed a similar pattern, with most injuries occurring during spring and summer and fewest during fall and winter. Our subgroup analysis did not find a statistically significant seasonal variation in non–sports-related injuries; the frequency of these injuries was highest in spring but did not achieve statistical significance. Our results show a similar trend to those reported by Scott et al7 who found a 33% increase (P < 0.05) in Achilles tendon injuries duringspring in their catchment area of Vancouver, Canada. Interestingly, we have a greater proportion of non–sports-related injuries in our data set (34% versus 24%) likely because our study considered both surgically and nonsurgically treated patients, whereas the previous study included only surgical patients. Maffulli et al5 retrospectively reviewed 15 years of records from the National Health Service in Scotland and found that although the overall incidence of the injuries increased over the study period, there was no evidence of a seasonal difference (although they did note a reduced number of cases in fall, consistent with our findings). Suchak et al8 performed a similar review in Edmonton, Canada, and although they also noted that most injuries occurred during spring, no statistical significance was noted.
The reasons for this seasonal variation are likely multifactorial. It has been suggested that spring is a transitional period of increasing athletic activity for recreational athletes.7 Inglis and Sculco's9 comprehensive work on Achilles rupture noted that “most of the patients […] admitted to being ‘out of shape’ at the time of their tendon rupture inasmuch as the rupture occurred early in the season.” Conversely, Parekh et al6 investigated ATRs in National Football League football players and found that in this group, most injuries occurred during the regular season as opposed to preseason training (65% versus 35%, respectively). However, the injury patterns found in professional athletes are not necessarily generalizable to the recreational athlete because these individuals typically maintain a high level of fitness and participate in training activities year-round. Indeed, our data set included only four professional- and three college-level athletes (approximately 4% of the total sports-related injuries seen), so extrapolation of our findings beyond the recreational athlete is not possible.
We found that for our patients with sports-related injuries, both the average age (37.5 versus 56.2 years) and average body mass index (26.8 versus 28.7) were statistically significantly lower, suggesting that they were younger and more physically fit patients. We also found a statistically significant increase in the incidence of pain preceding the tendon rupture in patients with non–sports-related injuries. These findings suggest that there may be differing populations of patients who have ATRs. Older patients may have more severe tendinosis requiring less of an eccentric contracture (ie, less activity), and younger patients may be more likely to have a clinically silent tendinosis that requires a more aggressive eccentric contracture to end in rupture. Indeed, most young athletic patients who rupture their Achilles tendons have no clinical symptoms beforehand. However, it is uncertain to what extent such a process is involved in our patient population because routine MRI or ultrasonography is not conducted for Achilles ruptures in our institution.
Basketball accounted for most sports-related injuries in our series. However, any sport that requires rapid movements, jumping, and sprinting (ie, many opportunities for eccentric contracture) likely presents a similar risk of Achilles injury. The most likely explanation for this finding is simply the popularity of basketball in our patient community. Other studies of Achilles ruptures from Europe similarly reflect popular sports in the local culture. While Inglis' study found basketball was the most common source of injury in the United States, raquet sports and soccer represented the highest prevalence in Denmark and Hungary, respectively, reflecting the regional popularity of these sports. Of note, no seasonal connection was made in these studies.1,9,10
These findings could help provide evidence-based guidance for patient education and community counseling with the goal of injury prevention. Primary prevention of acute ATR is founded on maintaining healthy collagen that has the ability to resist applied forces.11 Regular physical exercise is necessary to develop a strong blood supply to the collagen and to delay degenerative changes and collagen fiber fatigue within the tendon.12 In addition to regular physical activity, preactivity warm-up periods are important to increase the temperature and extensibility of the tendon and to prepare it for loading.12,13 Although clinical studies investigating the role of stretching on preventing Achilles tendinopathy are lacking, stretching may enhance tendon extensibility, and many clinicians recommend including gastrocnemius and soleus stretches into the warm-up routine. Eccentric ankle plantar flexor strengthening, mimicking the ankle's loading response, has been linked to the prevention of acute ATR by minimizing Achilles tendinosis.14 Finally, fluoroquinolone and steroid-associated tendinopathy and tendon rupture have been well described, and certain precautions should be taken in athletic and highly active patients, especially during spring or when beginning a new training regimen. Specific evidence regarding what measures are most effective is lacking; however, guidelines detailing important considerations and emphasizing close monitoring have been published.15
Our study has several limitations. First, this study is a retrospective chart review, and as such, we relied on preexisting records, which may have been incomplete or contained incorrect data. We also used only the records from two attending surgeons at our institution, a large academic medical center, which may or may not be representative of the region as a whole. However, this study was not intended to be an epidemiologic study or to report true incidence in the population. Although we reviewed all the available records, only 245 contained adequate information to be included, which is a smaller sample size than some of the comparable studies in the literature.
Conclusions
As ATRs continue to become more common, the need for recognition of risk factors and preventive education becomes increasingly important in the orthopaedic surgery community and for primary care physicians, athletic trainers, coaches, and athletes. Our study helps confirm that there is an increased risk of ATR during spring when abrupt increases in sporting activity are common. Future studies are needed to elucidate the pathophysiologic mechanisms underlying this vulnerability.
Footnotes
Dr. Greisberg or an immediate family member serves as a board member, owner, officer, or committee member of the American Academy of Orthopaedic Surgeons and American Orthopaedic Foot & Ankle Society; has received research support from Extremity Medical; and has received publishing royalties from Saunders/Mosby-Elsevier. Dr. Vosseller or an immediate family member has received IP royalties from New Clip Technics; and has received publishing royalties from Saunders/Mosby-Elsevier; serves as a consultant to DJ Orthopedics; serves as a board member, owner, officer, or committee member of the American Academy of Orthopaedic Surgeons and American Orthopaedic Foot & Ankle Society; and serves as an editorial board member of Foot and Ankle Orthopedics. None of the following authors or any immediate family member has received anything of value from or has stock or stock options held in a commercial company or institution related directly or indirectly to the subject of this article: Dr. Caldwell, Dr. Lightsey, Dr. Trofa, and Dr. Swindell.
References
- 1.Houshian S, Tscherning T, Riegels-Nielsen P: The epidemiology of Achilles tendon rupture in a Danish county. Injury 1998;29:651-654. [DOI] [PubMed] [Google Scholar]
- 2.Ho G, Tantigate D, Kirschenbaum J, Greisberg JK, Vosseller JT: Increasing age in Achilles rupture patients over time. Injury 2017;48:1701-1709. [DOI] [PubMed] [Google Scholar]
- 3.Claessen FM, de Vos RJ, Reijman M, Meuffels DE: Predictors of primary Achilles tendon ruptures. Sport Med 2014;44:1241-1259. [DOI] [PubMed] [Google Scholar]
- 4.Vosseller JT, Ellis SJ, Levine DS, et al. : Achilles tendon rupture in women. Foot Ankle Int 2013;34:49-53. [DOI] [PubMed] [Google Scholar]
- 5.Maffulli N, Waterston SW, Squair J, Reaper J, Douglas AS: Changing incidence of Achilles tendon rupture in Scotland: A 15-year study. Clin J Sport Med 1999;9:157-160. [DOI] [PubMed] [Google Scholar]
- 6.Parekh SG, Wray WH, Brimmo O, Sennett BJ, Wapner KL: Epidemiology and outcomes of Achilles tendon ruptures in the national football league. Foot Ankle Spec 2009;2:283-286. [DOI] [PubMed] [Google Scholar]
- 7.Scott A, Grewal N, Guy P: The seasonal variation of Achilles tendon ruptures in vancouver, Canada: A retrospective study. BMJ Open 2014;4:e004320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Suchak AA, Bostick G, Reid D, Blitz S, Jomha N: The incidence of Achilles tendon ruptures in Edmonton, Canada. Foot Ankle Int 2005;26:932-936. [DOI] [PubMed] [Google Scholar]
- 9.Inglis AE, Sculco TP: Surgical repair of ruptures of the tendo Achillis. Clin Orthop Relat Res 1981:160-169. [PubMed] [Google Scholar]
- 10.Jozsa L, Kvist M, Balint BJ, et al. : The role of recreational sport activity in Achilles tendon rupture. Am J Sports Med 1989;17:338-343. [DOI] [PubMed] [Google Scholar]
- 11.Hess GW: Achilles tendon rupture: A review of etiology, population, anatomy, risk factors, and injury prevention. Foot Ankle Spec 2010;3:29-32. [DOI] [PubMed] [Google Scholar]
- 12.Leppilahti J, Orava S: Total Achilles tendon rupture: A review. Sports Med 1998;25:79-100. [DOI] [PubMed] [Google Scholar]
- 13.Milgrom C, Finestone A, Zin D, Mandel D, Novack V: Cold weather training: A risk factor for Achilles paratendinitis among recruits. Foot Ankle Int 2003;24:398-401. [DOI] [PubMed] [Google Scholar]
- 14.Schepsis AA, Jones H, Haas AL: Achilles tendon disorders in athletes. Am J Sports Med 2002;30:287-305. [DOI] [PubMed] [Google Scholar]
- 15.Hall MM, Finnoff JT, Smith J: Musculoskeletal complications of fluoroquinolones: Guidelines and precautions for usage in the athletic population. PM R 2011;3:132-142. [DOI] [PubMed] [Google Scholar]