Abstract
Gastrointestinal stromal tumors (GISTs) arise from the intestinal pacemaker cells of Cajal. Wild-type gastrointestinal stromal tumors (WT-GIST) are a unique and uncommon subtype of GISTs that lack activating mutations in the tyrosine kinase c-KIT or platelet derived growth factor receptor alpha (PDGFRA) receptors. The lack of these growth-stimulating mutations renders tyrosine kinase receptor inhibitors, such as imatinib mesylate, relatively ineffective against these tumors. WT-GIST arises most commonly due to underlying alternate proliferative signals associated with germ-line, genetic mutations. WT-GIST frequently arises in patients with BRAF mutations, Carney’s Triad or neurofibromatosis type-1 (NF-1). All patients with WT-GIST require a careful examination for germ-line mutations and very close observation for recurrent tumors. Surgery remains a mainstay therapy for these patients. This review aims to discuss the most recent data available on the diagnosis and treatment of WT-GIST.
Keywords: Gastrointestinal stromal tumor (GIST), sarcoma, succinate dehydrogenase (SDH), wild-type gastrointestinal stromal tumor (WT-GIST)
Introduction
Originating from the interstitial cells of Cajal, gastrointestinal stromal tumors (GISTs) are the most common mesenchymal neoplasms of the gastrointestinal (GI) tract (1,2). Subendothelial in location, GISTs typically present in the seventh decade of life and can arise anywhere along the GI tract, most commonly in the stomach. The discovery of the KIT and platelet derived growth factor receptor alpha (PDGFRA) tyrosine-kinase gain of function mutations, which result in continuous activation and signaling, dramatically altered the understanding and treatment of GISTs (3,4). Approximately 90% of GISTs are driven by gain-of-function mutations in one of the two type-III tyrosine kinase receptors. Although resection remains a principle therapy, tyrosine-kinase inhibitors have revolutionized the treatment of advanced and recurrent GISTs, allowing many patients with advanced disease to live many years and in some instances, obtain complete remission (5-8).
Wild-type gastrointestinal stromal tumors (WT-GISTs) are defined as GISTs that lack the gain-of-function mutations in KIT and PDGFRA (9). Due to the different molecular drivers and the distinct tumor biology and behavior of these wild-type neoplasms, a different approach to treatment may be required when addressing these distinct GISTs.
Epidemiology of WT-GIST
Regardless of subtype, the incidence of all GISTs is approximately 14–20 per million population (1). The incidence of WT-GIST is as much as 10% of all GISTs (10). Patients with WT-GISTs usually present at a much younger age. GISTs arising in younger patients are much more commonly associated with the wild-type variant. In patients under 23 years of age, 85% of GISTs are WT (4,11).
Molecular characteristics of WT-GIST
The majority of GISTs have mutations in the proto-oncogenes KIT or PDGFRA. Mutations in these tyrosine kinase receptors result in ligand independent kinase activation, resulting in cellular proliferation and oncogenesis (1,3,4,9). Wild-type GIST variants are negative for mutations in KIT and PDGFRA. Consequently, these rare wild-type GISTs are generally resistant to tyrosine kinase inhibitors (i.e., imatinib and sunitinib) currently used in the treatment of the more common variety of GISTs (1). Thus, an understanding of the molecular characteristics of these wild-type GISTs is important for making clinical decisions and for the future development of targeted therapeutic agents against these rare tumors.
Recent studies demonstrate that WT-GISTs are an entity with multiple subtypes. Of these subtypes, the succinate dehydrogenase (SDH) deficiency variant is the most common. The SDH-ubiquinone complex II is an enzyme complex found in the Krebs cycle and the electron transport chain. Loss of function of SDH is thought to play a central role in the pathogenesis of many WT-GISTs. It is postulated that SDH deficiency may lead to activation of insulin-like growth factor 1-receptor (IGF1R) signaling and results in oncogenesis. These SDH deficient GISTs arise exclusively in the stomach as multiple lesions. They also have a predilection for young female patients and are responsible for over half of gastric GISTs in patients under 40 years (1,12-15). Mutations of SDH are not solely exclusive to GIST pathogenesis and have been associated with other tumors such as malignant pheochromocytoma and renal cell carcinoma (13).
The majority of SDH deficient WT-GISTs are due to germline or somatic mutation in the SDH complex, specifically in genes coding for its subunits: SDHA, SDHB, SDHC, or SDHD. SDHA and SDHB code for subunits involved in the enzymatic activity of SDH, while SDHC and SDHD code for the subunits which anchor the SDH complex to the inner mitochondrial membrane. Mutations in all subunits have been implicated in WT-GIST formation; however, mutations in the SDHA subunit are most common. SDH deficiency can also be expressed without inactivating mutations of the gene itself, but through hypermethylation. Specifically, it has been found that methylation at the SDHC promoter leads to silencing of gene expression (16,17).
The remaining WT-GISTs are classified as SDH-competent. These tumors have demographic features similar to c-KIT/PDGFRA mutant tumors with the exception of their propensity to occur in the small bowel (17). SDH-competent WT-GISTs may be associated with other mutations such as Neurofibromatosis type-1 (NF1), BRAF V600E (BRAF), RAS, or quadruple WT GISTs, which lack abnormalities in c-KIT, PDGFRA, SDH and RAS (17-22).
Syndromic associations of WT-GIST
In addition to occurring sporadically, WT-GISTs may be the result of an associated syndrome. GISTs are a well-established manifestation of neurofibromatosis type-I (NF1), with up to 25% of patients with NF1 developing a GIST over their lifetime (23,24). Additionally, these tend to be WT-GISTs (25,26).
Carney-Stratakis syndrome (CSS) is characterized by paragangliomas and GISTs. Carney triad (CT) describes the association of paragangliomas with GISTs and pulmonary chondromas. Both CSS and CT have been associated with SDH-deficient WT-GISTs (14).
Familial GIST syndrome is a rare hereditary disorder characterized by germline gain-of-function KIT mutations and less commonly PDGFRA mutations. These are not associated with WT-GIST tumors (1).
Diagnosis
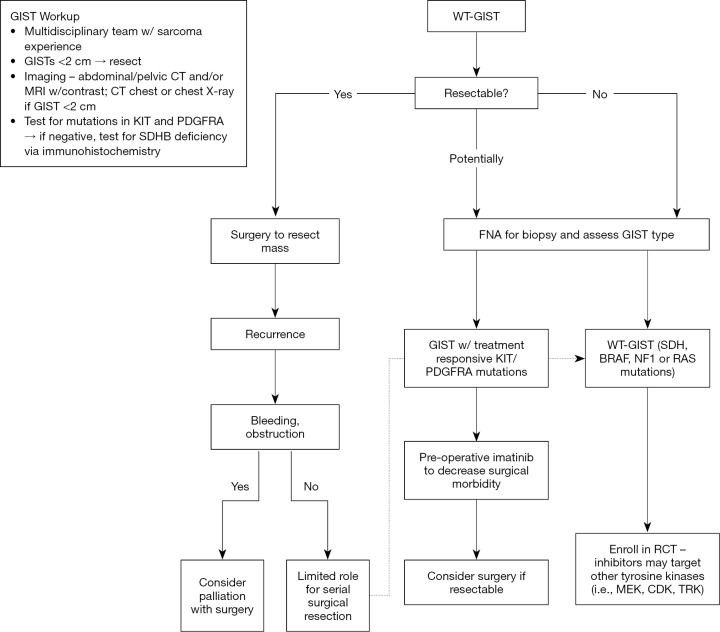
Initial diagnosis and treatment is similar for all GISTs and is outlined in Figure 1. Imaging, biopsy, pathologic examination and molecular analysis are all part of the diagnostic work up.
Figure 1.
Diagnostic algorithm for WT-GIST; WT-GIST, wild-type gastrointestinal stromal tumor.
Imaging
The diagnosis of all GIST can often be suspected based on imaging features. Computed tomography (CT) scan of the abdomen and pelvis showing a heterogeneously, vascularly enhancing exophytic mass emanating from the GI tract is the predominant pattern seen with GIST (27,28).
Endoscopic ultrasound and biopsy
Diagnosis of an abdominal mass suspicious for GIST can reasonably be treated with surgery directly without additional procedures. If the diagnosis remains unclear, however, endoscopic or endoscopic ultrasound-directed fine needle aspiration may be performed (29). Percutaneous biopsy should be avoided due to the risk of seeding the biopsy tract with cancerous cells. In the setting of large tumors PET scanning may also be considered to better stage patients and to monitor the metabolic activity of the tumor.
Pathologic analysis
Initial pathologic analysis must include the determination of the dimensions of the tumor and histologic analysis focusing specifically on mitotic rate. Size and mitotic rate are the main factors in risk stratification (Table 1). Testing for the presence of c-KIT and PDGFRA mutations is a standard part of the initial analysis for any GIST (29).
Table 1. Risk stratification for GIST.
| Risk of progression | Size (cm) | Mitotic count (per 50 HPF) |
|---|---|---|
| Very low | <2 | <5 |
| Low | 2–5 | <5 |
| Intermediate | <5 | 6–10 |
| 5–10 | <5 | |
| High | >5 | >5 |
| >10 | Any mitotic count |
Adapted with permission from Trifan et al. (30). HPF, high power fields; GIST, gastrointestinal stromal tumor.
Molecular subtyping
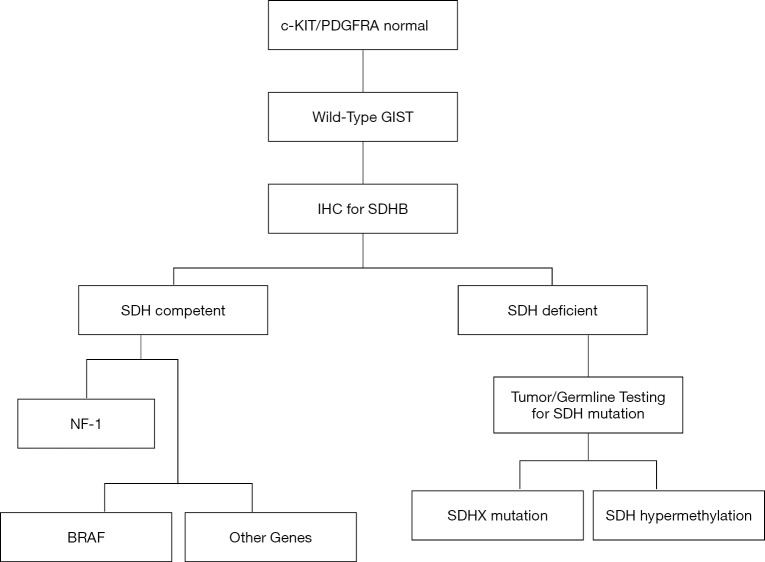
Tumors lacking c-KIT and PDGFRA mutations should be approached in a step wise fashion starting with testing for SDH status (Figure 2) (31). Immunohistochemical staining with observed loss of the ubiquitously expressed SDHB has proven to be an accurate and cost-efficient diagnostic marker for SDH deficiency (15,17,32,33). Patients with SDH competent tumors should be tested for mutations in NF1 and BRAF as these have been identified to be present in SDH competent WT-GISTs (34).
Figure 2.
Treatment algorithm for WT-GIST. WT-GIST, wild-type gastrointestinal stromal tumor.
Patients with SDH deficient WT-GISTs should undergo tumor and germline sequencing of SDH because those with SDHX germline mutations are at increased risk for developing paraganglioma, pheochromocytoma, and other tumors (35). Routine screening with total body magnetic resonance imaging (MRI), urine metanephrines, and/or plasma catecholamines along with referral to a genetic counselor should also be strongly considered (36).
Treatment for WT-GIST
In our current armamentarium against GISTs, surgical management remains standard and is the only option that offers the potential for cure in patients with resectable tumors (18). In about 60% of individuals, surgery can offer cure (27). GISTs are resistant to standard cytotoxic chemotherapeutics available (11). In patients with locally advanced disease, metastatic disease or recurrent disease, tyrosine kinase inhibitors, like imatinib mesylate, have offered patients a treatment option with studies demonstrating excellent response (9). However, WT-GISTs in particular remain a challenge as they are generally resistance to imatinib (31).
While treatment strategies for WT-GISTs are not clearly established. The NIH Pediatric and Wild-Type GIST clinic data demonstrated no improvement in event-free survival with extensive or serial resections and proposed surgical therapy to be reserved for initial resection and only repeat resections to address palliation of symptoms such as obstruction or bleeding (37). Nonetheless, surgical resection remains a critical component, perhaps the key component, in the overall treatment of WT-GIST as it provides the only chance for cure and can optimize palliation (38-40).
Although type-III tyrosine kinase receptor therapy has proven ineffective, there may be a role for alternative adjunct treatments in WT-GIST. Pazopanib, a vascular endothelial growth factor receptor (VEGFR) inhibitor has recently been shown to improve progression-free survival in patients with advanced GIST resistant to imatinib and sunitinib (41). Additionally, the BRAF inhibitor dabrafenib, has demonstrated prolonged antitumor activity in V600E BRAF-mutated GIST (42). MEK inhibition has similarly been shown to reduce the growth of tumors in patients with NF-1 (43). Lastly, inhibition of insulin-like growth factor receptor 1 has led to cytotoxicity and induced apoptosis in patients with WT-GIST (44). For all of the adjunctive therapies additional trials will be needed.
Conclusions
In summary, WT-GISTs represent a special subset of GIST that require specialized treatment strategies based on their unique biological characteristics. While surgical resection remains the cornerstone of treatment for resectable tumors and an option for symptomatic tumors, testing for SDH competence is indicated for all GISTs that lack c-KIT and PDGFRA mutations. Further testing and treatment must be individualized based on SDH competence and include testing for SDHX somatic and germline mutations, NF-1, V600E BRAF, RAS, and other genes. While these tumors are not responsive to imatinib, initiation of novel therapeutic agents based on additional testing may prove to be beneficial. WT-GIST still, however, represents a unique clinical entity for which additional research needs to be undertaken to establish the best therapeutic approach.
Acknowledgements
None.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.Miettinen M, Lasota J. Gastrointestinal stromal tumors. Gastroenterol Clin North Am 2013;42:399-415. 10.1016/j.gtc.2013.01.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Miettinen M, Lasota J. Histopathology of gastrointestinal stromal tumor. J Surg Oncol 2011;104:865-73. 10.1002/jso.21945 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hirota S, Isozaki K, Moriyama Y, et al. Gain-of-function mutations of c-kit in human gastrointestinal stromal tumors. Science 1998;279:577-80. 10.1126/science.279.5350.577 [DOI] [PubMed] [Google Scholar]
- 4.Heinrich MC, Corless CL, Duensing A, et al. PDGFRA activating mutations in gastrointestinal stromal tumors. Science 2003;299:708-10. 10.1126/science.1079666 [DOI] [PubMed] [Google Scholar]
- 5.Joensuu H, Roberts PJ, Sarlomo-Rikala M, et al. Effect of tyrosine kinase inhibitor STI571 in a patient with metastatic gastrointestinal stromal tumor. N Engl J Med 2001;344:1052-6. 10.1056/NEJM200104053441404 [DOI] [PubMed] [Google Scholar]
- 6.Pedroso FE, Raut CP, Xiao H, et al. Has the survival rate for surgically resected gastric gastrointestinal stromal tumors improved in the tyrosine kinase inhibitor era? Ann Surg Oncol 2012;19:1748-58. 10.1245/s10434-012-2222-9 [DOI] [PubMed] [Google Scholar]
- 7.Cheung MC, Zhuge Y, Yang R, et al. Disappearance of racial disparities in gastrointestinal stromal tumor outcomes. J Am Coll Surg 2009;209:7-16. 10.1016/j.jamcollsurg.2009.03.018 [DOI] [PubMed] [Google Scholar]
- 8.Perez EA, Livingstone AS, Franceschi D, et al. Current incidence and outcomes of gastrointestinal mesenchymal tumors including gastrointestinal stromal tumors. J Am Coll Surg 2006;202:623-9. 10.1016/j.jamcollsurg.2006.01.002 [DOI] [PubMed] [Google Scholar]
- 9.Heinrich MC, Corless CL, Blanke CD, et al. Molecular correlates of imatinib resistance in gastrointestinal stromal tumors. J Clin Oncol 2006;24:4764-74. 10.1200/JCO.2006.06.2265 [DOI] [PubMed] [Google Scholar]
- 10.Corless CL, Fletcher JA, Heinrich MC. Biology of gastrointestinal stromal tumors. J Clin Oncol 2004;22:3813-25. 10.1200/JCO.2004.05.140 [DOI] [PubMed] [Google Scholar]
- 11.Janeway KA, Liegl B, Harlow A, et al. Pediatric KIT wildtype and platelet-derived growth factor receptor alpha wild-type gastrointestinal stromal tumors share KIT activation but not mechanisms of genetic progression with adult gastrointestinal stromal tumors. Cancer Res 2007;67:9084-8. 10.1158/0008-5472.CAN-07-1938 [DOI] [PubMed] [Google Scholar]
- 12.Miettinen M, Lasota J, Sobin LH. Gastrointestinal stromal tumors of the stomach in children and young adults: a clinicopathologic, immunohistochemical, and molecular genetic study of 44 cases with long-term follow-up and review of the literature. Am J Surg Pathol 2005;29:1373-81. 10.1097/01.pas.0000172190.79552.8b [DOI] [PubMed] [Google Scholar]
- 13.Janeway KA, Kim SY, Lodish M, et al. Defects in succinate dehydrogenase in gastrointestinal stromal tumors lacking KIT and PDGFRA mutations. Proc Natl Acad Sci USA 2011;108:314-8. 10.1073/pnas.1009199108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Stratakis CA, Carney JA. The triad of paragangliomas, gastric stromal tumours, and pulmonary chondromas (Carney triad), and the dyad of paragangliomas and gastric stromal sarcomas (Carney-Stratakis syndrome): molecular genetics and clinical implications. J Intern Med 2009;266:43-52. 10.1111/j.1365-2796.2009.02110.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Miettinen M, Wang ZF, Sarlomo-Rikala M, et al. Succinate dehydrogenase-deficient GISTs: a clinicopathologic, immunohistochemical, and molecular genetic study of 66 gastric GISTs with predilection to young age. Am J Surg Pathol 2011;35:1712-21. 10.1097/PAS.0b013e3182260752 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Haller F, Moskaley EA, Faucz FR, et al. Aberrant DNA hypermethylation of SDHC: a novel mechanism of tumor development in Carney triad. Endocr Relat Cancer 2014;21:567-77. 10.1530/ERC-14-0254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Boikos SA, Pappo AS, Killian JK, et al. Molecular subtypes of KIT/PDGFRA wild-type gastrointestinal stromal tumors: a report from the National Institutes of Health Gastrointestinal Stromal Tumor Clinic. JAMA Oncol 2016;2:922-28. 10.1001/jamaoncol.2016.0256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nishida T, Tsujimoto M, Takahashi T, et al. Gastrointestinal stromal tumors in Japanese patients with neurofibromatosis type I. J Gastroenterol 2016;51:571-8. 10.1007/s00535-015-1132-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Huss S, Pasternack H, Ihle MA, et al. Clinicopathological and molecular features of a large cohort of gastrointestinal stromal tumors (GISTs) and review of the literature: BRAF mutations in KIT/PDGFRA wild-type GISTs are rare events. Hum Pathol 2017;62:206-14. 10.1016/j.humpath.2017.01.005 [DOI] [PubMed] [Google Scholar]
- 20.Hechtman JF, Zehir A, Mitchell T, et al. Novel oncogene and tumor suppressor mutations in KIT and PDGFRA wild type gastrointestinal stromal tumors revealed by next generation sequencing. Genes Chromosomes Cancer 2015;54:177-84. 10.1002/gcc.22230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pantaleo MA, Nannini M, Corless CL, et al. Quadruple wild-type (WT) GIST: defining the subset of GIST that lacks abnormalities of KIT, PDGFRA, SDH or RAS signaling pathways. Cancer Med 2015;4:101-3. 10.1002/cam4.325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Andersson J, Sihto H, Meis-Kindblom JM, et al. NF1-associated gastrointestinal stromal tumors have unique clinical, phenotypic, and genotypic characteristics. Am J Surg Pathol 2005;29:1170-6. 10.1097/01.pas.0000159775.77912.15 [DOI] [PubMed] [Google Scholar]
- 23.Ricci R. Syndromic gastrointestinal stromal tumors. Hered Cancer Clin Pract 2016;14:15. 10.1186/s13053-016-0055-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Agaimy A, Vassos N, Croner RS. Gastrointestinal manifestations of neurofibromatosis type 1 (Recklinghausen’s disease): clinicopathological spectrum with pathogenic considerations. Int J Clin Exp Pathol 2012;5:852-62. [PMC free article] [PubMed] [Google Scholar]
- 25.Mussi C, Schildhaus HU, Gronchi A, et al. Therapeutic consequences from molecular biology for gastrointestinal stromal patients affected by neurofibromatosis type 1. Clin Cancer Res 2008;14:4550-5. 10.1158/1078-0432.CCR-08-0086 [DOI] [PubMed] [Google Scholar]
- 26.Kinoshita K, Hirota S, Isozaki K, et al. Absence of c-kit gene mutations in gastrointestinal stromal tumours from neurofibromatosis type 1 patients. J Pathol 2004;202:80-5. 10.1002/path.1487 [DOI] [PubMed] [Google Scholar]
- 27.von Mehren M, Joensuu H. Gastrointestinal stromal tumors. J Clin Oncol 2018;36:136-43. 10.1200/JCO.2017.74.9705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sandrasegaran K, Rajesh A, Rydberg J, et al. Gastrointestinal stromal tumors: clinical, radiologic, and pathologic features. AJR Am J Roentgenol 2005;184:803-11. 10.2214/ajr.184.3.01840803 [DOI] [PubMed] [Google Scholar]
- 29.National Comprehensive Cancer Network. Soft Tissue Sarcoma (Version 2.2018). Available online: https://www.nccn.org/professionals/physician/gls/pdf/sarcoma.pdf, accessed September 22, 2018.
- 30.Trifan A, Singeap AM, Stanciu C. Small bowel stromal tumors: Approach by capsule endoscopy. In: Pascu O. editor. New Techniques in Gastrointestinal Endoscopy. InTech. Available online: http://www.intechopen.com/books/new-techniques-in-gastrointestinalendoscopy/small-bowel-stromal-tumors-approach-by-capsule-endoscopy, accessed on October 28, 2018.
- 31.Nishida T. Therapeutic strategies for wild-type gastrointestinal stromal tumor: is it different from KIT or PDGFRA-mutated GISTs? Transl Gastroenterol Hepatol 2017;2:92. 10.21037/tgh.2017.11.05 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gill AJ, Chou A, Vilain R, et al. Immunohistochemistry for SDHB divides gastrointestinal stromal tumors (GISTs) into 2 distinct types. Am J Surg Pathol 2010;34:636-44. [DOI] [PubMed] [Google Scholar]
- 33.Gaal J, Stratakis CA, Carney JA, et al. SDHB immunohistochemistry: a useful tool in the diagnosis of Carney-Stratakis and Carney triad gastrointestinal stromal tumors. Mod Pathol 2011;24:147-51. 10.1038/modpathol.2010.185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Agaram NP, Wong GC, Guo T, et al. Novel V600E BRAF mutations in imatinib-naïve and imatinib-resistant gastrointestinal stromal tumors. Genes Chromosomes Cancer 2008;47:853-59. 10.1002/gcc.20589 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Evenepoel L, Papathomas TG, Krol N, et al. Toward an improved definition of the genetic tumor spectrum associated with SDH germ-line mutations. Genet Med 2015;17:610-20. 10.1038/gim.2014.162 [DOI] [PubMed] [Google Scholar]
- 36.Jasperson KW, Kohlmann W, Gammon A, et al. Role of rapid sequence whole-body MRI screening in SDH-associated hereditary paraganglioma families. Fam Cancer 2014;13:257-65. 10.1007/s10689-013-9639-6 [DOI] [PubMed] [Google Scholar]
- 37.Weldon CB, Madenci AL, Boikos SA, et al. Surgical management of wild-type gastrointestinal stromal tumors: a report from the National Institutes of Health Pediatric Wild-Type GIST clinic. J Clin Oncol 2017;35:523-8. 10.1200/JCO.2016.68.6733 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kim BJ, Kays JK, Koniaris LG, et al. Understanding the critical role for surgery in the management of wild-type gastrointestinal stromal tumors (GIST). Transl Gastroenterol Hepatol 2017;2:91. 10.21037/tgh.2017.11.03 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Valsangkar N, Sehdev A, Misra S, et al. Current management of gastrointestinal stromal tumors: surgery, current biomarkers, mutations, and therapy. Surgery 2015;158:1149-64. 10.1016/j.surg.2015.06.027 [DOI] [PubMed] [Google Scholar]
- 40.Zhuge Y, Cheung MC, Yang R, et al. Pediatric intestinal foregut and small bowel solid tumors: a review of 105 cases. J Surg Res 2009;156:95-102. 10.1016/j.jss.2009.03.054 [DOI] [PubMed] [Google Scholar]
- 41.Mir O, Cropet C, Toulmonde M, et al. Pazopanib plus best supportive care versus best supportive care alone in advanced gastrointestinal stromal tumours resistant to imatinib and sunitinib (PAZOGIST): a randomised, multicenter, open-label phase 2 trial. Lancet Oncol 2016;17:632-41. 10.1016/S1470-2045(16)00075-9 [DOI] [PubMed] [Google Scholar]
- 42.Falchook GS, Trent JC, Heinrich MC, et al. BRAF mutant gastrointestinal stromal tumor: first report of regression with BRAF inhibitor dabrafenib (GSK2118436) and whole exomic sequencing for analysis of acquired resistance. Oncotarget 2013;4:310-5. 10.18632/oncotarget.864 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Jessen WJ, Miller SJ, Jousma E, et al. MEK inhibition exhibits efficacy in human and mouse neurofibromatosis tumors. J Clin Invest 2013;123:340-7. 10.1172/JCI60578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Tarn C, Rink L, Merkel E, et al. Insulin-like growth factor 1 receptor is a potential therapeutic target for gastrointestinal stromal tumors. Proc Natl Acad Sci USA 2008;105:8387-92. 10.1073/pnas.0803383105 [DOI] [PMC free article] [PubMed] [Google Scholar]