Abstract
Twin births among users of assisted reproductive technology (ART) pose serious risks to both mothers and infants. However, patients may prefer twins and may be unaware of the risks of twin pregnancies. Increasing use of elective single embryo transfers (eSET) through improved patient education could help to reduce twin births and related adverse health consequences. A systematic review of PUBMED and EMBASE databases was conducted to evaluate the effectiveness of patient education among ART users on knowledge of twin pregnancy risks, desire for twins, preference for or use of eSET, and twin pregnancy rates. Of 187 references retrieved, six met the selection criteria. Most focused on patients undergoing their first ART cycle aged < 35 years. Patient education was delivered via written materials, DVDs or discussion. Four studies reporting on knowledge of risks or desire for twins showed significant effects of oral and written descriptions of multiple pregnancy complications, risks of twins versus singletons, and DVDs with factual information. Five studies showed increased eSET use or preference after patients were educated on the risks of multiple pregnancy and success rates associated with different types of ART procedures, when combined with clinic policies that supported single blastocyst transfers or provided options for insurance. In younger ART users, patient education on twin pregnancy risks and success rates of eSET may improve knowledge of twin pregnancy risks and increase use of eSET, and may be important for wider implementation of eSET in countries such as the USA where the use of eSET remains low. Clinic policies of single blastocyst transfers or financial incentives may strengthen these effects.
Keywords: assisted reproductive technology, single embryo transfer, single blastocyst transfer, multiple pregnancy risks, patient education
Introduction
The use of assisted reproductive technology (ART) has increased steadily since 1978, when the first ART-conceived infant was born, both worldwide and in the USA (Adamson et al., 2006). As more than one embryo is often transferred during a procedure, patients who undergo ART treatment are more likely to deliver multiple-birth infants than women who conceive naturally (Stillman et al., 2013). In 2015, 1.7% of all infants born in the USA were conceived via ART, and 35% of ART-conceived infants were born in multiple deliveries, of which the majority (95.3%) were infants from twin deliveries. ART twins accounted for 17% of all twins born in the USA. Compared with ART singletons, ART twins are four-and-a-half times more likely to be born preterm, and more than six times more likely to be low birth weight (Sunderam et al., 2018). As a result, ART has a substantial impact on poor birth outcomes such as preterm birth and low birth weight in the USA (Stillman et al., 2013).
Single embryo transfer (SET) is the most effective method for preventing ART twin pregnancies, reducing the incidence of twins to 0–2% (McLernon et al., 2010, Pandian et al., 2005). According to the American Society for Reproductive Medicine (ASRM) and the Society for Assisted Reproductive Technology (SART), elective SET (eSET) may be appropriate among young (age < 35 years) patients with a favourable prognosis and good-quality embryos (SART/ASRM, P. C, 2012). This clinical practice may be mandatory based on clinic policies (Ryan et al., 2007). Although widely recognized as the best approach to reduce multiple births, except in a few European countries, the use of SET globally and in the USA is still limited (Maheshwari et al., 2011). In 2015, the rate of eSET in the USA was only 35% among women aged < 35 years (Sunderam et al., 2018). Furthermore, eSET rates have remained low despite studies showing comparable pregnancy and livebirth success rates with sequential SET procedures and double embryo transfer (DET) procedures among patients with a good prognosis (Crawford et al., 2016, Stillman et al., 2013). A review of the literature suggests that many patients prefer twins or may be unaware of the high risks associated with twin pregnancies (Leese and Denton, 2010, Murray et al., 2004, Ryan et al., 2007, Stillman et al., 2013). Addressing patient-level factors that affect decisions to transfer two embryos instead of one may be important for wider implementation of eSET. The aim of this systematic review was to evaluate the evidence on effectiveness of enhanced patient education on the following outcomes: (i) patients' knowledge of twin or multiple pregnancy risks or desire for twins or multiples; (ii) preference for or use of eSET procedures; and (iii) twin or multiple pregnancy rates.
Materials and methods
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines for systematic reviews were followed (Liberati et al., 2009, Moher et al., 2009). Two authors (MS, SLB) searched PUBMED independently for articles and abstracts published from 1 January 1978 (the year in which the first ART-conceived baby was born), and EMBASE for publications from inception, through to 16 June 2016. Articles were extracted using keywords and predefined Medical Subject Heading terms (Appendix 1).
Table 1 provides the selection criteria with the PICO (Participants, Interventions, Comparators, Outcomes) elements of the review. Studies were included if they were primary reports of the effects of enhanced (or standard) patient education compared with standard (or no) education on: (i) knowledge of twin or multiple pregnancy risks or desire for twins or multiples; (ii) preference for or use of eSET procedures; or (iii) rate of twin or multiple pregnancies. Studies were excluded for the following reasons: (i) did not include ART patients or patient education; (ii) independent effects of patient education could not be assessed; (iii) no original data; and (iv) no appropriate comparator.
Table 1.
Population, Intervention, Comparison and Outcome (PICO) elements of the review.
| Parameter | Inclusion criteria | Exclusion criteria |
|---|---|---|
| Participants | Patients or couples who use ART | Patients or couples who do not use ART |
| Interventions | Enhanced (or standard) patient education on twin or multiple pregnancy risks | Studies that did not include patient education |
| Comparators | i) Standard education | Studies without these defined comparators |
| ii) No patient education | ||
| iii) Pre-intervention | ||
| Outcomes | i) Knowledge of twin or multiple pregnancy risks or desire for twins or multiples | Studies without these defined outcomes |
| ii) Preference for eSET or use of eSET | ||
| iii) Rates of twin pregnancies and multiple births | ||
| Study design | Any study design between January 1978 and June 2016 that used original data | Studies that did not include original data |
ART, assisted reproductive technology; eSET, elective single embryo transfer.
Data were extracted and recorded in a predesigned evidence table by two authors (MS, SLB). Discrepancies were resolved by discussion and mutual agreement and, if needed, by reaching a consensus with another author (DMK). Abstracted information included first author's name, publication year, study design, study location, period of study, type of publication (full-length article or abstract), study population, type(s) of intervention used and comparators, primary and secondary objectives, and main results.
Two authors (MS, SLB) independently assessed the quality and level of bias of the included studies. Studies were ranked using the grading system developed by the US Preventive Services Task Force (USPSTF) (Harris et al., 2001). Level I studies were properly designed randomized controlled trials (RCTs). Level II-2 studies were well-designed cohort or case–control studies. Level II-3 studies were obtained from multiple time series with or without the intervention. Level III studies were opinions of respected authorities based on clinical experience, descriptive studies, case reports or reports of expert committees. National Institute of Health (NIH)/National Heart Lung and Blood Institute (NHLBI) (http://www.nhlbi.nih.gov/health-pro/guidelines/in-develop/cardiovascular-risk-reduction/tools/) criteria were used to determine the risk of bias. Summary odds ratios (OR) were not calculated, given the heterogeneity of the studies.
Results
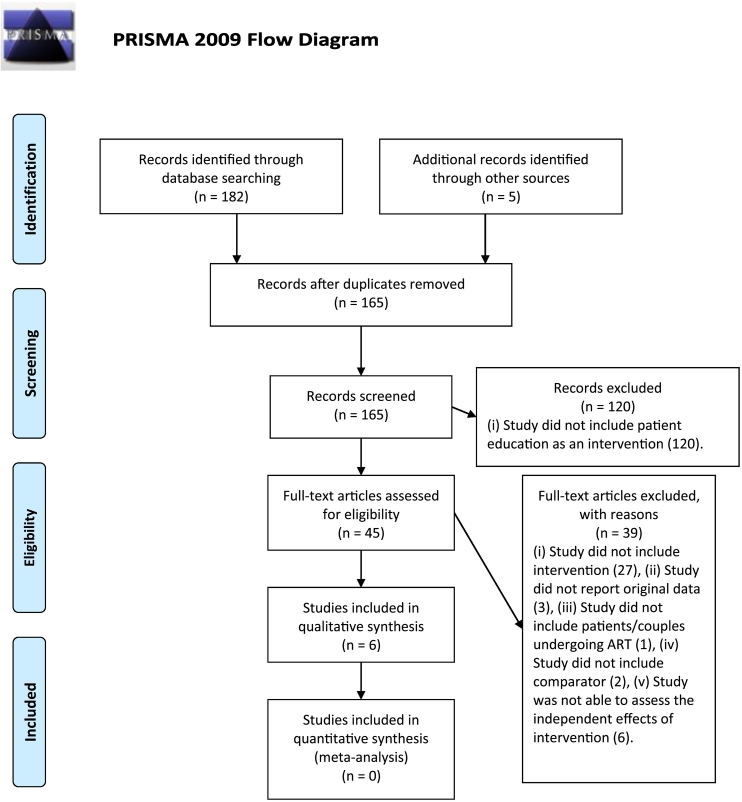
The predefined search headings and terms generated 187 references (113 references in PUBMED, 69 references in EMBASE and five references from the manual search) (Fig. 1). The number of unique references identified after duplicates were removed was 165. Of these, after review of the title and abstract, 120 references were excluded. The remaining 45 references were selected for full-text review. Six studies (five full articles and one abstract) met the inclusion criteria for the review.
Fig. 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses 2009 flow diagram. ART, assisted reproductive technology.
Study characteristics
Six studies reported data from single centres in Australia (n = 1) (Hope and Rombauts, 2010), Canada (n = 1) (Newton et al., 2007), the UK (n = 1) (Murray et al., 2004) and the USA (n = 3) (Arny et al., 2010, Griffin et al., 2012, Ryan et al., 2007) (Table 1), and varied methodologically (Table 2). The review included RCTs (n = 2), retrospective cohort studies (n = 1) and pre–post studies (n = 3). Education was provided through multiple mediums: oral communication (n = 4), written information (n = 6) and audio-visual information (n = 1). Studies also used different types of written communication tools such as cards, brochures and informational handouts. Types of patient education included information on twin or multiple pregnancy risks, advantages of SET, and data on pregnancy success rates associated with SET and DET.
Table 2.
Characteristics of included studies.
| Author, year | Study design, location, study period, publication type | Study population | Intervention, comparator | Primary objective, secondary objective | Main results | Assessment of study |
|---|---|---|---|---|---|---|
| Murray et al. (2004) | RCT: UK. October 2001–April 2003. Full-length article. |
First-time ART couples with no previous pregnancies (n = 272). Response rate: 200/272 = 73.5%. Mean age (female): 33.1–33.9 years. Mean years of infertility (couple): 3.4–4.0 years. | Group 2: Intervention (n = 66). Intervention: Single-page evidence-based document on twin pregnancy (including prematurity and disability) risks, both maternal and fetal/neonatal. Group 3: Intervention + discussion (n = 61). Comparator: Group 1 patients who received standard information provided to all patients (n = 62). |
Primary objective: To evaluate hypothetical acceptability of eSET. eSET preference was defined as couples' acceptability for a policy of eSET. Secondary objective: To evaluate knowledge of risks associated with twin pregnancy. |
Reported couples' joint decisions. Rates of eSET acceptability in Groups 1, 2 and 3 if patients believed that pregnancy rates declined with eSET: 27%, 30% and 32%, respectively (P = 0.39). Rates of eSET acceptability in Groups 1, 2 and 3 if patients believed that pregnancy rates were the same with DET and eSET: 82%, 83% and 87%, respectively (P = 0.76). Rates of eSET acceptability in Groups 1, 2 and 3 if cost of treatment was fixed regardless of number of cycles: 57%, 55% and 65%, respectively (P = 0.73). Knowledge that twins carry higher risks was high in all three groups with no significant differences (Group 1, 95%; Group 2, 98%; Group 3, 98%) (P = 0.26). Percentage of couples indicating that they would not mind having twins was high in all three groups with no significant differences (Group 1, 94%; Group 2, 95%; Group 3, 92%) (P = 0.70). |
Strengths: RCT study. Intervention was pilot tested before the trial and derived from published studies on eSET outcomes. Able to assess impact of educational intervention on eSET preference alone. Weaknesses: 25% (72/272) of eligible couples could not be recruited. Hypothetical acceptability of eSET was examined. Single-centre study. Quality of study: Level I Risk for bias: Moderate |
| Newton et al. (2007) | Pre–post study: Canada. December 2003–December 2004. Full-length article. |
ART couples after fresh transfer. n = 140. Men and women were interviewed separately. Response rate: women, 56% (79/140); men, 38% (53/140). Mean age (female): 33.3 years. Mean years of infertility (female): 3.0 years. |
Intervention: During the interview, brief description of potential increase in complications (pre-eclampsia, low birth weight, postpartum depression) of multiple pregnancy, followed by low-, medium- and high-risk scenarios presented orally and on a card. Comparator: Patient responses to interview questions that preceded provision of information on complications. |
Primary objective: To evaluate desire for different transfer options (including eSET) and twin pregnancies. eSET preference was defined as desire for different transfer options (including eSET). | Reported male and female preferences separately. Presentation of low-risk scenario decreased twin pregnancy desirability among men but not women (P < 0.001). Presentation of medium- and high-risk scenarios decreased twin pregnancy desirability among both men and women (P < 0.001). Presentation of low-, medium- and high-risk scenarios resulted in a significant increase in eSET desirability (P < 0.001) and a significant decrease in DET desirability (P < 0.001). Initial preference for DET > 75%. Perceived increase in chance of pregnancy with DET highly correlated to desire to transfer two embryos (P < 0.05). eSET preferences would decline if patients believed pregnancy rates would be lower with eSET. |
Strengths: Examined patients' reported desirability of embryo transfer practices before and after provision of risk information, and evaluated male and female preferences separately. Able to assess independent effect of patient education on desire for eSET. Weaknesses: Hypothetical scenario provided to patients during interview process immediately after embryo transfer; hence, degree to which findings would apply to actual selection of number of embryos to transfer, and whether reported desirability would change over time, is unknown. Risk information was brief (approximately 125 words). Only legally married or cohabiting couples were included. Lesbian couples and non-English-speaking couples were excluded. Assessment of immediate response to hypothetical risk scenarios. Single-centre study. Self-reported. Small sample size. Quality of study: Level II-3 Risk for bias: High |
| Ryan et al. (2007) | Pre–post study on educational intervention and retrospective cohort study of mSBT clinic policy: USA. September 2004–June 2005. Full-length article. |
Educational campaign included all new ART couples. n = 120. Response rate for completion of both pre- and post-education questionnaires: 110/120 = 92%. Mean age (female): 32.4 years. Mean years of infertility (couple): 2.8 years. Concurrent mSBT policy was targeted at couples at high risk for twins: first-time ART IVF patients aged < 38 years with at least seven embryos, no previous failed cycles and at least one good-quality blastocyst. n = 355 transfer cycles. Mean age: 33 years. Mean years of infertility: not reported. |
Intervention: Multifaceted intervention. One-page educational description of comparative risks of twins versus singletons and discussion with physician; concurrent implementation of mSBT policy for couples at high risk for twin pregnancies. Comparator: Survey responses prior to educational campaign; cycle outcomes prior to mSBT policy. |
Primary objective: To evaluate MPR. Secondary objective: Knowledge of twin risks, desired number of embryos transferred. eSET preference was defined as preference for desired number of embryos transferred. |
Reported couples' joint decisions. Knowledge of twin risks improved after educational intervention (from 61% correct responses about risks prior to intervention to 93% correct responses after intervention; P < 0.05). More patients preferred SET after the educational campaign (61%) than before the campaign (22%) (P < 0.001). Before and after the educational campaign, 75% of patients would choose SET only if pregnancy rates were equivalent to or better than DET. After the educational campaign, 25% of the patients would continue to choose DET over SET even if the pregnancy rates were equivalent. |
Strengths: Compared responses before and after intervention. Used evidence-informed education. Able to assess independent effects of education component on knowledge of twin risks and preference for SET. Weaknesses: Cannot separately evaluate the impact of the educational intervention on MPR as all patients at high risk for twins were subject to clinic's mandatory mSBT policy. No adjustment for confounders. Single-centre study. Quality of study: Level II-3 Risk for bias: Moderate |
| Arny et al. (2010) | Retrospective cohort study: USA. January 2005–December 2009. Conference abstract. | Cycle-specific analysis of ART patients. Blastocyst transfers performed for cycles with more than six top-quality embryos available (1/1/07–6/8/08) or more than four top-quality embryos available (6/9/08–12/31/09). n = 677 autologous cycles, patients aged < 35 years. Mean age and mean years of infertility were not reported. |
Intervention: Multifaceted intervention. eSET with blastocyst transfers for selected patients (initiated in 2007) and enhanced patient education regarding twin pregnancy risks (initiated in January 2009). Education included mandatory lecture, written information on twin pregnancy risks, and sessions with practitioners. Clinic-specific graphs showing association between number of embryos transferred, pregnancy rates and twin rates were provided. Comparator: Cleavage-stage transfers performed during 2005–2006 (with no patient education or policy) and 2007–2008 (policy but no patient education). |
Primary objective: To evaluate use of eSET. Secondary objective: To evaluate PR and twin pregnancies. |
eSET rates increased from 15.7% in 2005–2006 (37/236) to 31.2% in 2007–2008 (88/282) to 46.5% (74/159) in 2009 (P < 0.05). The increase in eSET rates from 31.2% to 46.5% after enhanced patient education was significant (P < 0.0013). Twin pregnancy rates decreased significantly from 35% in 2005–2006 (42/120) to 29.9% in 2007–2008 (43/144) to 20.5% in 2009 (18/88) (P = 0.02). The decrease in twin pregnancy rates from 29.9% to 20.5% after enhanced patient education was not significant. No significant change in pregnancy rate over all time periods. |
Strengths: Compared effectiveness of intervention on rates of eSET, pregnancies, twins and triplets. Able to assess independent effects of education component on eSET rates and twin rates after initiation of single blastocyst policy. Weaknesses: Reports combined eSET rates for cleavage and blastocyst transfers. No information on patient characteristics. Single-centre study. Quality of study: Level II-2 Risk for bias: High |
| Hope and Rombauts (2010) | RCT: Australia. February–October 2007. Full-length article. |
First-time ART couples. n = 215. Response rate: 131/215 = 61%. Mean age (female): 33.6 years (DVD), 34.7 years (brochure). Mean years of infertility (female): 2.5–2.7 years. |
Intervention: Educational DVD containing information on twin pregnancy risks. DVD was 12 min long and included interview with embryologist, obstetrician, and two mothers of twins (one with uncomplicated delivery, the other with preterm delivery) and images of children. Comparator: Brochure containing identical factual information on twin pregnancy risks and challenges as included in DVD. Baseline pre-intervention data also used for comparison with data from DVD and brochure groups. |
Primary objective: To evaluate preference for eSET. Secondary objective: To evaluate changes in knowledge of twin pregnancy risks. eSET preference was defined as preference for eSET. |
Reported couples' joint decisions. Compared with brochure group, DVD group were more likely to agree that twins are usually smaller (P = 0.01), more likely to require neonatal intensive care unit admission (P = 0.044), more likely to have learning disabilities (P = 0.003), less likely to breast feed (P = 0.003), and more likely to have heart abnormalities (P = 0.004). Compared with baseline data, after intervention, a significant increase in acceptability of eSET in brochure group (39.2% to 66.7%) and DVD group (32.6% to 82.6%) but change significantly more pronounced in DVD group (P = 0.014). DVD group were significantly more likely to prefer eSET compared with brochure group among individuals who were initially undecided about the number of embryos to transfer (86% versus 42%; P = 0.0003). Both groups had improved knowledge of twin risks after the intervention. |
Strengths: RCT study with staff blinded to randomization. Able to assess independent effect of education component. Weaknesses: Recruitment bias from excluding non-English-speaking couples and those who did not have access to a DVD player. Sample size not large enough to evaluate statistical significance of actual number of embryos transferred (only 68/100 couples completing study had more than one embryo available). Single-centre study. Did not meet intention-to-treat analysis criteria as not all participants randomized completed the study. Quality of study: Level I Risk for bias: High |
| Griffin et al. (2012) | Pre–post study: USA. September 2008–October 2009. Full-length article. |
Couples undergoing first ART treatment, aged 21–38 years. Clinic had equivalent pregnancy success rates from SET and DET. n = 163. Response rate: 163/500 = 32.6%. Mean age (female): 32.1 years. Mean years of infertility: not reported. |
Intervention: Educational handout describing maternal and fetal risks of twin gestation was assessed alone and in three different payment scenarios (patient pays $15,000 for each cycle, insurance covers up to two cycles, insurance covers unlimited cycles). Comparator: Survey responses prior to reviewing educational handout. |
Primary objective: To evaluate patients' preference of SET versus DET in the context of three different payment scenarios. eSET preference was defined as preference for SET. | Reported couples' joint decisions. Among couples who thought they would conceive with IVF, after education alone, preference for singletons increased significantly from 37% to 67%, and preference for twins decreased significantly from 20% to 12% (P < 0.001). Patients who had no stated preference declined from 43% to 21% (P < 0.001). Education regarding risks of multiple gestations significantly increased preference for SET for all insurance scenarios (P < 0.001). More patients would choose SET in the context of unlimited insurance coverage for ART versus having to pay out of pocket (80% versus 61%) (P < 0.001). |
Strengths: Anonymous survey. Used logistic regression to determine whether patient characteristics were associated with preference for SET. Able to assess impact of educational handout alone and in each payment scenario. Weaknesses: Excluded couples with previous ART. Hypothetical scenarios. Low response rate. Single-centre study. Quality of study: Level II-3 Risk for bias: High |
ART, assisted reproductive technology; BT, blastocyst transfer; CPR, clinical pregnancy rate; DET, double embryo transfer; eSBT, elective single blastocyst transfer; eSET, elective single embryo transfer; ICSI, intra-cytoplasmic sperm injection; mSBT, mandatory single blastocyst transfer; MPR, multiple pregnancy rate; PGD, pre-implantation genetic diagnosis; RCT, randomized controlled trial; SBT, single blastocyst transfer; SET, single embryo transfer.
Three studies reported on the effects of patient education alone (Hope and Rombauts, 2010, Murray et al., 2004, Newton et al., 2007). Two studies reported on the effects of patient education and mandatory single blastocyst transfer policies (Arny et al., 2010, Ryan et al., 2007). One study reported on the effects of patient education and different hypothetical levels of insurance availability (Griffin et al., 2012). Four studies reported couples' joint decisions (Griffin et al., 2012, Hope and Rombauts, 2010, Murray et al., 2004, Ryan et al., 2007), and one study reported male and female preferences separately (Newton et al., 2007). Four studies reported on the duration of infertility, which ranged from 2.5 years to 4.0 years (Hope and Rombauts, 2010, Murray et al., 2004, Newton et al., 2007, Ryan et al., 2007).
Study quality
The evidence from the included studies was graded according to USPSTF standards (Table 2). The internal validity of the studies was assessed using NIH/NHLBI tools. Studies ranged from moderate to high risk of bias.
Outcome measures
Knowledge of twin pregnancy risks or desire for twins
Five studies examined the effects of patient education on knowledge of twin pregnancy risks or desire for twins (Griffin et al., 2012, Hope and Rombauts, 2010, Murray et al., 2004, Newton et al., 2007, Ryan et al., 2007). Of these, four studies reported the effects of patient education alone (Griffin et al., 2012, Hope and Rombauts, 2010, Murray et al., 2004, Newton et al., 2007), and the fifth study reported on the effects of patient education on new ART patients while a clinic policy of mandatory single blastocyst transfers for patients at high risk for twin pregnancies was initiated (Ryan et al., 2007).
Patient education
An RCT conducted in the UK compared the effects of patient education on knowledge about risks of twin pregnancies in three groups, and found no significant differences in knowledge that twins carry higher risks among the three groups (Murray et al., 2004). Group 1 received standard clinic information (control), Group 2 received standard information plus an additional information leaflet about twin pregnancy risks including maternal and fetal/neonatal risks, and Group 3 received the same information as Group 2 plus an additional discussion session with a nurse. When asked whether twins carried greater risks, 95% of Group 1 said yes, versus 98% in Groups 2 and 3. When asked whether they would prefer twins to no pregnancy, 97–100% responded affirmatively. Additionally, 92–95% of the couples in the three groups said that they would not mind having twins.
In a pre–post study conducted in Canada, three potential complications of multiple pregnancies (pre-eclampsia, low birth weight and postpartum depression) were described orally and visually with cards during an interview, which occurred immediately after embryo transfer (Newton et al., 2007). Three different risk scenarios were then presented for these complications, representing low risk (5%, 10% and 15%, respectively), medium risk (10%, 30% and 30%, respectively) and high risk (20%, 60% and 60%, respectively), with medium risk being most representative of an accurate scenario for multiple birth. After the presentation of each risk-level scenario, participants rated their desire for transferring one to four embryos and for twin pregnancies. Compared with the responses obtained before the interview, responses following scenarios described as medium or high risk for pre-eclampsia, low birth weight and postpartum depression showed a significant decrease in the desire for twin pregnancies (P < 0.001) among both men and women. However, among men, even scenarios showing low risk for pre-eclampsia, low birth weight and postpartum depression significantly decreased the desire for twins (P < 0.05).
A third study, an RCT conducted in Australia, compared the effectiveness of an educational DVD with the effectiveness of a brochure, both describing identical factual information on the risks associated with twin pregnancies (Hope and Rombauts, 2010). The DVD included interviews with an embryologist, obstetrician and two mothers of twins (one with an uncomplicated twin pregnancy and the other with a twin pregnancy resulting in preterm delivery). The DVD also included images of the twins from the uncomplicated delivery at play, and images of the preterm twins soon after birth and during neonatal intensive care. Results showed significantly improved knowledge of twin pregnancy risks in the DVD and brochure groups relative to baseline; however, compared with the brochure group, those who saw the DVD were more likely to indicate that twins are usually smaller (P = 0.01), more often require neonatal intensive care (P = 0.04), more often have learning disabilities (P = 0.003), and more often have heart abnormalities (P = 0.004).
A pre–post study in the USA, conducted in a clinic with equivalent SET and DET pregnancy rates, used educational handouts on the risks of twin pregnancies during counselling (Griffin et al., 2012). Assuming successful conception with in-vitro fertilization (IVF), after education, the preference for singletons increased significantly from 37% to 67%, and the preference for twins decreased significantly from 20% to 12% (P < 0.001).
Patient education with a single blastocyst transfer policy
Another pre–post study in the USA assessed the effects of patient education on knowledge of twin pregnancy risks while a clinic-wide mandatory single blastocyst transfer policy was implemented (Ryan et al., 2007). This study found that a one-page summary of comparative health risks of twins versus singletons coupled with a discussion with a physician significantly improved knowledge of twin pregnancy risks among all new patients, from 61% pre-intervention to 93% post-intervention (P < 0.05).
Preference for eSET procedures and increased use of eSET
All six studies reported the effects of patient education on preference for eSET procedures or use of eSET. Of these, three studies investigated the effects of patient education alone (Hope and Rombauts, 2010, Murray et al., 2004, Newton et al., 2007), two studies reported the effects of patient education concurrently or after initiation of a single blastocyst transfer policy (Arny et al., 2010, Ryan et al., 2007), and one study reported the effects of patient education in the context of hypothetical insurance scenarios (Griffin et al., 2012).
Patient education
The RCT conducted in the UK that compared the effects of two enhanced patient education strategies with the effects of standard written clinical information provided to all IVF patients did not find significant associations between these interventions and the acceptability of eSET (Murray et al., 2004). Among patients who believed that pregnancy rates for SET approached those of DET, the percentage of patients that reportedly would find eSET acceptable was 83% for Group 2, 87% for Group 3 and 82% for Group 1 (P = 0.76). Among patients who believed that pregnancy rates would decline with eSET, acceptability of eSET did not differ by group (standard, 27%; additional written information, 30%; additional written information plus nurse discussion, 32%) (P = 0.39). However, a lower rate of eSET acceptability was found in this group than among those who believed that SET and DET pregnancy rates were similar.
The Canadian study showed that presentation of low-, medium- and high-risk information increased the desirability of eSET (P < 0.001) and decreased the desirability of DET (P < 0.001) compared with baseline preferences (Newton et al., 2007). Initial preference for DET was high (> 75% among women) and highly correlated with a desire to transfer two embryos to maximize the chance of pregnancy at baseline (r = 0.26, P < 0.05); however, although one-third of patients viewed eSET positively, another one-third of patients had an extremely negative opinion of this option.
The RCT conducted in Australia noted a significantly higher preference for eSET following each intervention compared with baseline, but the increase in preference was more pronounced in the DVD group (33% pre-intervention, 83% post-intervention) than in the brochure group (39% pre-intervention, 67% post-intervention) (P = 0.014) (Hope and Rombauts, 2010).
Patient education with a single blastocyst transfer policy
One USA study found that more patients preferred SET after the educational campaign (61%) than before the campaign (22%) (P < 0.001) (Ryan et al., 2007). However, before and after the educational campaign, 75% of the patients would choose SET only if pregnancy rates were equivalent to or better than DET.
Another US study demonstrated the effects of patient education after initiation of a single blastocyst transfer policy on the use of eSET (Arny et al., 2010). In this study, single blastocyst transfers were offered to selected patients aged < 35 years. Patient education consisted of mandatory lectures, individual sessions with physicians or nurses, written information regarding risks associated with twin pregnancies, and use of clinic-specific bar graphs providing visual information of the association between number of embryos transferred, and pregnancy rates and twin rates. This study showed an increase in eSET rates (reported jointly for cleavage and blastocyst transfers) from 15.7% in the pre-intervention period (2005–2006) to 31.2% after adoption of a single blastocyst transfer policy in 2007–2008, and to 46.5% after education was coupled with a single blastocyst transfer policy in 2009 (P < 0.05). The increase in eSET rate from 31.2% (after initiation of a single blastocyst transfer policy) to 46.5% (with a single blastocyst transfer policy and education) was also significant (P < 0.0013).
Patient education with financial incentives
Another US pre–post study assessed the effects of patient education under three hypothetical insurance scenarios (Griffin et al., 2012). Patients were presented with hypothetical options for three levels of insurance coverage (up to $15,000 out-of-pocket costs per cycle, two cycle coverage and unlimited coverage). Preference for SET increased significantly (P < 0.001) for all three groups after education on the risks of twin pregnancies relative to responses prior to the educational intervention.
Rates of twin pregnancies
Only one study reported the effects of patient education on the twin pregnancy rate (Arny et al., 2010). This study failed to report a significant decline in the twin pregnancy rate after education following initiation of a single blastocyst transfer policy.
Discussion
Among younger patients undergoing their first treatment cycle, patient education may increase awareness of success rates of livebirths of SET versus DET, and maternal and infant health risks of twin pregnancies, and also increase the incidence of single blastocyst transfer procedures. Clinic policies and the availability of insurance coverage may further support these effects.
Patient education was delivered in multiple formats including mandatory lectures and DVDs. Effective interventions included: presentation of medium- and high-risk scenarios for potential pregnancy complications associated with multiple pregnancies, such as pre-eclampsia, low birth weight and postpartum depression, followed by visual reinforcement with cards; one-page educational description of comparative risks of twins versus singletons coupled with discussion; educational handouts describing maternal and fetal risks of twin pregnancies; factual information; and patient education that was combined with clinic policies promoting single blastocyst transfers or insurance options.
Four out of five studies that reported on knowledge of twin pregnancy risks or desire for twins showed that patient education had a significant impact. Audio-visual education was shown to be particularly effective, as this approach may help patients to personalize risks. Two important findings are that patient education on comparative risks of twins versus singletons may improve knowledge of twin pregnancy risks, and that a patient's preference for twins may decrease after education if the eSET and DET pregnancy rates are equivalent.
Further, desire for twins among men decreased after discussions of all levels of risk, whereas only medium- or high-risk scenarios reduced women's desire for twins, a finding that may be explained by higher baseline understanding of twin pregnancy risks among women or a stronger desire for children (Newton et al., 2007). In this study, the intervention took place after embryo transfer; whether such an approach would also be effective if implemented prior to embryo transfer was not reported in this study.
Five of the six studies that reported on eSET use or preference showed positive impacts of patient education. Although a small percentage of patients may be opposed to eSET, many would choose eSET if the success rates of SET and DET were equivalent. The study that failed to show a significant impact of patient education found that perceived eSET acceptability rates were higher among those who believed that pregnancy rates were similar between DET and eSET as opposed to those who believed that pregnancy rates declined with eSET, suggesting that acceptability may be associated with perceptions of lower pregnancy rates associated with eSET (Murray et al., 2004). Although the intrinsic desire for twins may be higher among women, the desire to transfer two embryos may also be correlated with perceived increase in the chance of pregnancy with DET (Newton et al., 2007).
One notable finding was that the effects of clinic policies on single blastocyst transfers may be strengthened with education, resulting in increased use of eSET (Arny et al., 2010). Another notable finding is that patient education can significantly increase preference for eSET in the context of both medium and unlimited insurance coverage for ART compared with no insurance (Griffin et al., 2012).
Several studies relevant to this review were excluded because the effects of patient education could not be assessed independently from additional components of the study intervention (Table 3). These studies, conducted in several different countries, showed that educational interventions coupled with clinic policies (Khalaf et al., 2008, Kodama et al., 2009) or financial incentives (Coetzee et al., 2007, Kreuwel et al., 2013, van Peperstraten et al., 2010) resulted in increases in single blastocyst transfers, and suggest that, globally, similar factors drive patient decisions concerning how many embryos to transfer and the types of incentives that affect those decisions. While unable to disentangle the independent effects of education, in general, these studies complement the findings in this systematic review, that information on comparative success rates by procedures, clinic policies and financial options may strengthen the effects of patient education among ART users.
Table 3.
Additional relevant studies that included patient education as part of a multifaceted intervention.
| Author, year | Study design, location, study period, publication type | Study population | Intervention, comparator | Primary objective, secondary objective | Main results | Assessment of study |
|---|---|---|---|---|---|---|
| Marek et al. (2005) | Retrospective cohort study: USA. Conference abstract. |
ART patients aged ≤ 37 years and patients using donor oocytes with at least two freeze-quality blastocysts. Cycle-specific analysis. n = 263 cycles (pre-intervention: 152 cycles, post-intervention: 111 cycles). Mean age and mean years of infertility were not reported. |
Intervention: Multifaceted intervention. Comprehensive educational programme on twin risks. Financial incentives for SBT: free cryopreservation services and free subsequent frozen–thawed BT if needed. Comparator: Patients receiving standard care (prior to implementation of the incentive programme). |
Primary objective: To evaluate use of SBT. | SBT rates for autologous cycles almost doubled (33–60%; P < 0.01) after incentive programme. SBT rates for donor cycles increased from 27% to 64% (P < 0.01). Ongoing pregnancy rates remained stable. |
Strengths: Reports rates of SBT, pregnancies and multiple births before and after intervention. Distinguishes between autologous and donor cycles. Patient education included risks and complications of twin pregnancies. Weaknesses: Small sample size. No adjustment for patient characteristics. Unknown whether findings represent a single clinic or multiple centres. No information on dates of recruitment or outcomes. Not able to assess independent effect of education component. Quality of study: Level II-2 Risk for bias: High |
| Coetzee et al. (2007) | Retrospective cohort study: New Zealand. 2003–2004. Full-length article. |
Publicly funded and private ART patients. Cycle-specific analysis. n = 280 in 2003 and n = 298 in 2004. Mean age: 36.2 years (private insurance), 33.5 years (public insurance). Mean years of infertility: not reported. |
Intervention: Multifaceted intervention. Implementation of clinic-wide SET policy in 2004, written and verbal information about age-dependent twin pregnancy risks, advantages of SET, twin pregnancy risks, and free funded second cycle. Comparator: Patients receiving standard care (typically DET) in 2003. |
Primary objective: To evaluate use of SET. | Rates of SET increased from 14% to 49% from 2003 to 2004. Among women aged ≤ 35 years, SET increased from 13% to 62%. The increase was greater among publicly funded patients (from 19% to 63%) than private patients (from 5% to 30%). |
Strengths: Reports both rates of eSET and pregnancies by age before and after intervention, and by funding status. Weaknesses: Donor egg cycles were excluded. No adjustment for patient characteristics. Single-centre study. Not able to assess independent effect of education component. Quality of study: Level II-2 Risk for bias: High |
| Khalaf et al. (2008) | Retrospective cohort study: UK. July 2004– June 2007. Full-length article. |
Good-prognosis ART patients (age < 40 years and extra embryos available for cryopreservation). Cycle-specific analysis, pre- and post-intervention n = 2451 [n = 1198 in 2004/2005 (pre-intervention) and n = 1253 in 2006/2007 (post-intervention)]. Mean age (female): 35.2 years (pre-intervention) and 35.8 years (post-intervention). Mean years of infertility: not reported. |
Intervention: Multifaceted intervention 2006/2007. Selective SBT with an educational programme on multiple pregnancy risks and advantages of SBT. Audio-visual and written information, provided at monthly patient information seminars and during patient consultations. Information was also displayed in waiting areas. Comparator: Good-prognosis patients receiving standard care in 2004/2005 (transfer of up to three cleavage-stage embryos). |
Primary objective: To evaluate CPR and MPR. |
The proportion of eSET increased significantly from 1.9% (5/263) in 2004/2005 to 38% (129/342) in 2006/2007 (RR 21.9, 95% CI 9.1–52.7; P < 0.001). CPR increased from 27% pre-intervention to 32% post-intervention (P = 0.015) due to higher CPR in women with blastocyst transfer. MPR declined significantly from 32% to 17% (P < 0.001). |
Strengths: Large sample size. Reports actual rather than hypothetical scenario. Weaknesses: Only 9% of cycles started in 2006/2007 had an elective SBT. Cycles involving PGD, donated oocytes or cryopreserved embryos were excluded. Patient perception of educational materials was not assessed, and effects of educational component were not assessed separately from effects of SBT strategy. Measures of association were not adjusted for confounders. Single-centre study. Not able to assess independent effect of education component. Quality of study: Level II-2 Risk for bias: High |
| Kodama et al. (2009) | Retrospective cohort study: Japan. December 2002–December 2003, January 2004–April 2007, May 2007–December 2008. Conference abstract. |
ART patients. Cycle-specific analysis. n = 404 cycles. Mean age (female): 34.3 years (Period I), 34.4 years (Period II) and 36.5 years (Period III). Mean years of infertility: not reported. |
Intervention: Multifaceted intervention. Educational counselling on twin pregnancy risks and clinic's eSBT policy. The study was divided into three time periods. Period I: 12/2002 to 12/2003 (n = 64) with a dual BT policy. Period II: 1/2004 to 4/2007 (n = 188) with eSBT for women aged < 36 years with at least two top-quality blastocysts and less than three failed BT cycles. Period III: 5/2007 to 12/2008 (n = 152) with eSBT for women aged < 40 years with at least two lower-quality blastocysts and less than three failed BT cycles and counselling about twin risks. Period III included educational counselling. Comparator: Transfers that occurred under dual BT policy with no educational counselling. |
Primary objective: To evaluate MPR and PR. | The number of BTs in Period III (1.1 ± 0.03) was lower than in Periods I (1.8 ± 0.05) and II (1.5 ± 0.03) (P < 0.001). PRs were similar for these periods. MPRs in Period III (1.8%) were lower than in Periods I (28%) and II (13%) (P < 0.001). |
Strengths: Compared effectiveness of eSBT and counselling on twin risks in two age groups: < 36 and < 40 years. Not able to assess independent effects of education component on MPRs. Weaknesses: No details of educational counselling provided. No adjustment for potential confounders. Single-centre study. Quality of study: Level II-2 Risk for bias: High |
| van Peperstraten et al. (2010) | RCT: Netherlands. November 2006–December 2008. Full-length article. | ART couples from five clinics undergoing first cycle or first cycle following successful previous ART, women aged < 40 years. n = 344. Response rate: 308/344 = 92.4%. Mean age (female): 32.0 years (intervention group), 31.7 years (control group). Mean years of infertility (couple): 2.2–2.3 years. |
Intervention: Multifaceted intervention (decision aid, reimbursement offer for fourth ART cycle if SET for first two cycles with no resulting pregnancy, in person discussion of decision and reimbursement offer with nurse, followed by standard care counselling and phone call follow-up from nurse). Comparator: Standard counselling. |
Primary objective: To evaluate the use of SET. | After the first treatment cycle, higher SET rate in intervention group (43%) versus control group (32%) (P = 0.05). After the second treatment cycle, higher SET rate in intervention group (26%) versus control group (16%) (P = 0.20). After the first treatment cycle, twin pregnancies were lower in the intervention group (n = 6) compared with the control group (n = 10), but this difference was not statistically significant (P = 0.33). |
Strengths: RCT study encompassing five clinics. Decision aid developed from evidence-based criteria. Demonstrates cost effectiveness of SET, and cost per couple was lower in the intervention group despite free fourth cycle. Weaknesses: Limited generalizability to countries with less than three cycles of publicly funded ART cycles. Difference in SET use among two groups was lower than expected based on power calculations and sample size. Higher SET rates in intervention group could be due to reimbursement offer. Self-report bias. Greater than 20% dropout rate. Not able to assess impact of decision aid separate from multicomponent intervention Quality of study: Level I Risk for bias: Moderate |
| Kreuwel et al. (2013) | Retrospective cohort study: Netherlands. November 2006–December 2008 Full-length article. |
Couples undergoing first ART cycle, aged < 40 years. n = 308. Response rate: 222/308 = 72.1%. Mean age (female): 31–32 years. Mean years of infertility (couple): 2 years. |
Intervention: Multifaceted intervention (standard, decision aid plus free fourth ART cycle (n = 20), decision aid plus free fourth ART cycle with counselling by ART nurse (n = 37), decision aid plus free fourth ART cycle, counselling by ART nurse and follow-up phone call (n = 52). The decision aid booklet contained information about chances of and risks of singletons versus twin pregnancies. Comparator: Patients receiving standard care (n = 113). |
Primary objective: To evaluate eSET rate for each intervention type. Secondary objective: To evaluate the degree to which intervention strategy influenced decision on number of embryos to transfer. |
After adjustment for baseline characteristics, there was no difference in eSET rate for any of the intervention strategies, compared with standard care. Couples rated physician advice, decision aids and counselling as most important elements in decision making; reimbursement offer and phone call were ranked as least important compared with physician advice, decision aids and counselling (P < 0.001). |
Strengths: Eligible couples selected from previously conducted RCT; data analysed were obtained in RCT. Able to evaluate relative importance of different types of interventions in patient decision making. Multivariate analyses used to adjust for confounders. Multi-centre study. Weaknesses: Potential bias in the selection of couples into different groups. Limited generalizability for countries that do not offer public funding of three ART cycles. No information on dates of recruitment or outcomes. Quality of study: Level II-2 Risk for bias: Moderate |
ART, assisted reproductive technology; BT, blastocyst transfer; CI, confidence interval; CPR, clinical pregnancy rate; DET, double embryo transfer; eSBT, elective single blastocyst transfer; eSET, elective single embryo transfer; ICSI, intra-cytoplasmic sperm injection; mSBT, mandatory single blastocyst transfer; MPR, multiple pregnancy rate; PGD, pre-implantation genetic diagnosis; RCT, randomized controlled trial; RR, relative risk; SBT, single blastocyst transfer; SET, single embryo transfer.
Specifically, these studies showed that, when coupled with patient education, monetary incentives may be effective in increasing the use of eSET in countries as culturally diverse as the USA, Japan and New Zealand. In the USA, one study found that patients who were offered a monetary incentive programme that included free cryopreservation, limited storage of blastocysts, and a subsequent frozen cycle at no additional cost if the first cycle did not result in a live birth, elected single blastocyst transfers more often than patients without such incentives (58.8% versus 33.3%; P < 0.01) (Marek et al., 2005). Another study in New Zealand compared the effects of a clinic-wide SET policy compared with standard care, which was typically DET, and reported an overall increase in SET uptake after the introduction of patient education coupled with a second free cycle (Coetzee et al., 2007). A third study in Japan following the implementation of an elective single blastocyst policy paired with patient education on the risks of twin pregnancies showed a decline in multiple pregnancy rates from 28% in Period I (DET policy) to 13% in Period II (single blastocyst policy for women aged < 36 years) and to 1.8% in Period III (single blastocyst policy for women aged < 40 years coupled with education) (P < 0.001) (Kodama et al., 2009).
Conversely, patient education had limited effects on patient preference for eSET in countries with greater availability of public funding for ART treatment, such as Denmark and Sweden (Blennborn et al., 2005, Højgaard et al., 2007). The Danish study found that, after receiving written information on the complications of twin pregnancies followed by an oral consultation with doctors and nurses further emphasizing the risks, 58.7% of couples reported that they preferred twins while 37.9% preferred having one child at a time. Furthermore, couples with no children significantly preferred twins [OR 2.01, 95% confidence interval (CI) 1.28–3.16] compared with those who had children (Højgaard et al., 2007). There were many reasons for the preference for twins, including desire for children to have siblings (23.3%), positive attitude towards twins (22.5%) and a wish for fewer ART treatments (19.3%). A majority (75%) of patients planned to transfer two embryos at the next treatment after the educational intervention, and suggested that a mandatory single blastocyst transfer policy would be in conflict with patient interests. Findings from the Swedish study suggested that, compared with patients who transferred two embryos, there was no difference in knowledge of increased risks associated with multiple pregnancies among those who transferred a single embryo (adjusted OR 1.1, 95% CI 0.66–2.00), while a perceived higher chance of pregnancy significantly affected the decision to transfer one versus two embryos (adjusted OR 0.13, 95% CI 0.05–0.29) (Blennborn et al., 2005). Older women (mean age 36 years) preferred DET, while younger women (mean age 34 years) with extra embryos available preferred eSET. Notably, partner influence was most strongly associated with the decision to transfer one versus two embryos. The reason for patient preferences varied between these studies. One study suggested that a desire for twins was intrinsic and strong among couples who had no children (Højgaard et al., 2007). The second study suggested that patients chose two embryos due to a perceived higher chance of pregnancy (Blennborn et al., 2005). The studies were conducted in Denmark and Sweden where costs of IVF may be of secondary importance due to the availability of publicly funded cycles. This is in sharp contrast to the USA, where universal public funding of ART cycles is not available.
Overall, these studies demonstrated that financial costs play a key role in countries without public funding for ART treatments, and could be offset through different mechanisms including increasing the availability of public funding for IVF, insurance coverage and clinic-sponsored incentives (e.g. free cryopreservation services and free transfer of cryopreserved embryos), and thereby change patient preferences (Coetzee et al., 2007, Griffin et al., 2012, Marek et al., 2005). The effects of financial incentives may be weaker in countries that provide free publicly funded IVF cycles and have higher uptake of SET, such as Denmark, Sweden and the Netherlands, compared with countries with no universal public funding for IVF (Blennborn et al., 2005, Højgaard et al., 2007, Kreuwel et al., 2013). Furthermore, regardless of funding incentives, the desire for biological children may over-ride concerns about the risks of twin pregnancies among patients, especially women, even after education. To ensure treatment success, patients may opt to take a more risky approach that can endanger the health of the mother and infants by transferring multiple embryos, rather than forego the chance of conceiving their own biological child. Therefore, patient education should continue to focus on the risks of twin pregnancies, and explore more personalized ways which may be more effective to communicate such risks.
Strengths and limitations
As far as is known, this is the first systematic review of the effectiveness of patient education on desire for twins, knowledge of the risks of twin pregnancies, and use of eSET. Few studies have been conducted in this area. This study addresses an important gap in the current literature.
One limitation of this review is that the included studies were old and did not assess the use of web-based educational materials. Additionally, several relevant studies were excluded from the systematic review as they did not fulfil the PICO requirements, either because they did not include a comparator or they did not report on the independent effects of patient education. A few studies were excluded as they were too small to be relevant.
Additionally, none of the included studies examined the effects of patient characteristics, such as years of infertility, on their embryo transfer choices. Longer durations of infertility can augment both the desire for biological children as well as stress associated with failed treatments. Research shows that almost 20–50% of IVF patients reported at least mild-to-moderate symptoms of stress-associated depression, which can worsen with unsuccessful treatment cycles. The findings suggest that patient education is complex as patients often try to balance costs with their desire for children, which can be stressful. Future studies should incorporate information on managing stress in patient education, as it may be a salient factor in how patients make decisions regarding the number of embryos transferred.
Studies not included but relevant to this review provided important insights on the effectiveness of multifaceted interventions that coupled education with single blastocyst transfer strategies or financial incentives on reducing the desire for twins and increasing the use of eSET. More studies that can differentiate between the effects of patient education and the effects of SET policies and/or financial incentives are needed.
Further, all included studies were conducted in single centres that are more likely to treat homogenous patients, and therefore are less likely to be broadly applicable. The studies also varied methodologically. The evidence from RCTs was mixed. Some studies addressed hypothetical scenarios that may vary from actual transfer choices. The quality of the studies also varied, with four studies showing high risk of bias.
Implications
The summarized evidence may have implications for ART patient education, especially in the USA where national eSET rates remain low, even among patients with a good prognosis, and twins still account for the majority of ART-conceived multiple births (95%) (Sunderam et al., 2018). Studies included in this review suggested that patient education and clinic policies can increase the use of eSET, and some patients may choose SET over DET with economic incentives.
Conclusions
Couples in the USA seeking ART treatment may be influenced by the high out-of-pocket cost per cycle and may be more concerned about pregnancy rates per cycle (Lemos et al., 2013) rather than asociated risks. This review suggests that new approaches to patient education programmes are needed that can be implemented in clinical settings. Such programmes should focus on the effectiveness of blastocyst transfers in improving pregnancy rates and achieving livebirths, and should be coupled with financial incentives that alleviate or remove economic barriers to the use of eSET among patients with a good prognosis. Patient education should also address gender differences in attitudes towards twin pregnancy risks, and more attention should be focused on educating women about the medical risks to both the mother and infants (Blennborn et al., 2005, Højgaard et al., 2007, Newton et al., 2007).
Additionally, a core part of patient education should help to raise awareness of the risks of twin pregnancies, which are generally not perceived as high risk despite the body of evidence showing significantly higher morbidity and mortality rates for the mother and infants. In particular, patient education of potential advantages of single blastocyst transfer may increase the acceptability of eSET among patients with a good prognosis, especially among those patients who may otherwise be less aware of these treatment options.
Acknowledgements
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Biography

Dr. Saswati Sunderam is a health scientist in the Division of Reproductive Health at the Centers for Disease Control and Prevention (CDC). She is the lead author of Assisted Reproductive Technology (ART) Surveillance Summary, an annual CDC Morbidity and Mortality Weekly Report publication. This publication is critical for monitoring multiple births and preterm births in states. In 2015, ART Surveillance Summary was cited by the Journal for Obstetrics and Gynecology as one of the four best articles in the area of assisted reproduction and multiple pregnancy reduction published in the past year.
Declaration: The authors report no financial or commercial conflicts of interest.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.rbms.2018.10.017.
Appendix 1
PUBMED keywords used were (Patient attitudes OR patient education OR patient preference) AND (embryo transfer OR single embryo transfer) AND (twins OR twin gestation OR twin birth OR twin pregnancy OR multiple birth OR multiple gestation OR multiple pregnancy OR in vitro fertilization OR assisted reproductive technology. MESH terms used were: (((‘patients’[MeSH Terms] OR ‘patients’[All Fields] OR ‘patient’[All Fields]) AND (‘attitude’[MeSH Terms] OR ‘attitude’[All Fields] OR ‘attitudes’[All Fields])) OR (‘patient education handout’[Publication Type] OR ‘patient education as topic’[MeSH Terms] OR ‘patient education’[All Fields]) OR (‘patient preference’[MeSH Terms] OR (‘patient’[All Fields] AND ‘preference’[All Fields]) OR ‘patient preference’[All Fields])) AND ((‘embryo transfer’[MeSH Terms] OR (‘embryo’[All Fields] AND ‘transfer’[All Fields]) OR ‘embryo transfer’[All Fields]) OR (‘single embryo transfer’[MeSH Terms] OR (‘single’[All Fields] AND ‘embryo’[All Fields] AND ‘transfer’[All Fields]) OR ‘single embryo transfer’[All Fields])) AND ((‘twins’[MeSH Terms] OR ‘twins’[All Fields]) OR ((‘twins’[MeSH Terms] OR ‘twins’[All Fields] OR ‘twin’[All Fields]) AND (‘pregnancy’[MeSH Terms] OR ‘pregnancy’[All Fields] OR ‘gestation’[All Fields])) OR ((‘twins’[MeSH Terms] OR ‘twins’[All Fields] OR ‘twin’[All Fields]) AND (‘parturition’[MeSH Terms] OR ‘parturition’[All Fields] OR ‘birth’[All Fields])) OR (‘pregnancy, twin’[MeSH Terms] OR (‘pregnancy’[All Fields] AND ‘twin’[All Fields]) OR ‘twin pregnancy’[All Fields] OR (‘twin’[All Fields] AND ‘pregnancy’[All Fields])) OR (‘multiple birth offspring’[MeSH Terms] OR (‘multiple’[All Fields] AND ‘birth’[All Fields] AND ‘offspring’[All Fields]) OR ‘multiple birth offspring’[All Fields] OR (‘multiple’[All Fields] AND ‘birth’[All Fields]) OR ‘multiple birth’[All Fields]) OR (‘pregnancy, multiple’[MeSH Terms] OR (‘pregnancy’[All Fields] AND ‘multiple’[All Fields]) OR ‘multiple pregnancy’[All Fields] OR (‘multiple’[All Fields] AND ‘gestation’[All Fields]) OR ‘multiple gestation’[All Fields]) OR (‘pregnancy, multiple’[MeSH Terms] OR (‘pregnancy’[All Fields] AND ‘multiple’[All Fields]) OR ‘multiple pregnancy’[All Fields] OR (‘multiple’[All Fields] AND ‘pregnancy’[All Fields])) OR (‘in vitro fertilisation’[All Fields] OR ‘fertilization in vitro’[MeSH Terms] OR (‘fertilization’[All Fields] AND ‘vitro’[All Fields]) OR ‘fertilization in vitro’[All Fields] OR (‘vitro’[All Fields] AND ‘fertilization’[All Fields]) OR ‘in vitro fertilization’[All Fields]) OR (‘reproductive techniques, assisted’[MeSH Terms] OR (‘reproductive’[All Fields] AND ‘techniques’[All Fields] AND ‘assisted’[All Fields]) OR ‘assisted reproductive techniques’[All Fields] OR (‘assisted’[All Fields] AND ‘reproductive’[All Fields] AND ‘technology’[All Fields]) OR ‘assisted reproductive technology’[All Fields])) AND ((‘1978/01/01’[PDAT]: ‘2016/06/16’[PDAT]) AND ‘humans’[MeSH Terms]).
The search was not limited to a specific study design. Search was restricted to 1/1/1978–06/16/2016; species – human.
Appendix 2. Supplementary data
PRISMA Checklist.
References
- Adamson G.D., de Mouzon J., Lancaster P., Nygren K.G., Sullivan E., Zegers-Hochschild F. World collaborative report on in vitro fertilization, 2000. Fertil. Steril. 2006;85(6):1586–1622. doi: 10.1016/j.fertnstert.2006.01.011. [DOI] [PubMed] [Google Scholar]
- Arny M.J., Duncan D., E.M., T., S., L., D.R., G., K.A., L. Increasing elective single embryo transfers and reducing twin pregnancies without affecting pregnancy rate in patients < 35 years old. Fertil. Steril. 2010;94(2) (Supplement, September 2010) [Google Scholar]
- Blennborn M., Nilsson S., Hillervik C., Hellberg D. The couple's decision-making in IVF: one or two embryos at transfer? Hum. Reprod. 2005;20(5):1292–1297. doi: 10.1093/humrep/deh785. [DOI] [PubMed] [Google Scholar]
- Coetzee K., Stewart B., Peek J., Hutton J.D. Acceptance of single-embryo transfer by patients. Fertil. Steril. 2007;87(1):207–209. doi: 10.1016/j.fertnstert.2006.05.065. [DOI] [PubMed] [Google Scholar]
- Crawford S., Boulet S.L., Mneimneh A.S., Perkins K.M., Jamieson D.J., Zhang Y., Kissin D.M. Costs of achieving live birth from assisted reproductive technology: a comparison of sequential single and double embryo transfer approaches. Fertil. Steril. 2016;105(2):444–450. doi: 10.1016/j.fertnstert.2015.10.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffin D., Brown L., Feinn R., Jacob M.C., Scranton V., Egan J., Nulsen J. Impact of an educational intervention and insurance coverage on patients' preferences to transfer multiple embryos. Reprod. BioMed. Online. 2012;25(2):204–208. doi: 10.1016/j.rbmo.2012.04.006. [DOI] [PubMed] [Google Scholar]
- Harris R.P., Helfand M., Woolf S.H., Lohr K.N., Mulrow C.D., Teutsch S.M., Atkins D. Current methods of the US Preventive Services Task Force: a review of the process. Am. J. Prev. Med. 2001;20(3 Suppl):21–35. doi: 10.1016/s0749-3797(01)00261-6. [DOI] [PubMed] [Google Scholar]
- Højgaard A., Ottosen L.D., Kesmodel U., Ingerslev H.J. Patient attitudes towards twin pregnancies and single embryo transfer - a questionnaire study. Hum. Reprod. 2007;22(10):2673–2678. doi: 10.1093/humrep/dem173. [DOI] [PubMed] [Google Scholar]
- Hope N., Rombauts L. Can an educational DVD improve the acceptability of elective single embryo transfer? A randomized controlled study. Fertil. Steril. 2010;94(2):489–495. doi: 10.1016/j.fertnstert.2009.03.080. [DOI] [PubMed] [Google Scholar]
- Khalaf Y., E.-T. T., Coomarasamy A., Kamal A., Bolton V., Braude P. Selective single blastocyst transfer reduces the multiple pregnancy rate and increases pregnancy rates: A pre- and postintervention study. BJOG. 2008;115(3):385–390. doi: 10.1111/j.1471-0528.2007.01584.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kodama T., Hara T., Sato K., Yoshida A., Inoue Y. Elective single blastocyst transfer policy for women 40 years old plus strict patient education reduce the number of embryo transfers and multiple pregnancies without compromising the pregnancy rate. Fertil. Steril. 2009;1:S245. [Google Scholar]
- Kreuwel I.A., van Peperstraten A.M., Hulscher M.E., Kremer J.A., Grol R.P., Nelen W.L., Hermens R.P. Evaluation of an effective multifaceted implementation strategy for elective single-embryo transfer after in vitro fertilization. Hum. Reprod. 2013;28(2):336–342. doi: 10.1093/humrep/des371. [DOI] [PubMed] [Google Scholar]
- Leese B., Denton J. Attitudes towards single embryo transfer, twin and higher order pregnancies in patients undergoing infertility treatment: a review. Hum. Fertil. (Camb) 2010;13(1):28–34. doi: 10.3109/14647270903586364. [DOI] [PubMed] [Google Scholar]
- Lemos E.V., Zhang D., Van Voorhis B.J., Hu X.H. Healthcare expenses associated with multiple vs singleton pregnancies in the United States. Am. J. Obstet. Gynecol. 2013;209(6) doi: 10.1016/j.ajog.2013.10.005. (586.e581-586.e511) [DOI] [PubMed] [Google Scholar]
- Liberati A., Altman D.G., Tetzlaff J., Mulrow C., Gotzsche P.C., Ioannidis J.P.…Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6(7) doi: 10.1371/journal.pmed.1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maheshwari A., Griffiths S., Bhattacharya S. Global variations in the uptake of single embryo transfer. Hum. Reprod. Update. 2011;17(1):107–120. doi: 10.1093/humupd/dmq028. [DOI] [PubMed] [Google Scholar]
- Marek D.M.J., Chantlis S., Kaufmann R., Lynch D., Meintjes M. The effect of a comprehensive incentive program on patient participation in elective single blastocyst transfers. Fertil. Steril. 2005;2005(84):S85–S86. [Google Scholar]
- McLernon D.J., Harrild K., Bergh C., Davies M.J., de Neubourg D., Dumoulin J.C.…Bhattacharya S. Clinical effectiveness of elective single versus double embryo transfer: meta-analysis of individual patient data from randomised trials. BMJ. 2010;341 doi: 10.1136/bmj.c6945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher D., Liberati A., Tetzlaff J., Altman D.G. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA Statement. Open Med. 2009;3(3):e123–e130. [PMC free article] [PubMed] [Google Scholar]
- Murray S., Shetty A., Rattray A., Taylor V., Bhattacharya S. A randomized comparison of alternative methods of information provision on the acceptability of elective single embryo transfer. Hum. Reprod. 2004;19(4):911–916. doi: 10.1093/humrep/deh176. [DOI] [PubMed] [Google Scholar]
- Newton C.R., McBride J., Feyles V., Tekpetey F., Power S. Factors affecting patients' attitudes toward single- and multiple-embryo transfer. Fertil. Steril. 2007;87(2):269–278. doi: 10.1016/j.fertnstert.2006.06.043. [DOI] [PubMed] [Google Scholar]
- Pandian Z., Templeton A., Serour G., Bhattacharya S. Number of embryos for transfer after IVF and ICSI: a Cochrane review. Hum. Reprod. 2005;20(10):2681–2687. doi: 10.1093/humrep/dei153. [DOI] [PubMed] [Google Scholar]
- Ryan G.L., Sparks A.E., Sipe C.S., Syrop C.H., Dokras A., Van Voorhis B.J. A mandatory single blastocyst transfer policy with educational campaign in a United States IVF program reduces multiple gestation rates without sacrificing pregnancy rates. Fertil. Steril. 2007;88(2):354–360. doi: 10.1016/j.fertnstert.2007.03.001. [DOI] [PubMed] [Google Scholar]
- SART/ASRM, P. C Elective single-embryo transfer. Fertil. Steril. 2012;97(4):835–842. doi: 10.1016/j.fertnstert.2011.11.050. [DOI] [PubMed] [Google Scholar]
- Stillman R., Richter K., Jones H. Refuting a misguided campaign against the goal of single-embryo transfer and singleton birth in assisted reproduction. Hum. Reprod. 2013;28(10):2599–2607. doi: 10.1093/humrep/det317. [DOI] [PubMed] [Google Scholar]
- Sunderam S., Kissin D.M., Crawford S.B., Folger S.G., Boulet S.L., Warner L., Barfield W.D. Assisted Reproductive Technology Surveillance - United States, 2015. MMWR Surveill. Summ. 2018;67(3):1–24. doi: 10.15585/mmwr.ss6703a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Peperstraten A., Nelen W., Grol R., Zielhuis G., Adang E., Stalmeier P.…Kremer J. The effect of a multifaceted empowerment strategy on decision making about the number of embryos transferred in in vitro fertilisation: randomised controlled trial. BMJ. 2010;341:c2501. doi: 10.1136/bmj.c2501. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
PRISMA Checklist.