Abstract
Objective
To determine whether patients discharged from hospital during the December holiday period have fewer outpatient follow-ups and higher rates of death or readmission than patients discharged at other times.
Design
Population based retrospective cohort study.
Setting
Acute care hospitals in Ontario, Canada, 1 April 2002 to 31 January 2016.
Participants
217 305 children and adults discharged home after an urgent admission, during the two week December holiday period, compared with 453 641 children and adults discharged during two control periods in late November and January.
Main outcome measures
The primary outcome was death or readmission, defined as a visit to an emergency department or urgent rehospitalisation, within 30 days. Secondary outcomes were death or readmission and outpatient follow-up with a physician within seven and 14 days after discharge. Multivariable logistic regression with generalised estimating equations was used to adjust for characteristics of patients, admissions, and hospital.
Results
217 305 (32.4%) patients discharged during the holiday period and 453 641 (67.6%) discharged during control periods had similar baseline characteristics and previous healthcare utilisation. Patients who were discharged during the holiday period were less likely to have follow-up with a physician within seven days (36.3% v 47.8%, adjusted odds ratio 0.61, 95% confidence interval 0.60 to 0.62) and 14 days (59.5% v 68.7%, 0.65, 0.64 to 0.66) after discharge. Patients discharged during the holiday period were also at higher risk of 30 day death or readmission (25.9% v 24.7%, 1.09, 1.07 to 1.10). This relative increase was also seen at seven days (13.2% v 11.7%, 1.16, 1.14 to 1.18) and 14 days (18.6% v 17.0%, 1.14, 1.12 to 1.15). Per 100 000 patients, there were 2999 fewer follow-up appointments within 14 days, 26 excess deaths, 188 excess hospital admissions, and 483 excess emergency department visits attributable to hospital discharge during the holiday period.
Conclusions
Patients discharged from hospital during the December holiday period are less likely to have prompt outpatient follow-up and are at higher risk of death or readmission within 30 days.
Introduction
The Christmas holiday is characterised by festivities, social commitments, and synchronised time off work for parents with school aged children. During these busy two weeks, the need for urgent medical care continues, with influenza and other respiratory viruses responsible for increased hospital visits.1 2 3 4 5 6 Although acute hospital based services are usually available during the holiday period, this might not be the case for outpatient care. Early follow-up of outpatients with a physician provides an opportunity for education, drug review, discussion of results, and detection of clinical deterioration.7 This practice is associated with reduced readmissions for patients with some chronic diseases,8 9 10 and it is now a quality indicator for primary care practices.11
Studies of the “weekend effect” have described increased mortality in patients admitted to hospital on weekends compared with weekdays.12 13 14 One proposed mechanism is decreased staffing of hospitals during off-hours.15 Delays in testing and procedures on weekends provide further evidence of real differences in weekend care.16 17 The comparatively few studies examining the effect of timing of hospital discharge on patient outcomes have reported mixed results.18 19 20 21 22 Patients discharged at weekends tend to be younger, have fewer comorbidities, and have shorter lengths of hospital stay than patients discharged on weekdays.20 22 23
We hypothesised that the December holiday period is a vulnerable time for patients discharged from hospital, as reduced staffing levels could affect coordination of care and access to follow-up. We tested whether patients discharged from hospital during the holiday period were at greater risk of death or readmission than patients discharged at other times. In addition, we compared follow-up with a physician in these two groups.
Methods
We conducted a population based retrospective cohort study of patients discharged from acute care hospitals between 1 April 2002 and 31 January 2016, in Ontario, Canada. ICES in Toronto, Canada, collects deidentified health administrative data for all residents with a health insurance number, including information on hospital admissions,24 emergency department visits,25 outpatient visits to a physician,26 27 and demographics and vital statistics.28
Study population
We identified all patients discharged to the community (not to a nursing home, rehabilitation centre, or other acute care facility) after an urgent hospital admission in Ontario between 1 April 2002 and 31 January 2016. We excluded three groups likely to have noticeably different follow-up needs and risk of readmission: newborns, women admitted for an obstetrical delivery, patients admitted for palliative care, or those with a length of hospital stay more than 100 days (see supplementary appendix figure 1). We also excluded people with missing age, missing sex, invalid home locations, invalid death dates, or who were discharged outside the December holiday or control periods. Only the patient’s first hospital discharge was selected.
Study periods
We defined the two week December holiday, which comprises Christmas Day and New Year’s Day, as described in the school year calendar in the province of Ontario.29 As the start and end dates shift each year to always begin and end with a weekend, and to ensure that the follow-up window most closely aligned with the holiday period, we chose Fridays as the start and end dates (see supplementary appendix table 1).
We selected two winter time control periods that were separate from the December holiday. These control periods began four weeks before and four weeks after the start of that year’s December holiday period, in late November and January. Control periods contained the same number of Fridays, weekdays, and weekends as the holiday period, but no statutory holidays.
Patient and hospital characteristics
We examined hospital type and several characteristics of patients and admissions: year of hospital discharge, age, sex, rural residence, Charlson comorbidity index score,30 socioeconomic status (measured using median neighbourhood income), length of hospital stay, arrival by ambulance, diagnosis, discharged with home support or against medical advice, and previous healthcare usage (emergency department visits, hospital stays, outpatient visits, home care visits).
Outcomes
The primary outcome was a composite of death or readmission within 30 days of hospital discharge. Readmission was defined as either an emergency department visit or an urgent rehospitalisation. Secondary outcomes were outpatient follow-up with any physician within seven and 14 days of hospital discharge (see supplementary appendix table 2). We also reported death or readmission within seven and 14 days, as well as death, urgent rehospitalisation, or visit to an emergency department within 7, 14, and 30 days of discharge. We selected discrete outcomes for our main analyses owing to intuitive interpretation and policy relevance of these outcomes, as performance indicators are often based on binary outcomes at 7, 14, and 30 days.
Statistical analysis
We compared patients discharged during the December holiday with those discharged during the control periods. Univariate comparisons used standardised differences of means, with a difference of less than 0.10 (10%) considered to be unimportant. Baseline characteristics with standardised differences below this threshold have a negligible correlation with the exposure group.31 Standardised differences are often used to compare propensity score matched groups, and they can also be used to compare characteristics in unmatched observational studies.31 32 With large sample sizes, small differences in means can result in statistically significant values, yet standardised differences provide an estimate of the magnitude of the difference between groups.
For illustrative purposes, we plotted time to death or readmission using a Kaplan-Meier curve. For all outcome comparisons we report unadjusted and adjusted odds ratios (with 95% confidence intervals). Adjusted odds ratios were obtained with logistic regression models estimated using generalised estimating equations methods and including all measured patient and hospital characteristics.33 To account for clustering of patients within hospitals we used an exchangeable correlation structure.34 Where information on income fifth was missing, this was set to a level of “0” and included in the model.
We undertook a confirmatory analysis using a propensity score matched cohort and time-to-event analysis for the primary outcome (see supplementary appendix table 3). To evaluate the temporal relation between Christmas Day and short term outcomes we plotted the proportion of patients experiencing each seven day outcome according to their day of discharge, for 30 days before to 30 days after Christmas Day.
Subgroup analyses
We examined outcomes for adults with an in-hospital diagnosis of heart failure or chronic obstructive pulmonary disease. Patients with these high risk chronic conditions might benefit from early follow-up.8 9 10
We also tested for effect modification by baseline risk of readmission, as estimated by the LACE (Length of stay of index admission, Acuity of admission, Comorbidities, and Emergency department visits within past six months before hospital admission) score, a validated tool to predict 30 day death or readmission in adults after hospital discharge.35 As others have done, we defined high risk as a LACE score of 10 or more, corresponding to a predicted risk of 12% or more for 30 day death or readmission.36 37 To obtain adjusted odds ratios for the effect of holiday admission in high and low risk groups, we modified our earlier logistic regression model by including an interaction term between hospital discharge during the holiday period and risk group.
Similarly, we tested for an interaction term between hospital discharge during the holiday period and calendar period (2002-08 or 2009-15). Analyses were carried out using SAS software, version 9.4 (SAS Institute, Carey, NC).
Patient and public involvement
No patients were involved in setting the research question or the outcome measures, nor were they involved in developing plans for recruitment, design, or implementation of the study. No patients were asked to advise on interpretation or writing up of results. We plan to disseminate the results of the research to the general public through the use of press releases.
Results
Patient characteristics
Of 670 946 eligible participants, 93 092 (13.9%) were children, 303 579 (45.3%) were adults aged less than 65, and 274 275 (40.9%) were older adults. Half (n=335 715, 50.0%) of the patients were female, and half had no baseline comorbidities (n=354 130, 52.8%). Most (n=477 044, n=71.1%) had no hospital admission in the previous year, although more than half (n=390 612, 58.2%) had visited an emergency department at least once in the past six months. The most common diagnoses for hospital admission were diseases of the circulatory system (n=113 013, 16.8%), digestive system (n=105 571, 15.7%), and respiratory system (n=89 781, 13.4%). The median length of hospital stay was 3 days (interquartile range 2-7 days).
Overall, 217 305 (32.4%) patients were discharged during the December holiday period and 453 641 (67.6%) during the two control periods. Patients discharged during the holiday period were similar to those discharged during the control periods (table 1).
Table 1.
Baseline characteristics of patients discharged during the December holiday period and control periods (late November and January). Values are numbers (percentages) unless stated otherwise
| Characteristics | Study periods | SD* | |
|---|---|---|---|
| Holiday (n=217 305) | Control (n=453 641) | ||
| Year of hospital discharge†: | |||
| 2002 | 17 485 (8.0) | 37 411 (8.2) | 0.01 |
| 2003 | 18 329 (8.4) | 37 072 (8.2) | 0.01 |
| 2004 | 17 324 (8.0) | 35 678 (7.9) | 0.00 |
| 2005 | 15 327 (7.1) | 33 978 (7.5) | 0.02 |
| 2006 | 15 004 (6.9) | 30 956 (6.8) | 0.00 |
| 2007 | 14 349 (6.6) | 30 167 (6.6) | 0.00 |
| 2008 | 14 053 (6.5) | 29 955 (6.6) | 0.01 |
| 2009 | 14 265 (6.6) | 30 234 (6.7) | 0.00 |
| 2010 | 14 724 (6.8) | 29 764 (6.6) | 0.01 |
| 2011 | 14 418 (6.6) | 31 193 (6.9) | 0.01 |
| 2012 | 15 509 (7.1) | 31 366 (6.9) | 0.01 |
| 2013 | 15 498 (7.1) | 31 773 (7.0) | 0.00 |
| 2014 | 15 896 (7.3) | 32 001 (7.1) | 0.01 |
| 2015 | 15 124 (7.0) | 32 093 (7.1) | 0.00 |
| Patient age (years)‡: | |||
| <18 | 30 195 (13.9) | 62 897 (13.9) | 0.00 |
| 18-64 | 96 895 (44.6) | 206 684 (45.6) | 0.02 |
| ≥65 | 90 215 (41.5) | 184 060 (40.6) | 0.02 |
| Female | 107 466 (49.5) | 228 249 (50.3) | 0.02 |
| Rural residence | 32 016 (14.7) | 68 815 (15.2) | 0.01 |
| Income fifth§: | |||
| 1 (lowest) | 49 491 (22.8) | 103 747 (22.9) | 0.00 |
| 2 | 45 452 (20.9) | 94 616 (20.9) | 0.00 |
| 3 | 42 039 (19.3) | 88 370 (19.5) | 0.00 |
| 4 | 41 637 (19.2) | 85 902 (18.9) | 0.01 |
| 5 (highest) | 37 569 (17.3) | 78 547 (17.3) | 0.00 |
| Median (interquartile range) length of hospital stay (days) | 3 (2-6) | 3 (2-7) | 0.08 |
| Arrival by ambulance at index admission | 71 036 (32.7) | 141 767 (31.3) | 0.03 |
| Charlson comorbidity index score: | |||
| 0 (lowest) | 113 977 (52.5) | 240 153 (52.9) | 0.01 |
| 1 | 43 413 (20.0) | 86 556 (19.1) | 0.02 |
| 2 | 24 728 (11.4) | 52 023 (11.5) | 0.00 |
| 3 | 14 198 (6.5) | 29 772 (6.6) | 0.00 |
| ≥4 (highest) | 20 989 (9.7) | 45 137 (9.9) | 0.01 |
| Discharged against medical advice | 3027 (1.4) | 5658 (1.2) | 0.01 |
| Discharged with support services | 34 783 (16.0) | 78 155 (17.2) | 0.03 |
| Outpatient visits with physicians in past year¶: | |||
| 0-5 | 73 248 (33.7) | 150 037 (33.1) | 0.01 |
| 6-10 | 52 313 (24.1) | 109 320 (24.1) | 0.00 |
| 11-15 | 36 623 (16.9) | 77 413 (17.1) | 0.01 |
| >15 | 55 121 (25.4) | 116 871 (25.8) | 0.01 |
| Assigned primary care provider | 207 160 (95.3) | 433 365 (95.5) | 0.01 |
| Emergency room visits in past 6 months¶: | |||
| 0 | 90 716 (41.7) | 189 618 (41.8) | 0.00 |
| 1 | 64 674 (29.8) | 132 115 (29.1) | 0.01 |
| ≥2 | 61 915 (28.5) | 131 908 (29.1) | 0.01 |
| ≥1 urgent hospital admissions in past year | 57 177 (26.3) | 121 453 (26.8) | 0.01 |
| ≥1 elective hospital admission in past year | 18 292 (8.4) | 38 576 (8.5) | 0.00 |
| ≥1 home care visits in past 6 months | 16 078 (7.4) | 34 211 (7.5) | 0.01 |
| Hospital type: | |||
| Teaching | 54 481 (25.1) | 114 760 (25.3) | 0.01 |
| Community | 144 601 (66.5) | 299 320 (66.0) | 0.01 |
| Small | 8803 (4.1) | 19 138 (4.2) | 0.01 |
| Paediatric | 6,220 (2.9) | 13 016 (2.9) | 0.00 |
| Rural location | 32 016 (14.7) | 68 815 (15.2) | 0.01 |
| Missing | 3200 (1.5) | 7407 (1.6) | 0.01 |
| Diagnostic category for most responsible diagnosis**: | |||
| Diseases of circulatory system | 35 757 (16.5) | 77 256 (17.0) | 0.02 |
| Diseases of digestive system | 33 963 (15.6) | 71 608 (15.8) | 0.00 |
| Diseases of respiratory system | 33 696 (15.5) | 56 085 (12.4) | 0.09 |
| Symptoms, signs, and abnormal clinical and laboratory findings, not elsewhere classified | 21 041 (9.7) | 46 743 (10.3) | 0.02 |
| Injury, poisoning, and certain other consequences of external causes | 22 049 (10.1) | 44 670 (9.8) | 0.01 |
| Diseases of genitourinary system | 10 416 (4.8) | 22 613 (5.0) | 0.01 |
| Mental and behavioural disorders | 8630 (4.0) | 22 052 (4.9) | 0.04 |
| Neoplasms | 7032 (3.2) | 15 981 (3.5) | 0.02 |
| Pregnancy, childbirth, and the puerperium | 6090 (2.8) | 12 787 (2.8) | 0.00 |
| Endocrine, nutritional, and metabolic diseases | 6753 (3.1) | 13 905 (3.1) | 0.00 |
Standardised difference of means.
Fiscal year from 1 April to 31March.
Grouped by life stage: children, adults, and older adults.
Missing observations n=1117 for holiday, n=2459 for control.
Categorised on basis of most common values.
Top 10 most common diagnostic categories (holiday and control groups combined).
Follow-up with a physician
Patients discharged during the holiday period were less likely to have follow-up with a physician within seven days (36.3% v 47.8%, adjusted odds ratio 0.61, 95% confidence interval 0.60 to 0.62) and 14 days (59.5% v 68.7%, 0.65, 0.64 to 0.66). Per 100 000 patients, there were 2999 fewer follow-ups within 14 days attributable to discharge during the holiday period. The decreased likelihood of follow-up associated with discharge during the holiday period was observed across patient characteristics (see supplementary appendix table 4).
Death or readmission
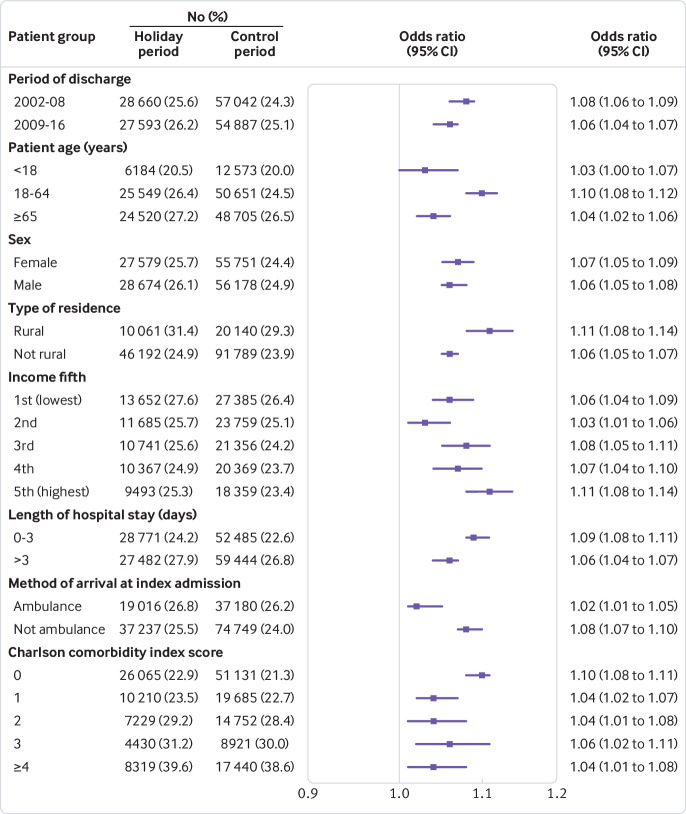
Time to death or readmission differed between patients in the holiday period group and control periods group (log-rank test P<0.001, fig 1). Patients discharged during the holiday period were at increased risk of death or readmission within 30 days (25.9% v 24.7%, 1.09, 1.07 to 1.10). This was explained by an increased risk of return to the emergency department (24.3% v 23.0%, 1.09, 1.07 to 1.10), rehospitalisation (11.8% v 11.4%, 1.06, 1.04 to 1.08), and death (1.5% v 1.5%, 1.06, 1.02 to 1.10) within 30 days (table 2). The increased risk of death or readmission associated with discharge during the holiday period was further accentuated within seven days (13.2% v 11.7%, 1.16, 1.14 to 1.18) and 14 days (18.6% v 17.0%, 1.14, 1.12 to 1.15). A confirmatory time-to-event analysis in a propensity score matched cohort (see supplementary appendix table 5) showed consistent results (death or readmission hazard ratio 1.08, 95% confidence interval 1.07 to 1.09).
Fig 1.
Kaplan-Meier curve of time to composite of 30 day death or readmission after hospital discharge
Table 2.
Unadjusted and adjusted outcomes of patients discharged from hospital during the December holiday period and control periods (late November and January). Values are numbers (percentages) unless stated otherwise
| Outcome measures | Study periods | Unadjusted estimates (95% CI) | Adjusted odds ratio* (95% CI) | |||
|---|---|---|---|---|---|---|
| Holiday (n=217 305) | Control (n=453 641) | Risk difference (%) | Odds ratio | |||
| Primary outcome | ||||||
| 30 day death or readmission | 56 253 (25.9) | 111 929 (24.7) | 1.2 (1.0 to 1.4) | 1.07 (1.05 to 1.08) | 1.09 (1.07 to 1.10) | |
| 30 day emergency department visit | 52 704 (24.3) | 104 468 (23.0) | 1.2 (1.0 to 1.4) | 1.07 (1.06 to 1.08) | 1.09 (1.07 to 1.10) | |
| 30 day rehospitalisation | 25 624 (11.8) | 51 802 (11.4) | 0.4 (0.2 to 0.5) | 1.04 (1.02 to 1.05) | 1.06 (1.04 to 1.08) | |
| 30 day death | 3216 (1.5) | 6570 (1.5) | 0.0 (0.0 to 0.1) | 1.02 (0.98 to 1.07) | 1.06 (1.02 to 1.10) | |
| Secondary outcomes | ||||||
| 7 day outpatient follow-up | 78 838 (36.3) | 216 592 (47.8) | 11.5 (11.2 to 11.7) | 0.62 (0.62 to 0.63) | 0.61 (0.60 to 0.62) | |
| 14 day outpatient follow-up | 129 337 (59.5) | 311 648 (68.7) | 9.2 (8.9 to 9.4) | 0.67 (0.66 to 0.68) | 0.65 (0.64 to 0.66) | |
| 7 day death or readmission | 28 665 (13.2) | 53 191 (11.7) | 1.5 (1.3 to 1.6) | 1.14 (1.13 to 1.16) | 1.16 (1.14 to 1.18) | |
| 7 day emergency department visit | 27 240 (12.5) | 49 888 (11.0) | 1.5 (1.4 to 1.7) | 1.16 (1.14 to 1.18) | 1.17 (1.15 to 1.19) | |
| 7 day rehospitalisation | 10 549 (4.9) | 21 023 (4.6) | 0.2 (0.1 to 0.3) | 1.05 (1.03 to 1.08) | 1.07 (1.04 to 1.09) | |
| 7 day death | 683 (0.3) | 1278 (0.3) | 0.0 (0.0 to 0.1) | 1.12 (1.02 to 1.22) | 1.14 (1.04 to 1.25) | |
| 14 day death or readmission | 40 433 (18.6) | 77 010 (17.0) | 1.6 (1.4 to 1.8) | 1.12 (1.10 to 1.13) | 1.14 (1.12 to 1.15) | |
| 14 day emergency department visit | 38 168 (17.6) | 71 882 (15.9) | 1.7 (1.5 to 1.9) | 1.13 (1.12 to 1.15) | 1.15 (1.13 to 1.16) | |
| 14 day rehospitalisation | 16 697 (7.7) | 33 321 (7.4) | 0.3 (0.2 to 0.5) | 1.05 (1.03 to 1.07) | 1.07 (1.05 to 1.09) | |
| 14 day death | 1444 (0.7) | 2872 (0.6) | 0.03 (0.0 to 0.1) | 1.05 (0.99 to 1.12) | 1.08 (1.02 to 1.14) | |
Adjusted for year of hospital discharge, age, sex, rural residence, Charlson comorbidity index score, socioeconomic status, length of hospital stay, arrival by ambulance, diagnosis, discharge with home supports or against medical advice previous healthcare usage (emergency department visits, rehospitalisations, outpatient visits, home care visits), and hospital type.
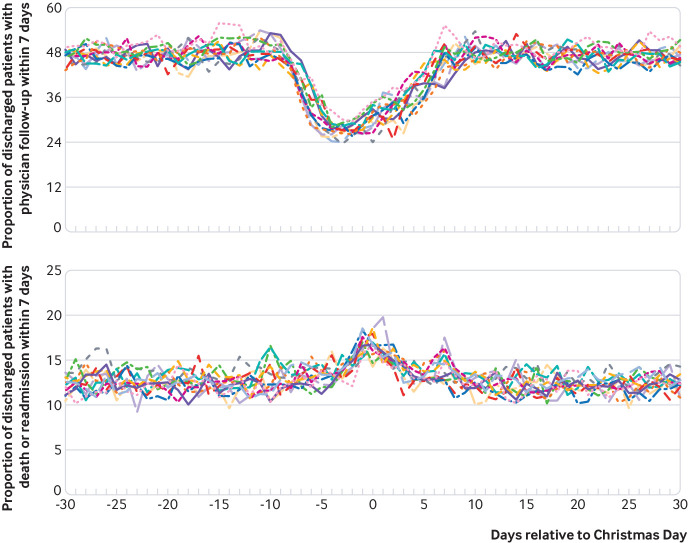
The increased unadjusted risk of 30 day death or readmission was observed across many patient characteristics, and no group showed a statistically significant decreased risk (fig 2). The holiday related risk seemed to be greatest for patients with a genitourinary condition, neoplasm, pregnancy related condition, or injury. Overall, per 100 000 patients there were 26 excess deaths, 188 excess rehospitalisations, and 483 excess visits to an emergency department attributable to being discharged from hospital during the holiday period.
Fig 2.
Forest plot of unadjusted results for 30 day death or readmission after hospital discharge during the Christmas holiday period or two controls periods, stratified by baseline patient and hospital characteristics (see appendix figure 2 for detailed graphic)
Analysis of “Christmas effect”
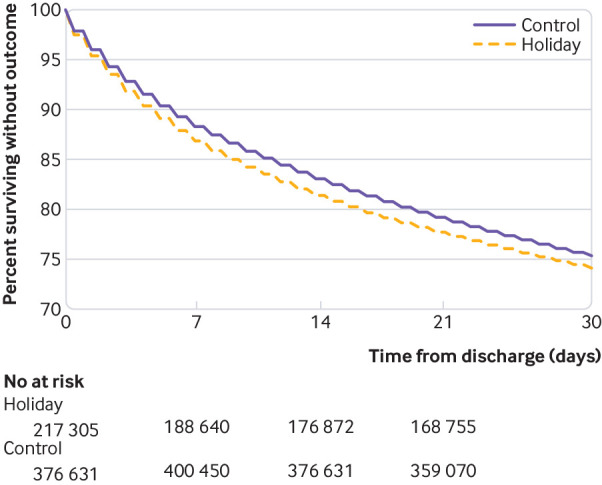
Patients discharged during the week before or week after Christmas Day were less likely to have follow-up within seven days (33.6% v 47.6%, odds ratio 0.56, 95% confidence interval 0.55 to 0.56) than those discharged before or after this period (fig 3). Patients discharged during the week before or the week after Christmas Day were at higher risk of death or readmission within seven days (14.2% v12.4%, 1.17, 1.15 to 1.18) than those discharged before or after this period (fig 3 and appendix figure 3). The absolute risk difference between the week before or the week after Christmas Day and the surrounding period was 14.0% (95% confidence interval 13.8% to 14.2%) for follow-up within seven days and 1.8% (1.6% to 1.9%) for death or readmission within seven days.
Fig 3.
Proportion of patients with seven day outpatient follow-up with a physician and seven day death or readmission, by day of discharge, relative to Christmas Day. Lines represent unadjusted results of a single year, for 2002-15
Subgroup analyses
Patients admitted to hospital for heart failure were significantly less likely to have follow-up within seven days (36.5% v 50.6%, adjusted odds ratio 0.55, 95% confidence interval 0.51 to 0.58) and 14 days (60.7% v 72.2%, 0.58, 0.54 to 0.61) if discharged during the holiday period. They were also at increased risk of 30 day death or readmission (31.9% v 30.9%, 1.06, 1.01 to 1.12). This was explained by an increased risk of visits to an emergency department (see supplementary appendix table 6). A similar pattern was observed within seven and 14 days after discharge.
Patients admitted to hospital for chronic obstructive pulmonary disease were significantly less likely to have follow-up within seven days (29.9% v 41.2%, adjusted odds ratio 0.59, 95% confidence interval 0.55 to 0.63) and 14 days (54.6% v 64.1%, 0.64, 0.60 to 0.68) if discharged during the holiday period. The risk of death or readmission in such patients discharged during the holiday period was not significant at 30 days (26.4% v 27.8%, 0.99, 0.93 to 1.05), but it was increased at seven days (10.9% v 9.7%, 1.19, 1.09 to 1.30) and 14 days (17.5% v 16.5%, 1.13, 1.05 to 1.21), driven by an increased risk of visits to an emergency department and rehospitalisations (see supplementary appendix table 7).
Of adults discharged during the holiday and control periods, 69 840 (35.7%) and 148 601 (38.0%), respectively, had a LACE score of 10 or greater, indicating a higher baseline risk of readmission (standardised difference in scores between groups was 0.05). Patients with a high LACE score (holiday 60.4% v control 70.8%, adjusted odds ratio 0.60, 95% confidence interval 0.59 to 0.62) and low LACE score (holiday 59.2% v control 68.2%, 0.67, 0.66 to 0.68) were less likely to have follow-up within 14 days if discharged during the holiday period. The holiday related decrease in follow-up was more pronounced in patients with a high risk LACE score (P<0.001 for interaction between LACE score group and discharge during the holiday period). A similar pattern was seen for follow-up within seven days (see supplementary appendix table 8).
The holiday related risk of 30 day death or readmission was more pronounced in patients with a low risk LACE score (holiday 22.5% v control 20.8%, adjusted odds ratio 1.12, 95% confidence interval 1.10 to 1.13) than those with a high risk LACE score (holiday 34.4% v control 33.1%, 1.06, 1.04 to 1.09, P for interaction <0.001, see supplementary appendix table 5). A similar pattern was observed within 14 days; however, at seven days this distinction between high risk and low risk groups was not apparent (P for interaction 0.25).
Patients discharged from hospital in 2009-15 had a greater holiday related decrease in follow-up within seven and 14 days (2002-08 adjusted odds ratio 0.67, 95% confidence interval 0.66 to 0.68, 2009-15 0.63, 0.62 to 0.65, P for interaction <0.001). The period (2002-08 or 2009-15) of discharge did not significantly alter the relation between discharge during the holiday period and the risk of 30 day death or readmission (P=0.09, see supplementary appendix table 9). However, patients discharged from hospital in 2002-08 had a significantly greater holiday related risk for seven day death or readmission (holiday 13.2% v control 11.5%, 1.18, 1.15 to 1.20) than those discharged in 2009-15 (holiday 13.2% v control 11.9%, 1.13, 1.11 to 1.16, P for interaction 0.008).
Discussion
This study found that Ontarians discharged from hospital during the two week December holiday period had an increased risk of 30 day death or readmission compared with patients discharged during late November and January. The greatest holiday related increase in risk was within seven days of hospital discharge. Patients discharged during the December holiday were also less likely to have follow-up with a physician within seven and 14 days of hospital discharge. Per 100 000 patients, 26 excess deaths, 188 excess rehospitalisations, 483 excess visits to an emergency department, and 2999 fewer follow-up appointments could be attributed to being discharged from hospital during the December holiday.
The differences in outcomes could not be explained by observed hospital or patient characteristics, including admission diagnosis. Moreover, the increased unadjusted 30 day risk of death or readmission was observed across many patient characteristics, and no group showed a significantly decreased risk of death or readmission at 30 days. Although patients admitted to hospital on weekends might be sicker than their weekday counterparts,38 patients discharged from hospital on weekends typically have characteristics associated with a lower risk for readmission, such as younger age, fewer comorbidities, and shorter hospital stay.20 We similarly observed that patients discharged during the holiday period had a slightly lower baseline risk of readmission, as predicted by the LACE score. Patients at higher baseline risk had a lower holiday attributable 30 day risk of death or readmission than patients at lower baseline risk of readmission. Similarly, the 30 day risk of death or readmission for patients with chronic obstructive pulmonary disease was not significantly increased with discharge during the holiday period. The seemingly paradoxical findings observed in these key patient subgroups might suggest that holiday related risk is not proportional to baseline risk and could predominantly affect an otherwise lower risk group of patients. One example of how this could occur would be if in a setting of reduced resources over the holidays, clinicians prioritise higher risk patients for more thorough discharge planning.
Several possible mechanisms might explain how the December holiday period could lead to decreased follow-up. Firstly, the holiday period might be a time of reduced access to outpatient care, as clinic staff suspend work for a prolonged, and coordinated, holiday. Patients might not be able to contact their physician or could encounter difficulties in booking appointments. Secondly, patients might prefer to postpone their follow-up visit until their usual physician is available, or until the end of the holiday festivities or travel commitments. Thirdly, hospital based coordination of follow-up care might be reduced over the holidays, with staffing reductions mirroring those in outpatient clinics. Similar to procedural delays encountered during off-hours,16 17 elements of discharge planning (eg, drug review, patient education, care coordination) could be limited by staff reductions during the holiday period.
The relation between discharge from hospital during the holiday period and death or readmission might also be explained in several ways. Firstly, for many the December holiday is filled with festive activities and potential physiological stressors (eg, tense interpersonal exchanges, lack of sleep, increased intake of alcohol, sodium, and sugar). These altered circumstances could destabilise an acute medical condition. Secondly, family members who are on holiday leave might prompt a relative to return early to the emergency department. Yet, the increased risk of readmission and death observed in our study suggests that such visits are not limited to minor conditions. Thirdly, decreased follow-up, as found in our study, could reduce the chance of identifying avoidable complications or early deterioration. In this study, we have not tested whether differences in follow-up explain the association between discharge during the holiday period and death or readmission; our findings only provide an ecological clue to the possibility that decreased follow-up and increased death or readmissions coexist.39 To determine whether follow-up mediates the relation between hospital discharge during the holiday period and death or readmission, tools need to be developed to test a time varying binary mediator of a time-to-event outcome.
Limitations of this study
Our study has several limitations. We used many strategies to increase the comparability of groups and minimise bias when possible. Although length of hospital stay, comorbidities, and previous attendance at an emergency department are known predictors of post-discharge outcomes,35 40 they are imperfect proxies for more detailed clinical information on severity of illness. Thus, the possibility of confounding due to unmeasured differences remains. Furthermore, it is possible that increased out-of-province travel during the December holiday led us to underestimate rates of death or readmission in participants discharged during this period. Yet this would be expected to bias our findings towards the null hypothesis. Finally, our finding of a decrease in outpatient follow-up among patients discharged during the holiday period might not be generalisable to all populations. In particular, follow-up rates can be expected to vary according to local community practices.
We found that discharge from hospital during the December holiday is a novel risk factor for both reduced follow-up and increased death or readmission. More detailed information on patient severity of illness would strengthen the argument for causation between discharge during the holiday period and health outcomes. Further study of the potential role of follow-up in mediating this relation is now justified. Rather than rushing to get patients home, hospital clinicians should pay attention to discharge planning for this vulnerable group, ensuring optimal patient education, drug review, and follow-up care. Discharged patients, unlike unwanted gifts, should not be returned after the holidays.
What is already known on this topic
Many studies have found that patients admitted to hospital during off-hours are at increased risk of in-hospital mortality
Some studies have found that patients discharged from hospital on Fridays or at weekends are at increased risk of readmission
The outcomes of patients discharged during the December holiday period have not been described
What this study adds
Patients discharged during the December holiday period have an increased risk of death or readmission within 7, 14, and 30 days
Patients discharged during the holiday period are also less likely to have an outpatient follow-up visit with a physician within seven or 14 days of discharge
The baseline characteristics of patients discharged during the holiday period did not differ meaningfully from those discharged during control periods
Acknowledgments
We thank the patients who contributed their health record information to this study.
Web extra.
Extra material supplied by authors
Supplementary information: additional tables 1-9 and figures 1-3
Contributors: All authors had full access to all of the data (including statistical reports and tables) in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. LL-S is the guarantor. LL-S, PCA, NMI, DAR, and CMB conceived and designed the study. LL-S, JL, and CMB analysed and interpreted the data. LL-S drafted the manuscript. All authors critically revised the manuscript for important intellectual content. LL-S and JL carried out the statistical analysis. CMB obtained funding. LL-S and JL provided administrative, technical, or material support. CMB supervised the study. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Competing interests: All authors have completed the ICMJE uniform disclosure form and declare (with the exception of disclosures that follow): no support from any organisation for the submitted work, no financial relationships with any organisations that might have an interest in the submitted work in the previous three years, no other relationships or activities that could appear to have influenced the submitted work.
Funding: This study was supported by a Canadian Institutes of Health Research (CIHR) and Canadian Patient Safety Institute Chair in Patient Safety and Continuity of Care (CMB). CMB also reports support from the Department of Medicine at the University of Toronto. LL-S reports support from a CIHR fellowship award (FRN 146714), and the Philipson scholar programme at the University of Toronto. PCA reports support from a mid-career investigator award from the Heart and Stroke Foundation. NMI reports support from a CIHR new investigator award and from the Department of Family and Community Medicine at the University of Toronto. DAR reports support from a Canada Research Chair in Medical Decision Science.
This study was supported by ICES, which is funded by an annual grant from the Ontario Ministry of Health and Long term Care (MOHLTC). The opinions, results, and conclusions reported in this paper are those of the authors and are independent from the funding sources. No endorsement by ICES or the Ontario MOHLTC is intended or should be inferred. Parts of this material are based on data and information compiled and provided by the Canadian Institute for Health Information (CIHI). However, the analyses, conclusions, opinions, and statements expressed herein are those of the author, and not necessarily those of CIHI. The CIHR, ICES, the MOHLTC, and the Canadian Patient Safety Institute had no involvement in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Ethical approval: This study was approved by the research ethics boards of the University of Toronto and Sunnybrook Health Sciences Centre.
Data sharing: Technical appendix and statistical code available from LL-S at lauren.lapointe.shaw@mail.utoronto.ca.
Transparency: The manuscript’s guarantor (LL-S) affirms that the manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned have been explained.
References
- 1. Knight J, Schilling C, Barnett A, Jackson R, Clarke P. Revisiting the “Christmas Holiday Effect” in the Southern Hemisphere. J Am Heart Assoc 2016;5:e005098. 10.1161/JAHA.116.005098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Phillips DP, Jarvinen JR, Abramson IS, Phillips RR. Cardiac mortality is higher around Christmas and New Year’s than at any other time: the holidays as a risk factor for death. Circulation 2004;110:3781-8. 10.1161/01.CIR.0000151424.02045.F7. [DOI] [PubMed] [Google Scholar]
- 3. Kloner RA, Poole WK, Perritt RL. When throughout the year is coronary death most likely to occur? A 12-year population-based analysis of more than 220 000 cases. Circulation 1999;100:1630-4. 10.1161/01.CIR.100.15.1630 [DOI] [PubMed] [Google Scholar]
- 4. Meine TJ, Patel MR, DePuy V, et al. Evidence-based therapies and mortality in patients hospitalized in December with acute myocardial infarction. Ann Intern Med 2005;143:481-5. 10.7326/0003-4819-143-7-200510040-00006 [DOI] [PubMed] [Google Scholar]
- 5. Reedman LA, Allegra JR, Cochrane DG. Increases in heart failure visits after Christmas and New Year’s Day. Congest Heart Fail 2008;14:307-9. 10.1111/j.1751-7133.2008.00021.x. [DOI] [PubMed] [Google Scholar]
- 6. Johnston NW. The similarities and differences of epidemic cycles of chronic obstructive pulmonary disease and asthma exacerbations. Proc Am Thorac Soc 2007;4:591-6. 10.1513/pats.200706-064TH. [DOI] [PubMed] [Google Scholar]
- 7. Dharmarajan K, Krumholz HM. Risk after hospitalization: we have a lot to learn. J Hosp Med 2015;10:135-6. 10.1002/jhm.2309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Sharma G, Kuo YF, Freeman JL, Zhang DD, Goodwin JS. Outpatient follow-up visit and 30-day emergency department visit and readmission in patients hospitalized for chronic obstructive pulmonary disease. Arch Intern Med 2010;170:1664-70. 10.1001/archinternmed.2010.345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. McAlister FA, Youngson E, Bakal JA, Kaul P, Ezekowitz J, van Walraven C. Impact of physician continuity on death or urgent readmission after discharge among patients with heart failure. CMAJ 2013;185:E681-9. 10.1503/cmaj.130048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Hernandez AF, Greiner MA, Fonarow GC, et al. Relationship between early physician follow-up and 30-day readmission among Medicare beneficiaries hospitalized for heart failure. JAMA 2010;303:1716-22. 10.1001/jama.2010.533. [DOI] [PubMed] [Google Scholar]
- 11.Ontario HQ. Indicator Technical Specifications Quality Improvement Plan 2014/15. Ottawa, Ontario, 2014. [Google Scholar]
- 12. Kostis WJ, Demissie K, Marcella SW, Shao YH, Wilson AC, Moreyra AE, Myocardial Infarction Data Acquisition System (MIDAS 10) Study Group Weekend versus weekday admission and mortality from myocardial infarction. N Engl J Med 2007;356:1099-109. 10.1056/NEJMoa063355. [DOI] [PubMed] [Google Scholar]
- 13. Aylin P, Alexandrescu R, Jen MH, Mayer EK, Bottle A. Day of week of procedure and 30 day mortality for elective surgery: retrospective analysis of hospital episode statistics. BMJ 2013;346:f2424. 10.1136/bmj.f2424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Bell CM, Redelmeier DA. Mortality among patients admitted to hospitals on weekends as compared with weekdays. N Engl J Med 2001;345:663-8. 10.1056/NEJMsa003376. [DOI] [PubMed] [Google Scholar]
- 15. Lapointe-Shaw L, Bell CM. It’s not you, it’s me: time to narrow the gap in weekend care. BMJ Qual Saf 2013;23;180-2. 10.1136/bmjqs-2013-002674. [DOI] [PubMed] [Google Scholar]
- 16. Bell CM, Redelmeier DA. Waiting for urgent procedures on the weekend among emergently hospitalized patients. Am J Med 2004;117:175-81. 10.1016/j.amjmed.2004.02.047. [DOI] [PubMed] [Google Scholar]
- 17. Magid DJ, Wang Y, Herrin J, et al. Relationship between time of day, day of week, timeliness of reperfusion, and in-hospital mortality for patients with acute ST-segment elevation myocardial infarction. JAMA 2005;294:803-12. 10.1001/jama.294.7.803. [DOI] [PubMed] [Google Scholar]
- 18. Beck CE, Khambalia A, Parkin PC, Raina P, Macarthur C. Day of discharge and hospital readmission rates within 30 days in children: A population-based study. Paediatr Child Health 2006;11:409-12. 10.1093/pch/11.7.409 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. van Walraven C, Bell CM. Risk of death or readmission among people discharged from hospital on Fridays. CMAJ 2002;166:1672-3. [PMC free article] [PubMed] [Google Scholar]
- 20. McAlister FA, Youngson E, Padwal RS, Majumdar SR. Similar outcomes among general medicine patients discharged on weekends. J Hosp Med 2015;10:69-74. 10.1002/jhm.2310. [DOI] [PubMed] [Google Scholar]
- 21. Graham LE, Leff B, Arbaje AI. Risk of hospital readmission for older adults discharged on friday. J Am Geriatr Soc 2013;61:300-1. 10.1111/jgs.12107. [DOI] [PubMed] [Google Scholar]
- 22. McAlister FA, Au AG, Majumdar SR, Youngson E, Padwal RS. Postdischarge outcomes in heart failure are better for teaching hospitals and weekday discharges. Circ Heart Fail 2013;6:922-9. 10.1161/CIRCHEARTFAILURE.113.000336. [DOI] [PubMed] [Google Scholar]
- 23. Tickoo S, Fonarow GC, Hernandez AF, Liang L, Cannon CP. Weekend/holiday versus weekday hospital discharge and guideline adherence (from the American Heart Association’s Get with the Guidelines--Coronary Artery Disease database). Am J Cardiol 2008;102:663-7. 10.1016/j.amjcard.2008.04.053. [DOI] [PubMed] [Google Scholar]
- 24. Juurlink DN, Preyra C, Croxford R, et al. Canadian Institute for Health Information Discharge Abstract Database: A Validation Study. Institute for Clinical Evaluative Sciences, 2006. [Google Scholar]
- 25.Canadian Institute for Health Information. CIHI Data Quality Study of Ontario Emergency Department Visits for Fiscal Year 2004-2005—Executive Summary. Ottawa, 2007. [Google Scholar]
- 26. Shah BR, Hux JE, Laupacis A, Zinman B, Cauch-Dudek K, Booth GL. Administrative data algorithms can describe ambulatory physician utilization. Health Serv Res 2007;42:1783-96. 10.1111/j.1475-6773.2006.00681.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Stukel T, Glazier RH, Schultz SE, et al. Multispecialty physician networks in Ontario. Open Med 2013;7(2). [PMC free article] [PubMed] [Google Scholar]
- 28. Iron K, Zagorski BM, Sykora K, et al. Living and Dying in Ontario: An Opportunity for Improved Health Information. ICES Investigative Report. Institute for Clinical Evaluative Sciences, 2008. [Google Scholar]
- 29.EdCan Network. School Calendar https://www.edcan.ca/: Canadian Education Association; [accessed Feb 21 2018.
- 30. Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care 2005;43:1130-9. 10.1097/01.mlr.0000182534.19832.83 [DOI] [PubMed] [Google Scholar]
- 31. Austin PC. Using the Standardized Difference to Compare the Prevalence of a Binary Variable Between Two Groups in Observational Research. Commun Stat Simul Comput 2009;38:1228-34. 10.1080/03610910902859574. [DOI] [Google Scholar]
- 32. Austin PC. Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat Med 2009;28:3083-107. 10.1002/sim.3697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Zeger SL, Liang KY. Longitudinal data analysis for discrete and continuous outcomes. Biometrics 1986;42:121-30. 10.2307/2531248 [DOI] [PubMed] [Google Scholar]
- 34. Burton P, Gurrin L, Sly P. Extending the simple linear regression model to account for correlated responses: an introduction to generalized estimating equations and multi-level mixed modelling. Stat Med 1998;17:1261-91. [DOI] [PubMed] [Google Scholar]
- 35. van Walraven C, Dhalla IA, Bell C, et al. Derivation and validation of an index to predict early death or unplanned readmission after discharge from hospital to the community. CMAJ 2010;182:551-7. 10.1503/cmaj.091117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Brener SS, Bronksill SE, Comrie R, Huang A, Bell CM. Association between in-hospital supportive visits by primary care physicians and patient outcomes: A population-based cohort study. J Hosp Med 2016;11:418-24. 10.1002/jhm.2561. [DOI] [PubMed] [Google Scholar]
- 37. Dhalla IA, O’Brien T, Morra D, et al. Effect of a postdischarge virtual ward on readmission or death for high-risk patients: a randomized clinical trial. JAMA 2014;312:1305-12. 10.1001/jama.2014.11492. [DOI] [PubMed] [Google Scholar]
- 38. Walker AS, Mason A, Quan TP, et al. Mortality risks associated with emergency admissions during weekends and public holidays: an analysis of electronic health records. Lancet 2017;390:62-72. 10.1016/S0140-6736(17)30782-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Hofstede SN, van Bodegom-Vos L, Kringos DS, Steyerberg E, Marang-van de Mheen PJ. Mortality, readmission and length of stay have different relationships using hospital-level versus patient-level data: an example of the ecological fallacy affecting hospital performance indicators. BMJ Qual Saf 2018;27:474-83. 10.1136/bmjqs-2017-006776. [DOI] [PubMed] [Google Scholar]
- 40. van Walraven C, Wong J, Forster AJ. LACE+ index: extension of a validated index to predict early death or urgent readmission after hospital discharge using administrative data. Open Med 2012;6:e80-90. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary information: additional tables 1-9 and figures 1-3