Abstract
BACKGROUND
Improvements in health behaviors and academic outcomes have been associated with school-based health centers (SBHCs). However, underlying mechanisms for these associations have been largely unexamined, particularly among lower-income youth. The current study examines the relationship between SBHCs and school connectedness and whether this relationship differs by youths’ socioeconomic status (SES).
METHODS
Student-level cross-sectional data from 503 traditional high schools in California were analyzed using multi-level regression models. California Healthy Kids Survey 2013–14 data included information on three dimensions of school connectedness and demographic characteristics including SES as measured by parental education. School-level demographic data was gathered from publicly available sources.
RESULTS
Although no significant relationship between SBHCs and any of the school connectedness dimensions emerged, there were significant cross-level interactions between SBHCs and parent education. SBHCs were more positively associated with school connectedness (adult caring, adult expectations, and meaningful participation) among lower SES students compared to students with higher SES.
CONCLUSIONS
SBHCs may be particularly effective in affecting school connectedness among lower income youth populations. This has wide ranging implications with regards to planning (eg careful selection of where SBHCs can be most effective), and future research (eg examining the effectiveness of specific SBHC strategies that support connectedness).
Keywords: School-based health centers, school connectedness, socioeconomic status, parental education
Over the past decade, there has been a significant increase in the implementation of school-based health centers (SBHCs). In 2015 2,315 centers were in operation across 49 states, a 20% increase over a three-year period (http://censusreport.sbh4all.org/). This is not surprising given recent research on SBHCs that has noted significant positive effects on youth health and academic outcomes including high school completion and Grade Point Average (GPA); grade promotion, lower rates of hospitalizations Emergency Room visits, and substance use; and higher rates of contraception use (for current review see Centers for Disease Control community guide1). The pathway(s) through which these outcomes are achieved, or mechanism(s) of action, however, remain unclear. It may be that SBHCs impact outcomes through multiple and interacting processes such as direct contact with students for prevention, intervention and/or treatment; training of teachers and staff to identify risk factors or behaviors for immediate referral; and/or creating systematic change around how students, staff and administrators approach health.
School connectedness has recently received some attention as a possible mechanism of action.2,3 School connectedness is defined as “the belief by students that adults in the school care about their learning as well as about them as individuals.”4 It has been characterized by a positive attitude towards school, sense of belonging at school, and connection with teachers and peers.5 The construct is often operationalized with a summary score of school asset indicators based on student report of perceived expectations, caring, and closeness to adults within the school system.4,6,7 Various school characteristics have been identified that predict school connectedness, including positive classroom management climates, level of student participation in extracurricular activities, tolerant disciplinary policies, higher socioeconomic status of the student body, racial homogeneity, and small school size.5,7 School connectedness has been associated with multiple protective health effects including lower emotional distress, suicidal thoughts and behaviors, acting out, violence, substance use, and higher age of sexual debut.7–10 Importantly, SBHC are often established in predominantly poor, urban communities where one might expect lower school connectedness among students.5
A small number of studies have noted an association between SBHC exposure and school connectedness. A study using the 2009 California Healthy Kids Survey data from 15 schools with an SBHC examined the association between student-reported utilization of SBHCs and various dimensions of school connectedness and found a positive association between use (any use vs. non-use) as well as a positive dose-response association. Any use of the SBHC was positively associated with having caring relationships with adults, high expectations by adults, and meaningful participation within the school setting. Additionally, students who reported accessing their SBHC more than ten times reported higher ratings of these three school connectedness dimensions compared to students who utilized their SBHC fewer times.11 Additional research has demonstrated that students who access SBHCs have higher levels of school bonding and school attachments than students who do not use SBHCs.3
It may be that school connectedness is an intermediary outcome between SBHCs and various health and academic outcomes.12 Multiple strategies exist that contribute to developing and maintaining school connectedness among youth;4,13 SBHCs are well positioned to incorporate or foster these approaches including adult support, school environment, physical and emotional safety, creating trusting relationships, creating positive behavioral norms and supportive peer groups. For example, in addition to providing physical and mental health care services, SBHCs have adult staff who may provide students with a sense of safety and caring. SBHCs may also directly influence school disciplinary policies as teachers may be more likely to refer students with behavioral problems rather than recommend suspension or expulsion. Additionally, SBHCs often help students and staff create innovative peer education programs that support peer leadership and peer education programs around risky behaviors.14 While SBHCs may increase school connectedness, SBHCs are often established in schools and communities with substantial social deficits: poverty, discrimination, lowered educational expenditures; these deficits result in lower school connectedness.
To date, studies focusing on the relationship between school connectedness and SBHCs have focused solely on youth attending schools with an SBHC and comparing SBHC users and non-users. It is unclear, however, whether there may be a school-level effect as a function of general SBHC exposure, regardless of use. As noted above, SBHCs can (1) contribute to school-wide programming and decision-making; (2) support teachers by addressing physical and mental health needs of students; (3) serve as an additional resource to both students and administrators; (4) reduce the burden of care placed on teachers; and (5) provide students with a safety net if needed. Therefore, one might expect to see school-wide effects independent of individual students’ use.
Additionally, given that SBHCs aim to address the health needs of underserved youth, it may be that the effect of SBHCs on school connectedness will be stronger among youth of low socioeconomic status (SES). Low-SES youth are more likely to be uninsured than higher-SES youth. They are also less likely to have visited a doctor or dentist, have a medical home, have medication prescribed, or have used hospital outpatient services, and more likely to have used the emergency room, compared to higher-SES youth.15,16 Few studies have examined the differential effects of SBHCs on student subgroups, especially as defined by socioeconomic status; this has been identified by the CDC as an evidence gap.1
Using California state-wide data on over 500 schools, the current study tests two hypotheses:
Youth who attend schools with SBHCs will have higher levels of school connectedness than youth who attend schools without an SBHC;
The relationship between SBHCs and school connectedness will be stronger among low SES youth, regardless of SBHC use.
METHODS
Participants and Procedure
The study used student-level data from the California Healthy Kids Survey (CHKS), administered during the 2013–2014 school year to 1,591 middle and high schools, including alternative schools (n=57), continuation high schools (n=148), middle and junior high schools (n=552) and other school types. The CHKS Survey is a cross-sectional survey administered to California 7th, 9th and 11th grade students to gain insight into student health behaviors and associated correlates. The survey is anonymous, and depending on school and/or district policy, requires active or passive consent prior to administration during a class period (for more information see http://chks.wested.org/about/).
The current study focused on regular public high schools (eg responsible for instruction in the standard curriculum, face-to-face instruction, following local district policy, and divided into distinct grades; n=534). Additionally, 25 charter high schools, 2 high schools with fewer than 10 students who completed surveys, 1 high school without data on parent education level, and 3 high schools with data only on middle school students were excluded. The final analytic dataset included student-level data from 503 high schools. Publicly available aggregated school-level data in order to adjust for school-level differences was merged with this dataset.
Instrumentation
School Connectedness
Caring relationships with a school-based adult, high expectations by a school-based adult, and meaningful participation at school were the three subscales of school connectedness. The subscales were developed using pre-existing items 11 and exhibited high levels of internal consistency (adult caring: α = .81, adult expectations: α = .85; meaningful participation: α = .78).
Each subscale was measured with three positively worded items: “At my schools there is a teacher or some other adult who really cares about me,” “At my school there is a teacher or some other adult who always wants me to do my best”, “At school I do things that make a difference”), with Likert response items ranging from 1 (“not at all”) to 4 (“very much true”). For each subscale, an average and standardized score was calculated if participants responded to at least 2 questions within each subscale.
Student-Level Demographic Variables (Level 1)
Students self-reported their race/ethnicity (White, Black, Hispanic/Latino, Asian or Pacific Islander [A PI], other), sex (male and female), and grade (9 through 12). They also reported the highest education level (college graduate, some college, high school degree, less than high school degree, I don’t know) of the parent who went furthest in school. The latter item was used as a proxy for socioeconomic status.17,18
School-level Variables (Level 2)
A list of all California schools that have health clinics was obtained from the California School-Based Health Alliance (CA-SBHA) website. This list includes a list of school-linked, on-site, and mobile health vans that serve California elementary, middle, and high schools. Included on the list is the name of the SBHC and school name. A dichotomous variable (1 = yes, 0 = no) was created to indicate on-site SBHC.
The following school-level demographic covariates were obtained from the California Department of Education: percentage of students within school with free/reduced price lunch (range: 1.6–98.5%); percentage of White students within school (range: 0.2–87.5%); and total size of student body (range: 31–4,868). All school-level covariates were standardized to equalize the range and assess the relative effect of each variable.
Data Analyses
In the 503 schools, 333,058 students in grades 9–12 completed surveys. A total of 12,218 participants who were missing data for 1 or more school connectedness subscales, and an additional 11,936 participants who were missing data on at least one of the demographic variable were removed. An additional 8,904 participants who self-reported that they only answered some or no questions truthfully were also removed as is the standard.19 The final analytic sample had 300,000 participants.
The analyses were conducted using Stata version 14 (College Station, TX). Differences were described in student- and school-level characteristics between schools with and without SBHCs using frequencies, percentages, and chi-square tests for categorical variables, and means, standard deviations, and t-tests for continuous variables. This was followed by an examination of bivariate associations of the school connectedness variables with student- and school-level variables using means and standard deviations and p-values derived from multilevel linear regression models using Stata’s mixed command, which adjusts for the nesting of students within schools.
Using multilevel linear regression models, final models were built using the following process for each school connectedness variable. In step 1, unconditional models were fit (ie no predictor variables) with random intercepts for schools, which allow the average school connectedness to vary between schools. In step 2, level 1 and level 2 variables were added. In step 3, cross-level interaction between SBHCs and parent education were added. Final models, used Stata’s post-estimation margins command to estimate the predicted standardized scores for each outcome, generating an estimate for each subgroup defined by SBHC presence and parent education, averaged across the other level 1 and 2 variables. Random intercept models were added due to model convergence issues.20
RESULTS
As shown in Table 1, 9.7% of schools (N=49) had SBHCs. Students at schools with SBHCs, compared to students at schools without SBHCs, had significantly lower parent education levels (less than a high school degree: 20.3% vs. 14.9%, respectively) and were less likely to be non-Hispanic White (9.1% vs. 24.1%, respectively). For the school-level variables, schools with SBHCs had significantly lower percentages of the student body that was White and higher percentages of the student body that was eligible for free/reduced price lunch (18.5% vs. 25.9%, respectively) compared to schools without SBHCs.
Table 1.
Characteristics of the Total Sample and by Schools With and Without School-Based Health Centers: California Healthy Kids Survey, California, 2013–2014
| Total sample | Without School-Based Health Center | With School-Based Health Center | |||||
|---|---|---|---|---|---|---|---|
|
|
|
||||||
| n | (%) | n | (%) | n | (%) | p-value | |
| STUDENT-LEVEL VARIABLES | |||||||
| Total Number of Participants (row percentage) | 300,000 | (100.0) | 263,108 | (87.7) | 36,892 | (12.3) | |
| Parent’s Highest Education Level | |||||||
| Less than high school degree | 46,662 | (15.6) | 39,180 | (14.9) | 7,482 | (20.3) | < .01 |
| High school degree | 52,510 | (17.5) | 45,049 | (17.1) | 7,461 | (20.2) | |
| Some college | 42,258 | (14.1) | 37,414 | (14.2) | 4,844 | (13.1) | |
| College degree | 115,479 | (38.5) | 104,871 | (39.9) | 10,608 | (28.8) | |
| Don’t know | 43,091 | (14.4) | 36,594 | (13.9) | 6,497 | (17.6) | |
| Race/ethnicity | |||||||
| Black | 11,559 | (3.9) | 8,927 | (3.4) | 2,632 | (7.1) | < .01 |
| White | 66,800 | (22.3) | 63,431 | (24.1) | 3,369 | (9.1) | |
| Hispanic/Latino | 148,809 | (49.6) | 131,706 | (50.1) | 17,103 | (46.4) | |
| Asian or Pacific Islander | 43,331 | (14.4) | 32,721 | (12.4) | 10,610 | (28.8) | |
| Other | 29,501 | (9.8) | 26,323 | (10.0) | 3,178 | (8.6) | |
| Gender | |||||||
| Male | 145,336 | (48.4) | 127,464 | (48.4) | 17,872 | (48.4) | 0.996 |
| Female | 154,664 | (51.6) | 135,644 | (51.6) | 19,020 | (51.6) | |
| Grade | |||||||
| 9th | 139,310 | (46.4) | 125,440 | (47.7) | 13,870 | (37.6) | < .01 |
| 10th | 23,724 | (7.9) | 17,545 | (6.7) | 6,179 | (16.7) | |
| 11th | 119,402 | (39.8) | 106,987 | (40.7) | 12,415 | (33.7) | |
| 12th | 17,564 | (5.9) | 13,136 | (5.0) | 4,428 | (12.0) | |
| SCHOOL-LEVEL VARIABLES | |||||||
| Total Number of Schools (row percentage) | 503 | (100.0) | 454 | (90.3) | 49 | (9.7) | |
| Total size of student body, mean (sd) | 1,618.3 | (846.5) | 1,615.0 | (849.0) | 1,649.7 | (830.9) | 0.786 |
| Percentage of student body that is White, mean (sd) | 30.7 | (23.7) | 32.8 | (23.6) | 12.1 | (15.5) | < .01 |
| Percentage of student body eligible for free/reduced price lunch, mean (sd) | 54.3 | (25.7) | 52.7 | (25.9) | 69.3 | (18.5) | < .01 |
Note. p-values were derived from chi-square tests for categorical variables and t-tests for continuous variables.
In bivariate analyses of the associations between school connectedness dimensions and student- and school-level characteristics (Table 2), school connectedness outcomes were significantly associated with all student-level variables. Compared to parents with a college degree, students with lower parent educational attainment had lower levels of all three school connectedness dimensions (p < .01 for all Chi-square tests). At the school level, SBHCs were associated with lower average adult expectations (p = .03) and meaningful participation (p = .04), but not associated with adult caring.
Table 2.
Bivariate Associations of School Connectedness Variables (N=300,000): California Healthy Kids Survey, California, 2013–2014
| Adult Caring (unstandardized scale) | Adult Expectations (unstandardized scale) | Meaningful Participation (unstandardized scale) | |||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|||||||
| mean | (sd) | p-value | mean | (sd) | p-value | mean | (sd) | p-value | |
| STUDENT-LEVEL VARIABLES | |||||||||
| Parent’s Highest Education Level | |||||||||
| Less than high school degree | 2.61 | (0.86) | < .01 | 2.85 | (0.87) | < .01 | 2.03 | (0.84) | < .01 |
| High school degree | 2.69 | (0.84) | < .01 | 2.93 | (0.84) | < .01 | 2.13 | (0.85) | < .01 |
| Some college | 2.75 | (0.83) | < .01 | 2.99 | (0.82) | < .01 | 2.19 | (0.84) | < .01 |
| College degree | 2.87 | (0.81) | referent | 3.10 | (0.80) | referent | 2.35 | (0.85) | referent |
| Don’t know | 2.59 | (0.83) | < .01 | 2.85 | (0.85) | < .01 | 2.02 | (0.82) | < .01 |
| Race/ethnicity | |||||||||
| Black | 2.78 | (0.85) | < .01 | 3.01 | (0.86) | < .01 | 2.26 | (0.86) | 0.317 |
| White | 2.90 | (0.82) | referent | 3.10 | (0.80) | referent | 2.31 | (0.85) | referent |
| Hispanic/Latino | 2.66 | (0.85) | < .01 | 2.91 | (0.85) | < .01 | 2.10 | (0.85) | < .01 |
| Asian or Pacific Islander | 2.76 | (0.77) | < .01 | 3.01 | (0.78) | < .01 | 2.28 | (0.84) | 0.075 |
| Other | 2.76 | (0.84) | < .01 | 2.99 | (0.84) | < .01 | 2.24 | (0.86) | < .01 |
| Gender | |||||||||
| Boy | 2.75 | (0.84) | referent | 2.97 | (0.84) | referent | 2.23 | (0.86) | referent |
| Girl | 2.73 | (0.84) | < .01 | 2.99 | (0.83) | < .01 | 2.15 | (0.85) | < .01 |
| Grade | |||||||||
| 9th | 2.68 | (0.83) | referent | 2.97 | (0.83) | referent | 2.19 | (0.83) | referent |
| 10th | 2.67 | (0.84) | < .01 | 2.91 | (0.85) | < .01 | 2.10 | (0.84) | < .01 |
| 11th | 2.81 | (0.84) | < .01 | 3.00 | (0.83) | < .01 | 2.21 | (0.88) | < .01 |
| 12th | 2.84 | (0.86) | < .01 | 2.96 | (0.86) | < .01 | 2.20 | (0.91) | < .01 |
| SCHOOL-LEVEL VARIABLES | |||||||||
| School-based health center | |||||||||
| No | 2.74 | (0.84) | referent | 2.98 | (0.84) | referent | 2.20 | (0.86) | referent |
| Yes | 2.72 | (0.82) | 0.450 | 2.94 | (0.82) | 0.036 | 2.16 | (0.83) | 0.040 |
| Total size of student body, correlation | −0.01 | 0.087 | −0.01 | 0.082 | −0.01 | < .01 | < .01 | ||
| Percentage of student body that is White, correlation | 0.08 | < .01 | 0.06 | < .01 | 0.07 | < .01 | < .01 | ||
| Percentage of student body eligible for free/reduced price lunch, correlation | −0.09 | < .01 | −0.06 | < .01 | 0.08 | < .01 | < .01 | ||
Note. P-values were derived from multilevel models using Stata’s mixed command.
After controlling for student- and school- level variables, overall, there was no significant relationship between SBHCs and any of the school connectedness dimensions. Significant between-school variation indicates that schools differed from one another with regards to overall levels of adult caring (variance component [VC]=0.02; standard error [SE]=0.002), adult expectations (VC=0.02; SE=0.001), and meaningful participation (VC=0.02; SE=0.001). Controlling for covariates, students with higher SES reported significantly higher school connectedness scores on all three dimensions (adult caring, adult expectations, and meaningful participation) compared to students with lower SES (Table 3). There were also significant differences by race and ethnicity, with Black, Hispanic/Latino and API students reporting lower scores compared to White students. Differences also emerged by sex and grade. At the school-level, school size was negatively associated with adult caring, adult expectations, and meaningful participation. Percentage of the school body eligible for free/reduced price lunch was negatively associated with adult caring.
Table 3.
Multivariable Associations of School Connectedness Variables (N=300,000): California Healthy Kids Survey, California, 2013–2014
| Adult Caring (standardized scale) | Adult Expectations (standardized scale) | Meaningful Participation (standardized scale) | ||||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| B (95% CI) | p-value | B (95% CI) | p-value | B (95% CI) | p-value | |
| Intercept | 0.17 (0.16, 0.19) | < .01 | 0.20 (0.18, 0.21) | < .01 | 0.26 (0.25, 0.28) | < .01 |
| STUDENT-LEVEL VARIABLES | ||||||
| Parent’s highest education level | ||||||
| Less than high school degree | −0.25 (−0.26, −0.23) | < .01 | −0.25 (−0.26, −0.24) | < .01 | −0.30 (−0.31, −0.29) | < .01 |
| High school degree | −0.16 (−0.17, −0.15) | < .01 | −0.17 (−0.18, −0.15) | < .01 | −0.20 (−0.21, −0.19) | < .01 |
| Attended some college | −0.10 (−0.12, −0.09) | < .01 | −0.11 (−0.12, −0.09) | < .01 | −0.14 (−0.15, −0.13) | < .01 |
| College degree | referent | referent | referent | |||
| Don’t know | −0.26 (−0.27, −0.25) | < .01 | −0.25 (−0.27, −0.24) | < .01 | −0.33 (−0.34, −0.32) | < .01 |
| Race/ethnicity | ||||||
| Black | −0.07 (−0.09, −0.05) | < .01 | −0.05 (−0.07, −0.03) | < .01 | 0.01 (−0.01, 0.03) | 0.244 |
| White | referent | referent | referent | |||
| Hispanic/Latino | −0.16 (−0.17, −0.15) | < .01 | −0.13 (−0.14, −0.11) | < .01 | −0.11 (−0.12, −0.10) | < .01 |
| Asian or Pacific Islander | −0.14 (−0.15, −0.13) | < .01 | −0.07 (−0.08, −0.06) | < .01 | 0.01 (−0.01, 0.02) | 0.260 |
| Other | −0.11 (−0.12, −0.10) | < .01 | −0.10 (−0.11, −0.08) | < .01 | −0.03 (−0.04, −0.01) | < .01 |
| Gender | ||||||
| Boy | referent | referent | referent | |||
| Girl | −0.02 (−0.03, −0.01) | < .01 | 0.02 (0.02, 0.03) | < .01 | −0.09 (−0.09, −0.08) | < .01 |
| Grade | ||||||
| 9th | referent | referent | referent | |||
| 10th | 0.04 (0.02, 0.06) | < .01 | −0.02 (−0.04, −0.01) | < .01 | −0.05 (−0.07, −0.04) | < .01 |
| 11th | 0.14 (0.13, 0.15) | < .01 | 0.02 (0.01, 0.02) | < .01 | 0.01 (0.01, 0.02) | < .01 |
| 12th | 0.25 (0.23, 0.27) | < .01 | 0.04 (0.02, 0.06) | < .01 | 0.07 (0.05, 0.08) | < .01 |
| SCHOOL-LEVEL VARIABLES | ||||||
| School-based health center | ||||||
| No | referent | referent | referent | |||
| Yes | 0.03 (−0.01, 0.07) | 0.095 | −0.01 (−0.04, 0.03) | 0.755 | −0.01 (−0.05, 0.02) | 0.430 |
| Total size of student body | −0.01 (−0.03, −0.00) | 0.037 | −0.01 (−0.03, −0.00) | 0.032 | −0.03 (−0.04, −0.02) | < .01 |
| Percentage of student body that is White | 0.00 (−0.02, 0.02) | 0.950 | 0.00 (−0.02, 0.02) | 0.905 | −0.01 (−0.02, 0.01) | 0.403 |
| Percentage of student body eligible for free/reduced price lunch | −0.02 (−0.04, −0.00) | 0.019 | 0.00 (−0.01, 0.02) | 0.616 | −0.00 (−0.02, 0.01) | 0.662 |
Note. CI = confidence interval.
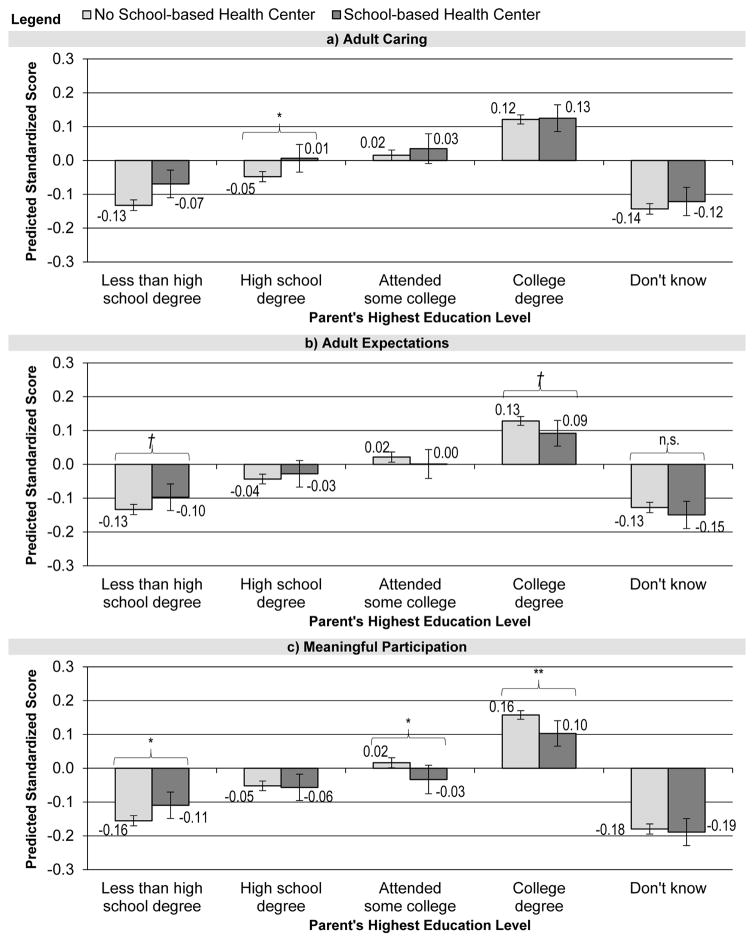
In interaction analyses, the effects of SBHCs were more positively associated with adult caring, adult expectations, and meaningful participation among students with lower SES compared to students with higher SES (Table 4 and Figure 1). For adult caring, there was no difference between attending schools with or without SBHCs for students who had parents with a college degree. However, the effects of attending a school with SBHC significantly increased adult caring for students of lower SES, those whose parents had either a high school degree or less than a high school degree. Among students whose parents had less than a high school degree, for instance, predicted standardized scores were 0.06 points higher among students in SBHC schools for adult caring, 0.04 for adult expectations, and 0.03 for meaningful participation than among students of the same SES level in schools without an SBHC.
Table 4.
Multivariable Associations of School Connectedness Variables with Cross-Level Interactions between School-based Health Centers and Parent’s Highest Education Level (N=300,000): California Healthy Kids Survey, California, 2013–2014
| Adult Caring (standardized scale) | Adult Expectations (standardized scale) | Meaningful Participation (standardized scale) | ||||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| B (95% CI) | p-value | B (95% CI) | p-value | B (95% CI) | p-value | |
| Intercept | 0.18 (0.16, 0.19) | < .01 | 0.20 (0.18, 0.21) | < .01 | 0.27 (0.25, 0.28) | < .01 |
| STUDENT-LEVEL VARIABLES | ||||||
| Parent’s highest education level | ||||||
| Less than high school degree | −0.25 (−0.27, −0.24) | < .01 | −0.26 (−0.27, −0.25) | < .01 | −0.31 (−0.33, −0.30) | < .01 |
| High school degree | −0.17 (−0.18, −0.16) | < .01 | −0.17 (−0.18, −0.16) | < .01 | −0.21 (−0.22, −0.20) | < .01 |
| Attended some college | −0.11 (−0.12, −0.09) | < .01 | −0.11 (−0.12, −0.09) | < .01 | −0.14 (−0.15, −0.13) | < .01 |
| College degree | referent | referent | referent | |||
| Don’t know | −0.26 (−0.28, −0.25) | < .01 | −0.26 (−0.27, −0.24) | < .01 | −0.34 (−0.35, −0.32) | < .01 |
| Race/ethnicity | ||||||
| Black | −0.07 (−0.09, −0.05) | < .01 | −0.05 (−0.07, −0.03) | < .01 | 0.01 (−0.01, 0.03) | 0.193 |
| White | referent | referent | referent | |||
| Hispanic/Latino | −0.16 (−0.17, −0.15) | < .01 | −0.13 (−0.14, −0.11) | < .01 | −0.11 (−0.12, −0.10) | < .01 |
| Asian or Pacific Islander | −0.14 (−0.15, −0.13) | < .01 | −0.07 (−0.08, −0.06) | < .01 | 0.01 (−0.01, 0.02) | 0.247 |
| Other | −0.11 (−0.12, −0.09) | < .01 | −0.10 (−0.11, −0.08) | < .01 | −0.03 (−0.04, −0.01) | < .01 |
| Gender | ||||||
| Boy | referent | referent | referent | |||
| Girl | −0.02 (−0.03, −0.01) | < .01 | 0.02 (0.02, 0.03) | < .01 | −0.09 (−0.09, −0.08) | < .01 |
| Grade | ||||||
| 9th | referent | referent | referent | |||
| 10th | 0.04 (0.02, 0.06) | < .01 | −0.02 (−0.04, −0.01) | < .01 | −0.05 (−0.07, −0.03) | < .01 |
| 11th | 0.14 (0.13, 0.15) | < .01 | 0.02 (0.01, 0.02) | < .01 | 0.01 (0.01, 0.02) | < .01 |
| 12th | 0.25 (0.23, 0.26) | < .01 | 0.04 (0.02, 0.06) | < .01 | 0.07 (0.05, 0.08) | < .01 |
| SCHOOL-LEVEL VARIABLES | ||||||
| School-based health center | ||||||
| No | referent | referent | referent | |||
| Yes | 0.00 (−0.04, 0.05) | 0.863 | −0.04 (−0.08, 0.00) | 0.075 | −0.05 (−0.09, −0.02) | < .01 |
| Total size of student body | −0.01 (−0.03, −0.00) | 0.038 | −0.01 (−0.02, −0.00) | 0.033 | −0.03 (−0.04, −0.02) | < .01 |
| Percentage of student body that is White | 0.00 (−0.02, 0.02) | 0.964 | 0.00 (−0.02, 0.02) | 0.922 | −0.01 (−0.02, 0.01) | 0.381 |
| Percentage of student body eligible for free/reduced price lunch | −0.02 (−0.04, −0.00) | 0.022 | 0.00 (−0.01, 0.02) | 0.577 | −0.00 (−0.02, 0.01) | 0.712 |
| CROSS-LEVEL INTERACTIONS | ||||||
| Parent’s highest education level × School-based health center | ||||||
| Less than high school degree × School-based health center | 0.06 (0.03, 0.09) | < .01 | 0.07 (0.04, 0.11) | < .01 | 0.10 (0.07, 0.13) | < .01 |
| High school degree × School-based health center | 0.05 (0.02, 0.08) | < .01 | 0.05 (0.02, 0.08) | < .01 | 0.05 (0.02, 0.08) | < .01 |
| Attended some college × School-based health center | 0.02 (−0.02, 0.05) | 0.386 | 0.02 (−0.02, 0.05) | 0.384 | 0.01 (−0.03, 0.04) | 0.783 |
| College degree × School-based health center | referent | referent | referent | |||
| Don’t know × School-based health center | 0.02 (−0.02, 0.05) | 0.293 | 0.01 (−0.02, 0.05) | 0.400 | 0.05 (0.01, 0.08) | < .01 |
Note. CI = confidence interval
Figure 1. Predicted Standardized School Connectedness Scores for Students With and Without School-based Health Centers by Parent’s Highest Education Level (N=300,000): California Healthy Kids Survey, California, 2013–2014.
Note. Predicted scores were estimated from multilevel linear regression models and averaged across level 1 and level 2 variables. P-values were calculated using Stata’s post estimation lincom command, which estimated p-values from linear combinations of coefficients based on the final models with the cross-level interactions. † p < .10; * p< .05; ** p < .01
DISCUSSION
These analyses, conducted using data from a large sample of racially and ethnically diverse high school students from more than 500 schools in California, provide support for a positive effect of SBHC presence for low SES students on some dimensions of school connectedness, independent of SBHC utilization. With regards to the first hypothesis, students in schools with an SBHC did not differ from students in schools without SBHCs with regards to school connectedness. However, a more nuanced examination, taking into account the strong confounding between student- and school-level characteristics and the presence of an SBHC, revealed support for the second hypothesis. Specifically, that the positive effect of SBHC presence was stronger and significant specifically for students of lower SES. In multilevel models examining cross-level interactions, students of lower SES in a school with an SBHC scored higher on all three dimensions of school connectedness compared to low-SES students in a school without SBHCs, and SBHCs were not as protective for higher-SES students.
The analyses are consistent with previous findings that noted a significant link between SBHC utilization and higher levels of school connectedness,3,11 and expand this to some segments of the broader school population independent of SBHC utilization. Most importantly, these findings suggest that SBHCs can have a positive effect on the most vulnerable students. School connectedness is linked to improved academic outcomes, and better psychosocial and health status. Adolescents of lower SES, in other studies, have been found to have lower levels of school connectedness, in addition to other social belonging factors that are protective of behavioral and emotional health for adolescents, including community support and parent connectedness.5,22–25 The analyses here indicate the same: there was a strong inverse dose-response relationship between SES and all three dimensions of school connectedness. Given the links between SES and lower levels of social support and social belonging found in these other studies, and the significant impact on school connectedness for students with parents with lowest educational attainment in multilevel analyses presented here, these findings provide support that SBHCs can promote connectedness and support in the school setting where it may be lacking in other settings, such as at home or in communities.
These findings should be considered in the context of some limitations. First, variables of interest were limited, given the use of a publicly-available dataset not designed to answer this particular research question. For example, parents’ educational attainment was used as a crude proxy for socioeconomic status, with some research suggesting that the incomes of people with the same educational level can widely vary based on race, ethnicity, sex, and age.21 Second, while the dataset has a large, diverse sample suggesting external validity to broad population groups, the data are only from schools in California and therefore may not generalize to other settings. And third, the study is cross-sectional and correlational and thus causality assumptions and selection concerns exist. However, by controlling for school-level characteristics associated with the presence or absence of SBHCs, the study aims to address selection effects. Large longitudinal datasets are needed to examine changes in school climate following SBHC implementation.
Despite these limitations, the findings point to a possible mechanism of action whereby SBHCs impact positive health and academic outcomes through school connectedness among lower SES youth. The current study is a necessary starting point to inform future research such as ascertaining what specific strategies, messages, training, and/or outreach are being conducted by SBHCs that are effective in supporting school connectedness and to what extent these approaches can be replicated across SBHC and non-SBHC campuses to have a wide-reaching effect.
IMPLICATIONS FOR SCHOOL HEALTH
Efforts to promote health through SBHCs and to enhance school connectedness may lead to improved adolescent health and wellbeing. The first goal (promoting health through SBHCs) may also contribute to the second goal (enhancing school connectedness), particularly for low-SES adolescents. Similar to the Whole School, Whole Community, Whole Child (WSCC) model, it is necessary to move beyond the question of are these models effective or not. Rather, the focus now should be on examining what factors or combination of factors makes these environmental approaches successful. Additional research will be needed to examine the specific ways in which SBHCs operationalize school connectedness to promote safety and social support for vulnerable adolescent populations, as defined by socioeconomic status or other characteristics associated with behavioral and emotional health such as family structure or sexual orientation. With SBHCs now serving more than 2.3 million children and adolescents,26 identifying and deploying strategies to promote school connectedness has the potential to reach a significant segment of the population.
Acknowledgments
This study was supported by Grant Number 1R01HD073386-01A1 from the National Institute of Child Health and Human Development (NICHD) and the National Institute on Drug Abuse (F31DA037647). The contents of this paper are solely the responsibility of the authors and do not necessarily represent official views of NICHD or NIH.
Footnotes
Human Subjects Approval Statement
This study was approved by the Prevention Research Centers Institutional Review Board (IRBnet # 555340-21).
Contributor Information
Melina Bersamin, Senior Research Scientist, Prevention Research Center, 180 Grand Ave. Suite, 1200, Oakland CA, 94612, Phone: 510-883-5712, Fax: 510-644-0594.
Robert W. S. Coulter, Doctoral Candidate, Department of Behavioral and Community Health Sciences, Graduate School of Public Health, University of Pittsburgh, 130 De Soto Street, Pittsburgh, PA 15261, Phone: 716-297-1790.
Jenna Gaarde, Research Assistant, Prevention Research Center, 180 Grand Ave. Suite, 1200, Oakland CA, 94612, Phone: 510-883-5712, Fax: 510-644-0594.
Samantha Garbers, Assistant Professor, Department of Population and Family Health, Columbia University Mailman School of Public Health, 60 Haven Ave, B-2, Room 2D, New York, NY 10032, Phone: 212-305-0123, Fax: 212-305-7024.
Christina Mair, Assistant Professor, Department of Behavioral and Community Health Sciences, Graduate School of Public Health, University of Pittsburgh, 130 De Soto Street, Pittsburgh, PA 15261, Phone: 412-624-3613.
John Santelli, Chair, Department of Population and Family Health, Columbia University Mailman School of Public Health, 60 Haven Ave, B-2, New York, NY 10032, Phone: 212-304-5200, Fax: 212-305-7024.
References
- 1.Guide to Community Preventive Services. Promoting health equity through education programs and policies: School-based health centers. 2015 http://www.thecommunityguide.org/healthequity/education/schoolbasedhealthcenters.html, 2016.
- 2.Strolin-Goltzman J. The relationship between school-based health centers and the learning environment. J Sch Health. 2010;80(3):153–159. doi: 10.1111/j.1746-1561.2009.00480.x. [DOI] [PubMed] [Google Scholar]
- 3.Strolin-Goltzman J, Sisselman A, Melekis K, Auerbach C. Understanding the relationship between school-based health center use, school connection, and academic performance. Health Soc Work. 2014;39(2):83–91. doi: 10.1093/hsw/hlu018. [DOI] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention. Atlanta, GA: US Department of Health and Human Services; 2009. School connectedness: Strategies for increasing protective factors among youth. [Google Scholar]
- 5.Thompson D, Iachan R, Overpeck M, Ross J, Gross L. School connectedness in the health behavior in school-aged children study: The role of student, school, and school neighborhood characteristics. J Sch Health. 2006;76(7):379–386. doi: 10.1111/j.1746-1561.2006.00129.x. [DOI] [PubMed] [Google Scholar]
- 6.Chung-Do JJ, Goebert DA, Chang JY, Hamagani F. Developing a comprehensive school connectedness scale for program evaluation. J Sch Health. 2015;85(3):179–188. doi: 10.1111/josh.12237. [DOI] [PubMed] [Google Scholar]
- 7.McNeely CA, Nonnemaker JM, Blum RW. Promoting school connectedness: Evidence from the National Longitudinal Study of Adolescent Health. J Sch Health. 2002;72(4):138–146. doi: 10.1111/j.1746-1561.2002.tb06533.x. [DOI] [PubMed] [Google Scholar]
- 8.Whitlock JL. Youth perceptions of life at school: Contextual correlates of school connectedness in adolescence. Appl Dev Sci. 2006;10(1):13–29. [Google Scholar]
- 9.Resnick MD, Bearman PS, Blum RW, et al. Protecting adolescents from harm: Findings from the National Longitudinal Study on Adolescent Health. JAMA. 1997;278(10):823–832. doi: 10.1001/jama.278.10.823. [DOI] [PubMed] [Google Scholar]
- 10.Resnick MD, Harris LJ, Blum RW. The impact of caring and connectedness on adolescent health and well-being. J Paediatr Child Health. 1993;29(s1):S3–S9. doi: 10.1111/j.1440-1754.1993.tb02257.x. [DOI] [PubMed] [Google Scholar]
- 11.Stone S, Whitaker K, Anyon Y, Shields JP. The relationship between use of school-based health centers and student-reported school assets. J Adolesc Health. 2013;53(4):526–532. doi: 10.1016/j.jadohealth.2013.05.011. [DOI] [PubMed] [Google Scholar]
- 12.Geierstanger SP, Amaral G, Mansour M, Walters SR. School-Based Health Centers and Academic Performance Research Challenges and Recommendations. J Sch Health. 2001;74(9):347–352. doi: 10.1111/j.1746-1561.2004.tb06627.x. [DOI] [PubMed] [Google Scholar]
- 13.Blum RW, Libbey HP. Wingspread declaration on school connections. J Sch Health. 2004;74(7):233–234. doi: 10.1111/j.1746-1561.2004.tb08279.x. [DOI] [PubMed] [Google Scholar]
- 14.Sisselman A, Strolin-Goltzman J, Auerbach C, Sharon L. Innovative services offered by school-based health centers in New York City. Child Sch. 2012;34(4):213–221. [Google Scholar]
- 15.Strickland BB, Jones JR, Ghandour RM, Kogan MD, Newacheck PW. The medical home: health care access and impact for children and youth in the United States. Pediatrics. 2011;127(4):604–611. doi: 10.1542/peds.2009-3555. [DOI] [PubMed] [Google Scholar]
- 16.Simpson L, Owens PL, Zodet MW, et al. Health care for children and youth in the United States: Annual report on patterns of coverage, utilization, quality, and expenditures by income. Ambul Pediatr. 2005;5(1):6–e20. doi: 10.1367/A04-119R.1. [DOI] [PubMed] [Google Scholar]
- 17.Bornstein MH, Hahn C-S, Suwalsky JT, Haynes OM. The Hollingshead four-factor index of social status and the socioeconomic index of occupations. Socioeconomic status, parenting, and child development. In: Bornstein MH, Bradley RH, editors. Socioeconomic status, parenting, and child development. Mahwah, NJ: Erlbaum; 2003. pp. 29–82. [Google Scholar]
- 18.Entwisle DR, Astone NM. Some practical guidelines for measuring youth’s race/ethnicity and socioeconomic status. Child Dev. 1994;65(6):1521–1540. [Google Scholar]
- 19.Kim EK, Furlong MJ, Dowdy E, Felix ED. Exploring the relative contributions of the strength and distress components of dual-factor complete mental health screening. Can J Sch Psychol. 2014;29(2):127–140. [Google Scholar]
- 20.Snijders TAB, Bosker RJ. Multilevel analysis: An introduction to basic and advanced multilevel modeling. 2. London: Sage Publishers; 2012. [Google Scholar]
- 21.Braveman PA, Cubbin C, Egerter S, et al. Socioeconomic status in health research: one size does not fit all. JAMA. 2005;294(22):2879–2888. doi: 10.1001/jama.294.22.2879. [DOI] [PubMed] [Google Scholar]
- 22.Escarce JJ. Socioeconomic status and the fates of adolescents. Health Serv Res. 2003;38(5):1229–1233. doi: 10.1111/1475-6773.00173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.McNeely CA, Falci C. School Connectedness and the Transition Into and Out of Health-Risk Behavior among Adolescents: A Comparison of Social Belonging and Teacher Support. J Sch Health. 2004;74(7):284–292. doi: 10.1111/j.1746-1561.2004.tb08285.x. [DOI] [PubMed] [Google Scholar]
- 24.Daly B, Buchanan C, Dasch K, Eichen D, Lenhart C. Promoting school connectedness among urban youth of color: Reducing risk factors while promoting protective factors. The Prevention Researcher. 2010;17(3):18–21. [Google Scholar]
- 25.McLoyd VC, Kaplan R, Purtell KM, Bagley E, Hardaway CR, Smalls C. Poverty and socioeconomic disadvantage in adolescence. In: Lerner R, Steinberg L, editors. Handbook of Adolescent Psychology. Hoboken, NJ: John Wiley & Sons; 2009. pp. 444–491. [Google Scholar]
- 26.Lofink H, Schelar E, Taylor K, Schlitt J, Even M, Burns A, et al. 2013–2014 School-Based Health Alliance Census Report. Washington, D.C: School-Based Health Alliance; 2015. [Google Scholar]