Abstract
Background and Purpose:
While providing medical services, hospitals generate many data about patients. Such medical data could contribute to better treatments once their associations or patterns have been identified. With properly analyzed medical data, traditional knowledge at an individual level could be further extended to broader populations. This comprehensive study was performed to demonstrate the effectiveness of light using medical data accumulated over 15 years.
Methods:
Patients who were admitted to the window or door side of a six-bedded room were included. Patients admitted to the emergency room and elderly people aged >80 years were excluded. Patients’ length of stay was compared per what bed they were in (excluding middle beds). A multiple regression analysis was performed with patients admitted to the window or door side to determine whether the window affected their hospital stay. In addition, a multiple regression analysis was performed after adjusting for confounders by 1:1 matching between the two groups (ie, age, sex, and admitting department).
Results:
Participants were 38 788 patients with a bed near the window and 46 233 patients with a bed near the door. Results revealed that patients’ length of stay was shorter for those near the window compared with those near the door, which was also true after group matching (33 921 participants in each group).
Conclusions:
Clinical trials that test evidence-based designs of physical environments in wards or hospital rooms are usually difficult to perform. As an alternative strategy, using accumulated electronic medical data, we assessed this key element of hospital design.
Keywords: Electronic medical record, database, light, evidence-based design, physical environment
Introduction
It is difficult to alter the architecture of hospitals after they are built; therefore, it is necessary to consider various treatment-related aspects beforehand, both for the benefits of patients and health care providers. Traditionally, medicine has pursued evidence-based treatments, which establish a procedure by defining and measuring changes in outcomes, depending on the presence or absence of a treatment, and by judging their efficacy. Moreover, architecture has introduced the concept of evidence-based designs. Since any change in the physical environment might affect the progress of diseases in various ways, the rationale for studying these associations is clear. The belief that the physical environment of a hospital could affect the recovery of patients has existed since ancient times; however, it is difficult to support this assumption, because randomized controlled trials—although often conducted in medicine—are rarely adopted in architecture.
Medical facilities, whose aims are the prevention and diagnosis of diseases as well as rehabilitation, consist of various types of spatial areas to achieve those purposes. A ward is the medical place where patients tend to stay for the longest period; therefore, ward environments directly or indirectly affect treatment outcomes. Many studies have examined the effects of various physical ward environments on disease outcomes of including the reduction of hospital-acquired infections. For example, physicians have strived to reduce iatrogenic infections. Because an infection is caused by contact, physical isolation between patients, ventilation system components, and easy-to-clean facilities are key architectural features.
Light is another critical ward environment aspect that not only leads to a decrease in patients’ distress but can also increase patient satisfaction.1–4 Full-spectrum light prophylactically controls viral and staph infections and also significantly improves physical working capacity by decreasing heart and pulse rates, lowering systolic blood pressure, and increasing oxygen uptake.5 Inadequate light has a direct effect on fatigue, diseases, insomnia, alcohol addictions, suicides, and other psychiatric diseases.6 Therefore, light has been emphasized and used in the design of medical facilities.1,3 It is noteworthy that the effectiveness of light can be better understood in relation to length of stay (LOS) because it has been reported that exposure to light affects LOS.3
Generally, while providing medical services, hospitals generate many data about patients, and this massive medical information is accumulated and stored digitally. Such medical data could contribute to better treatments once their associations or patterns have been identified. With properly analyzed medical data, traditional knowledge at an individual level could be further extended to broader populations. Therefore, this comprehensive study was performed to demonstrate the effectiveness of light using medical data accumulated over 15 years.
Methods
Participants
This study used information from a hospital database from January 1, 1998 to December 31, 2013. With 1031 beds, a hospital ward comprises one-, two-, four-, or six-bedded rooms. When a patient is hospitalized, he or she is randomly placed in an empty room in our hospital. Beds close to the door had restricted light and beds close to the window had light. Length of stay was defined as the time from hospital admission to discharge.
Inclusion and exclusion criteria
Outpatients and patients admitted to the emergency room, elderly people aged >80 years, persons who were moved to a hospital within 3 days after admission, and patients admitted for more than 180 days were excluded. Patients’ data were included in this study if they had been hospitalized in a six-bedded room and assigned to a bed either next to the window or next to the door and had not changed beds or rooms (patients with a bed in the middle were excluded).
Study design and independent variable matching
A retrospective cohort study design was used to compare the group that was exposed to natural light (window) and the group that was not (door). In public health, a retrospective cohort design can be used to compare groups of individuals. Recently, the use of observational data has increased, and many investigators use matching techniques to create a control group that is similar to the treatment group. We used the exact matching method, that is, select one patient in the case group (window) and one patient in the control group (door) with the same characteristics (ie, age, sex, admitting department). Because the data did not include illness severity and LOS can differ based on department, we matched admitting department. Medical departments were grouped appropriately. The number of patients admitted to each department was counted, and the rest were grouped except for the top five departments. All study protocols were reviewed and approved by the hospital’s institutional review board.
Statistical analyses
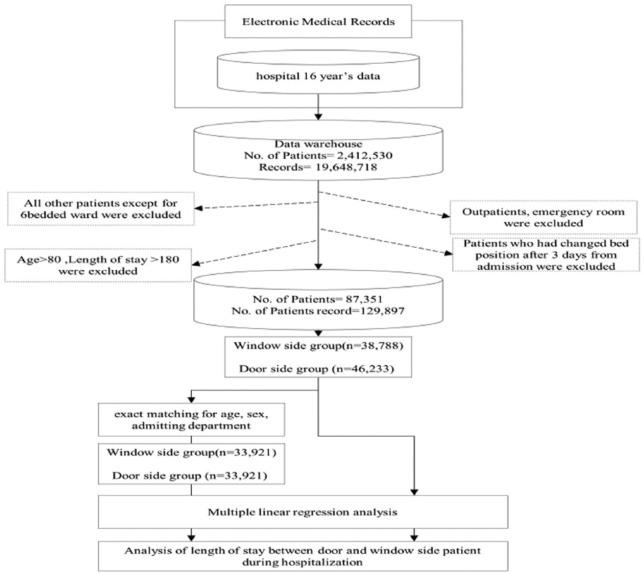
Chi-square tests were employed to compare categorical variables (ie, age group, sex, and department) at the time of hospitalization. The Mann-Whitney test for nonparametric data was employed to compare continuous variables, such as age and LOS. A multiple linear regression analysis was performed to examine what variables affected LOS. In addition, a multiple linear regression analysis was again performed after 1:1 exact matching (see Figure 1).
Figure 1.
Study design and work flow.
Software tools
All data were processed using Eclipse 4.2.2 (IBM, Riverton, NJ) for Java Programming, MS-SQL 2008 (Microsoft, Redmond, WA) for the database management system, and the R package (R Development Core Team, Vienna, Austria) for statistical analyses.
Results
LOS analysis before exact matching
Participants baseline characteristics and LOS are shown in Table 1. The age, sex, department, and LOS of both groups significantly differed.
Table 1.
Baseline characteristics and LOS of window side and door side group before 1:1 matching.
| Characteristics | Door side group (N = 46 233) | Window side group (N = 38 788) | P-value |
|---|---|---|---|
| Sex, n (%) | <.001 | ||
| Male | 25 764 (55.7%) | 20 685 (53.3%) | |
| Female | 20 469 (44.3%) | 18 103 (46.7%) | |
| Age | 44.0 [20.0; 61.0] | 39.0 [12.0; 58.0] | <.001a |
| Age categories, n (%) | <.001 | ||
| 0–10 | 8759 (20.5%) | 9156 (25.3%) | |
| 11–20 | 2795 (6.5%) | 2713 (7.5%) | |
| 21–30 | 3211 (7.5%) | 2908 (8.0%) | |
| 31–40 | 4756 (11.1%) | 4135 (11.4%) | |
| 41–50 | 5800 (13.6%) | 4721 (13.1%) | |
| 51–60 | 6280 (14.7%) | 4855 (13.4%) | |
| 61–70 | 6229 (14.6%) | 4576 (12.7%) | |
| >70 | 4928 (11.5%) | 3091 (8.5%) | |
| Department, n (%) | <.001 | ||
| GS | 6546 (14.2%) | 5617 (14.5%) | |
| PED | 5855 (12.7%) | 5929 (15.3%) | |
| ENT | 4686 (10.1%) | 4435 (11.4%) | |
| GIMD | 4510 (9.8%) | 2918 (7.5%) | |
| HOMD | 2882 (6.2%) | 2639 (6.8%) | |
| OS | 2887 (6.2%) | 2138 (5.5%) | |
| Others | 18 867 (40.8%) | 15 112 (39.0%) | |
| Length of stay | 5.0 [3.0; 8.0] | 4.0 [3.0; 7.0] | <.001a |
Abbreviations: ENT, ear, nose, throat; GIMD, gastrointestinal medicine; GS, general surgery; HOMD, hemato-oncology; LOS: length of stay; OS, orthopedic surgery; PED, pediatrics.
The Mann-Whitney test was performed.
A multiple regression analysis was conducted to determine whether there was any difference in LOS between groups after controlling for confounding variables. After controlling for confounders, the LOS of the window side group was still significantly shorter than the LOS of the door side group (Table 2).
Table 2.
Summary of multiple linear regression for variables predicting LOS.
| Coefficient | Length of stay | |||
|---|---|---|---|---|
| Estimates | Std. error | Conf. int (95%) | P-value | |
| (Intercept) | 4.58 | 0.09 | 4.41 to 4.75 | <.001 |
| Window side group | −0.43 | 0.05 | −0.52 to −0.34 | <.001 |
| Female | −0.03 | 0.05 | −0.12 to 0.06 | .549 |
| Age | 0.04 | 0.00 | 0.04 to 0.04 | <.001 |
| Department: PED | 0.08 | 0.10 | −0.11 to 0.27 | .393 |
| Department: ENT | −1.28 | 0.09 | −1.46 to −1.10 | <.001 |
| Department: GIMD | 0.51 | 0.10 | 0.32 to 0.70 | <.001 |
| Department: HOMD | −0.31 | 0.11 | −0.52 to −0.10 | .003 |
| Department: OS | 5.31 | 0.11 | 5.09 to 5.52 | <.001 |
| Department: Others | 0.59 | 0.07 | 0.46 to 0.73 | <.001 |
| Observations | 85 021 | |||
| R2/adjusted R2 | 0.064/0.064 | |||
Abbreviations: ENT, ear, nose, throat; GIMD, gastrointestinal medicine; GS, general surgery; HOMD, hemato-oncology; LOS: length of stay; OS, orthopedic surgery; PED, pediatrics.
LOS analysis after 1:1 exact matching
Participants’ baseline characteristics and LOS after 1:1 exact matching are shown in Table 3. After matching, all variables except LOS showed no significant difference between the two groups.
Table 3.
Baseline characteristics and LOS of window side and door side group after 1:1 matching.
| Characteristics | Door side group (N = 33 921) | Window side group (N = 33 921) | P-value |
|---|---|---|---|
| Sex, n (%) | 1.000 | ||
| Male | 18 489 (54.5%) | 18 489 (54.5%) | |
| Female | 15 432 (45.5%) | 15 432 (45.5%) | |
| Age | 39.0 [9.0; 57.0] | 39.0 [9.0; 57.0] | .825 |
| Age categories, n (%) | .913 | ||
| 0–10 | 8832 (28.0%) | 8785 (27.7%) | |
| 11–20 | 2135 (6.8%) | 2187 (6.9%) | |
| 21–30 | 2254 (7.1%) | 2299 (7.3%) | |
| 31–40 | 3471 (11.0%) | 3478 (11.0%) | |
| 41–50 | 4052 (12.8%) | 4085 (12.9%) | |
| 51–60 | 4246 (13.4%) | 4251 (13.4%) | |
| 61–70 | 3945 (12.5%) | 4022 (12.7%) | |
| >70 | 2644 (8.4%) | 2580 (8.1%) | |
| Department, n (%) | 1.000 | ||
| GS | 6148 (18.1%) | 6148 (18.1%) | |
| PED | 5141 (15.2%) | 5141 (15.2%) | |
| ENT | 3934 (11.6%) | 3934 (11.6%) | |
| GIMD | 2684 (7.9%) | 2684 (7.9%) | |
| HOMD | 2342 (6.9%) | 2342 (6.9%) | |
| OS | 1824 (5.4%) | 1824 (5.4%) | |
| Others | 11 848 (34.9%) | 11 848 (34.9%) | |
| Length of stay | 4.0 [3.0; 6.0] | 4.0 [3.0; 6.0] | <.001a |
Abbreviations: ENT, ear, nose, throat; GIMD, gastrointestinal medicine; GS, general surgery; HOMD, hemato-oncology; LOS: length of stay; OS, orthopedic surgery; PED, pediatrics.
The Mann-Whitney test was performed.
A multiple regression analysis was performed once again, which determine that light affected LOS after 1:1 exact matching (Table 4).
Table 4.
Summary of multiple linear regression for variables predicting LOS after window side group and door side group 1:1 matching.
| Coefficient | Length of stay | |||
|---|---|---|---|---|
| Estimates | Std. error | Conf. int (95%) | P-value | |
| (Intercept) | 4.32 | 0.04 | 4.24 to 4.40 | <.001 |
| Window side group | −0.12 | 0.03 | −0.17 to -0.06 | <.001 |
| Female | 0.03 | 0.03 | −0.03 to 0.09 | .281 |
| Age | 0.03 | 0.00 | 0.03 to 0.03 | <.001 |
| Department: PED | −0.34 | 0.06 | −0.45 to −0.22 | <.001 |
| Department: ENT | −1.27 | 0.06 | −1.38 to −1.15 | <.001 |
| Department: GIMD | −0.06 | 0.07 | −0.20 to 0.09 | .451 |
| Department: HOMD | −1.04 | 0.08 | −1.19 to −0.89 | <.001 |
| Department: OS | 3.14 | 0.08 | 2.99 to 3.29 | <.001 |
| Department: Others | −0.35 | 0.05 | −0.45 to −0.24 | <.001 |
| Observations | 67 842 | |||
| R2/adjusted R2 | 0.082/0.081 | |||
Abbreviations: ENT, ear, nose, throat; GIMD, gastrointestinal medicine; GS, general surgery; HOMD, hemato-oncology; LOS: length of stay; OS, orthopedic surgery; PED, pediatrics.
Discussion
The focus on productivity and cost-containment in health care systems is currently a sustaining challenge to hospital management. The LOS in a hospital represents one of the most essential aspects to measure the quality of patient care and it is one of the most widely used variables to evaluate resource allocation in hospitals. Length of stay is also a critical measure to determine the required number of beds for hospitals during planning,7 and it is a key indicator for comparing procedures in hospitals across countries.8 Allocating beds and resources efficiently by shortening patients’ LOS is a chief way to achieve maximum productivity in hospitals.9 Reducing LOS restores hospital capacity, increases productivity and profits, decreases waiting lists, and heightens patient satisfaction. Furthermore, the beneficial effects of LOS on the public through the National Insurance System have been reviewed intensively. Several methods, such as early discharge planning, have been recommended for reducing LOS.8 Medical personnel involved in patients’ hospital care is under certain pressures worldwide to minimize LOS.10 Because the LOS is a very robust variable to evaluate the performance of hospitals, we selected it as our key variable.
Some studies have investigated light and its efficacy as part of the ward environment. Lewy et al11 found that being exposed to light had a faster effect than did taking antidepressants; they reported that it took at least 4-6 weeks for an antidepressant to show its effect in seasonal depressive disorders, whereas light could decrease depressive symptoms within 2 weeks. Morning light was also more effective than afternoon or night light. Walch et al12 examined spinal surgery patients and randomly assigned them to two conditions: a ward with light versus a ward with the light blocked. Being exposed to more than 46% light, the patients tended to report less distress and pains than did those in the dark ward, and they also needed 22% fewer painkillers, which led to 21% savings in total treatment costs. Furthermore, light is especially effective when targeting patients with psychiatric disorders, particularly depression.
These results suggest that it is vital to consider light in ward arrangements;3 however, there have been few studies scrutinizing the differences in LOS depending on light conditions. Beauchemin and Hays13 reported that the LOS of patients with depression in a bright ward was brief (mean = 2.6 days), and Beauchemin and Hays14 further found that the LOS of patients after myocardial infarction, especially women, was short-lived (mean = 3.7 days). In addition, in Korea, Kim15 showed that light had a positive effect on patients’ resilience, which decreased their LOS.
There have been a few investigations that directly examined the relationship between light and LOS; however, they examined specific clinical samples. Therefore, it is difficult to generalize prior findings to broader populations due to limitations such as small sample sizes, short research durations, and specific-disease study populations. Consequently, it is necessary to examine the effectiveness of light on patients with diverse diseases to compensate for such limitations.4
Although we posit that light depending on the location of beds has the primary influence on LOS, there are other likely mediating variables. First, light might have affected medical errors. Many studies have reported that illumination has an effect on performance, suggesting that a visual inspection could be disturbed at a low light level.16 In addition, other studies have demonstrated that errors in medication dispensing differ depending on light levels.17 However, the idea that low light could have increased medical errors, and that this in turn increased the LOS is not convincing, because areas far from a window are maintained at more than 1500 lux, which would not be considered as dark.
Second, light in a ward may have had an influence on sleep. Experiencing stress due to a disease would reasonably alter a patient’s sleeping patterns, and defective sleep itself can increase stress and delirium18,19 and decrease immunity.20 Such processes might elevate the morbidity stemming from diseases.21,22 Given that a light change reflected in the retina is the most influential factor for circadian rhythm, the nearer a patients is to a window, the more light he or she gets exposed to, which might have affected circadian rhythms and consequently lowered his or her LOS. Many studies have reported that a decrease in light due to the ward design, such as the location of the beds, leads to poor nighttime sleep.23,24
Other mediators in the ward design are also plausible. Many investigations have suggested that having a good view has a positive effect on the treatment outcomes of diseases. Depending on the presence of a window, some patients would have had an outside view whereas others would not. Perhaps watching the “outside world” decreases patients’ stress and improves disease outcomes. In addition, noise may have affected LOS. Noise can influence performance in medicine.25 Although some studies raised doubts about the effect of noise, their crucial limitation was that their experiments lacked real clinical relevance.26,27 Patients next to the doors could have been exposed to more noise (from outside the room). In a patient satisfaction survey, noise was the biggest difference between patients in single-bed rooms versus those in multi-bed rooms28,29; hence, noise may have been a key alternative variable that affected LOS in this study.
Conclusions
Through analysis of a large medical database, we demonstrated that patients with beds next to the window had shorter LOS than did those next to the door. We posit that this was due to the presence of natural light. This has implications for hospital design. Clinical trials that test evidence-based designs of physical environments in hospitals are difficult to perform; therefore, our alternative strategy of using accumulated electronic medical data has value.
Footnotes
Funding:The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the Ministry of Education of the Republic of Korea and the National Research Foundation of Korea (NRF-2015S1A3A2047031, NRF-2014R1A1A1007557).
Declaration of Conflicting Interests:The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Author Contributions: JSN, C-GC and H-KL contributed to the design of the research. MYP and HM performed analysis of the results. All authors wrote the manuscript.
References
- 1. Malenbaum S, Keefe FJ, Williams AC, Ulrich R, Somers TJ. Pain in its environmental context: implications for designing environments to enhance pain control. Pain. 2008;134:241–244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ulrich RS, Lundén O, Eltinge JL. Effects of exposure to nature and abstract pictures on patients recovering from heart surgery. Paper presented at: Thirty-Third Meeting of the Society for Psychophysiological Research; October 27-31, 1993; Rottach-Egern, Germany. [Google Scholar]
- 3. Ulrich RS, Zimring C, Quan X, Joseph A. The environment’s impact on stress. In: Marberry S, ed. Improving Healthcare With Better Building Design. Chicago, IL: Health Administration Press; 2006:37–61. [Google Scholar]
- 4. Ulrich RS, Zimring C, Zhu X, et al. A review of the research literature on evidence-based healthcare design. Health Environ Res Des J. 2008;1:61–125. [DOI] [PubMed] [Google Scholar]
- 5. Marberry SO. Innovations in Healthcare Design: Selected Presentations from the First Five Symposia on Healthcare Design. New York, NY: John Wiley & Sons; 1995. [Google Scholar]
- 6. Navil A, Mardaljevic J. Useful daylight illuminances: a replacement for daylight factors. Energ Buildings. 2006;38:905–913. [Google Scholar]
- 7. Lave JR, Leinhardt S. The cost and length of a hospital stay. Inquiry. 1976;13:327–343. [PubMed] [Google Scholar]
- 8. Kulinsaya E, Kornbrot D, Gao H. Length of stay as a performance indicator: robust statistical methodology. IMA J Manage Math. 2005;16:369–381. [Google Scholar]
- 9. Heggestad T. Do hospital length of stay and staffing ratio affect elderly patients’ risk of readmission? a nation-wide study of Norwegian hospitals. Health Serv Res. 2002;37:647–665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Clarke A. Why are we trying to reduce length of stay? evaluation of the costs and benefits of reducing time in hospital must start from the objectives that govern change. Qual Health Care. 1996;5:172–179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Lewy AJ Bauer VK Cutler NL et al. Morning vs.. evening light treatment of patients with winter depression. Arch Gen Psychiatry. 1998;55:890–896. [DOI] [PubMed] [Google Scholar]
- 12. Walch JM, Rabin BS, Day R, Williams JN, Choi K, Kang JD. The effect of sunlight on post-operative analgesic medication usage: a prospective study of patients undergoing spinal surgery. Psychosom Med. 2005;67:156–163. [DOI] [PubMed] [Google Scholar]
- 13. Beauchemin KM, Hays P. Sunny hospital rooms expedite recovery from severe and refractory depressions. J Affect Disord. 1996;40:49–51. [DOI] [PubMed] [Google Scholar]
- 14. Beauchemin KM, Hays P. Dying in the dark: sunshine, gender and outcomes in myocardial infarction. J R Soc Med. 1998;91:352–354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Kim HS. The Effect of Natural Light of Patient Rooms in Hospital on Recovery Time of Patients [master’s dissertation], Seoul, Korea; Department of Architectural Engineering, Hanyang University; 2005. [Google Scholar]
- 16. Bergström H, Sundström V, van Grondelle R, Åkesson E, Gillbro T. Energy transfer within the isolated light-harvesting B800–850 pigment-protein complex of Rhodobacter sphaeroides. Biochim Biophys Acta. 1986;85:279–287. [Google Scholar]
- 17. Lam RW, Buchanan A, Clark CM, Remick RA. Ultraviolet versus non-ultraviolet light therapy for seasonal affective disorder. J Clin Psychiatry. 1991;52:213–216. [PubMed] [Google Scholar]
- 18. Novaes MAFP, Aronovich A, Ferraz MB, Knobel E. Stressors in ICU: patients’ evaluation. Intensive Care Med. 1997;23:1282–1285. [DOI] [PubMed] [Google Scholar]
- 19. Topf M, Thompson S. Interactive relationships between hospital patients’ noise-induced stress and other stress with sleep. Heart Lung. 2001;30:237–243. [DOI] [PubMed] [Google Scholar]
- 20. Wallace CJ, Robins J, Alvord LS, Walker JM. The effect of earplugs on sleep measures during exposure to simulated intensive care unit noise. Am J Crit Care. 1999;8:210–219. [PubMed] [Google Scholar]
- 21. Krachman SL, D’Alonzo GE, Criner GJ. Sleep in the intensive care unit. Chest. 1995;107:1713–1720. [DOI] [PubMed] [Google Scholar]
- 22. Parthasarathy S, Tobin MJ. Sleep in the intensive care unit. Intensive Care Med. 2004;30:197–206. [DOI] [PubMed] [Google Scholar]
- 23. BaHammam A. Sleep in acute care units. Sleep Breath. 2006;10:6–15. [DOI] [PubMed] [Google Scholar]
- 24. Wakamura T, Tokura H. Influence of bright light during daytime on sleep parameters in hospitalized elderly patients. J Physiol Anthropol App Human Sci. 2001;20:345–351. [DOI] [PubMed] [Google Scholar]
- 25. Leather P, Beale D, Sullivan L. Noise, psychosocial stress and their interaction in the workplace. J Environ Psychol. 2003;23:213–222. [Google Scholar]
- 26. Goodell KH, Cao CG, Schwaitzberg SD. Effects of cognitive distraction on performance of laparoscopic surgical tasks. J Laparoendosc Adv Surg Tech A. 2006;16:94–98. [DOI] [PubMed] [Google Scholar]
- 27. Moorthy K, Munz Y, Undre S, Darzi A. Objective evaluation of the effect of noise on the performance of a complex laparoscopic task. Surgery. 2004;136:25–30. [DOI] [PubMed] [Google Scholar]
- 28. Southwell MT, Wistow G. Sleep in hospitals at night: are patients’ needs being met? J Adv Nurs. 1995;21:1101–1109. [DOI] [PubMed] [Google Scholar]
- 29. Yinnon AM, Ilan Y, Tadmor B, Altarescu G, Hershko C. Quality of sleep in the medical department. Br J Clin Pract. 1992;46:88–91. [PubMed] [Google Scholar]