Abstract
Background:
Avulsion fractures involving the tibial eminence are considered equivalent in terms of the cause to anterior cruciate ligament (ACL) tears; however, there are limited data comparing the outcomes of adolescent patients undergoing surgical fixation of a tibial eminence fracture (TEF) with those undergoing ACL reconstruction.
Purpose:
To compare the clinical outcomes, subsequent ACL injury rates, and activity levels between adolescent patients who underwent TEF fixation with patients with midsubstance ACL tears who required acute reconstruction.
Study Design:
Cohort study; Level of evidence, 3.
Methods:
This study included a group of patients with TEFs treated with surgical fixation matched to a group of similar patients with ACL tears treated with reconstruction between the years 2001 and 2015. Data regarding the initial injury, surgical intervention, ACL/ACL graft injury rates, and physical examination findings were recorded. Clinical and functional outcomes were obtained using a physical examination, the International Knee Documentation Committee (IKDC) subjective score, the Lysholm score, and the Tegner activity score.
Results:
Sixty patients with a mean follow-up of 57.7 months (range, 24-206 months) were included; 20 patients (11 male, 9 female; mean age, 11.9 years [range, 7-15 years]) who underwent surgical fixation for a TEF were matched to a group of 40 patients (23 male, 17 female; mean age, 12.5 years [range, 8-5 years]) who underwent reconstruction for ACL tears. The TEF group demonstrated significantly lower postoperative IKDC scores (TEF group, 94.0; ACL group, 97.2; P = .04) and Lysholm scores (TEF group, 92.4; ACL group, 96.9; P = .02). The TEF group returned to sport 119 days sooner (P < .01), but there was no difference in postoperative Tegner scores (TEF group, 7.3; ACL group, 7.6; P = .16). The TEF group demonstrated increased postoperative anterior laxity (P = .02) and a higher rate of postoperative arthrofibrosis (P = .04). There was no difference in subsequent ACL injuries (P = .41).
Conclusion:
Both groups demonstrated quality outcomes at a minimum 2-year follow-up. Patients with TEFs demonstrated lower mean clinical outcome scores compared with patients with ACL tears, but the differences were less than reported minimal clinically important difference values. Additionally, the TEF group experienced more postoperative anterior laxity and had a higher rate of postoperative arthrofibrosis. There was no difference in the rate of subsequent ACL injuries. The TEF group returned to sport sooner than the ACL group, but the postoperative activity levels were similar.
Keywords: tibial eminence fracture, ACL tear, ACL avulsion, pediatric ACL, ACL reconstruction
Avulsion fractures involving the tibial eminence of the knee are considered equivalent, in terms of the cause, to anterior cruciate ligament (ACL) tears.12 Although these fractures have been described in adults,20 they are more common in the pediatric population.6 Pediatric tibial eminence fractures (TEFs), as opposed to ACL ruptures, result from incomplete ossification of the tibial eminence with failure through the cancellous subchondral bone interface.50
A classification system for TEFs was first published in 1959 by Meyers and McKeever39 and was later modified by Zaricznyj.52 Type 1 represents nondisplaced fractures, which are generally treated without surgery.12,44,47 Some controversy exists regarding the proper treatment of type 2 fractures, which occur when the anterior one-third to one-half of the tibial eminence is lifted up or displaced. Most studies support nonoperative treatment for type 2 injuries with possible attempted closed reduction.6,12,14 Type 3A and 3B fractures represent completely displaced fragments, and type 3B fractures are distinguished by additional cephalad rotation of the fragment. Type 4 fractures are displaced and comminuted. Various surgical options have been described for type 3 and 4 fractures,‡ but the general consensus is that operative treatment is necessary.6,14,36 Gans et al14 conducted a systematic review and concluded that no consensus exists regarding the ideal surgical technique for the treatment of displaced TEFs. This stems from the wide array of described techniques and lack of literature directly comparing the options. A high rate of arthrofibrosis after both open and arthroscopic surgical fixation of TEFs has been widely reported in the literature.1,37,52
Comparative outcomes after various ACL reconstruction techniques have also been studied exhaustively.15,46,51 Some authors have reported postoperative complications that are unique to the pediatric population. For example, there is a known risk of injuries to the growth plate, causing possible growth arrest, with transphyseal ACL reconstruction.26,30 Additionally, the risk of subsequent ACL injuries is higher in pediatric patients compared with adults.13,23,33 In the pediatric population, TEFs and ACL tears have often been considered analogous injuries,41 but a direct comparison of their outcomes is lacking in the current literature.
The purpose of this matched-cohort study was to compare the clinical outcomes, subsequent ACL injury rates, and activity levels between pediatric patients undergoing surgical treatment of TEFs and patients requiring surgery for midsubstance ACL ruptures at a minimum 2-year follow-up. Both groups were treated surgically and were matched based on age, sex, physeal maturity, and preinjury activity level. We hypothesized that the TEF group would show an improvement in knee function after surgery, a lower rate of subsequent ACL injuries, and higher activity levels than the ACL group at a minimum 2-year follow-up.
Methods
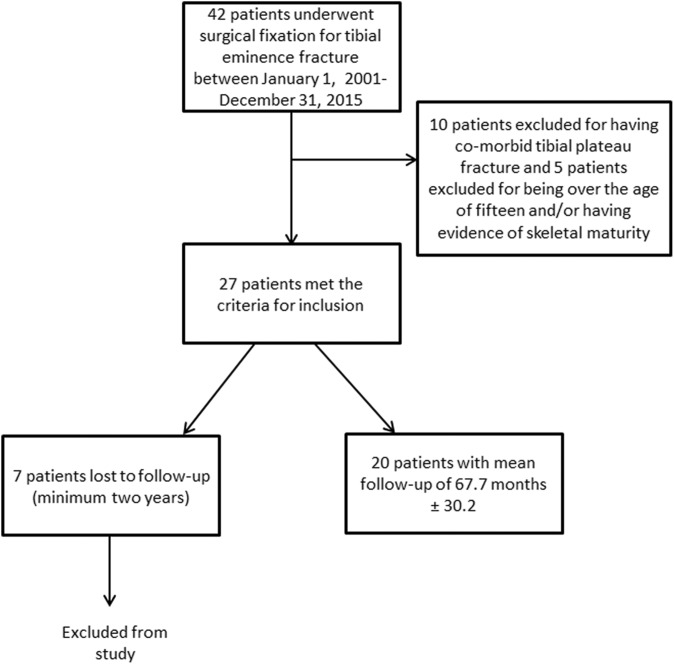
Approval from an institutional review board was granted before commencement of the study. Electronic medical records were searched for all patients who underwent surgical fixation for a TEF between January 1, 2001, and December 31, 2015. Patients were included if they (1) underwent fixation of a confirmed eminence fracture, (2) were younger than 15 years old at the time of surgery, and (3) had a minimum of 2-year follow-up. Exclusion criteria were as follows: (1) concomitant tibial plateau fracture, (2) multiligament knee injury, (3) nonoperative management of an eminence fracture, or (4) less than 2 years of follow-up (Figure 1).
Figure 1.
Patient selection methodology.
The diagnosis of a TEF (Figure 2) was confirmed by imaging. Fractures were graded based on the modified classification system of Meyers and McKeever.39,52 All data regarding the initial injury, surgical intervention, physis status, age, body mass index, sex, Tegner activity score, and physical examination findings were recorded preoperatively. All operative procedures were performed by 1 of 5 fellowship-trained orthopaedic surgeons at a single tertiary-care medical center. Concurrent injuries were recorded along with concomitant procedures, as documented in the operative report. If a subsequent procedure on the injured or contralateral knee was needed, the procedure date and time to injury were analyzed.
Figure 2.
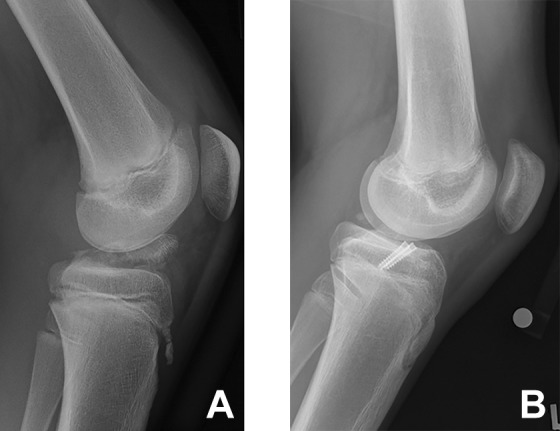
Example of a type 4 tibial eminence fracture (A) preoperatively and (B) after surgical fixation.
The primary postoperative clinical outcome measures were the International Knee Documentation Committee (IKDC)5,19 subjective score and Lysholm34 score. The postoperative ACL status was determined based on Lachman testing at final follow-up, as performed by the attending orthopaedic surgeon. Examination results were reported based on the IKDC criteria. For Lachman testing, compared with the contralateral knee, grading was as follows: 0, normal (–1 to 2 mm); 1+, nearly normal (3 to 5 mm); 2+, abnormal (6 to 10 mm); and 3+, severely abnormal (>10 mm).16 The subsequent ACL injury rate as well as knee range of motion (ROM) on physical examination were also investigated. The postoperative activity level was reported based on the Tegner activity score and return-to-sport rate. Postoperatively, TEF healing was determined by radiographic analysis.
Matched Cohort
A designated database of 120 pediatric (<16 years old) ACL reconstructions performed within our institution between January 1, 2001, and December 31, 2015, was deidentified and blinded. From this pool, patients were matched to our study group only on the basis of sex, age, physis status, and preinjury activity level. A matching ratio of 2:1 resulted in 40 patients who underwent ACL reconstruction, with a mean age of 12.5 ± 1.7 years. The 2:1 matching ratio was employed to increase the power and precision of results and to control for confounding variables when the sample size is small.17,29,38 All reconstructions were performed by 1 of 5 fellowship-trained orthopaedic surgeons at a single tertiary-care medical center.
Surgical Technique
All patients in the TEF group underwent surgical treatment for their fracture. An open technique42,50 was used in 8 patients, and in the remaining 12 patients, an arthroscopic technique35,49 was used. Suture fixation35,42 was used in 7 patients, and screw fixation was utilized in 13 patients.25,44 Gans et al14 conducted a systematic review evaluating these different surgical and fixation techniques. They ultimately concluded that no consensus on the ideal technique could be established and that all were reasonable options.
Postoperatively, patients were limited to touch weightbearing, and the knees were kept in full extension with a knee immobilizer for 3 weeks.25 After 3 weeks, ROM exercises consisting of active flexion and passive extension were begun. At 6 weeks, patients returned for nonstanding anteroposterior and lateral knee radiographs, and the hinged knee brace was removed. After this, full active knee ROM and weightbearing as tolerated were allowed. Patients typically engaged in an ACL rehabilitation and prevention program. Patients were allowed to return to sport as early as 3 months postoperatively, and by 6 months postoperatively, the majority of patients had returned to activities as tolerated based on strength and functional criteria.
Various techniques were used for ACL reconstruction in the ACL group because of the evolving standard of care over the years of this study. All 40 patients received a hamstring graft. An autograft was used in 37 patients, a hybrid allograft/autograft in 2 patients, and an allograft in 1 patient. During the early years of this study, a transtibial femoral drilling technique45 was used in 18 patients. A transportal/anatomic drilling technique45 was utilized in 19 patients. In the remaining 3 patients, an outside-in technique10,45 was used. A transphyseal technique was used in 36 patients, and a physeal-sparing technique was used in 4 patients.43
Postoperatively, patients in the ACL group were allowed to bear weight as tolerated with crutches for the first 2 weeks. Patients were allowed to discontinue crutches and a knee brace as tolerated. The patients began an ACL rehabilitation/prevention program. Patients began straight-line jogging at 3 to 4 months, and they were cleared for return to sport at 6 to 12 months postoperatively based on strength and functional criteria.
Statistical Analysis
An a priori analysis was used to determine the TEF group size needed to demonstrate postoperative outcome efficacy. Based on the IKDC validation and responsiveness data published by Irrgang et al,19 an alpha of 0.05, and power of 0.80, it was determined that 14 patients would be needed to demonstrate significant postoperative improvements. Descriptive statistics including means, standard deviations, and ranges were applied as appropriate to assess the available demographic, surgical, physical examination, and patient-reported outcome data. Statistical hypothesis testing was performed using the Fisher exact test and Wilcoxon rank-sum test. Analysis was performed with 95% CIs, and P values <.05 were considered statistically significant. All statistical analyses were performed using JMP software (version 12.0.1; SAS Institute) and G*Power 3.1.9.2 (G*Power Team).
Results
The final patient cohort consisted of 60 patients. The TEF group consisted of 20 patients who had undergone surgical fixation of a TEF, and the matched group consisted of 40 patients who had undergone ACL reconstruction. All patients had a minimum 2-year follow-up. The mean time to final follow-up in the TEF group was 67.7 ± 30.2 months compared with 52.7 ± 49.3 months in the ACL group. Demographics were similar between the 2 groups, but the TEF group underwent surgery much sooner after an injury compared with the ACL group (Table 1). The ACL group had a higher rate of comorbid injuries (Table 2). Additionally, the ACL group had a higher rate of concomitant procedures, which consisted of meniscal repair in the majority of cases (Table 3).
TABLE 1.
Patient Demographicsa
| TEF Group (n = 20) | ACL Group (n = 40) | P Value | |
|---|---|---|---|
| Age, y | 11.9 ± 3.0 | 12.5 ± 1.7 | .19 |
| Male sex, n (%) | 11 (55) | 23 (58) | .99 |
| Right laterality, n (%) | 6 (30) | 23 (58) | — |
| Skeletal immaturity, % | 100 | 100 | .99 |
| Preinjury Tegner activity score | 8.1 ± 0.9 | 8.0 ± 0.6 | .43 |
| Time from injury to surgery, d | 8.9 ± 6.7 | 76.8 ± 41.8 | <.01b |
| Modified Meyers and McKeever grade | 2.5 ± 0.6 | — | — |
| Latest follow-up, mo | 67.7 ± 30.2 | 52.7 ± 49.3 | <.01b |
aData are shown as mean ± SD unless otherwise indicated. ACL, anterior cruciate ligament; TEF, tibial eminence fracture.
bStatistically significant between-group difference (P < .05).
TABLE 2.
Comorbid Injuriesa
| TEF Group (n = 20) | ACL Group (n = 40) | P Value | |
|---|---|---|---|
| None | 17 (85) | 19 (48) | <.01c |
| Medial meniscal injury | 0 (0) | 10 (25) | .02c |
| Lateral meniscal injury | 1 (5) | 12 (30) | .04c |
| MCL injury | 3 (15) | 0 (0) | .03c |
| Otherb | 0 (0) | 1 (3) | .99 |
aData are shown as n (%). One patient in the TEF group had both an MCL sprain and a lateral meniscal injury. Two patients in the ACL group had both medial and lateral meniscal injuries. ACL, anterior cruciate ligament; MCL, medial collateral ligament; TEF, tibial eminence fracture.
bOne patient in the ACL group had a contusion of the lateral femoral condyle that was managed with microfracture 4 years after ACL reconstruction; this patient did not fail and had excellent patient-reported outcomes at final follow-up.
cStatistically significant between-group difference (P < .05).
TABLE 3.
Concomitant Surgery With Index ACL Reconstructiona
| TEF Group (n = 20) | ACL Group (n = 40) | P Value | |
|---|---|---|---|
| None | 19 (95) | 22 (55) | <.01b |
| Partial lateral meniscectomy | 1 (5) | 3 (7.5) | .99 |
| Medial meniscal repair | 0 (0) | 8 (20) | .04b |
| Lateral meniscal repair | 0 (0) | 9 (22.5) | .02b |
aData are shown as n (%). Two patients in the ACL group underwent both medial and lateral meniscal repair. ACL, anterior cruciate ligament; TEF, tibial eminence fracture.
bStatistically significant between-group difference (P < .05).
Clinical Outcomes
The mean postoperative patient-reported outcomes including the IKDC and Lysholm scores were significantly lower in the TEF group (Table 4).
TABLE 4.
Patient-Reported Outcomesa
| TEF Group | ACL Group | ||
|---|---|---|---|
| (n = 20) | (n = 40) | P Value | |
| Tegner activity score | 7.3 ± 1.3 | 7.6 ± 1.4 | .16 |
| Lysholm score | 92.4 ± 9.3 | 96.9 ± 7.1 | .02b |
| IKDC score | 94.0 ± 8.8 | 97.2 ± 7.5 | .04b |
aData are shown as mean ± SD. ACL, anterior cruciate ligament; IKDC, International Knee Documentation Committee; TEF, tibial eminence fracture.
bStatistically significant between-group difference (P < .05).
Physical Examination Findings
Failures were excluded from the analysis of postoperative physical examination results. The TEF group had significantly greater anterior laxity at postoperative follow-up. Lachman testing results are shown in Table 5.
TABLE 5.
Postoperative Lachman Testing Resultsa
| Grade | TEF Group (n = 19) | ACL Group (n = 34) | P Value |
|---|---|---|---|
| 0 | 14 (74) | 33 (97) | .02b |
| 1+ | 4 (21) | 1 (3) | |
| 2+ | 1 (5) | 0 (0) |
aData are shown as n (%). Failures were excluded. ACL, anterior cruciate ligament; TEF, tibial eminence fracture.
bStatistically significant between-group difference (P < .05).
In the TEF group, the mean preoperative ROM was 11.7° ± 4.0° of extension to 65.8° ± 34.1° of flexion; postoperatively it was 2.1° ± 2.7° of extension to 129.4° ± 15.8° of flexion. The ROM arc significantly increased after surgery (from 54.1° to 127.3°; P < .01).
In the ACL group, the mean preoperative ROM was –1.0° ± 9.3° of hyperextension to 119.2° ± 24.6° of flexion; postoperatively it was –0.5° ± 5.9° of hyperextension to 134.2° ± 14.6° of flexion. The ROM arc significantly increased after surgery (from 120.2° to 134.6°; P = .01). The final ROM arc was not significantly different between groups.
Subsequent ACL Injuries
In the TEF group, 1 patient (5%) sustained an ACL rupture 41 weeks after TEF fixation during a sport-related injury and required ACL reconstruction; his graft reruptured 2 years later, and he required revision ACL reconstruction.
In the ACL group, 6 patients (15%) sustained an ACL rerupture at a mean of 43.4 ± 41.2 months, 5 of which occurred during sport-related activities and 1 with activities of daily living. All required revision ACL reconstruction and remained free of further reruptures at latest available follow-up. The failure rate did not significantly differ between the TEF and ACL groups (P = .41).
Tegner Activity Score
No significant difference between groups was seen in the postoperative activity level, according to the Tegner activity score at follow-up (Table 4). The mean Tegner activity score decreased in both the TEF group (from 8.1 to 7.3; P = .05) and ACL group (from 8.0 to 7.6; P = .40) when compared with preinjury levels; however, these findings were not statistically significant.
Return to Sport
The mean time to return to sport was 161 ± 87.6 days in the TEF group versus 280 ± 91.1 days in the ACL group (P < .01). Two patients in each group never returned to sport.
TEF Healing
Radiographic evidence of healing was seen in all 20 patients in the TEF group at a mean of 70 days after surgery.
Complications
The arthrofibrosis rate was higher in the TEF group (P = .04). Surgical complications in the TEF group included 4 cases of arthrofibrosis (20%), for which 3 patients required arthroscopic intervention; 1 case of hemarthrosis (5%) requiring aspiration; and 1 case of superficial wound dehiscence managed nonoperatively. For the cases of arthrofibrosis, 2 of the index surgeries were performed with open arthrotomy, with 1 being fixed with sutures and the other with screws. The additional 2 cases were treated with arthroscopic screw fixation.
In the ACL group, there were 2 cases of hemarthrosis (5%) requiring arthrocentesis, 2 cases requiring tibial screw and washer removal (5%), 1 case of arthrofibrosis (2.5%) requiring arthroscopic intervention, and 1 case of a growth plate injury requiring epiphysiodesis for a leg-length discrepancy more than 5 years after the index ACL reconstruction.
Discussion
The mechanisms of injury for TEFs and ACL tears are similar, but the results of surgical treatment have not been directly compared. In the present study, the TEF group demonstrated decreased clinical outcome scores and an increased rate of postoperative arthrofibrosis and anterior laxity compared with the ACL group. There was no difference in the rate of subsequent ACL injuries or postoperative activity level between groups, although the TEF group returned to sport sooner.
Both groups demonstrated very good outcome scores at a minimum 2-year follow-up, but the TEF group had lower IKDC and Lysholm scores compared with the ACL group. The mean IKDC score of 97.2 and mean Lysholm score of 96.9 in the ACL group are comparable with those published in previous studies with a similar follow-up time.48 The mean Lysholm and IKDC scores in the TEF group are also comparable with the scores in previously published cohorts.14 This supports the validity of the mean clinical outcome scores of both groups in the present study.
The difference in IKDC and Lysholm scores between groups was statistically significant. This suggests that patients with TEFs may have lower functionality compared with patients with ACL tears; however, the differences were less than the established minimal clinically important difference (MCID) (Lysholm, 10.1; IKDC, 11.5).9,19 It should be noted that these MCID values were based on a group of patients with a mean age of 40.5 years and may not directly apply to the young patients in the present study.18 There is a need to establish MCID values specific to the adolescent population.
The TEF group demonstrated increased anterior laxity compared with the ACL group on Lachman testing at midterm follow-up. Persistent anterior laxity after a TEF is consistent with previously published studies.7,14,25,44 In the present study, 26% of patients in the TEF group demonstrated grade ≥1+ on Lachman testing at follow-up. The relevance of this finding is unknown. It has been hypothesized that the increased laxity is the result of a mild injury to the ACL at the time of an eminence fracture.1,3,25,50 This relatively high rate of persistent anterior laxity has caused some to question whether it would lead to future ligament, chondral, or meniscal injuries.25 This has not yet been demonstrated in the current literature, and it did not appear to be a factor in the current study.
The increased anterior laxity did not correlate with an increase in the rate of subsequent ACL injuries when compared with the ACL group. In the TEF group, 1 patient (5%) sustained a subsequent ACL rupture 41 weeks after TEF fixation. Aderinto et al1 reported a 10% rate of symptomatic anterior laxity after TEF fixation. It is unclear how many patients went on to require revision or ACL reconstruction. Aderinto et al1 did report that the risk of symptomatic anterior laxity is much more common when these fractures are treated nonoperatively. In the ACL group of the current study, 6 (15%) patients sustained a rerupture at a mean of 43.4 months postoperatively. The rate of reruptures in the ACL group is slightly higher than in some previously reported studies.22,28 This is likely related to the relatively young mean age of the ACL group in this study.2,4
Both groups demonstrated a decrease in the Tegner score at midterm follow-up. This finding is likely more related to the high level of competitive athletic involvement in the younger population, which commonly decreases with age.27 The Tegner scores in the present study are very comparable with those in other published studies for both the TEF25 and the ACL48 groups. The TEF group returned to sport sooner than the ACL group, but no difference was seen in the rate of return to sport, as the majority returned in both groups. Patients tend to be cleared earlier for return to sport after TEF treatment compared with those after ACL reconstruction because fracture healing occurs faster than ligamentization of the ACL graft.11
There were no major intraoperative complications in either group. The TEF group had a higher rate of postoperative arthrofibrosis than the ACL group (20% vs 2.5%, respectively). Other studies have reported similar rates of arthrofibrosis after fracture fixation and report it as the most common postoperative complication.1 Rehabilitation protocols did differ between the 2 groups, and notably, patients in the TEF group required 3 weeks of knee immobilization in full extension to protect the fracture fixation site. This prolonged period of immobilization may have contributed to the increased rate of arthrofibrosis in the TEF group. It is also possible that the shorter time from injury to surgery in the TEF group may have contributed to the higher arthrofibrosis rate. In the ACL group, 1 patient developed a leg-length discrepancy and required epiphysiodesis. The growth plate does seem to be at an increased risk of injuries with ACL reconstruction compared with TEF fixation, depending on the method of ACL socket and tunnel drilling.
Given the constellation of these findings, one could certainly question whether the ACL should be reconstructed at the time of the TEF rather than fixed. This is not our current practice, as there is likely some benefit to preserving the native anatomy and proprioceptive fibers of the native ACL. More research is certainly needed on this topic.
There are several limitations to this work that merit discussion, as the inherent drawbacks of any retrospective study are well established. Unfortunately, the cohort was too small to perform subgroup analysis of the different TEF fixation techniques and approaches. Examiners were not blinded, and the pivot-shift test was not consistently performed. Additionally, functional testing was not compared between groups. Although injuries with major prognostic implications such as multiligament injuries were excluded, we were unable to match the groups based on any additional concomitant injuries. There were more meniscal tears in the ACL group and more medial collateral ligament injuries in the TEF group. However, we do not feel that this greatly affected the results of the study, as the majority of the meniscal tears were repaired and the medial collateral ligament injuries did not require operative intervention. This allowed the native anatomy to be preserved in both groups. It is possible that the increased rate of meniscal tears may have major implications regarding the long-term prognosis of the knees in the ACL group. The TEF group had a greater mean follow-up time, but all patients in both groups achieved a minimum 2-year follow-up. No instrumented measuring device was used for the physical examination, which limited interexaminer reliability. Despite these limitations, to our knowledge, this is the first study directly comparing the outcomes of patients with TEFs with patients with ACL tears after surgical treatment.
Conclusion
Both study groups demonstrated good outcomes at a minimum 2-year follow-up. Patients with TEFs demonstrated lower mean clinical outcome scores compared with patients with ACL tears, but the differences were less than reported MCID values. Additionally, the TEF group experienced more postoperative anterior laxity and had a higher rate of postoperative arthrofibrosis. There was no difference in the rate of subsequent ACL injuries. The TEF group returned to sport sooner than the ACL group, but the postoperative activity levels were similar. These results can be useful for clinical decision making and discussion with patients and their families who are affected by these injuries.
Footnotes
One or more of the authors has declared the following potential conflicts of interest or source of funding: T.A.M. is a consultant for OrthoPediatrics, has stock/stock options in Viking Scientific, has received honoraria from BroadWater, and has received educational support from Arthrex. D.L.D. receives research support from Arthrex and has stock/stock options in Tenex Health and Sonex Health, and her spouse has stock/stock options in Tenex Health and Sonex Health. B.A.L. receives royalties from Arthrex; is a consultant for Arthrex and Smith & Nephew; and receives research support from Arthrex, Biomet, Smith & Nephew, and Stryker. M.J.S. receives royalties from Arthrex, is a consultant for Arthrex, and receives research support from Stryker. A.J.K. receives research support from Aesculap/B. Braun, the Arthritis Foundation, Ceterix, and Histogenics; receives royalties from Arthrex; and is a consultant for Arthrex, Vericel, and DePuy. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the Mayo Clinic (No. 15-000601).
References
- 1. Aderinto J, Walmsley P, Keating JF. Fractures of the tibial spine: epidemiology and outcome. Knee. 2008;15(3):164–167. [DOI] [PubMed] [Google Scholar]
- 2. Ahlden M, Samuelsson K, Sernert N, Forssblad M, Karlsson J, Kartus J. The Swedish National Anterior Cruciate Ligament Register: a report on baseline variables and outcomes of surgery for almost 18,000 patients. Am J Sports Med. 2012;40(10):2230–2235. [DOI] [PubMed] [Google Scholar]
- 3. Ahmad CS, Stein BE, Jeshuran W, Nercessian OA, Henry JH. Anterior cruciate ligament function after tibial eminence fracture in skeletally mature patients. Am J Sports Med. 2001;29(3):339–345. [DOI] [PubMed] [Google Scholar]
- 4. Allen MM, Pareek A, Krych AJ, et al. Are female soccer players at an increased risk of second anterior cruciate ligament injury compared with their athletic peers? Am J Sports Med. 2016;44(10):2492–2498. [DOI] [PubMed] [Google Scholar]
- 5. Anderson AF, Irrgang JJ, Kocher MS, Mann BJ, Harrast JJ; International Knee Documentation Committee. The International Knee Documentation Committee subjective knee evaluation form: normative data. Am J Sports Med. 2006;34(1):128–135. [DOI] [PubMed] [Google Scholar]
- 6. Anderson CN, Anderson AF. Tibial eminence fractures. Clin Sports Med. 2011;30(4):727–742. [DOI] [PubMed] [Google Scholar]
- 7. Baxter MP, Wiley JJ. Fractures of the tibial spine in children: an evaluation of knee stability. J Bone Joint Surg Br. 1988;70(2):228–230. [DOI] [PubMed] [Google Scholar]
- 8. Bley JA, Pomajzl RJ, Smith PA. Knotless arthroscopic reduction and internal fixation of a displaced anterior cruciate ligament tibial eminence avulsion fracture. Am J Orthop (Belle Mead NJ). 2017;46(4):203–208. [PubMed] [Google Scholar]
- 9. Briggs KK, Lysholm J, Tegner Y, Rodkey WG, Kocher MS, Steadman JR. The reliability, validity, and responsiveness of the Lysholm score and Tegner activity scale for anterior cruciate ligament injuries of the knee: 25 years later. Am J Sports Med. 2009;37(5):890–897. [DOI] [PubMed] [Google Scholar]
- 10. Burnham JM, Malempati CS, Carpiaux A, Ireland ML, Johnson DL. Anatomic femoral and tibial tunnel placement during anterior cruciate ligament reconstruction: anteromedial portal all-inside and outside-in techniques. Arthrosc Tech. 2017;6(2):e275–e282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Claes S, Verdonk P, Forsyth R, Bellemans J. The “ligamentization” process in anterior cruciate ligament reconstruction: what happens to the human graft? A systematic review of the literature. Am J Sports Med. 2011;39(11):2476–2483. [DOI] [PubMed] [Google Scholar]
- 12. Coyle C, Jagernauth S, Ramachandran M. Tibial eminence fractures in the paediatric population: a systematic review. J Child Orthop. 2014;8(2):149–159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Fauno P, Rahr-Wagner L, Lind M. Risk for revision after anterior cruciate ligament reconstruction is higher among adolescents: results from the Danish Registry of Knee Ligament Reconstruction. Orthop J Sports Med. 2014;2(10):2325967114552405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Gans I, Baldwin KD, Ganley TJ. Treatment and management outcomes of tibial eminence fractures in pediatric patients: a systematic review. Am J Sports Med. 2014;42(7):1743–1750. [DOI] [PubMed] [Google Scholar]
- 15. Gifstad T, Sole A, Strand T, Uppheim G, Grontvedt T, Drogset JO. Long-term follow-up of patellar tendon grafts or hamstring tendon grafts in endoscopic ACL reconstructions. Knee Surg Sports Traumatol Arthrosc. 2013;21(3):576–583. [DOI] [PubMed] [Google Scholar]
- 16. Hefti F, Muller W, Jakob RP, Staubli HU. Evaluation of knee ligament injuries with the IKDC form. Knee Surg Sports Traumatol Arthrosc. 1993;1(3-4):226–234. [DOI] [PubMed] [Google Scholar]
- 17. Hennessy S, Bilker WB, Berlin JA, Strom BL. Factors influencing the optimal control-to-case ratio in matched case-control studies. Am J Epidemiol. 1999;149(2):195–197. [DOI] [PubMed] [Google Scholar]
- 18. Irrgang JJ, Anderson AF, Boland AL, et al. Development and validation of the International Knee Documentation Committee subjective knee form. Am J Sports Med. 2001;29(5):600–613. [DOI] [PubMed] [Google Scholar]
- 19. Irrgang JJ, Anderson AF, Boland AL, et al. Responsiveness of the International Knee Documentation Committee subjective knee form. Am J Sports Med. 2006;34(10):1567–1573. [DOI] [PubMed] [Google Scholar]
- 20. Ishibashi Y, Tsuda E, Sasaki T, Toh S. Magnetic resonance imaging AIDS in detecting concomitant injuries in patients with tibial spine fractures. Clin Orthop Relat Res. 2005;(434):207–212. [DOI] [PubMed] [Google Scholar]
- 21. Janarv PM, Westblad P, Johansson C, Hirsch G. Long-term follow-up of anterior tibial spine fractures in children. J Pediatr Orthop. 1995;15(1):63–68. [DOI] [PubMed] [Google Scholar]
- 22. Kaeding CC, Aros B, Pedroza A, et al. Allograft versus autograft anterior cruciate ligament reconstruction: predictors of failure from a MOON prospective longitudinal cohort. Sports Health. 2011;3(1):73–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Kaeding CC, Pedroza AD, Reinke EK, Huston LJ; MOON Consortium, Spindler KP. Risk factors and predictors of subsequent ACL injury in either knee after ACL reconstruction: prospective analysis of 2488 primary ACL reconstructions from the MOON cohort. Am J Sports Med. 2015;43(7):1583–1590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Kendall NS, Hsu SY, Chan KM. Fracture of the tibial spine in adults and children: a review of 31 cases. J Bone Joint Surg Br. 1992;74(6):848–852. [DOI] [PubMed] [Google Scholar]
- 25. Kocher MS, Foreman ES, Micheli LJ. Laxity and functional outcome after arthroscopic reduction and internal fixation of displaced tibial spine fractures in children. Arthroscopy. 2003;19(10):1085–1090. [DOI] [PubMed] [Google Scholar]
- 26. Koman JD, Sanders JO. Valgus deformity after reconstruction of the anterior cruciate ligament in a skeletally immature patient: a case report. J Bone Joint Surg Am. 1999;81(5):711–715. [DOI] [PubMed] [Google Scholar]
- 27. Kostogiannis I, Ageberg E, Neuman P, Dahlberg L, Friden T, Roos H. Activity level and subjective knee function 15 years after anterior cruciate ligament injury: a prospective, longitudinal study of nonreconstructed patients. Am J Sports Med. 2007;35(7):1135–1143. [DOI] [PubMed] [Google Scholar]
- 28. Krych AJ, Jackson JD, Hoskin TL, Dahm DL. A meta-analysis of patellar tendon autograft versus patellar tendon allograft in anterior cruciate ligament reconstruction. Arthroscopy. 2008;24(3):292–298. [DOI] [PubMed] [Google Scholar]
- 29. Krych AJ, King AH, Berardelli RL, Sousa PL, Levy BA. Is subchondral acetabular edema or cystic change on MRI a contraindication for hip arthroscopy in patients with FAI? Response. Am J Sports Med. 2016;44(4):NP20–NP21. [DOI] [PubMed] [Google Scholar]
- 30. Liddle AD, Imbuldeniya AM, Hunt DM. Transphyseal reconstruction of the anterior cruciate ligament in prepubescent children. J Bone Joint Surg Br. 2008;90(10):1317–1322. [DOI] [PubMed] [Google Scholar]
- 31. Liljeros K, Werner S, Janarv PM. Arthroscopic fixation of anterior tibial spine fractures with bioabsorbable nails in skeletally immature patients. Am J Sports Med. 2009;37(5):923–928. [DOI] [PubMed] [Google Scholar]
- 32. Lu XW, Hu XP, Jin C, Zhu T, Ding Y, Dai LY. Reduction and fixation of the avulsion fracture of the tibial eminence using mini-open technique. Knee Surg Sports Traumatol Arthrosc. 2010;18(11):1476–1480. [DOI] [PubMed] [Google Scholar]
- 33. Lynch TS, Parker RD, Patel RM, et al. The impact of the Multicenter Orthopaedic Outcomes Network (MOON) research on anterior cruciate ligament reconstruction and orthopaedic practice. J Am Acad Orthop Surg. 2015;23(3):154–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Lysholm J, Gillquist J. Evaluation of knee ligament surgery results with special emphasis on use of a scoring scale. Am J Sports Med. 1982;10(3):150–154. [DOI] [PubMed] [Google Scholar]
- 35. Mah JY, Adili A, Otsuka NY, Ogilvie R. Follow-up study of arthroscopic reduction and fixation of type III tibial-eminence fractures. J Pediatr Orthop. 1998;18(4):475–477. [PubMed] [Google Scholar]
- 36. May JH, Levy BA, Guse D, Shah J, Stuart MJ, Dahm DL. ACL tibial spine avulsion: mid-term outcomes and rehabilitation. Orthopedics. 2011;34(2):89. [DOI] [PubMed] [Google Scholar]
- 37. McLennan JG. The role of arthroscopic surgery in the treatment of fractures of the intercondylar eminence of the tibia. J Bone Joint Surg Br. 1982;64(4):477–480. [DOI] [PubMed] [Google Scholar]
- 38. Melugin HP, Johnson NR, Wu IT, Levy BA, Stuart MJ, Krych AJ. Is treatment of Segond fracture necessary with combined anterior cruciate ligament reconstruction? Am J Sports Med. 2018;46(4):832–838. [DOI] [PubMed] [Google Scholar]
- 39. Meyers MH, McKeever FM. Fracture of the intercondylar eminence of the tibia. J Bone Joint Surg Am. 1959;41(2):209–220. [PubMed] [Google Scholar]
- 40. Meyers MH, McKeever FM. Fracture of the intercondylar eminence of the tibia. J Bone Joint Surg Am. 1970;52(8):1677–1684. [PubMed] [Google Scholar]
- 41. Najdi H, Thevenin-Lemoine C, Sales de Gauzy J, Accadbled F. Arthroscopic treatment of intercondylar eminence fractures with intraepiphyseal screws in children and adolescents. Orthop Traumatol Surg Res. 2016;102(4):447–451. [DOI] [PubMed] [Google Scholar]
- 42. Owens BD, Crane GK, Plante T, Busconi BD. Treatment of type III tibial intercondylar eminence fractures in skeletally immature athletes. Am J Orthop (Belle Mead NJ). 2003;32(2):103–105. [PubMed] [Google Scholar]
- 43. Pierce TP, Issa K, Festa A, Scillia AJ, McInerney VK. Pediatric anterior cruciate ligament reconstruction: a systematic review of transphyseal versus physeal-sparing techniques. Am J Sports Med. 2017;45(2):488–494. [DOI] [PubMed] [Google Scholar]
- 44. Reynders P, Reynders K, Broos P. Pediatric and adolescent tibial eminence fractures: arthroscopic cannulated screw fixation. J Trauma. 2002;53(1):49–54. [DOI] [PubMed] [Google Scholar]
- 45. Robin BN, Jani SS, Marvil SC, Reid JB, Schillhammer CK, Lubowitz JH. Advantages and disadvantages of transtibial, anteromedial portal, and outside-in femoral tunnel drilling in single-bundle anterior cruciate ligament reconstruction: a systematic review. Arthroscopy. 2015;31(7):1412–1417. [DOI] [PubMed] [Google Scholar]
- 46. Samuelsen BT, Webster KE, Johnson NR, Hewett TE, Krych AJ. Hamstring autograft versus patellar tendon autograft for ACL reconstruction: is there a difference in graft failure rate? A meta-analysis of 47,613 patients. Clin Orthop Relat Res. 2017;475(10):2459–2468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Shepley RW. Arthroscopic treatment of type III tibial spine fractures using absorbable fixation. Orthopedics. 2004;27(7):767–769. [DOI] [PubMed] [Google Scholar]
- 48. Sousa PL, Krych AJ, Cates RA, Levy BA, Stuart MJ, Dahm DL. Return to sport: does excellent 6-month strength and function following ACL reconstruction predict midterm outcomes? Knee Surg Sports Traumatol Arthrosc. 2017;25(5):1356–1363. [DOI] [PubMed] [Google Scholar]
- 49. Wiegand N, Naumov I, Vamhidy L, Not LG. Arthroscopic treatment of tibial spine fracture in children with a cannulated Herbert screw. Knee. 2014;21(2):481–485. [DOI] [PubMed] [Google Scholar]
- 50. Wiley JJ, Baxter MP. Tibial spine fractures in children. Clin Orthop Relat Res. 1990;(255):54–60. [PubMed] [Google Scholar]
- 51. Xie X, Liu X, Chen Z, Yu Y, Peng S, Li Q. A meta-analysis of bone-patellar tendon-bone autograft versus four-strand hamstring tendon autograft for anterior cruciate ligament reconstruction. Knee. 2015;22(2):100–110. [DOI] [PubMed] [Google Scholar]
- 52. Zaricznyj B. Avulsion fracture of the tibial eminence: treatment by open reduction and pinning. J Bone Joint Surg Am. 1977;59(8):1111–1114. [PubMed] [Google Scholar]