Abstract
Background
To evaluate the prevalence, risk factors and treatment of retinopathy of prematurity (ROP) in Turkey and to establish screening criteria for this condition.
Methods
A prospective cohort study (TR-ROP) was performed between 1 April 2016 and 30 April 2017 in 69 neonatal intensive care units (NICUs). Infants with a birth weight (BW)≤1500 g or gestational age (GA)≤32 weeks and those with a BW>1500 g or GA>32 weeks with an unstable clinical course were included in the study. Predictors for the development of ROP were determined by logistic regression analyses.
Results
The TR-ROP study included 6115 infants: 4964 (81%) with a GA≤32 weeks and 1151 (19%) with a GA>32 weeks. Overall, 27% had any stage of ROP and 6.7% had severe ROP. A lower BW, smaller GA, total days on oxygen, late-onset sepsis, frequency of red blood cell transfusions and relative weight gain were identified as independent risk factors for severe ROP in infants with a BW≤1500 g. Of all infants, 414 needed treatment and 395 (95.4%) of the treated infants had a BW≤1500 g. Sixty-six (16%) of the treated infants did not fulfil the Early Treatment for Retinopathy of Prematurity requirements for treatment.
Conclusions
Screening of infants with a GA≤34 weeks or a BW<1700 g appears to be appropriate in Turkey. Monitoring standards of neonatal care and conducting quality improvement projects across the country are recommended to improve neonatal outcomes in Turkish NICUs.
Trial registration number
NCT02814929, Results.
Keywords: Retina, Child Health (paediatrics), Treatment Medical, Neovascularisation
Introduction
Retinopathy of prematurity (ROP), a vasoproliferative disorder of the immature retina in premature infants, is a significant cause of blindness in many middle-income countries. The prevalence of ROP is lower in high-income countries, where risk factors such as oxygen administration and blood oxygen saturation are strictly monitored.1 Severe ROP is typically found in infants with a very low gestational age (GA) at birth in developed countries.1 2 Heavier and more mature babies can also develop ROP in developing countries, because there is insufficient awareness of the risk factors of the disease process, a shortage of skilled professionals and/or a shortage of essential equipment to care for infants.3
In recent years, Turkey has been developing programmes to improve neonatal health. This study (TR-ROP) determined the prevalence and treatment modalities of infants with ROP in Turkey and was the first multicentre study to analyse risk factors for ROP development in the country. Based on data obtained from infants, criteria for ROP screening in Turkey were evaluated. Because Turkey has received many refugees in recent years, this study also evaluated the prevalence of ROP in preterm infants born to refugees.
Methods
The TR-ROP study was promoted by the Turkish Neonatology Society and included preterm infants screened for ROP between 1 April 2016 and 30 April 2017. In Turkey, the total number of neonatal intensive care units (NICUs) including neonatologists on the medical staff is 134 (22 private, 40 university and 72 state hospitals). In total, 69 NICUs (8 private, 39 university and 22 state hospitals) agreed to take part in the study (51% of all). Heads of the NICUs and directors of hospitals gave written consent to participate in the research. It was approved by the ethics committee and informed consent was obtained from the parents before the initial screening.
Study population
This prospective cohort study evaluated the incidence and severity of ROP in relation to GA, birth weight (BW) and treatment modalities. The independent risk factors for the development of severe ROP in infants with a BW≤1500 g and for any ROP in infants with a BW>1500 g were assessed.
Infants with a BW≤1500 g or GA≤32 weeks and those with a BW>1500 g or GA>32 weeks, who were determined by the attending clinician to be at risk for ROP development, were screened. Then the medical records of retinal examinations of preterm infants who met the screening criteria were evaluated. The data on refugee infants were also recorded. Examinations took place in the NICU or outpatient facility (for discharged infants). Eligible infants who were discharged before the first screening and missed or did not complete all screening sessions were excluded from the study. The data are restricted to all babies who underwent all the screening sessions. Infants with congenital anomalies, chromosomal abnormalities and those who died before the first ophthalmic examination were excluded from the study.
Dataset
Neonatologists who agreed to participate in this study provided data regarding ROP in their NICUs. A case report form (CRF) for each enrolled patient was completed by the participating neonatologist. Data were collected through an online data entry system via a special network named the ‘Trials-Network’. All the questions in the CRF were required to be answered. The data entry system did not allow the collaborator to proceed and submit the data if no response was received for any question in the CRF. Anonymous data were entered into password protected database to maintain confidentiality. The records from 69 NICUs were pooled together and analysed at the end of the study.
Clinical characteristics
Antenatal, natal and postnatal risk factors for the development of ROP including maternal age, use of antenatal corticosteroids, preeclampsia/eclampsia, infants of diabetic mothers, chorioamnionitis (clinical or histopathological), in vitro fertilisation, multiple births, mode of delivery, sex, GA, BW, small for gestational age (SGA; 10th percentile),4 resuscitation in the delivery room, respiratory distress syndrome (RDS), surfactant treatment, duration of invasive/noninvasive mechanical ventilation and oxygen therapy, intracranial haemorrhage >Grade II according to Papile staging,5 haemodynamically significant patent ductus arteriosus (PDA), early/late neonatal sepsis (clinically proven or culture positive), necrotising enterocolitis (NEC)≥Stage II in accordance with the modified Bell criteria,6 the number of red blood cell (RBC) transfusions (15 mL/kg for each transfusion), bronchopulmonary dysplasia (BPD), oxygen requirement at 36 weeks postmenstrual age, relative weight gain and breastfeeding were recorded on the CRF for each patient.
Ophthalmic examinations
The International Classification of ROP guidelines were used to record the stage of the disorder, location by zone and signs of plus disease.7 All infants meeting the screening criteria were scheduled to have their first examination at between 4 and 6 weeks of life. Ophthalmic examinations were continued until full retinal vascularisation and the maximum stage of ROP for each infant was reported. The data were analysed for the most advanced stage of ROP in the eye with the most severe disease.
Severe ROP was defined as ROP needing treatment. Criteria for treatment of ROP were based on the Early Treatment for Retinopathy of Prematurity (ETROP);8 however, not all treated patients met this criteria and were defined as the ‘unclassified’ group. The study also investigated the need for laser photocoagulation, intravitreal bevacizumab (IVB) and vitreoretinal surgery for ROP.
The NICUs having no treatment options transferred the infants to other facilities where ROP treatment is available. The referring neonatologists completed the CRF forms for these patients after being in contact with the receiving facilities.
Statistical analyses
Statistical analyses were conducted using SPSS statistical software for Windows, V.21.0 (SPSS, Chicago, Illinois, USA). The results are presented as numbers (n), frequencies (%), means with the respective SDs and medians with their IQRs. Parametric tests were used to analyse variables. The χ2 test was used to compare categorical variables. A two-tailed value of p≤0.05 was considered statistically significant. Multiple logistic regression analyses were used to evaluate risk factors for any degree of ROP (BW>1500 g) and severe ROP in infants (BW≤1500 g), using the selection of factors associated (p≤0.05) with ROP determined by univariate analyses. In the model, no ROP versus severe ROP (BW≤1500 g) and no ROP versus any degree of ROP (BW>1500 g) were compared. Variables with a p≤0.05 using logistic regression analyses were accepted as independent risk factors. The OR and 95% CI for each risk factor were determined. The one-way analysis of variance was performed to determine the statistical significance for GA and BW among NICUs in university, state and private hospitals.
Results
During the study period, data from 69 centres including NICUs of 39 university hospitals (2823 infants), 22 state hospitals (2605 infants) and 8 private hospitals (687 infants) were obtained. All of the participating centres had ophthalmology units for ROP screening, but only 41/69 performed laser photocoagulation and/or antivascular endothelial growth factor (anti-VEGF) treatments and 5/69 centres performed vitreoretinal surgery.
The TR-ROP study included 6115 preterm infants: 4964 (81%) with a GA≤32 weeks and 1151 (19%) with a GA>32 weeks. The mean BW and GA for the total cohort were 1,457±479 g and 28.9±6.3 weeks, respectively. There were 3163 (51.7%) females and 2952 (48.3%) males in the study group. The mean postnatal day and postmenstrual age at the initial diagnosis of ROP were 49.2±16 days and 33.8±2.9 weeks, respectively. Overall, 27% of the patients were found to have any stage of ROP and 6.7% had severe ROP. The incidences of ROP and severe ROP in relation to GA and BW are shown in table 1. The majority (96%) of infants with any stage of ROP had a GA≤32 weeks and 80% of the infants with severe ROP had a GA≤28 weeks.
Table 1.
ROP in relation to gestational age and birth weight
| Gestational age (weeks) | Screened infants (n) | Any ROP (n, %) | Severe ROP (n, %) |
| ≤28 | 1539 | 968 (62.9) | 332 (21.6) |
| 29–32 | 3425 | 666 (19.4) | 76 (2.2) |
| Subtotal (≤32) | 4964 | 1634 (32.9) | 409 (8.2) |
| 33–35 | 1030 | 56 (6.1) | 6 (0.6) |
| >35 | 121 | 5 (4.1) | – |
| Total | 6115 | 1695 (27) | 414 (6.7) |
| Birth weight (g) | Screened infants (n) | Any ROP (n, %) | Severe ROP (n, %) |
| ≤1000 | 1109 | 761 (68) | 288 (26) |
| 1001–1250 | 1085 | 438 (40) | 74 (6.8) |
| 1251–1500 | 1296 | 269 (20.8) | 33 (2.5) |
| Subtotal (≤1500) | 3490 | 1468 (42) | 395 (11) |
| 1501–2000 | 1944 | 201 (10.3) | 19 (1) |
| >2000 | 681 | 26 (3.8) | – |
| Total | 6115 | 1695 (27) | 414 (6.7) |
ROP, retinopathy of prematurity.
Of the total study cohort, a total of 551 infants (9%) were born to refugees. There were no statistically significant differences in any degree of ROP and severe ROP between very low birth weight (VLBW) infants of citizens (n=3193) and refugees (n=297).
Univariate analyses identified several risk factors as potential markers. Table 2 shows the relationships between severe ROP and risk factors in infants with a BW≤1500 g.
Table 2.
Univariate analyses of covariates for severe ROP development in infants with a BW≤1500 g
| Covariates | Infants BW≤1500 g | Univariate analysis (Severe ROP vs No ROP) |
|||
| No ROP (n=2022) | Severe ROP (n=395) | P value | 95% CI | OR | |
| Maternal age (years)* | 28.9±6.4 | 28.7±6.2 | 0.565 | 0.979 to 1.012 | 0.995 |
| Antenatal steroid, two doses | 870 (43%) | 145 (36.7 %) | 0.02‡ | 0.614 to 0.959 | 0.767 |
| Preeclampsia | 544 (26 %) | 83 (21%) | 0.015‡ | 0.556 to 0.938 | 0.722 |
| Gestational diabetes | 106 (5 %) | 23 (5.8 %) | 0.640 | 0.702 to 1.777 | 1.117 |
| Chorioamnionitis | 165 (8 %) | 56 (14 %) | <0.001‡ | 1.343 to 2.570 | 1.858 |
| IVF pregnancy | 247 (12%) | 41 (10 %) | 0.832 | 0.586 to 1.180 | 0.832 |
| Multiple births | |||||
| Twins | 424 (21%) | 80 (20.3 %) | 0.728 | 0.729 to 1.248 | 0.953 |
| Triplets | 76 (3.8 %) | 14 (3.5%) | 0.810 | 0.519 to 1.668 | 0.931 |
| Vaginal delivery | 236 (12 %) | 83 (21 %) | <0.001‡ | 1.524 to 2.656 | 2.012 |
| Gestational age (weeks)* | 29.8±2.2 | 26.5±1.9 | <0.001‡ | 0.441 to 0.511 | 0.475 |
| BW (g)* | 1215±215 | 888±228 | <0.001‡ | 0.994 to 0.995 | 0.994 |
| Male gender | 934 (46 %) | 207 (52 %) | 0.028‡ | 1.035 to 1.593 | 1.284 |
| SGA | 520 (25.7 %) | 50 (12.7 %) | <0.001‡ | 0.306 to 0.572 | 0.418 |
| Resuscitation at birth | 853 (42 %) | 306 (77 %) | <0.001‡ | 3.667 to 6.070 | 4.717 |
| RDS | 1228 (83 %) | 361 (91 %) | <0.001 | 4.820 to 9.957 | 6.928 |
| Surfactant treatment | 959 (47 %) | 340 (86 %) | <0.001‡ | 5.092 to 9.240 | 6.859 |
| Duration of invasive mechanical ventilation (days)† | 0±2 (0–148) | 17±40 (0–308) | <0.001‡ | 1.063 to 1.080 | 1.071 |
| Duration of noninvasive ventilation (days)† | 3±7 (0–87) | 18±22 (0–120) | <0.001‡ | 1.079 to 1.100 | 1.090 |
| Total days on oxygen† | 10±23 (0–171) | 65±53 (0–308) | <0.001‡ | 1.047 to 1.057 | 1.052 |
| PDA requiring treatment | 349 (36 %) | 210 (53 %) | <0.001‡ | 4.326 to 6.837 | 5.438 |
| Intracranial haemorrhage (>Grade II) | 73 (3.6 %) | 70 (17.7 %) | <0.001‡ | 4.057 to 8.142 | 5.748 |
| Early-onset neonatal sepsis | 433 (21 %) | 167 (42 %) | <0.001‡ | 2.149 to 3.378 | 2.694 |
| Late-onset neonatal sepsis | 677 (33 %) | 294 (74 %) | <0.001‡ | 4.537 to 7.394 | 5.792 |
| NEC (≥Stage II) | 142 (7 %) | 84 (21 %) | <0.001‡ | 2.680 to 4.840 | 3.601 |
| BPD | 273 (13 %) | 266 (67 %) | <0.001 | 10.324 to 16.884 | 13.203 |
| Frequency of RBC transfusions | |||||
| Once | 426 (21 %) | 41 (10%) | <0.001‡ | 2.637 to 7.503 | 4.448 |
| Twice and more | 532 (26 %) | 331 (83%) | <0.001‡ | 18.607 to 44.438 | 28.756 |
| Breastfeeding more than 80% of feeding at PN 28 days, (n, %) | 1347 (66 %) | 162 (41 %) | <0.001‡ | 0.279 to 0.434 | 0.348 |
| Age of regain BW (days)* | 11.3±5.1 | 14.5±6 | <0.001‡ | 1.080 to 1.121 | 1.100 |
| Relative weight gain at 28 days (g)* | 382±180 | 229±135 | <0.001‡ | 0.993 to 0.995 | 0.994 |
*The values are presented as mean±SD.
†The values are presented as median±IQR, min-max values are given in parentheses.
‡The variables that were put in the logistic regression model.
BPD, bronchopulmonary dysplasia; BW, birth weight; IVF, in vitro fertilisation; n, number of patients; NEC, necrotising enterocolitis; p, significant difference between patients with severe ROP versus those with no ROP, defined as p<0.05; PDA, patent ductus arteriosus; PN, postnatal; RBC, red blood cell; RDS, respiratory distress syndrome; ROP, retinopathy of prematurity; SGA, small for gestational age.
All risk factors found to be significant were analysed using a multivariate logistic regression model. Table 3 shows the independent risk factors for severe ROP in VLBW infants.
Table 3.
Independent risk factors for severe retinopathy of prematurity in infants with a birth weight≤1500 g
| Adjusted OR | 95% CI | P value | |
| Gestational age (weeks)* | 0.812 | 0.726 to 0.910 | <0.001 |
| Birth weight (g)† | 0.998 | 0.997 to 0.999 | <0.001 |
| Small for gestational age | 0.471 | 0.277 to 0.799 | 0.005 |
| Total days on oxygen‡ | 1.025 | 1.019 to 1.031 | <0.001 |
| Late-onset sepsis | 1.423 | 1.016 to 1.994 | 0.04 |
| Frequency of red blood cell transfusions≥twice | 2.384 | 1.389 to 4.092 | 0.002 |
| Relative weight gain at 28 days (grams) | 0.998 | 0.997 to 0.999 | <0.001 |
P<0.05 represents statistical significance.
*OR for every week.
†OR for every 1 g.
‡OR for each day on oxygen.
Using multivariate logistic regression analyses, the following were independent risk factors for any ROP in infants with BW>1500 g: GA (for every 100 g) (OR, 0.863; 95% CI 0.775 to 0.960; p=0.007), BW (for every week) (OR, 0.997; 95% CI 0.996 to 0.998; p<0.001), RBC transfusion (≥once) (OR, 1.545; CI 1.067 to 2.237; P=0.021) and total days on oxygen (for each day on oxygen) (OR, 1.023; CI 1.014 to 1.032; p<0.001).
Of all of the infants screened for ROP, 414 (6.7%) needed treatment. A total of 395 (95.4%) of the treated infants had a BW≤1500 g and treatment was performed in 19 infants with a BW of 1501–2000 g. Severe ROP was diagnosed in five babies with BW>1500 g and GA>32 weeks who required treatment. Treatment was applied bilaterally in 385 patients and was performed in one eye in 29 cases. Five infants with a GA≤28 weeks underwent vitreoretinal surgery. Table 4 lists the severities and treatment modalities of ROP in the treated patients.
Table 4.
Severity and treatment modalities of ROP in treated patients
| Severity of ROP | Only IVB | Only laser treatment | IVB and laser treatment | Total N, (%) |
| APROP | 45 | 26 | 15 | 86 (20.8%) |
| Type 1 ROP | 93 | 145 | 24 | 262 (63.3%) |
| Zone I, any stage of ROP with plus | 28 | 9 | 7 | 44 |
| Zone I, stage 3 without plus | 6 | 2 | 2 | 10 |
| Zone II, stage 2 or 3 with plus | 59 | 134 | 15 | 208 |
| Type 2 ROP | 20 | 24 | - | 44 (10.6%) |
| Zone I, stage 1 or 2 without plus | 4 | 5 | - | 9 |
| Zone II, stage 3 without plus | 16 | 19 | - | 35 |
| Unclassified | 6 | 15 | 1 | 22 (5.3%) |
| Zone II, stage 1 with plus | 4 | 5 | - | 9 |
| Zone III, stage 2 with plus | 1 | 6 | 1 | 8 |
| Zone III, stage 3 with plus | 1 | 4 | - | 5 |
| Total N, (%) | 164 (39.6%) |
210 (50.7%) |
40 (9.7%) |
414 (100%) |
APROP, aggressive posterior retinopathy of prematurity; IVB, intravitreal bevacizumab; N, number of patients; ROP, retinopathy of prematurity.
The incidence of severe ROP in university hospitals, in state hospitals and in private hospitals was 6.2%, 6.8% and 8.4% respectively. Mean GA and mean BW of infants with severe ROP varied between different types of NICU (table 5).
Table 5.
Mean BWs and GAs of infants with severe ROP according to types of units
| University hospitals (n=192) |
State hospitals (n=164) |
Private hospitals (n=58) |
P value* | |
| Mean GA (weeks) | 26.3±2 | 26.7±2.2 | 27.9±2.1 | <0.05 |
| Mean BW (g) | 878±250 | 905±273 | 1128±299 | <0.05 |
*The values are significantly higher in private hospitals than in university and state hospitals.
BW, birth weight; GA, gestational age; n, number of patients; ROP, retinopathy of prematurity.
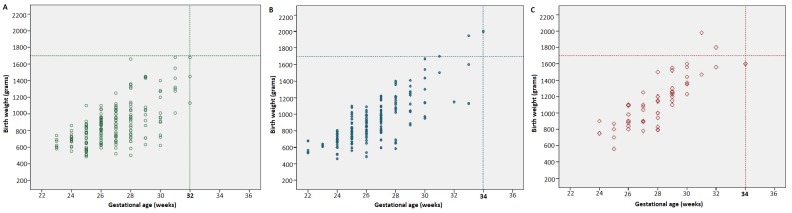
Appropriate criteria for screening for the NICUs in university hospitals should be <1700 g or ≤32 weeks and for the NICUs in state hospitals and private hospitals should be <1700 g or ≤34 weeks (figure 1).
Figure 1.
Plots of BW versus GA for infants treated for ROP in three different types of NICU. (A) University hospitals. (B) State hospitals. (C) Private hospitals. BW, birth weight; GA, gestational age; NICU, neonatal intensive care unit; ROP, retinopathy of prematurity.
Discussion
ROP is a serious morbidity of prematurity, whose incidence and severity increase with decreasing GA and BW. Studies conducted in high-income countries have shown that infants born at ≥32 weeks are not at risk for developing ROP and most infants born at >28 weeks who develop ROP have a mild disease that spontaneously regressed without treatment.9 The findings of the TR-ROP study were comparable to those from other developing countries and showed that more mature and heavier babies were at risk for severe ROP.10
There were no differences in any ROP and severe ROP development between VLBW infants of refugees and citizens in our study. The Ministry of Health of Turkey has been involved in direct healthcare services in the refugee camps and through the referral of refugees to Turkish hospitals. The 2015 report of the Turkish Neonatology Society reported a mortality rate of 26% for babies with a BW<1500 g, according to data obtained from 59 NICUs.11 However, there were insufficient data on the neonatal mortality of refugees in this report.
GA, BW and oxygen therapy are well-known major risk factors in the development of ROP.12 In this study, a lower BW, shorter GA and total days on oxygen were found as independent risk factors for severe ROP in infants with a BW≤1500 g and for any ROP in infants with a BW>1500 g.
Some previous studies have reported that the prevalence of ROP was higher in SGA infants compared with appropriate for GA preterms, while SGA was not found to be a risk factor for ROP in other reports.13 14 Factors that are considered an increased risk for severe ROP in SGA babies include chronic uterine hypoxia, abnormal growth factor levels, nutrient restriction and antioxidant deficiency.15 However, in our study, SGA was surprisingly associated with a decreased incidence of severe ROP in VLBW infants when using a multivariate logistic regression model.
There was a relationship between poor postnatal weight gain and an increased risk for ROP.16 Poor postnatal weight gain was also found as an independent risk factor for severe ROP in infants with a BW≤1500 g in our study. Using univariate analyses, several risk factors including RDS, respiratory support, sepsis, NEC, PDA, intracranial haemorrhage and BPD were significantly associated with severe ROP in VLBW infants in our cohort. These perinatal morbidities may have decreased postnatal weight gains.
This study showed that RBC transfusions had strong effects on the development of ROP. Transfusions may increase oxygen delivery to the retina because of the lower oxygen affinity of adult haemoglobin in packed red cells. Repeated transfusions may also cause free iron accumulation, which may result in increased production of free hydroxyl radicals as assessed by the Fenton reaction, resulting in damage to the retina.17 Although the role of blood transfusions as a risk factor for ROP was suggested by numerous reports,18 19 several studies have reported that a transfusion limitation policy did not reduce the prevalence of ROP.20 Our data suggested that limiting blood transfusion in regards to threshold haemoglobin values in guidelines could contribute to reducing the prevalence of ROP.
Multiple studies have reported the role of neonatal sepsis in the development of ROP.21 22 In this study, late onset sepsis was an independent risk factor for severe ROP in VLBW infants. Sepsis may act through cytokines and endotoxins, which directly affect retinal angiogenesis. This process is frequently accompanied by hypotension, which can cause tissue perfusion impairment and retinal ischaemia.23
Treatment was performed in 6.7% of the infants screened for ROP in the current study. In nearly half of the infants with severe ROP, the treatment modality involved laser photocoagulation and IVB was performed in the other half as the first choice. A nationwide population-based study from the UK reported that diode laser photocoagulation was performed in 90.5% of infants requiring treatment.1 The higher usage of IVB in our study may be due to ease of administration (typically at the bedside). In addition, paediatric anaesthesia for performing laser photocoagulation was not available in some NICUs in our study.
Notably, 66 (16%) of 414 infants were treated earlier than type 1 ROP and did not fulfil the ETROP requirements for treatment in our study. Twenty-six of these 66 infants were treated with IVB. The popularity of anti-VEGF agents is increasing in Turkey; however, the long-term safety and efficacy of these agents are still not definitively known. The risk of progression to retinal detachment in type 1 ROP is around 15%, but is much lower with less severe disease.8 Evidence-based data are not available to confirm a favourable risk–benefit ratio of IVB usage in cases earlier than type 1 ROP.
In our study, the incidence of severe ROP varied between the three types of NICU which reflects the differences in neonatal care. The rates of severe ROP were lower in university hospital NICUs, where practices for newborn care are likely to be better than non-university NICUs. Based on the results of present study, the screening criteria for ROP need to be wider in state and private hospitals than applied in the university hospitals. ROP programmes in Turkey should adopt the criteria of <1700 g or ≤34 weeks to capture all babies requiring treatment.
The strength of the TR-ROP study was that it was a large multicentre cohort study that allowed us to prospectively obtain data via a special network. However, the neonatologists did not go through any training in order to standardise definitions of potential risk factors before the study started. Similarly, the participating ophthalmologists also did not undergo any processes to standardise how they graded ROP. These situations are the limitations of the study.
In conclusion, screening criteria for ROP in Turkey needs to be wider than developed countries. The high incidence of infants with ROP in our study emphasised the need for aggressive measures for prevention and control of the disease. The safe implementation of oxygen therapy with appropriate monitoring, better antenatal and neonatal care, meticulous attention to hygienic procedures and control of sepsis may reduce the prevalence of ROP. Therefore, monitoring standards of neonatal care and conducting quality improvement projects across the country are essential for improving neonatal outcomes in Turkish NICUs.
Acknowledgments
We thank Bulent Celik from the Department of Statistics, Gazi University, Ankara, for statistical analysis.
Footnotes
Contributors: All authors made substantial contributions to conception, design, analysis and interpretation of data and contributed to writing the article and approved the current version.
Funding: This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors
Competing interests: None declared.
Patient consent: Guardian consent obtained.
Ethics approval: The study was approved by the ethical review committee of Gulhane Faculty of Medicine.
Provenance and peer review: Not commissioned; externally peer reviewed.
Collaborators: TR-ROP Study Group Collaborators (Neonatology): Fatma Nur Sari (Dr Zekai Tahir Burak Women’s Health Education and Research Hospital, University of Health Sciences, Ankara); Guner Karatekin (Zeynep Kamil Maternity and Children’s Training and Research Hospital, University of Health Sciences, Istanbul); Esad Koklu (Megapark Hospital, Kahramanmaras); Huseyin Altunhan (Necmettin Erbakan University, Meram Faculty of Medicine, Konya); Hatice Turgut (Inonu University Faculty of Medicine, Malatya); Fatma Narter (Kartal Lutfi Kirdar Education and Research Hospital, University of Health Sciences, Istanbul); Nuriye Tarakci (Dr Faruk Sukan Maternity and Children’s Hospital, Konya); Kadir Serafettin Tekgunduz (Ataturk University Faculty of Medicine, Erzurum); Servet Ozkiraz (Medicalpark Hospital, Gaziantep); Cumhur Aydemir (Bulent Ecevit University Faculty of Medicine, Zonguldak); Ahmet Ozdemir (Erciyes University Faculty of Medicine, Kayseri); Bilin Cetinkaya (Baskent University Faculty of Medicine, Adana); Ebru Kazanci (Kanuni Sultan Suleyman Training and Research Hospital, University of Health Sciences, Istanbul); Ayhan Tastekin (Medipol University, Istanbul); Sebnem Calkavur (Dr Behcet Uz Children’s Hospital, University of Health Sciences, Izmir); Banu Mutlu Ozyurt (Mersin State Hospital, Mersin); Yasar Demirelli (Erzurum Nenehatun Maternity Hospital, Erzurum); Huseyin Selim Asker (NCR International Hospital, Gaziantep); Birgul Mutlu (Doruk Yildirim Private Hospital, Bursa); Ozgun Uygur (Tepecik Training and Research Hospital, University of Health Sciences, Izmir); Hilal Ozkan (Uludag University Faculty of Medicine, Bursa); Didem Armangil (Yuksek Ihtisas University Faculty of Medicine, Ankara); Ferda Ozlu (Cukurova University Faculty of Medicine, Adana); Mustafa Kurthan Mert (Numune Training and Education Hospital, University of Health Sciences, Adana); Hacer Ergin (Pamukkale University Faculty of Medicine, Denizli); Beyza Ozcan (Konya Education and Research Hospital, University of Health Sciences, Konya); Evrim Kiray Bas (Sisli Hamidiye Etfal Education and Research Hospital, University of Health Sciences, Istanbul); Emel Okulu (Ankara University Faculty of Medicine, Ankara); Betul Acunas (Trakya University Faculty of Medicine, Edirne); Ulker Celik (Denizli State Hospital, Denizli); Sait Ilker Uslu (Ondokuz Mayıs University, Faculty of Medicine, Samsun); Mehmet Mutlu (Karadeniz Technical University Faculty of Medicine, Trabzon); Nihat Demir (Yuzuncu Yil University Faculty of Medicine, Van); Funda Eroglu (Ankara Guven Hospital, Ankara); Zeynel Gokmen (Baskent University Faculty of Medicine, Konya); Serdar Beken (Acibadem University Faculty of Medicine, Istanbul); Bilge Tanyeri Bayraktar (Bezmialem University Faculty of Medicine, Istanbul); Nilay Hakan (Mugla Sitki Kocman University Faculty of Medicine, Mugla); Kazım Kucuktasci (Denizli Private Saglik Hospital, Denizli); Aysen Orman (Firat University Faculty of Medicine, Elazig); Serdar Comert (Suleymaniye Maternity, Research & Training Hospital, University of Health Sciences, Istanbul); Sabahattin Ertugrul (Dicle University Faculty of Medicine, Diyarbakir); Nuran Ustun (Medeniyet University Faculty of Medicine, Istanbul); Ozlem Sahin (Umraniye Education and Research Hospital, University of Health Sciences, Istanbul); Demet Terek (Ege University Faculty of Medicine, Izmir); Yusuf Kale (Cengiz Gokcek Maternity and Children’s Hospital, Gaziantep); Murat Konak (Konya Selcuk University Faculty of Medicine, Konya); Sadık Yurttutan (Kahramanmaras Sutcu Imam University Faculty of Medicine, Kahramanmaras); Ozge Aydemir (Osmangazi University Faculty of Medicine, Eskisehir); Aysegul Zenciroglu (Dr Sami Ulus Maternity and Children’s Hospital, University of Health Sciences, Ankara); Dilek Sarici (Kecioren Education and Research Hospital, University of Health Sciences, Ankara); Nilufer Guzoglu (Kirikkale University Faculty of Medicine, Kirikkale); Sahin Hamilcikan (Bagcilar Education and Research Hospital, University of Health Sciences, Istanbul); Tugba Gursoy (Koc University Faculty of Medicine, Istanbul); Funda Tuzun (Dokuz Eylul University Faculty of Medicine, Izmir); Rahmi Ors (Medova Hospital, Konya); Selda Arslan (Mustafa Kemal University Faculty of Medicine, Hatay); Arzu Akdag (Bursa Dortcelik Children’s Hospital, Bursa); Asli Memisoglu (Marmara University Faculty of Medicine, Istanbul); Beril Yasa (Istanbul University, Istanbul Faculty of Medicine, Istanbul); Berna Hekimoglu (Trabzon Kanuni Education and Research Hospital, University of Health Sciences, Trabzon); Ozden Turan (Baskent University Faculty of Medicine, Ankara); Hakan Aylanc (Onsekizmart University Faculty of Medicine, Canakkale); Sahin Takci (Gaziosmanpasa University Faculty of Medicine, Tokat); Tolga Celik (Hacettepe University Faculty of Medicine, Ankara); Suzan Sahin (Adnan Menderes University Faculty of Medicine, Aydin); Ilknur Kilic (Atasehir Kadikoy Sifa Hospital, Istanbul). TR-ROP Study Group Collaborators (Ophthalmology): Caner Kara (Etlik Zubeyde Hanim Women’s Health Teaching and Research Hospital, University of Health Sciences, Ankara); Zuhal Ozen Tunay (Dr Zekai Tahir Burak Women’s Health Education and Research Hospital, University of Health Sciences, Ankara); Gokhan Celik (Zeynep Kamil Maternity and Children’s Training and Research Hospital, University of Health Sciences, Istanbul); Ibrahim Gozen (Megapark Hospital, Kahramanmaras); Gunhal Satirtav (Necmettin Erbakan University, Meram Faculty of Medicine, Konya); Nihat Polat (Inonu University Faculty of Medicine, Malatya); Ayse Yesim Oral (Kartal Lutfi Kirdar Education and Research Hospital, University of Health Sciences, Istanbul); Mine Tokgoz (Konya Numune Hospital, Konya); Sadullah Keles (Ataturk University Faculty of Medicine, Erzurum); Burak Bilgin (Medicalpark Hospital, Gaziantep); Silay Canturk Ugurbas (Bulent Ecevit University Faculty of Medicine, Zonguldak); Cagatay Karaca (Erciyes University Faculty of Medicine, Kayseri); Nedime Sahinoglu Keskek (Baskent University Faculty of Medicine, Adana); Dilbade Yildiz Ekinci (Kanuni Sultan Suleyman Training and Research Hospital, University of Health Sciences, Istanbul); Ozlem Balci (Istanbul Medipol University, Istanbul); Emir Volkan Altan (Dr Behcet Uz Children’s Hospital, University of Health Sciences, Izmir); Sevda Bakbak(Mersin State Hospital, Mersin); Nihan Aksu Ceylan (Erzurum Regional Education and Research Hospital, University of Health Sciences, Erzurum); Sabit Kimyon (Gaziantep University Faculty of Medicine, Gaziantep); Gunay Alyamac (Retina Eye Hospital, Bursa); Gamze Ture (Tepecik Training and Research Hospital, University of Health Sciences, Izmir); Meral Yildiz (Uludag University Faculty of Medicine, Bursa); Feyza Calis (Yuksek Ihtisas University Faculty of Medicine, Ankara); Selcuk Sizmaz (Cukurova University Faculty of Medicine, Adana); Emine Sukgen (Numune Training and Education Hospital, University of Health Sciences, Adana); Ebru Nevin Cetin (Pamukkale University Faculty of Medicine, Denizli); Muammer Ozcimen, (Konya Education and Research Hospital, University of Health Sciences, Konya); Semra Tiryaki Demir (Sisli Hamidiye Etfal Education and Research Hospital, University of Health Sciences, Istanbul); Huban Atila (Ankara University Faculty of Medicine, Ankara); Altan Ozal (Trakya University Faculty of Medicine, Edirne); Gokhan Tufaner (Denizli State Hospital, Denizli); Ozlem Eski Yucel (Ondokuz Mayıs University Faculty of Medicine, Samsun); Mehmet Kola (Karadeniz Technical University Faculty of Medicine, Trabzon); Erbil Seven (Yuzuncu Yil University Faculty of Medicine, Van); Sengul Ozdek (Gazi University Faculty of Medicine, Ankara); Ali Hakan Durukan (Ankara Guven Hospital, Ankara); Ali Kal (Baskent University Faculty of Medicine, Konya); Ali Riza Cenk Celebi (Acibadem University Faculty of Medicine; Istanbul); Ibrahim Arif Koytak (Bezmialem University Faculty of Medicine, Istanbul); Goksu Alacamli (Mugla Sitki Kocman University Faculty of Medicine, Mugla); Arif Esme (Denizli Private Saglik Hospital; Denizli); Onur Catak (Firat University Faculty of Medicine, Elazig); Irfan Perente (Suleymaniye Maternity, Research & Training Hospital, University of Health Sciences, Istanbul); Alparslan Sahin (Dicle University Faculty of Medicine, Diyarbakir); Aylin Ardagil Akcakaya (Istanbul Medeniyet University Faculty of Medicine Istanbul); Gulunay Kiray (Umraniye Education and Research Hospital, University of Health Sciences, Istanbul); Serhat Nalcaci (Ege University Faculty of Medicine, Izmir); Umit Aksoy (Cengiz Gokcek Maternity and Children’s Hospital, Gaziantep); Berker Bakbak (Konya Selcuk University Faculty of Medicine, Konya); Aysegul Comez (Kahramanmaras Sutcu Imam University Faculty of Medicine, Kahramanmaras); Huseyin Gursoy (Osmangazi University Faculty of Medicine, Eskisehir); Emrah Utku Kabatas (Dr Sami Ulus Maternity and Children’s Hospital, University of Health Sciences, Ankara); Ikbal Seza Petricli (Etlik Zubeyde Hanim Women’s Health Teaching and Research Hospital, University of Health Sciences, Ankara); Mehmet Erhan Yumusak (Kirikkale University Faculty of Medicine, Kirikkale); Ahmet Kirgiz (Bagcilar Education and Research Hospital, University of Health Sciences, Istanbul); Gunay Uludag (Koc University Faculty of Medicine, Istanbul); Aylin Yaman (Dokuz Eylul University Faculty of Medicine, Izmir); Zeynep Dadaci (Medova Hospital, Konya);Ali Karatas (Bursa Dortcelik Children’s Hospital, Bursa); Hande Celiker (Marmara University Faculty of Medicine, Istanbul);Zafer Cebeci (Istanbul University, Istanbul Faculty of Medicine, Istanbul); Mahmut Cenap Esenulku (Trabzon Kanuni Education and Research Hospital, University of Health Sciences, Trabzon); Imren Akkoyun (Baskent University, Faculty of Medicine, Ankara); Ismail Ersan (Onsekizmart University Faculty of Medicine, Canakkale); Selim Demir (Gaziosmanpasa University Faculty of Medicine, Tokat); Sibel Kadayifcilar (Hacettepe University Faculty of Medicine, Ankara); Ayse Ipek Akyuz Unsal (Adnan Menderes University Faculty of Medicine, Aydin); Mumin Hocaoglu (Istanbul Retina Institute, Istanbul).
Correction notice: This article has been corrected since it published Online First. Typos in several of the Collaborator names have been corrected.
Contributor Information
TR-ROP Study Group:
Fatma Nur Sari, Guner Karatekin, Esad Koklu, Huseyin Altunhan, Hatice Turgut, Fatma Narter, Nuriye Tarakci, Kadir Serafettin Tekgunduz, Servet Ozkiraz, Cumhur Aydemir, Ahmet Ozdemir, Bilin Cetinkaya, Ebru Kazanci, Ayhan Tastekin, Sebnem Calkavur, Banu Mutlu Ozyurt, Yaşar Demirelli, Huseyin Selim Asker, Birgul Mutlu, Ozgun Uygur, Hilal Ozkan, Didem Armangil, Ferda Ozlu, Mustafa Kurthan Mert, Hacer Ergin, Beyza Ozcan, Evrim Kıray Bas, Emel Okulu, Betul Acunas, Ulker Celik, Sait Ilker Uslu, Mehmet Mutlu, Nihat Demir, Funda Eroglu, Zeynel Gökmen, Serdar Beken, Bilge Tanyeri Bayraktar, Nilay Hakan, Kazım Kucuktascı, Aysen Orman, Serdar Comert, Sabahattin Ertugrul, Nuran Ustun, Ozlem Sahin, Demet Terek, Yusuf Kale, Murat Konak, Sadık Yurttutan, Ozge Aydemir, Ayşegül Zenciroglu, Dilek Sarici, Nilufer Guzoglu, Sahin Hamilcikan, Tugba Gursoy, Funda Tuzun, Rahmi Ors, Selda Arslan, Arzu Akdag, Asli Memisoglu, Beril Yasa, Berna Hekimoglu, Ozden Turan, Hakan Aylanc, Sahin Takci, Tolga Celik, Suzan Sahin, Ilknur Kilic, Caner Kara, Zuhal Ozen Tunay, Gokhan Celik, Ibrahim Gozen, Gunhal Satirtav, Nihat Polat, Ayse Yesim Oral, Mine Tokgoz, Sadullah Keles, Burak Bilgin, Silay Canturk Ugurbas, Cagatay Karaca, Nedime Sahinoglu Keskek, Dilbade Yildiz Ekinci, Ozlem Balci, Emir Volkan Altan, Sevda Bakbak, Nihan Aksu Ceylan, Sabit Kimyon, Gunay Alyamac, Gamze Ture, Meral Yildiz, Feyza Calis, Selcuk Sizmaz, Emine Sukgen, Ebru Nevin Cetin, Muammer Ozcimen, Semra Tiryaki Demir, Huban Atila, Altan Ozal, Gokhan Tufaner, Ozlem Eski Yucel, Mehmet Kola, Erbil Seven, Sengul Ozdek, Ali Hakan Durukan, Ali Kal, Ali Riza Cenk Celebi, Ibrahim Arif Koytak, Goksu Alacamlı, Arif Esme, Onur Catak, Irfan Perente, Alparslan Sahin, Aylin Ardagil Akcakaya, Gulunay Kiray, Serhat Nalcaci, Umit Aksoy, Berker Bakbak, Aysegül Comez, Huseyin Gursoy, Emrah Utku Kabatas, Ikbal Seza Petricli, Mehmet Erhan Yumusak, Ahmet Kirgiz, Gunay Uludag, Aylin Yaman, Zeynep Dadaci, Ali Karatas, Hande Celiker, Zafer Cebeci, Mahmut Cenap Esenulku, Imren Akkoyun, İsmail Ersan, Selim Demir, Sibel Kadayifcilar, Ayse Ipek Akyuz Unsal, and Mumin Hocaoglu
Collaborators: TR-ROP Study Group
References
- 1. Adams GGW, Bunce C, Xing W, et al. Treatment trends for retinopathy of prematurity in the UK. BMJ Open 2017;21:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Gilbert C. Retinopathy of prematurity: a global perspective of the epidemics, population of babies at risk and implications for control. Early Hum Dev 2008;84:77–82. 10.1016/j.earlhumdev.2007.11.009 [DOI] [PubMed] [Google Scholar]
- 3. Chaudhry TA, Hashmi FK, Salat MS, et al. Retinopathy of prematurity: an evaluation of existing screening criteria in Pakistan. Br J Ophthalmol 2014;98:298–301. 10.1136/bjophthalmol-2013-304018 [DOI] [PubMed] [Google Scholar]
- 4. Mikolajczyk RT, Zhang J, Betran AP, et al. A global reference for fetal-weight and birthweight percentiles. Lancet 2011;377:1855–61. 10.1016/S0140-6736(11)60364-4 [DOI] [PubMed] [Google Scholar]
- 5. Papile LA, Burstein J, Burstein R, et al. Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1,500 gm. J Pediatr 1978;92:529–34. 10.1016/S0022-3476(78)80282-0 [DOI] [PubMed] [Google Scholar]
- 6. Bell MJ, Ternberg JL, Feigin RD, et al. Neonatal necrotizing enterocolitis. Therapeutic decisions based upon clinical staging. Ann Surg 1978;187:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. International Committee for the Classification of Retinopathy of Prematurity. The International Classification of Retinopathy of Prematurity revisited. Arch Ophthalmol 2005;123:991–9. 10.1001/archopht.123.7.991 [DOI] [PubMed] [Google Scholar]
- 8. Early Treatment For Retinopathy Of Prematurity Cooperative Group. Revised indications for the treatment of retinopathy of prematurity: results of the early treatment for retinopathy of prematurity randomized trial. Arch Ophthalmol 2003;121:1684–9. 10.1001/archopht.121.12.1684 [DOI] [PubMed] [Google Scholar]
- 9. Holmström G, Hellström A, Jakobsson P, et al. Evaluation of new guidelines for ROP screening in Sweden using SWEDROP - a national quality register. Acta Ophthalmol 2015;93:265–8. 10.1111/aos.12506 [DOI] [PubMed] [Google Scholar]
- 10. Tabarez-Carvajal AC, Montes-Cantillo M, Unkrich KH, et al. Retinopathy of prematurity: screening and treatment in Costa Rica. Br J Ophthalmol 2017;101:1709–13. 10.1136/bjophthalmol-2016-310005 [DOI] [PubMed] [Google Scholar]
- 11. Society TN. Mortality rates in Turkish NICUs in 2016. Turk Neonatol Soc Bull 2017;29:32–4. Article in Turkish. [Google Scholar]
- 12. Phelps DL. Retinopathy of prematurity : Martin RJ, Fanaroff AA, Walsh MC, Fanaroff and Martin’s neonatal perinatal medicine: diseases of the fetus and infant. Philadelphia: Elsevier Saunders, 2015:1767–74. [Google Scholar]
- 13. Bernstein IM, Horbar JD, Badger GJ, et al. Morbidity and mortality among very-low-birth-weight neonates with intrauterine growth restriction. The vermont Oxford Network. Am J Obstet Gynecol 2000;182:198–206. 10.1016/S0002-9378(00)70513-8 [DOI] [PubMed] [Google Scholar]
- 14. Filho JBF, Valiatti FB, Eckert GU, et al. Is being small for gestational age a risk factor for retinopathy of prematurity? A study with 345 very low birth weight preterm infants. J Pediatr 2009;85:48–54. 10.2223/JPED.1870 [DOI] [PubMed] [Google Scholar]
- 15. Kavurt S, Özcan B, Aydemir O, et al. Risk of retinopathy of prematurity in small for gestational age premature infants. Indian Pediatr 2014;51:804–6. 10.1007/s13312-014-0506-9 [DOI] [PubMed] [Google Scholar]
- 16. Hellström A, Hård AL, Engström E, et al. Early weight gain predicts retinopathy in preterm infants: new, simple, efficient approach to screening. Pediatrics 2009;123:e638–e645. 10.1542/peds.2008-2697 [DOI] [PubMed] [Google Scholar]
- 17. Wardle SP, et al. Effect of blood transfusion on lipid peroxidation in preterm infants. Arch Dis Child Fetal Neonatal Ed 2002;86:46F–8. 10.1136/fn.86.1.F46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Hesse L, Eberl W, Schlaud M, et al. Blood transfusion. Iron load and retinopathy of prematurity. Eur J Pediatr 1997;156:465–70. [DOI] [PubMed] [Google Scholar]
- 19. Dani C, Reali MF, Bertini G, et al. The role of blood transfusions and iron intake on retinopathy of prematurity. Early Hum Dev 2001;62:57–63. 10.1016/S0378-3782(01)00115-3 [DOI] [PubMed] [Google Scholar]
- 20. Kirpalani H, Whyte RK, Andersen C, et al. The Premature Infants in Need of Transfusion (PINT) study: a randomized, controlled trial of a restrictive (low) versus liberal (high) transfusion threshold for extremely low birth weight infants. J Pediatr 2006;149:301–7. 10.1016/j.jpeds.2006.05.011 [DOI] [PubMed] [Google Scholar]
- 21. Tolsma KW, Allred EN, Chen ML, et al. Neonatal bacteremia and retinopathy of prematurity: the ELGAN study. Arch Ophthalmol 2011;129:155–63. 10.1001/archophthalmol.2011.319 [DOI] [PubMed] [Google Scholar]
- 22. Stoll BJ, Hansen NI, Adams-Chapman I, et al. Neurodevelopmental and growth impairment among extremely low-birth-weight infants with neonatal infection. JAMA 2004;292:2357–65. 10.1001/jama.292.19.2357 [DOI] [PubMed] [Google Scholar]
- 23. Lee J, Dammann O. Perinatal infection, inflammation, and retinopathy of prematurity. Semin Fetal Neonatal Med 2012;17:26–9. 10.1016/j.siny.2011.08.007 [DOI] [PMC free article] [PubMed] [Google Scholar]