Abstract
Moral injury (MI) results from perpetration of or exposure to distressing events, known as morally injurious events (MIEs), that challenge moral beliefs and values. Due to the type of involvement in recent military conflicts, many veterans report MIEs that may cause dissonance and, in turn, MI. Although two existing measures assess MIEs, neither currently assesses the defining characteristics of MI (i.e., guilt, shame, difficulty forgiving self and others, and withdrawal). The present study reports the initial psychometric test of a modified version (Robbins, Kelley, Hamrick, Bravo, & White, 2017) of the Moral Injury Questionnaire – Military version (MIQ-M; Currier, Holland, Drescher, & Foy, 2015) in a sample of 328 military personnel (e.g., veterans, National Guard/reservists, active duty members). The MIQ-M was modified to assess both MIEs and the defining characteristics of MI. Exploratory factor analyses suggested a three-factor model of MIEs consisting of Atrocities of war, Psychological consequences of war, and Leadership failure or betrayal. The modified MIQ-M factors were correlated with defining characteristics of MI. In addition, each MIE factor and associated defining characteristics of MI were positively correlated with symptoms of posttraumatic stress disorder, depression, and anxiety, as well as substance use. The modified MIQ-M is a reliable measure of MI that is comprised of three subscales that are associated with, but distinct from, mental health outcomes. Although findings are promising, further research evaluating the applicability of the modified MIQ-M in clinical settings is required to establish construct validity of the defining characteristics and secondary manifestations of MI.
Keywords: military, moral injury, combat, exploratory factor analysis, mental health
Introduction
Moral injury (MI) is receiving rapidly increasing attention as a form of distress experienced by members of the military. MI is the impact of “perpetrating, failing to prevent, or bearing witness to acts that transgress deeply held moral beliefs and expectations”… “because [they] violate assumptions and beliefs about right and wrong and personal goodness” (Litz et al., 2009, p. 697, 698). MI is believed to be the result of morally injurious experiences (MIEs) such as witnessing the death of a civilian, killing, failing to prevent harm or death of another, witnessing or engaging in disproportionate violence, and experiencing leadership betrayal. The discrepancy between their experiences and their views of the world and the attributions for these discrepancies may lead veterans to develop the defining characteristics of MI (i.e., guilt, shame, lack of forgiveness of self and others, and withdrawal; Frankfurt & Frazier, 2016; Jinkerson, 2016; Litz et al., 2009; Maguen & Litz, 2012). Empirical research on MI has typically assessed MIEs but not the defining characteristics of MI.
A reliable, valid measure of MI is necessary to accurately assess MI among members of the military (both active duty and veterans). The Moral Injury Questionnaire – Military version (MIQ-M; Currier, Holland, Drescher et al., 2015) is a fairly comprehensive, unidimensional measure of exposure to MIEs related to military deployment. Robbins et al. (2017) modified the original MIQ-M for two main reasons: 1) to separate the acts of witnessing and engaging in experiences from single MIE items into separate MIE items, and 2) to incorporate new items assessing proposed defining characteristics of MI (i.e., guilt, shame, difficulties with forgiveness, withdrawal; Litz et al., 2009). The present study tested the factor structure of this modified version (Robbins, Kelley, Hamrick, Bravo, & White, 2017) of the MIQ-M and examined associations among MIEs, the defining characteristics of MI, and symptoms of depression, anxiety, and posttraumatic stress disorder (PTSD) among a community sample of military personnel.
MIEs and MI among Recent-era Veterans
Combat theaters place service members in complex situations in which even morally appropriate behaviors (i.e., actions consistent with rules of engagement/sanctioned actions) may conflict with personal beliefs of morality (e.g., Farnsworth, Drescher, Nieuwsma, Walser, & Currier, 2014). In recent conflicts, unconventional warzone features, such as the presence of unmarked combatants, potential civilian threats, and extensive use of improvised explosive devices in close quarters, have resulted in ambiguity regarding the identity of combatants and the appropriate course of action in battlefield decisions (Frankfurt & Frazier, 2016; Litz et al., 2009). In situations such as these and many others, some veterans may experience dissonance as they struggle to accept or construct meaning from these experiences. That is, the individual has to reconcile discrepancies between MIEs and the way they view the world. Attributions for these experiences and particularly, attributions that are global (do not consider the context in which MIEs occurred), internal (self-condemnation), and stable (consistently judging oneself as corrupted) may lead to the defining MI characteristics, such as guilt, shame, withdrawal, and a lack of forgiveness (Buechner & Jinkerson, 2016; Drescher et al., 2011; Litz et al., 2009; Nash & Litz, 2013). Commonly regarded as the primary working model of MI, Litz et al. (2009) conceptualized the defining characteristics of MI to include guilt, shame, difficulties with forgiveness, and withdrawal. These defining characteristics are further hypothesized to be the pathways to a host of secondary negative outcomes, including poor mental health (Currier, Holland, Drescher et al., 2015; Currier, Holland, & Malott, 2015; Drescher et al., 2011; Litz et al., 2009; Nash & Litz, 2013). Empirical support has demonstrated that exposure to MIEs is associated with depression, PTSD, and anxiety (Currier, Holland, & Malott, 2015; Maguen & Litz, 2012). For this reason, in the present study we examined symptoms of depression, anxiety, and PTSD.
Assessment of Moral Injury
To accurately assess MI among active duty members and veterans, an accurate, comprehensive empirical measure is necessary. At present, two published self-report measures are available that assess for exposure to MIEs. The Moral Injury Exposure Scale (MIES; Nash et al., 2013) is an 11-item measure containing two subscales of perceived transgressions (e.g., perpetrating acts of commission or acts of omission) and perceived betrayals (e.g., perceived betrayal by leaders, self, and trusted others). A second measure is the Moral Injury Questionnaire – Military version (MIQ-M; Currier, Holland, Drescher et al., 2015), a 20-item unidimensional measure focused on military deployment-related potential MIEs. Although both scales measure exposure to MIEs, neither assesses proposed defining characteristics of MI (i.e., guilt, shame, difficulties with forgiveness; Litz et al., 2009).
The current investigation sought to test a modified version of the MIQ-M (Currier, Holland, Drescher et al., 2015). Although fairly comprehensive, several items on the MIQ-M assess both witnessing and engaging in various combat experiences within a single item. Previous research has shown that the implications of combat on mental health vary as a function of personal responsibility (e.g., killing in combat, Bryan & Cukrowicz, 2011; Maguen et al., 2010). Moreover, self-reported participation (i.e., killing or attempting to kill) had a significant association with mental health outcomes even after controlling for witnessing trauma in both Vietnam veterans (Van Winkle & Safer, 2011) and Operation Enduring Freedom/Operation Iraqi Freedom Army medics (Pitts et al., 2014). For these reasons, Robbins et al. (2017) modified the original MIQ-M such that seven items that assessed both witnessing and engaging in various events (e.g., “I saw/was involved in the death of a child” and “I saw/experienced violence that was out of proportion to the event”) were separated into two items that assess direct involvement versus bearing witness.
Further, the original MIQ-M contained items that could be considered ‘causes’ (e.g., “I was involved in the death[s] of an innocent of war”) or ‘effects’ (e.g., “I feel guilt for surviving when others didn’t”) of MI. While the inclusion of effect indicator items was a novel step in the assessment of MI, the items sometimes conflated ‘causes’ (e.g., “I survived when others didn’t”) with appraisals or ‘effects’ (e.g., “I feel guilt for surviving when others didn’t”). Assessment of both the ‘causes’ (i.e., MIEs) and ‘effects’ (i.e., defining characteristics) associated with MI is a critical next step in the understanding of MI (Frankfurt & Frazier, 2016). Consequently, Robbins et al. (2017) modified the original MIQ-M by removing items that assessed the effect of exposure to MIEs (i.e., “I feel guilty over failing to save the life of someone in war”) and instead asked participants to rate the degree to which each MIE caused them guilt, shame, difficulty forgiving self, difficulty forgiving others, and withdrawal. The purpose of this study was to examine the factor structure of the MIEs in the modified MIQ-M and to examine how the MIE factors were associated with the defining characteristics of MI and symptoms that may be outcomes of MI (i.e., depression, anxiety, and PTSD).
Method
Participants
Although the original sample (n = 717) included members of the community, the subsample used in the current study were only participants who completed the moral injury assessment (i.e., only current or former members of the military who were deployed at least once). This study examined data from a subsample of n = 328 veterans (n = 228, 69.5%), National Guard/Reservists (n = 64, 19.5%), and active duty members (n = 31, 9.5%), with an average age of M = 32.42 years old (SD = 7.71). Military status was missing for five (1.5%) participants. There were two participants (<1% of the sample) who did not complete the PCL-5, the last questionnaire in the survey. Participant characteristics are displayed in Table 1. Most participants were male (n = 184, 56.1%), White (n = 223, 68.0%), married (n = 234, 71.3%), had completed some college (n = 302, 92.0%), and were employed (n = 254, 77.4%). The most represented branch of service was the Army (n = 152, 46.3%), and the majority of participants deployed as part of Operation Iraqi Freedom (OIF), Operation Enduring Freedom (OEF), or Operation New Dawn (OND) (n = 270, 82.3%). In the larger active duty population, 85% are male, the average age is 29, 69% are European American and approximately 15% are women (Office of the Deputy Assistant Secretary of Defense, 2014). Thus, our sample is comparable in terms of ethnic/racial background, but as might be expected in a predominantly veteran population, our sample was slightly older than the typical active duty member. Also, our sample contained approximately twice as many women as would be expected in an active duty or reserve population. Finally, and consistent with recent trends (National Center for Veterans Analysis and Statistics [NCVAS], 2011), 32% of our sample had advanced degrees (i.e., MS/MA, Ph.D., JD, MD, or other professional degree). This may be accounted for by our high rate of women participants (military women are more likely to attain advanced degrees; NCVAS, 2011).
Table 1.
Demographic Information for the Sample (n = 328)
| n | % | |
|---|---|---|
| Gendera | ||
| Male | 184 | 56.1% |
| Female | 121 | 36.9% |
| Racea | ||
| White | 223 | 68.0% |
| African American | 54 | 16.5% |
| Asian or Pacific Islander | 28 | 8.5% |
| Native American | 7 | 2.1% |
| Other | 10 | 3.0% |
| Hispanic/Latino/Spanish (yes) a | 73 | 22.3% |
| Relationship Statusa | ||
| Single, never married | 65 | 19.8% |
| Cohabitating | 7 | 2.1% |
| Married | 234 | 71.3% |
| Separated | 5 | 1.5% |
| Divorced | 16 | 4.9% |
| Highest Educationa | ||
| Some high school | 5 | 1.5% |
| High school diploma/GED | 13 | 4.0% |
| Some college | 69 | 21.0% |
| Associate’s degree | 70 | 21.3% |
| Bachelor’s degree | 58 | 17.7% |
| Graduate degree | 105 | 32.0% |
| Employment Statusa | ||
| Unemployed | 15 | 4.6% |
| Employed | 254 | 77.4% |
| Student | 54 | 16.5% |
| Branch of Military Affiliationa | ||
| Army | 152 | 46.3% |
| Navy | 98 | 29.9% |
| Air Force | 26 | 7.9% |
| Marines | 18 | 5.5% |
| National Guard | 13 | 4.0% |
| Reserves | 15 | 4.6% |
| Deployment for OIF/OEF/ONDa | ||
| Yes | 270 | 82.3% |
| No | 44 | 13.4% |
Note.
= Totals may not sum to 100% due to nondisclosure by some participants. OIF = Operation Iraqi Freedom, OEF = Operation Enduring Freedom, and OND = Operation New Dawn.
Procedure
We recruited participants through Facebook (n = 91, 27.7%), military listservs (n = 54, 16.5%), the Department of Psychology research pool at the participating university (n = 53, 16.2%), student veteran organization announcements (n = 42, 12.8%), snowball sampling via friends or family (n = 31, 9.5%), flyers (n = 8, 2.4%), Craigslist (n = 10, 3.0%), and other sources (n = 34, 10.4%). Advertisements targeted veterans and military members and contained a link to a fuller description of the study as well as the survey. After reviewing the study description and consenting to participate, participants completed an online self-report survey. Participants completed the survey in the order in which the questionnaires are described below. The survey took approximately 30 minutes to complete. Non-student participants were emailed a $10 Amazon gift card; students were given research credit or were entered into one of twenty $20.00 Amazon gift card raffles (all student participants were also veterans, active duty members, National Guard, or reservists). All study documents and procedures were approved by an Institutional Review Board committee at the participating university.
Materials
Moral injury
A modified version of the Moral Injury Questionnaire – Military Version (MIQ-M; Currier, Holland, Drescher et al., 2015) was used to assess MI. Seven of the original MIQ-M items assess both perpetration and witnessing MIEs within the same item. In the modified version (Robbins et al., 2017) used in the present study, these seven items were each partitioned into two items, one assessing involvement in and another assessing witnessing of MIEs. For example, the original MIQ-M item, “I saw/was involved in the death of an innocent during the war” became “I saw the death of an innocent in the war” and “I was involved in the death of an innocent in the war” in the modified MIQ-M. The partitioning yielded 27 items that assessed MIEs. Similar to the response scale in the original MIQ-M, participants were asked to endorse the frequency with which they had experienced each item in the context of warzone deployment(s) using a 4-point response scale ranging from 1 (Never) to 4 (Often).
In addition to assessing MIEs, we also assessed defining characteristics of MI. After each of the 27 MIE items, participants answered five questions that assessed the degree to which each MIE item caused them to: 1) “feel guilt”, 2) “feel shame”, 3) “have difficulties with forgiving myself”, 4) “have difficulties forgiving others”, and 5) “become withdrawn” for each experience. Thus, respondents completed 27 MIE items and 135 follow-up questions (5 followup questions per MIE item), for a total of 162 moral injury items. The response scale was identical for items for the defining characteristics of MI, with participants endorsing the frequency with which they experienced each defining characteristic using a 4-point response scale ranging from 1 (Never) to 4 (Often). The original MIQ-M includes two items that assess for guilt in the context of specific situations (i.e., “I feel guilt over failing to save the life of someone in the war” and “I feel guilt for surviving when others didn’t”). Because the present study uses follow-up items to assess the defining characteristics of MI, these two items were modified to omit the word guilt (i.e., “I felt guilt over failing to save the life of someone in the war” was changed to “I failed to save the life of someone in the war” and “I felt guilt over surviving when others didn’t” was changed to “I survived when others didn’t”). A description of score creation is included below, to reflect decisions made after factor analysis.
Depressive symptoms
Depressive symptoms were measured using the Short Form Center for Epidemiological Studies Depression Scale (CESD-10; Kohout, Berkman, Evans, & Cornoni-Huntley, 1993), a 10-item version of the 20-item CES-D (Radloff, 1977). Respondents were asked to rate the frequency with which they experienced each item (e.g., “I felt that everything I did was an effort” and “I could not get going”) during the past week. The present study modified the CESD-10’s response scale, using the CES-D’s original 4-point Likert scale, which ranges from 0 (“Rarely or none of the time [less than 1 day]”) to 3 (“Most or all of the time [5–7 days]”) as opposed to the 0 = no, 1 = yes scale used by Kohout et al. (1993) in the development of the CESD-10. The CES-D has demonstrated excellent psychometric properties in members of the military, fitting equally well for both men and women (Boisvert, McCreary, Wright, & Asmundson, 2003), and has demonstrated associations with, but distinctions from, PTSD in trauma-exposed members of the military (Elhai, Contractor, Palmieri, Forbes, & Richardson, 2011), demonstrating discriminant validity. The CESD-10 demonstrated acceptable internal consistency in the present study (α = .73).
Anxiety symptoms
Anxiety symptoms were measured using the Kremen Anxiety Scale (KAS; Kremen, 1996). The KAS is a 14-item measure that assesses psychological and physiological symptoms of worries, apprehension, and nervousness (“I am often nervous for no reason”). Similar to the scoring of the KAS in a study of military mothers (Kelley et al., 2002), the present study modified the KAS’s original 4-point Likert response scale, ranging from 1 (Does not apply at all) to 4 (Applies very strongly), using instead a 5-point Likert scale ranging from 1 (Never) to 5 (Always). The KAS has good internal consistency and predictive validity among adolescents and college students (Kremen, 1996) and enlisted military mothers (Kelley et al., 2002). Internal consistency in the present study was excellent (α = .90).
Posttraumatic stress disorder
To assess for PTSD symptoms, respondents completed the Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5; Blevins, Weathers, Davis, Witte, & Domino, 2015; Weathers et al., 2013). The PCL-5 is a 20-item self-report measure that assesses DSM-5 (American Psychiatric Association, 2013) PTSD symptom severity during the most recent one-month period. Respondents were asked to rate each item on a 5-point Likert scale ranging from 0 (Not at all) to 4 (Extremely). Item scores are summed to yield a total PTSD symptom severity score ranging from 0 to 80. The PCL-5 has demonstrated excellent internal consistency among active duty military (α = .95 at two-week follow-up; Wortmann et al., 2016) and veterans (α = .96; Bovin et al., 2015). In the present study, the PCL-5 also demonstrated excellent internal consistency (α = .96).
Hazardous alcohol use
Hazardous alcohol use was measured using the Alcohol Use Disorders Identification Test (AUDIT; Babor, De La Fuente, Saunders, & Grant, 2001). Response options range from 0 to 4 for all items, though labels for response options vary by item. Items were summed to yield a total hazardous alcohol use score (α = .85).
Drug abuse symptoms
Drug abuse symptoms were measured using the Drug Abuse Screening Test (DAST-10; Skinner, 1982). Ten items assess involvement with drugs over the past year, including the misuse of prescription and over-the-counter drugs. Participants indicated their use (yes = 1, no = 0) of each drug listed. Items were summed to yield the total number of drug abuse symptoms (α = .73).
Analysis Approach
An exploratory factor analysis (EFA) was conducted on the 27 items that assess MIEs. The results of the EFA were also used to guide the creation of defining characteristic scores based on the follow-up questions regarding guilt, shame, etc., that were hypothesized to reflect defining MI characteristics for each of the factors determined by the EFA. Internal consistency was examined for both MIE factors and the associated defining characteristics. In addition, correlations were conducted to establish associations between the identified MIE factors, the hypothesized defining characteristics of MI associated with each MIE factor, and mental health outcomes (i.e., anxiety symptoms, depressive symptoms, and PTSD symptoms). Missing data were handled using analysis-specific pairwise deletion. The amount of missing data was negligible (i.e., 2 cases [<1%] or fewer per variable, with the majority of variables containing no missing data). The items for the defining characteristics of MI has systematic missingness deliberately built in by excluding individuals who endorsed “never” for any particular MIE as described below.
Results
Exploratory Factor Analysis
Bartlett’s (1954) test of sphericity was statistically significant (p < .001), suggesting that the MIE data were appropriate for factor analysis. Further, the Kaiser-Meyer-Olkin (Kaiser, 1974) measure of sampling adequacy (.95) indicated that the sample size was appropriate for factor analysis. Maximum likelihood extraction was used for the EFA because univariate normality was met for all items. Given the expected correlations among factors, an oblique (promax) rotation was used. The scree plot indicated a three-factor solution was most appropriate, whereas Velicer’s (1976) minimum average parcel (MAP) test indicated a four-factor solution accounted for the most systematic variance, and parallel analysis (both generated using SPSS code by O’Connor, 2000) suggested a five-factor solution accounted for more variance than random data. All three solutions (i.e., three-factor, four-factor, and five-factor solutions) were examined. However, the four-factor and five-factor models had a greater number of cross-loadings (i.e., factor loadings ≥ .32). Further, after dropping cross-loaded items, both the four and five factor model resulted in one or more factors with only two items. In addition, the four and five factor models accounted for little additional variance (3.98% and 3.10% for the fourth and fifth factors, respectively). Moreover, the three-factor model was theoretically interpretable. Results from the three-factor model are presented in Table 2. As recommended (Costellow & Osborne, 2005; Tabachnick & Fidell, 2001), items that cross-loaded above .32 (i.e., 5 items) were dropped from further analyses, yielding 22 items that assess MIEs across the three domains.
Table 2.
Item Loadings across Three Factors
| Item | Factor | ‘Never’ | Non-‘Never’ | |||
|---|---|---|---|---|---|---|
|
| ||||||
| 1 | 2 | 3 | M (SD) | N (%) | N (%) | |
| 7. I saw violations of rules of engagement | .69 | .04 | .04 | 1.93 (0.81) | 110 (33.5) |
216 (65.9) |
| 8. I was involved in violations of rules of engagement | .84 | −.07 | .05 | 1.71 (0.77) | 154 (47.0) |
174 (53.0) |
| 10. I was involved in the death(s) of an innocent in the war | .67 | .12 | .01 | 1.77 (0.82) | 146 (44.5) |
182 (55.5) |
| 11. I failed to save the life of someone in the war | .53 | .19 | .19 | 1.71 (0.84) | 172 (52.4) |
155 (47.3) |
| 15. I was involved in violence that was out of proportion to the event | .83 | .01 | −.04 | 1.79 (0.82) | 146 (44.5) |
181 (55.2) |
| 16. I saw the death(s) of children | .37 | .29 | .19 | 1.68 (0.84) | 178 (54.3) |
150 (45.7) |
| 17. I was involved in the death(s) of children | .99 | −.07 | −.23 | 1.73 (0.77) | 150 (45.7) |
178 (54.3) |
| 19. I was sexually assaulted | .93 | −.23 | −.06 | 1.80 (0.80) | 136 (41.5) |
191 (58.2) |
| 22. I saw a “friendly-fire” incident | .56 | .15 | .13 | 1.80 (0.87) | 149 (45.4) |
179 (54.6) |
| 23. I was involved in a “friendly-fire” incident | .90 | −.06 | −.01 | 1.72 (0.80) | 156 (47.6) |
170 (51.8) |
| 24. I destroyed civilian property unnecessarily during the war | .62 | .29 | −.19 | 1.80 (0.77) | 129 (39.3) |
198 (60.4) |
| 26. I made mistakes in the war zone that led to injury or death | .77 | .10 | −.16 | 1.75 (0.95) | 134 (40.9) |
192 (58.5) |
| 27. I came to realize during the war that I enjoyed violence | .64 | .02 | .06 | 1.84 (0.90) | 145 (44.2) |
183 (55.8) |
| 6. I had an encounter(s) with the enemy that made him/her seem more “human” and made my job more difficult | .03 | .41 | .29 | 1.96 (0.90) | 120 (36.6) |
208 (63.4) |
| 9. I saw the death(s) of an innocent in the war | −.01 | .86 | −.09 | 2.01 (0.82) | 97 (29.6) |
231 (70.4) |
| 13. I survived when others didn’t | .12 | .58 | −.04 | 2.00 (0.81) | 95 (29.0) |
233 (71.0) |
| 18. I experienced tragic warzone events that were chaotic and beyond my control | −.16 | .92 | .03 | 2.06 (0.91) | 99 (30.2) |
227 (69.2) |
| 21. I felt betrayed or let-down by trusted civilians during the war | .27 | .46 | −.05 | 1.94 (0.81) | 108 (32.9) |
220 (67.1) |
| 25. Seeing so much death has changed me | −.02 | .61 | .14 | 1.97 (0.95) | 127 (38.7) |
199 (60.7) |
| 1. Things I saw in the war left me feeling betrayed or let-down by military/political leaders | −.23 | −.07 | .97 | 2.15 (1.00) | 110 (33.5) |
218 (66.5) |
| 2. Things I experienced in the war left me feeling betrayed or let-down by military/political leaders | −.22 | −.01 | .95 | 2.11 (0.95) | 102 (31.1) |
225 (68.6) |
| 4. There were times in the war that I saw revenge/retribution for things that happened | .19 | .21 | .35 | 2.09 (0.87) | 88 (26.8) |
239 (72.9) |
| Deleted Items | ||||||
| 3. I did things in the war that betrayed my personal values | 1.98 (0.92) | 127 (38.7) |
200 (61.0) |
|||
| 5. There were times in the war that I engaged in revenge/retribution for things that happened | 1.78 (0.88) | 160 (48.8) |
168 (51.2) |
|||
| 12. I had to make decisions in the war at times when I didn’t know the right thing to do | 1.96 (0.87) | 120 (36.6) |
208 (63.4) |
|||
| 14. I saw violence that was out of proportion to the event | 1.82 (0.90) | 154 (47.0) |
174 (53.0) |
|||
| 20. I sometimes treated civilians more harshly than was necessary | 1.91 (0.82) | 114 (34.8) |
214 (65.2) |
|||
Note. Factor 1 = [Atrocities of war], Factor 2 = [Psychological consequences of war], and Factor 3 = [Leadership failure or betrayal]. The 22 items that comprise the three-factor model are presented here, with five items dropped due to cross-loadings.
The three factors accounted for 62.59% of the variance in the items. Factor 1, Atrocities of war, consists of 13 items that capture death and extreme acts of violence or cruelty associated with war (e.g., “I saw the death(s) of children”). This factor (eigenvalue = 12.93) explained 47.90% of the variance. Factor 2, Psychological consequences of war, consists of six items that assess cognitive and emotional changes through changing world views or meaning-making (e.g., “Seeing so much death has changed me”). This factor (eigenvalue = 2.72) accounted for an additional 10.07% of the variance in the items. Factor 3, named Leadership failure or betrayal consists of three items that measure being let down or betrayed by those with authority (e.g., “Things I experienced in the war left me feeling betrayed or let-down by military/political leaders”). This factor (eigenvalue = 1.25) accounted for an additional 4.63% of the variance.
The three-factor findings for the current modified scale are in contrast to the original unidimensional structure of the MIQ-M. This may, in part, be due to splitting apart witnessing versus engaging in events that are potential MIEs. Of note, four of the seven item pairs that were split to acknowledge witnessing versus participating in events loaded on the same factors. Three pairs (i.e., ‘violations of rules of engagement’, ‘death[s] of children’, and ‘friendly-fire incident[s]’) loaded onto Factor 1, Atrocities of war, and one pair (i.e., ‘feeling betrayed or letdown by military/political leaders’) loaded onto Factor 3, Leadership failure or betrayal. One pair was split across factors; although involvement in ‘the death(s) of an innocent in the war’ loaded onto Factor 1, witnessing ‘the death(s) of an innocent in the war’ loaded onto Factor 2, Psychological consequences of war. Finally, two pairs had an item that was not included in the final scale (i.e., engaging in ‘revenge/retribution’ and witnessing ‘violence that was out of proportion to the event’ were dropped for cross-loading on multiple factors). The remaining items loaded on Factor 1 (involvement in ‘violence that was out of proportion to the event’), and Factor 3 (i.e., witnessing ‘revenge/retribution for things that happened’).
Reliability and Validity of the Factors
From the modified MIQ-M, three MIE scores were created that correspond to the three MIE factors: Atrocities of war (13 items), Psychological consequences of war (6 items), and Leadership failure or betrayal (3 items). These scores represented the mean for the 13, 6, and 3 items that assessed each of the MIE factors. Next, a score was created for MI defining characteristics (e.g., guilt, shame, etc.) for each of the three MIE factors. That is, a mean score was calculated based on the frequency with which participants experienced guilt, shame, difficulty forgiving self, difficulty forgiving others, and withdrawn behaviors for relevant MIEs within each of the three MIE factors (i.e., Atrocities of war, Psychological consequences of war, and Leadership failure or betrayal). One score was created for each factor for the combination of defining characteristics. For example, because Atrocities of war contained 13 MIE items, and each MIE item was followed by 5 items assessing defining characteristics of MI, the defining characteristics score for Atrocities of war reflects the mean of the associated 65 defining characteristics items (or 13*5). However, MIEs that the participant indicated they did not experience (by endorsing ‘never’) were excluded from this calculation (see Table 2 for a list of how many participants selected ‘never’ for each MIE). Thus, if participants only experienced 10 of the 13 Atrocities of War MIE items, the defining characteristics score reflected the mean of the associated 50 defining characteristic items. This score reflected the guilt, shame, difficulty forgiving self, difficulty forgiving others, and withdrawn behaviors reported by participants for the relevant MIEs the participant experienced associated with Atrocities of war. An overall defining characteristics score was used rather than individual indices due to the strong associations among MI characteristics. For Factor 1, correlations among guilt, shame, difficulty forgiving self, difficulty forgiving others, and withdrawal ranged from r = .86 to .95. For Factor 2, correlations ranged from r =.79 to .92. For Factor 3, correlations ranged from r =.67 to .83. These correlations indicated strong multicollinearity among defining characteristics of MI, and supported their treatment as one component.
Cronbach’s alphas indicated strong reliability for the MIE items that assess each of the three factors (Factor 1 [Atrocities of war]: α = .95, Factor 2 [Psychological consequences of war]: α = .85, and Factor 3 [Leadership failure or betrayal]: α = .78) as well as defining characteristics of MI scores for each of the three factors (Factor 1 [Atrocities of war]: α = .92, Factor 2 [Psychological consequences of war]; α = .92, and Factor 3 [Leadership failure or betrayal]: α = .88). As seen in Table 3, the three factors associated with MIEs had moderate to large correlations (.36 to .70) with one another, demonstrating related yet distinct domains. The defining characteristic scores had larger correlations (.65 to .90) with one another, suggesting the defining characteristics of moral injury are strongly related, possibly supporting the use of a single defining characteristics score across all factors (α = .94). Similarly, each defining characteristic of the MI score was strongly correlated with the associated MIE factor (Factor 1 [Atrocities of war]: r = .41, Factor 2 [Psychological consequences of war]; r = .59, and Factor 3 [Leadership failure or betrayal]: r = .51), and each MIE factor had strong correlations with the overall characteristics of MI score (.50 to .55). Moreover, MIE factors and defining characteristics of MI factors were moderately correlated with symptoms of anxiety (.31 to .55), depression (.33 to .53), and PTSD (.44 to .67). However, there were varying correlations with hazardous alcohol use (.21 to .73) and drug abuse symptoms (.00 to .55). Taken together, the MIE factors identified and defining characteristic scores were associated with, but distinct from, mental health outcomes. Moreover, select factors had much stronger associations with substance use than others, indicating differential relationships (e.g., stronger associations between Factor 1 and substance use [.55 to .73], weaker associations between Factor 3 and substance use [.00 to .21], and moderate associations for Factor 2 [.29 to .50]), and supporting the examination of separate factors.
Table 3.
Correlations among Study Variables
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Moral Injury AoW MIEs | – | |||||||||||
| 2. Moral Injury PCoW MIEs | .70* | – | ||||||||||
| 3. Moral Injury LFB MIEs | .36* | .56* | – | |||||||||
| 4. Moral Injury AoW Defining Characteristics | .41* | .34* | .51* | – | ||||||||
| 5. Moral Injury PCoW Defining Characteristics | .59* | .59* | .56* | .90* | – | |||||||
| 6. Moral Injury LFB Defining Characteristics | .52* | .46* | .51* | .65* | .73* | – | ||||||
| 7. Moral Injury all Defining Characteristics | .54* | .50* | .55* | .93* | .96* | .86* | – | |||||
| 8. Depressive Symptoms | .48* | .40* | .33* | .40* | .51* | .53* | .53* | – | ||||
| 9. Anxiety Symptoms | .32* | .31* | .41* | .47* | .53* | .53* | .55* | .67* | – | |||
| 10. PTSD Symptoms | .54* | .52* | .44* | .53* | .67* | .67* | .67* | .75* | .77* | – | ||
| 11. Hazardous Alcohol Use | .73* | .50* | .21* | .31* | .46* | .42* | .40* | .49* | .40* | .55* | – | |
| 12. Drug Abuse Symptoms | .55* | .29* | .00 | .03 | .21* | .27* | .22* | .34* | .06 | .29* | .50* | – |
| Mean | 1.77 | 1.99 | 2.12 | 2.21 | 2.14 | 2.12 | 2.11 | 12.14 | 37.12 | 32.63 | 12.83 | 2.92 |
| Standard Deviation | 0.63 | 0.66 | 0.78 | 0.67 | 0.66 | 0.67 | 0.66 | 5.84 | 11.49 | 19.35 | 8.79 | 2.38 |
Note. AoW = Atrocities of war, PCoW = Psychological consequences of war, LFB = Leadership failure or betrayal, and PTSD = post-traumatic stress disorder. All correlations are significant at p < .001
Finally, the comparisons among factors may be clearest visually. As seen in Figure 1, participants reported experiencing more MIEs and defining characteristics of MI (e.g., guilt, shame, etc.) for Factor 3 (Leadership failure or betrayal), followed by Factor 2 (Psychological consequences of war), with the lowest ratings for Factor 1 (Atrocities of war). In Figure 2, the sample has been split into low versus high MI for each factor, separately for MIEs as compared to defining characteristics of MI. Participants were split into high versus low using the mean of that factor for the current sample (see Table 2 for means). Each panel displays the mean levels for symptoms of depression, anxiety, and PTSD, respectively, for individuals high or low in each moral injury factor. In each case, more mental health symptoms were observed for the groups higher on moral injury. Discrepancies appear to be greatest when the split is dependent on defining characteristics of MI (i.e., individuals high on defining characteristics also reported the highest levels of depression, anxiety, and PTSD symptoms, whereas individuals low on defining characteristics of MI also reported the lowest levels of depression, anxiety, and PTSD symptoms). There are also noticeable differences among the factors for MIEs, with the smallest differences among symptoms of depression and PTSD observed for Factor 3 (Leadership failure or betrayal). These figures display how trends for moral injury may be similar, but distinct, associations that can be observed by factor, and for events versus defining characteristics.
Figure 1.

Means of MIE scores by factor (panel a) and MI defining characteristics scores by factor (panel b). Error bars represent the standard error of the mean. Defining characteristics are a combination of guilt, shame, difficulty forgiving self or others, and withdrawal. MIE = moral injury events, AoW = atrocities of war, PCW = psychological consequences of war, and LFB = leadership failure or betrayal.
Figure 2.
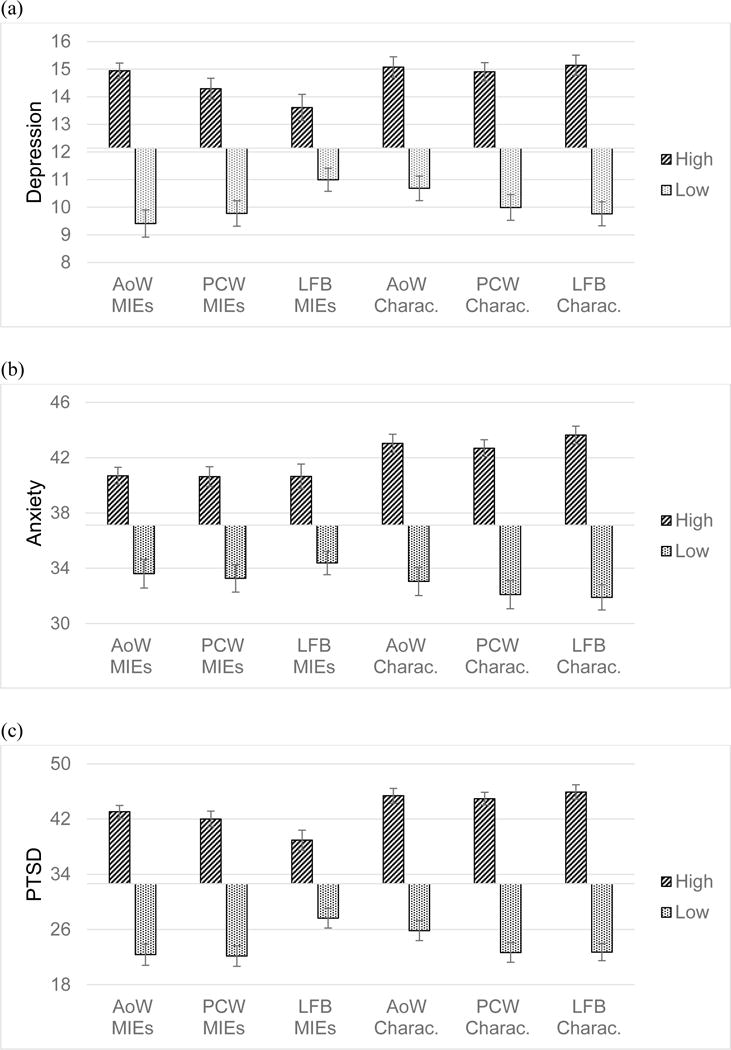
Means for symptoms of depression (panel a), anxiety (panel b), and PTSD (panel c) by moral injury factor. Note that participants have been split into high versus low on each factor using the mean of that factor for the current sample. The x-axis for each panel is placed at the mean for each outcome (depression M = 12.14 for panel a, anxiety M = 37.12 for panel b, PTSD M = 32.63 for panel c). Error bars represent the standard error of the mean. PTSD = posttraumatic stress disorder, MIE = moral injury events, Charac. = defining characteristics of moral injury (i.e., guilt, shame, difficulty forgiving self or others, withdrawal), AoW = atrocities of war, PCW = psychological consequences of war, and LFB = leadership failure or betrayal.
Discussion
The present study: a) tested the factor structure of a modified version (Robbins et al., 2017) of the MIQ-M (Currier et al., 2015) and, b) examined associations among MIEs, the defining characteristics of MI, and symptoms of depression, anxiety, and PTSD among a community sample of military personnel. MI characterizes exposure to morally ambiguous and ethically challenging events that conflict with an individual’s moral beliefs and ideals about the value of life. Despite a growing awareness of MI (Frankfurt & Frazier, 2016; Jinkerson, 2016; Maguen & Litz, 2012) and its associations with negative outcomes such as depression (Litz, et al., 2009), better measurement of MI is needed. From this vantage, the present study had three aims. First, we factor analyzed a slightly modified version (Robbins et al., 2017) of the Moral Injury Questionnaire – Military version (Currier, Holland, Drescher et al., 2015). Second, we tested the degree to which the identified MIE factors were associated with defining characteristics of MI (e.g., guilt, shame). Third, we examined correlations between the identified MI factors and symptoms of depression, anxiety, and PTSD. Although Currier and colleagues (2015) found the original MIQ-M to be unidimensional, results of the current study, in which the MIE-Q was modified and expanded, demonstrate the modified MIQ-M is best understood as a three-factor model consisting of Atrocities of war, Psychological consequences of war, and Leadership failure or betrayal.
Modified MIQ-M Factors
In this predominantly veteran community sample, results of the exploratory factor analyses of the modified MIQ-M demonstrated clear support for a MIE factor (i.e., Atrocities of war) that assesses direct and indirect exposure to extreme combat-related experiences such as those involving the death of children, noncombatants, or excessive violence. In addition, we found that being the victim of sexual assault significantly loaded with the Atrocities of war factor, suggesting the importance of non-combat events that may occur during deployments as an element of moral injury. The dimensionality found in the modified MIQ-M supports previous research suggesting that direct and indirect exposure to combat experiences involving the death of others or excessive violence may lead to especially deleterious mental health outcomes (Bryan & Cukrowicz, 2011; Litz et al., 2009; Maguen et al., 2010; Maguen & Litz, 2012). Our work supports previous MI research by demonstrating that MIEs that comprise Atrocities of war are associated with poor mental health outcomes among a community sample of military personnel.
Support was shown for a second MIE factor (i.e., Psychological consequences of war) that assesses both direct and indirect exposure to combat events that elicit cognitive and emotional changes (e.g., “I survived when others didn’t”, “I had an encounter(s) with the enemy that made him/her seem more ‘human’ and made my job more difficult”). This factor is consistent with previous research demonstrating the impact of trauma on larger meaning making systems (i.e., worldview, schemas; see Park, 2010 for a review). According to Park’s (2010) meaning-making model, when stressful or traumatic events violate global meaning systems (i.e., beliefs about the world, personal life goals, and feelings of purpose/meaning in life), distress or dissonance is elicited which initiates a process of meaning making in which people seek to resolve their problems and ameliorate negative emotions. The way individuals appraise trauma, including combat-related trauma, is a stronger predictor of distress than trauma exposure alone (Ehlers & Clark, 2000; Fairbrother & Rachman, 2006; Updegraff, Silver, & Holman, 2008). Additionally, the way an individual appraises their experience is further posited to significantly impact the development of MI such that global, internal, and stable attributions may result in greater MI (Litz et al., 2009). The positive association between this factor and poorer mental health outcomes is also consistent with empirical support in that exposure to MIEs was indirectly linked with PTSD, depression, and suicidality via the veterans’ ability to find meaning from their experiences (Currier, Holland, & Malott, 2015).
A third MIE factor (i.e., Leadership failure or betrayal) emerged, consisting of direct and indirect experiences of betrayal. This finding supports previous qualitative research suggesting that betrayal in the context of military operations, including failures of leadership and within-rank violence, contribute to moral injury (Drescher et al., 2011; Vargas, Hanson, Kraus, Drescher, & Foy, 2013). Within-unit trust is especially important in the context of warzone operations, which demand immediate obedience and performance of highly practiced orders (e.g., firing orders, damage control). If orders are issued and executed outside of the accepted rules of engagement (e.g., firing upon non-combatants or allied troops), the military member may not only lose trust in their leadership, but may also develop altered global beliefs about their own worth and goodness, ultimately viewing the self as immoral (Litz et al., 2009; Shay, 2002). Shay (2002) suggests that service members are less likely to experience combat-related psychological symptoms and moral injury when they trust both their peers and senior leadership to make ethically sound warzone decisions. This hypothesis is supported by research indicating that self-reports of strong, positive unit cohesion are significantly associated with lower rates of PTSD, depression, and stress-related declines in subjective well-being among recent-era service members (Armistead-Jehle, Johnston, Wade, & Ecklund, 2011; Griffith, 2002). Our work supports the proposed relationships between betrayal, moral injury, and mental health by demonstrating that MIEs that comprise Leadership failure or betrayal are associated with higher anxiety symptoms, depressive symptoms, and PTSD symptoms among a community sample of military personnel.
Moral Injury Defining Characteristics
While the field is beginning to gain an empirical understanding of MI, including multiple measures of MIEs, a major limitation is the lack of a validated measure of the defining characteristics of MI. To address this limitation, items assessing defining characteristics of MI (i.e., guilt, shame, difficulties with forgiving self, difficulties forgiving others, and withdrawal), based on Litz and colleagues’ (2009) model, were added to each MIE item in the modified MIQ-M (Currier, Holland, Drescher et al., 2015; Robbins et al., 2017). Defining characteristic scores in the current sample had strong reliability and were highly correlated across MIE factors. The current findings provide preliminary empirical support that the defining characteristics of MI, as measured by the modified MIQ-M, are highly overlapping. It will be important for future studies to determine whether the degree to which this overlap is due to measurement choices (e.g., similar wording for each item, relating each question to the preceding MIE could be probing general distress rather than distinguishing between specific feelings of guilt versus shame, etc.) or in fact that the defining characteristics of MI truly are highly related. Moreover, it may be due to the fact that participants cannot differentiate the guilt they feel from a single event from the guilt they feel from another event. They may be experiencing guilt, shame, etc., more globally in response to all MIEs rather than being able to extricate one MIE from another.
Both exposure to MIEs and the defining characteristics of MI (e.g., guilt, shame, etc.) were moderately correlated with symptoms of anxiety, depression, and PTSD, such that more MIE exposure and associated characteristics were associated with worse mental health symptoms. These findings reinforce that both exposure to these types of MIEs and the subsequent development of the defining characteristics of MI may have an important and wide-reaching impact on military members’ well-being. In fact, defining characteristics of MI had stronger correlations with mental health symptoms than did MIEs (Table 2), and split sample plots showed greater discrepancies among those higher versus lower in defining characteristics as compared to events (Figure 2). Additionally, mental health conditions, such as PTSD and depression, have a high rate of co-occurrence or comorbidity (Stander, Thomsen, & Highfill-McRoy, 2014). It is also important that future research examine whether MI may have distinct outcomes for mental health outcomes above that of combat exposure alone, and so forth.
Clinical Implications
Despite the increased empirical attention on moral injury, many mental health providers, particularly those working outside the U.S. Department of Veterans Affairs and Department of Defense, may be unaware of MI. Given the present findings, the modified MIQ-M could be used to extend current clinical assessment practices by expanding the utility of the original MIQ-M as a potential clinical instrument to produce the first simultaneous assessment of both MIE exposure and endorsement of defining characteristics of MI. A comprehensive measure encompassing both exposure and defining characteristics of MI could be used to guide the therapeutic process in important ways. Specifically, in the context of addressing combat trauma, clinicians need to be aware of the association between MIEs and presentation of related characteristics in order to develop an accurate understanding of the underlying etiology and to determine best treatment practices. The modified MIQ-M may be helpful as a screening measure. Mental health providers and others who work with these veterans (e.g., chaplains, members of the clergy) should conduct a more thorough interview to better understand exposure to MIEs, defining characteristics of MI, and ascertain the fundamental experiences and potential mechanisms that may be associated with mental health problems.
Limitations and Future Research
Methodological limitations of this study must be noted. First, this was a cross-sectional design, which prohibits the investigation of temporal relationships between exposure to MIEs, defining characteristics of MI, and other mental health concerns (i.e., symptoms of PTSD, anxiety, and depression). Longitudinal research design is an important next step to understanding the complex nature of MI. Second, there were limitations regarding the sample. We are unable to establish a rate of return for the survey; participants were recruited largely via remote marketing (e.g., online advertisements and paper flyers), making it impossible to determine how many potential participants heard about the study but chose not to participate. We also neglected to assess branch for National Guard and Reserves participants, and the current sample is fairly well educated, making replication critical. As a third issue, all data were collected via self-report and, although anonymity was assured, given the sensitive nature of the questions, participants may have been less likely to provide accurate information about violating rules of engagement, committing atrocities or other possible MIEs due to feelings of guilt/shame and/or fears of possible legal ramifications. In addition, participants retrospectively reported on MIEs, which may be subject to memory biases.
To address these limitations, replications with large-scale military groups are needed. These replications should focus on replicating the three-factor solution found in the current study, the strong correlations among factors and similar associations with mental health outcomes highlight the challenge of moral injury assessment. In addition, future research needs to be conducted within deployed environments in order to examine accounts of MIEs in real time. Research within deployed environments would also provide valuable information on the progressive development of MI. Further, the present study examined a community sample of veterans, National Guard/Reservists, and active duty members. Important differences may exist between community-based and clinical samples (Gahm, Lucenko, Retzlaff, & Fukuda, 2007). Future research would also benefit from evaluating the psychometric properties of the modified MIQ-M within a clinical setting.
In addition, the definition of MIEs developed by Litz et al. (2009) was used in the present study. A key part of the Litz et al. (2009) model of MI is appraisal or reflection of MIEs. Given that Factor 2 captures a broad range of experiences during war and reflection on these events, it may be important to broaden the definition of moral injury slightly to better reflect contemplation of MIEs. Importantly, studies such as the current examination may help inform the definition of MI.
Although the current investigation into the modified MIQ-M focused on defining characteristics of moral injury as suggested by Litz and colleagues (2009), additional models of MI (see Jinkerson’s [2016] syndrome model) have conceptualized loss of trust and spiritual/existential crisis (i.e., lower meaning in life) as other defining MI characteristics. Future research is needed to examine these other proposed defining characteristics as well as examine the delineation between primary and secondary manifestations of MI (see Litz et al., 2009 for a discussion). Finally, defining characteristics of MI were assessed for each MIE, regardless of level of endorsement for that specific experience. Data exploration indicates that participants did occasionally select a higher value for the symptom, even after indicating they never experienced the MIE. Participants may have been responding to characteristic items more globally. Future research should consider assessing the defining characteristics of MI referring to the totality of MIEs or each MIE domain, particularly in light of their strong associations. As discussed above, participants may have trouble extricating the guilt shame, etc., they feel from a single MIE as opposed to their global experience of MIEs. It is also possible the strength of the associations among defining characteristics of MI may diminish if assessed in a different way (i.e., in totality or via domain rather than in reference to each specific MIE). The current paper is a psychometric examination into modifying an existing scale (the MIQ-M) to incorporate defining characteristics of MI, and to explore domains of MIEs. It is a step forward in MI assessment, but future research should focus on the creation of a new scale to assess MI (both MIEs and defining characteristics, simultaneously). This would involve exploration into whether additional defining characteristics should be included (e.g., loss of trust, meaning in life), and if they can be linked to an individual MIE or are more representative of a global experience of MIEs.
Conclusions
The current investigation provides empirical support for the modified MIQ-M as a three-dimensional measure of MIEs, with strong associations with defining characteristics of MI (i.e., guilt, shame, difficulty forgiving self, difficulty forgiving others, and withdrawn behaviors). The three dimensions (Atrocities of war, Psychological consequences of war, and Leadership failure or betrayal) were associated with common mental health problems among military members (i.e., symptoms of depression, anxiety, and PTSD), consistent with previous research (Currier, Holland, Drescher, et al., 2015; Dennis et al., 2016; Monteith et al., 2016) and theoretical models (Jinkerson, 2016; Litz et al., 2009). The modified MIQ-M may help clinicians working with members of the military screen for MIEs as well as defining characteristics of MI.
Acknowledgments
This work was supported by a grant from the American Psychological Association to Michelle L. Kelley from the Society for Military Psychology (Division 19). Abby L. Braitman is supported by a research career development award (K01-AA023849) from the National Institute on Alcohol Abuse and Alcoholism (NIAAA). Adrian J. Bravo is supported by a training grant (T32-AA018108) from NIAAA.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th. Arlington, VA: American Psychiatric Publishing; 2013. [Google Scholar]
- Armistead-Jehle P, Johnston SL, Wade NG, Ecklund CJ. Posttraumatic stress in US Marines: The role of unit cohesion and combat exposure. Journal of Counseling & Development. 2011;89:81–88. doi: 10.1002/j.1556-6678.2011.tb00063.x. [DOI] [Google Scholar]
- Babor TF, De La Fuente JR, Saunders JB, Grant M. AUDIT—The Alcohol Use Disorders Identification Test: Guidelines for Use in Primary Health Care, Second edition. Geneva, Switzerland: World Health Organization; 2001. [Google Scholar]
- Bartlett MS. A note on the multiplying factors for various χ2 approximations. Journal of the Royal Statistical Society: Series B. 1954;16:296–298. [Google Scholar]
- Blevins CA, Weathers FW, Davis MT, Witte TK, Domino JL. The posttraumatic stress disorder checklist for DSM-5 (PCL-5): Development and initial psychometric evaluation. Journal of Traumatic Stress. 2015;28:489–498. doi: 10.1002/jts.22059. [DOI] [PubMed] [Google Scholar]
- Boisvert JA, McCreary DR, Wright KD, Asmundson GJG. Factorial validity of the Center for Epidemiologic Studies-Depression (CES-D) scale in military peacekeepers. Depression and Anxiety. 2003;17:19–25. doi: 10.1002/da.10080. [DOI] [PubMed] [Google Scholar]
- Bovin MJ, Marx BP, Weathers FW, Gallagher MW, Rodriguez P, Schnurr PP, Keane TM. Psychometric properties of the PTSD Checklist for Diagnostic and Statistical Manual of Mental Disorders–Fifth Edition (PCL-5) in veterans. Psychological Assessment. 2015;28:1379–1391. doi: 10.1037/pas0000254. [DOI] [PubMed] [Google Scholar]
- Bryan CJ, Cukrowicz KC. Associations between types of combat violence and the acquired capability for suicide. Suicide and Life-Threatening Behavior. 2011;41:126–136. doi: 10.1111/j.1943-278X.2011.00023.x. [DOI] [PubMed] [Google Scholar]
- Buechner B, Jinkerson J. Are moral injury and PTSD distinct syndromes?: Conceptual differences and clinical implications. In: Guilarte M, Buechner B, editors. Veteran and Family Reintegration. Santa Barbara, CA: Fielding Graduate University; 2016. pp. 47–79. [Google Scholar]
- Costello AB, Osborne JW. Best practices in exploratory factor analysis: Four recommendations for getting the most from your analysis. Practical Assessment Research & Evaluation. 2005;10(7):1–9. [Google Scholar]
- Currier JM, Holland JM, Drescher K, Foy D. Initial psychometric evaluation of the Moral Injury Questionnaire—Military version. Clinical Psychology & Psychotherapy. 2015;22:54–63. doi: 10.1002/cpp.1866. [DOI] [PubMed] [Google Scholar]
- Currier JM, Holland JM, Malott J. Moral injury, meaning making, and mental health in returning veterans. Journal of Clinical Psychology. 2015;71:229–240. doi: 10.1002/jclp.22134. [DOI] [PubMed] [Google Scholar]
- Dennis PA, Dennis NM, Van Voorhees EE, Calhoun PS, Dennis MF, Beckham JC. Moral transgression during the Vietnam War: A path analysis of the psychological impact of veterans’ involvement in wartime atrocities. Anxiety, Stress, & Coping. 2016;30(2):188–201. doi: 10.1080/10615806.2016.1230669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drescher KD, Foy DW, Kelly C, Leshner A, Schultz K, Litz B. An exploration of the viability and usefulness of the construct of moral injury in war veterans. Traumatology. 2011;17:8–13. doi: 10.1177/1534765610395615. [DOI] [Google Scholar]
- Ehlers A, Clark DM. A cognitive model of posttraumatic stress disorder. Behaviour Research and Therapy. 2000;38:319–345. doi: 10.1016/S0005-7967(99)00123-0. [DOI] [PubMed] [Google Scholar]
- Elhai JD, Contractor AA, Palmieri PA, Forbes D, Richardson JD. Exploring the relationship between underlying dimensions of posttraumatic stress disorder and depression in a national, trauma-exposed military sample. Journal of Affective Disorders. 2011;133(3):477–480. doi: 10.1016/j.jad.2011.04.035. [DOI] [PubMed] [Google Scholar]
- Fairbrother N, Rachman S. PTSD in victims of sexual assault: test of a major component of the Ehlers–Clark theory. Journal of Behavior Therapy and Experimental Psychiatry. 2006;37:74–93. doi: 10.1016/j.jbtep.2004.08.004. [DOI] [PubMed] [Google Scholar]
- Farnsworth J, Drescher K, Nieuwsma J, Walser R, Currier J. The role of moral emotions in military trauma: Implications for the study and treatment of moral injury. Review of General Psychology. 2014;18:249–262. doi: 10.1037/gpr0000018. [DOI] [Google Scholar]
- Frankfurt S, Frazier P. A review of research on moral injury in combat veterans. Military Psychology. 2016;28:318–330. doi: 10.1037/mil0000132. [DOI] [Google Scholar]
- Gahm GA, Lucenko BA, Retzlaff P, Fukuda S. Relative impact of adverse events and screened symptoms of posttraumatic stress disorder and depression among active duty soldiers seeking mental health care. Journal of Clinical Psychology. 2007;63:199–211. doi: 10.1002/jclp.20330. [DOI] [PubMed] [Google Scholar]
- Griffith J. Multilevel analysis of cohesion’s relation to stress, well-being, identification, disintegration, and perceived combat readiness. Military Psychology. 2002;14:217–239. doi: 10.1207/S15327876MP1403_3. [DOI] [Google Scholar]
- Jinkerson JD. Defining and assessing moral injury: A syndrome perspective. Traumatology. 2016;22:122–130. doi: 10.1037/trm0000069. [DOI] [Google Scholar]
- Kaiser HF. An index of factorial simplicity. Psychometrika. 1974;39:31–36. doi: 10.1007/BF02291575. [DOI] [Google Scholar]
- Kelley ML, Hock E, Jarvis MS, Smith KM, Gaffney MA, Bonney JF. Psychological adjustment of Navy mothers experiencing deployment. Military Psychology. 2002;14:199–216. doi: 10.1207/S15327876MP1403_2. [DOI] [Google Scholar]
- Kohout FJ, Berkman LF, Evans DA, Cornoni-Huntley J. Two shorter forms of the CES-D depression symptoms index. Journal of Aging and Health. 1993;5(2):179–193. doi: 10.1177/089826439300500202. [DOI] [PubMed] [Google Scholar]
- Kremen AM. Depressive tendencies and susceptibility to anxiety: Differential personality correlates. Journal of Personality. 1996;64:209–242. doi: 10.1111/j.1467-6494.1996.tb00820.x. [DOI] [PubMed] [Google Scholar]
- Litz BT, Stein N, Delaney E, Lebowitz L, Nash WP, Silva C, Maguen S. Moral injury and moral repair in war veterans: A preliminary model and intervention strategy. Clinical Psychology Review. 2009;29:695–706. doi: 10.1016/j.cpr.2009.07.003. [DOI] [PubMed] [Google Scholar]
- Maguen S, Litz B. Moral injury in veterans of war. PTSD Research Quarterly. 2012;23 Retrieved from: http://www.ptsd.va.gov/professional/newsletters/research-quarterly/v23n1.pdf. [Google Scholar]
- Maguen S, Lucenko BA, Reger MA, Gahm GA, Litz BT, Seal KH, Knight SJ, Marmar CR. The impact of reported direct and indirect killing on mental health symptoms in Iraq War veterans. Journal of Traumatic Stress. 2010;23:86–90. doi: 10.1002/jts.20434. [DOI] [PubMed] [Google Scholar]
- Monteith LL, Bahraini NH, Matarazzo BB, Soberay KA, Smith CP. Perceptions of institutional betrayal predict suicidal self-directed violence among veterans exposed to military sexual trauma. Journal of Clinical Psychology. 2016;72:743–755. doi: 10.1002/jclp.22292. [DOI] [PubMed] [Google Scholar]
- Nash WP, Litz BT. Moral injury: A mechanism for war-related psychological trauma in military family members. Clinical Child and Family Psychology Review. 2013;16:365–375. doi: 10.1007/s10567-013-0146-y. [DOI] [PubMed] [Google Scholar]
- Nash WP, Marino Carper TL, Mills MA, Au T, Goldsmith A, Litz B. Psychometric evaluation of the moral injury events scale. Military Medicine. 2013;178:646–652. doi: 10.7205/MILMED-D-I3-00017. [DOI] [PubMed] [Google Scholar]
- National Center for Veterans Analysis and Statistics. Educational attainment of veterans: 2000 to 2009. 2011 Retrieved from: https://www.va.gov/vetdata/docs/specialreports/education_final.pdf.
- O’Connor BP. SPSS and SAS programs for determining the number of components using parallel analysis and Velicer’s MAP test. Behavior Research Methods, Instruments, & Computers. 2000;32:396–402. doi: 10.3758/BF03200807. [DOI] [PubMed] [Google Scholar]
- Office of the Deputy Assistant Secretary of Defense. 2014 Demographics: Profile of the Military Community. Washington, DC: 2014. Retrieved from: http://download.militaryonesource.mil/12038/MOS/Reports/2014-Demographics-Report.pdf. [Google Scholar]
- Park CL. Making sense of the meaning literature: an integrative review of meaning making and its effects on adjustment to stressful life events. Psychological Bulletin. 2010;136:257–301. doi: 10.1037/a0018301. [DOI] [PubMed] [Google Scholar]
- Pitts BL, Chapman P, Safer MA, Unwin B, Figley C, Russell DW. Killing versus witnessing trauma: Implications for the Development of PTSD in combat medics. Military Psychology. 2014;25:537–544. doi: 10.1037/mil0000025. [DOI] [Google Scholar]
- Radloff LS. The CES-D scale a self-report depression scale for research in the general population. Applied psychological measurement. 1977;1(3):385–401. [Google Scholar]
- Robbins AT, Kelley ML, Hamrick HC, Bravo AJ, White TD. Modifying the Moral Injury Questionnaire: Including core symptomology; Poster presented at the annual meeting for the Association for Psychological Science; Boston, MA. 2017. [Google Scholar]
- Shay J. Odysseus in America: Combat trauma and the trials of homecoming. New York, NY: Scribner; 2002. [Google Scholar]
- Skinner HA. The Drug Abuse Screening Test. Addictive Behavior. 1982;7:363–371. doi: 10.1016/0306-4603(82)90005-3. [DOI] [PubMed] [Google Scholar]
- Stander VA, Thomsen CJ, Highfill-McRoy RM. Etiology of depression comorbidity in combat-related PTSD: A review of the literature. Clinical Psychology Review. 2014;34:87–98. doi: 10.1016/j.cpr.2013.12.002. [DOI] [PubMed] [Google Scholar]
- Tabachnick BG, Fidell LS. Using Multivariate Statistics. Boston: Allyn and Bacon; 2001. [Google Scholar]
- Updegraff JA, Silver RC, Holman EA. Searching for and finding meaning in collective trauma: Results from a national longitudinal study of the 9/11 terrorist attacks. Journal of Personality and Social Psychology. 2008;95:709–722. doi: 10.1037/0022-3514.95.3.709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Winkle EP, Safer MA. Killing versus witnessing in combat trauma and reports of PTSD symptoms and domestic violence. Journal of Traumatic Stress. 2011;24:197–110. doi: 10.1002/jts.20614. [DOI] [PubMed] [Google Scholar]
- Vargas A, Hanson T, Kraus D, Drescher KD, Foy DW. Moral injury themes in combat veterans’ narrative responses from the National Vietnam Veterans’ Readjustment Study (NVVRS) Traumatology. 2013;19:243–250. doi: 10.1177/1534765613476099. [DOI] [Google Scholar]
- Velicer WF. Determining the number of components from the matrix of partial correlations. Psychometrika. 1976;41:321–327. doi: 10.1007/BF02293557. [DOI] [Google Scholar]
- Weathers FW, Litz BT, Keane TM, Palmieri PA, Marx BP, Schnurr PP. The PTSD Checklist for DSM-5 (PCL-5) 2013 Retrieved from: http://www.ptsd.va.gov/professional/assessment/adult-sr/ptsd-checklist.asp.
- Wortmann JH, Jordan AH, Weathers FW, Resick PA, Dondanville KA, Hall-Clark B, Foa EB, Young-McCaughan S, Yarvis JS, Hembree EA, Mintz J, Peterson AL, Litz BT. Psychometric analysis of the PTSD Checklist-5 (PCL-5) among treatment-seeking military service members. Psychological Assessment. 2016;28:1392–1403. doi: 10.1037/pas0000260. [DOI] [PubMed] [Google Scholar]


