Widespread agreement exists in the transplant community that the disincentives facing kidney donors should be removed. The first step in this effort is to identify what these disincentives are and estimate their magnitude.
Four years ago, Klarenbach et al.1 made a valuable contribution to this effort. Analyzing living donor costs in Canada during the 2004–2008 period, they found that the average “workforce productivity cost” was C$6729. This included both time off from work for donation purposes for which the worker received no pay and time off from work for which the worker received sick pay, vacation pay, or employment insurance payments. The former is clearly a disincentive to kidney donation. However, part of the latter is also a disincentive, particularly the use of sick and vacation time/pay for kidney donation, because these could have been used for other purposes.
Much more importantly, the earlier study calculated the average “home productivity cost” by multiplying average wage rates by the time that donors were not able to perform household activities or care for dependents.1 The result was C$5521, which is an order of magnitude greater than the usual method of estimating these costs, i.e., by counting only out-of-pocket spending. The latter method seriously under estimates the disincentive facing donors/caregivers, because typically, (1) much of the burden of this care is assumed by nonremunerated caregivers, such as family members or friends; (2) the dependents may receive a decreased amount of care; and (3) the donor himself or herself may require care.
The sum of home and workforce average productivity costs in the 2014 study was C$12,250 in 2008 Canadian dollars. This is equivalent to US$12,735 in terms of the prices and standard of living of the United States in 2017, an amount much higher than what had previously been assumed for these costs.
In this issue of the Journal of the American Society of Nephrology, Klarenbach et al.2 have expanded and updated the earlier analysis using a much larger sample of living kidney donors (821 versus 100) during the 2009–2014 period. The current study broadly confirms the results of the earlier study, calculating that the sum of the two average productivity costs was C$11,849 in 2016 Canadian dollars, which is equivalent to US$10,816 in 2017.
There is widespread agreement in the transplant community that these two disincentives as well as the other disincentives facing living kidney donors should be removed. This is true for two reasons: (1) simple fairness to donors and (2) it would increase the supply of donated kidneys and thus reduce the number of patients prematurely dying from ESRD.
With regard to the second reason, the death toll from ESRD is very high in large part because of the severe shortage of transplant kidneys. Roughly speaking (all variables may not occur in exactly the same year), the incidence of treated ESRD is currently, about 126,000 patients per year, but only about 31,000 (25%) are added to the waiting list for a kidney from a deceased donor (Table 1). Moreover, only 20,000 (16%) actually receive a transplant kidney, of which 14,000 (11%) are from deceased donors and 6000 (5%) are from living donors. The approximately 106,000 (84%) who do not receive a transplant are fated to live an average of 5 years on dialysis therapy before dying prematurely.
Table 1.
Outcomes for US patients with ESRD (per year)
| Percent | ||
|---|---|---|
| Diagnosed with ESRD | 126,000 | 100 |
| Added to waiting list | 31,000 | 25 |
| Received a transplant | 20,000 | 16 |
| From a deceased donor | 14,000 | 11 |
| From a living donor | 6000 | 5 |
| Receive dialysis therapy until premature death | 106,000 | 84 |
Data reflect yearly rates in the United States from ref. 3.
The 16% of patients with ESRD who receive a transplant kidney are the fortunate ones, because it enables them to live much longer and healthier lives. In economic terms, the value of a transplant to a patient on the waiting list is about $937,000.4 Moreover, under the current system in which compensation of kidney donors is prohibited, each transplant saves taxpayers about $146,000, because the total lifetime cost for treating a transplant patient is far less than the lifetime cost for a patient receiving dialysis therapy, and the government accounts for most of the spending on both. Thus, the government could afford to compensate a kidney donor up to $146,000 and still save money for taxpayers.
Most of the focus of concern in the transplant community has been on the 25% of patients with ESRD who are added to the kidney waiting list, particularly how many receive a transplant, die, or are removed from the list because they become too sick to transplant. Little attention has been paid to the 75% who are not added to the list. But it is common knowledge that many of these patients with ESRD would medically benefit from a transplant, and – if there was no kidney shortage – would be recommended for the waiting list, would be accepted by a transplant center, and would receive a transplant.
What percentage of patients with ESRD fall into this category? No one knows for certain. However, to see the full extent of the harm done by the kidney shortage and the potential benefit from ending it, let us assume that 50% of those who are diagnosed with ESRD could medically benefit from a transplant. (This assumption is consistent with the findings of Schold et al.5 that, if all of the patients on dialysis who have a life expectancy of >5 years were placed on the kidney waiting list, the number on the list would almost double.) Thus, half of the 126,000 patients who are currently diagnosed with ESRD each year—63,000 patients—might medically benefit from a transplant. However, if only 20,000 patients per year receive a transplant, the remaining 43,000 would join the growing toll of those who die prematurely because of the kidney shortage. To put this in perspective, this is the same death toll as from 85 fully loaded 747s crashing each year.
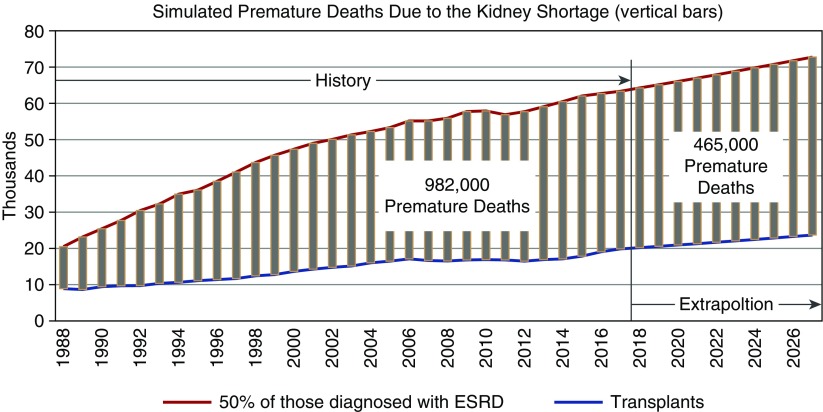
We can extend this grim logic from the current time back over the past 30 years for which we have data, as shown in Figure 1. The upper curve represents 50% of those diagnosed with ESRD each year, the lower curve indicates the annual number of transplants, and the vertical bars between the curves show the number of premature deaths each year. Summing over all the bars gives the cumulative premature death toll, which from 1988 to 2017 was a horrendous 982,000 (Figure 1). Additionally, if we extrapolate the trend in ESRD diagnoses and transplants over the past 10 years forward to the next 10 years, the death toll would increase by an additional 465,000.
Figure 1.
Estimates of the number of premature deaths due to the kidney shortage. The data suggesting that 50% of new patients with ESRD could benefit from a renal transplant allow an estimate of the number of premature deaths due to the kidney shortage. Numbers for incidence of ESRD and transplantation rates are from ref. 3.
Whatever the exact percentage of patients with ESRD who would medically benefit from a transplant, it is clear that the premature death toll from the kidney shortage is much larger than just those who die on the kidney transplant waiting list or are removed from it because they become too sick to transplant. It is also certainly large enough to motivate everyone in the transplant community to begin to reduce the kidney shortage by taking the first step—to which no one seems to object—removing the disincentives to kidney donation. That, in turn, would create the momentum to consider taking the next, somewhat controversial step to end the shortage, which is providing positive incentives to kidney donors.
We are aware that great progress is being made in producing synthetic organs through stem cell generation and three-dimensional printing. However, until the happy day arrives when such organs are readily available, we should address here and now the terrible premature death toll caused by the kidney shortage with a technology that is already available and proven—compensating donors for their kidneys. Any arguments against this approach (commodification, exploitation, etc.) must be weighed against this terrible death toll.
Disclosures
None.
Footnotes
Published online ahead of print. Publication date available at www.jasn.org.
See related article, “Financial Costs Incurred by Living Kidney Donors: A Prospective Cohort Study,” on pages 2847–2857.
References
- 1.Klarenbach S, Gill JS, Knoll G, Caulfield T, Boudville N, Prasad GV, et al. : Donor Nephrectomy Outcomes Research (DONOR) Network: Economic consequences incurred by living kidney donors: A Canadian multi-center prospective study. Am J Transplant 14: 916–922, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Klarenbach S, Przech S, Garg AX, Arnold JB, Barnieh L, et al. : Donor Nephrectomy Outcomes Research (DONOR) Network: Financial costs incurred by living kidney donors: A prospective cohort study. J Am Soc Nephrol 29: 2847–2857, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.U.S. Renal Data System (USRDS) 2017. Annual Data Report: Atlas of Chronic Kidney Disease and End-Stage Renal Disease in the United States, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, Bethesda, MD [Google Scholar]
- 4.Held PJ, McCormick F, Ojo A, Roberts JP: A cost-benefit analysis of government compensation of kidney donors. Am J Transplant 16: 877–885, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schold JD, Srinivas TR, Kayler LK, Meier-Kriesche HU: The overlapping risk profile between dialysis patients listed and not listed for renal transplantation. Am J Transplant 8: 58–68, 2008 [DOI] [PubMed] [Google Scholar]