A 39-year-old Caucasian man with a history of post-traumatic stress disorder sought medical care for intractable eye pain one day after he applied a tattoo to his right eye using a small-gauge needle. The patient had previously injected the left ocular surface without any complication approximately four years earlier. This time, his inferotemporal injection of green tattoo dye caused immediate pain, which then worsened to include headache, nausea, vomiting, photophobia, decreased vision, and periocular swelling over the next several hours. Past ocular history was significant for amblyopia of the left eye requiring patch therapy.
Best-corrected visual acuity in the emergency department was 20/60 in the right eye and 20/40 in the left. The right pupil was fixed and dilated at 6 mm while the left appeared normal, with no afferent pupillary defect present. This patient had extensive facial tattoos, including those of both upper eyelids. Intraocular pressure (IOP) was 20 mmHg in the right eye and 14 mmHg in the left. The conjunctiva of the right eye was chemotic and contained diffuse subconjunctival green pigmentation while his left eye conjunctiva appeared entirely black, but quiet [Figure 1A]. The right eye showed no signs of corneoscleral laceration or uveal prolapse. The anterior chamber was formed and contained moderate pigmented cells. A small amount of green ink was speckled across the posterior lens capsule. Diffuse green debris was present in the anterior vitreous and a large focal consolidation of green ink was visible in the inferior vitreous. No obvious retinal tear or detachment was visualized, but the view was partially obscured by the vitreous debris. Macular optical coherence tomography (OCT) showed no macular edema or detachment, though particles in the vitreous causing shadowing were noted.
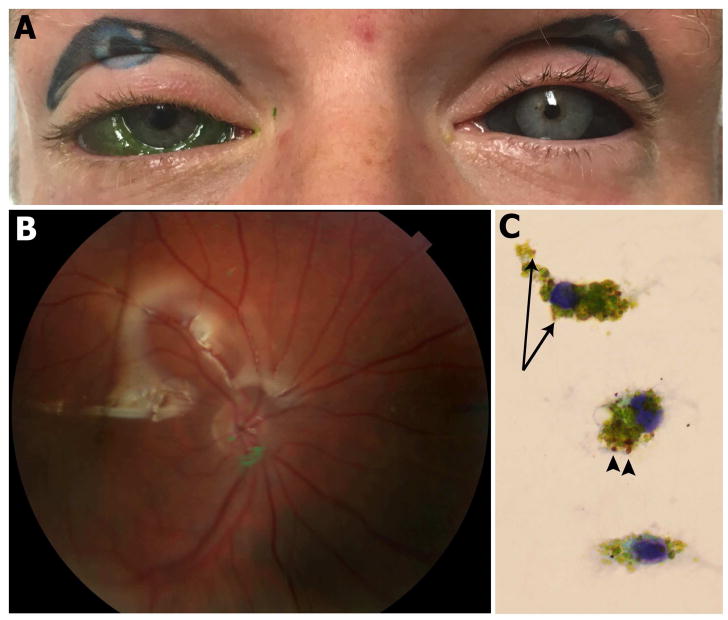
FIGURE 1. Subconjunctival tattoo and associated intraocular complications.
A. External photograph showing marked right-sided conjunctival chemosis following accidental globe penetration upon self-attempted subconjunctival injection of green tattoo ink. Bilateral upper eyelid and left ocular surface tattoos are also evident. B. Fundus photograph approximately 2 months after initial injection revealing persistent green ink overlying the optic nerve in the right eye. C. Photomicrograph of vitreous cytology obtained at the time of repeat vitrectomy and silicone oil removal procedure, revealing macrophages with abundant green-colored material in the cytoplasm, consistent with tattoo ink. Multiple reddish intracytoplasmic particles indicative of erythrocytic break-down products (arrowheads) and several golden-brown intracytoplasmic pigment particles indicative of hemosiderin (arrows) are also seen, consistent with prior vitreous hemorrhage (Pap stain, original magnification, x1000).
Given the presence of intraocular tattoo ink and our concern for progressive inflammation and toxicity as well as the possibility of a retinal tear or detachment, the patient agreed to urgent globe exploration and vitrectomy. During this procedure, after exposing the sclera (which remained unstained by the tattoo ink), we noted a green needle track 4mm from the limbus at the 7-o’clock position. Subsequent pars plana vitrectomy to remove the ink permitted a more detailed peripheral retinal exam and an inferior retinal break with a localized retinal detachment was discovered underneath the entry track. In addition, a mild inferior vitreous hemorrhage, superonasal choroidal detachment, and superotemporal serous subretinal fluid pocket were noted. Given the presence of a rhegmatogenous retinal detachment and our concerns that his exposure to an inflammatory stimulus would promote proliferative vitreoretinopathy, we employed extensive cerclage laser retinopexy of the vitreous base and silicone oil tamponade, after a full fluid-air exchange. Intravitreous injections of vancomycin (0.25 mg) and ceftazidime (0.5625 mg) were then given as a prophylactic measure.
Post-operatively, the patient’s visual acuity improved and his retina remained attached. Scattered green flecks of residual pigment were noted in the posterior pole on follow-up, most prominently around the optic nerve head [Figure 1B]. Three months following the initial injury, the patient was taken for repeat vitrectomy and silicone oil removal since his eye showed no signs of fibrosis or re-detachment. A sample of vitreous fluid containing residual ink was analyzed by cytology, revealing macrophages containing cytoplasmic green material and hemosiderin, consistent with his history of intravitreous tattoo ink and vitreous hemorrhage [Figure 1C].
At the patient’s most recent follow-up, approximately six months after his initial injury, his uncorrected Snellen visual acuity was 20/20-2 in the right eye and he had normal IOP. The conjunctiva remained tinted green. A faint amount of residual green particulate matter was present in the vitreous cavity, but macular OCT showed intact outer retinal architecture. Both a multi-focal and full-field electroretinogram at approximately 5 months post-operation were within normal limits, without evidence of either cone or rod dysfunction. Given the unknown long-term effects of intraocular tattoo ink, the patient will be followed indefinitely with periodic ophthalmologic examinations and serial electroretinograms to monitor for late-onset retinal toxicity.
Tattoo ink, by intent, is designed to permanently remain in place and resist degradation. Most tattoo inks are mixtures of solvents (carrier fluids such as ethanol, methanol, glycerol, or propylene glycol in sterile water) and pigments (often heavy metals, organic molecules, or carbon).1 Our patient used Radiant Colors Medium Green tattoo ink (Los Angeles, CA, USA), which contained sterile water, glycerol, isopropanol, and copper phthalocyanine (CI 74160 [Colour Index International]) and pigment yellow 74 (CI 11741). Long-term effects of ocular exposure to these pigments are unknown, but pure copper can cause retinal toxicity due to acute chalcosis, a potential cause of permanent vision loss.
Serious ocular sequelae can occur from subconjunctival tattooing, especially since it is usually performed by individuals who are not professionally trained in ocular surgery. Reported complications include anterior uveitis, secondary glaucoma, vitritis, proliferative vitreoretinopathy, and inadvertent globe penetration.2–3 To our knowledge, this case report is only the second showing intraocular cytopathology, which demonstrates persistent ink remnants engulfed by macrophages as well as intracytoplasmic erythrocytic particles from prior vitreous hemorrhage. This macrophage response is analogous to the previously reported histopathology seen in cutaneous tattoos in which the foreign pigment is engulfed by dermal macrophages, at times inciting a foreign-body granulomatous reaction.4 Poor visual outcomes are common when complications from subconjunctival tattooing occur. Accordingly, there have been efforts in several states to outlaw ocular tattooing and the person credited with its popularization has even disavowed the practice.5 Nevertheless, the practice of subconjunctival tattooing has spurred continued interest among tattoo artists and people seeking body modification, with some attempting the procedure themselves, as in this case. Ophthalmologists should be aware of the serious damage even minute amounts of tattoo ink can cause to the eye. Fortunately, because of prompt medical attention in this case, the tattoo ink was evacuated urgently. The patient avoided infectious and inflammatory complications and no significant visual impairment occurred. However, potential long-term visual sequelae may still be possible. If globe violation is suspected secondary to subconjunctival tattooing, we recommend prompt exploratory surgery and removal of the material in an operative setting.
Footnotes
Conflict of Interest: No conflicting relationship exists for any author
Financial Support: None
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Wood-Black F. Going Skin Deep: The Culture and Chemistry of Tattoos. [Accessed March 28, 2018];Going Skin Deep: The Culture and Chemistry of Tattoos - inChemistry. https://inchemistry.acs.org/content/inchemistry/en/atomic-news/tattoo-ink.html. Published February 1, 2017.
- 2.Cruz NFS, da Santos KS, Farah M, de L, Felberg S. Conjunctival Tattoo With Inadvertent Globe Penetration and Associated Complications. Cornea. 2017;36(5):625–627. doi: 10.1097/ICO.0000000000001163. [DOI] [PubMed] [Google Scholar]
- 3.Jalil A, Ivanova T, Bonshek R, Patton N. Unique case of eyeball tattooing leading to ocular penetration and intraocular tattoo pigment deposition. Clin Experiment Ophthalmol. 2015;43(6):594–596. doi: 10.1111/ceo.12501. [DOI] [PubMed] [Google Scholar]
- 4.Vagefi MR, Dragan L, Hughes SM, Klippenstein KA, Seiff SR, Woog JJ. Adverse reactions to permanent eyeliner tattoo. Ophthal Plast Reconstr Surg. 2006;22(1):48–51. doi: 10.1097/01.iop.0000196713.94608.29. [DOI] [PubMed] [Google Scholar]
- 5.Larratt S. The Eyeball Tattoo FAQ. [Accessed April 1, 2018];BME/News. https://news.bme.com/2012/10/18/the-eyeball-tattoo-faq/. Published October 18, 2012.