Abstract
BACKGROUND.
Childhood adversity has been shown to exert profound effects on basic psychological processes well into adulthood. Some of these processes, such as those related to reward and emotion, play critical roles in moral decision-making. As a population with high rates of childhood trauma as well as heterogenous clinical presentation, individuals with bipolar disorder (BD) constitute an enriched group in which to examine the correlates of trauma and other clinical variables with moral cognition.
METHODS.
62 euthymic BD patients and 27 controls responded to moral dilemma scenarios and completed the Childhood Trauma Questionnaire.
RESULTS.
Results revealed a main effect of diagnosis on moral decision-making only when both personal force and an intention were required, indicating a more utilitarian style in BD patients relative to controls. Several interesting patterns also emerged regardless of diagnostic status. Higher ratings of physical neglect were significantly associated with higher ratings of acceptability (a utilitarian tendency) across dilemma types, and a similar pattern was observed at the trend level for experiences of emotional neglect. Significant main effects on moral decision-making were also observed for sex, illness duration, and history of psychotic features in the BD sample.
LIMITATIONS.
The present study is limited by the self-reported nature of the CTQ and by the small number of trials of moral dilemmas. In addition, practical and clinical implications of the moral dilemmas paradigm are limited due to its abstract nature.
CONCLUSIONS.
Our results indicate that certain clinical features as well as childhood maltreatment (in particular neglect) may significantly impact moral decision making in adult life. Surprisingly, childhood trauma was associated with a more utilitarian style, which is in the opposite direction from previous effects shown in PTSD. Although speculative, our results suggest that there may be a protective quality associated with utilitarian moral decision-making tendencies.
Keywords: childhood trauma, bipolar disorder, moral dilemmas, moral decision-making
Introduction
Empirical investigations of moral psychology in the past 15 years have made substantial use of the theoretical framework known as the “dual process theory (DPT)”, proposed by Greene and colleagues (2004). DPT introduced a method to tease apart emotional and cognitive component processes in moral decision-making, known as the “moral dilemmas” paradigm. Moral dilemmas are short vignette-type scenarios which face the study participant with a difficult yes/no decision, in which both answers generally involve harm being caused to a person (or people). The most well-known scenario is the “trolley problem”, in which the reader must decide whether to prevent the deaths of five people about to be run over by a runaway trolley, but to do so, they must cause the death of a single person by pushing the person in front of the trolley. These dilemma-scenarios have proven a useful measure in psychological research in part due to their ability to delineate two types of neurocognitively-dissociable decision-making processes. These are known respectively as “utilitarian,” corresponding to a decision to maximize the positive outcomes by, for example, saving the five people, and “deontological,” corresponding to a decision that adheres to moral rules and duties, such as not to kill others, regardless of the consequences. It should be noted that this is a measure taken originally from literature in moral philosophy in which the terms “utilitarian” and “deontological” refer to complex views about the moral world, and when used in the context of psychological experiments, the terms are used rather in a looser fashion to refer simply to a cognitive tendency which aligns with characteristically “utilitarian” and “deontological” ideals. Findings in such work are never intended to demonstrate that research participants hold explicit, complex moral theories that account for their decisions.
Bipolar disorder (BD) is a major mood disorder that is characterized by both affective dysregulation (APA, 2013) and cognitive dysfunction (Burdick et al., 2014). These factors make BD of particular interest with regard to a dual-process approach to assessing moral decision-making (as both processes may be impaired by the illness), yet few studies have been conducted in this population. The limited past investigations of moral reasoning and moral emotions more generally in BD have found a number of differences between patients and HC participants. Epa, Czyzowska, Dudek, Siwek, & Gierowski (2014) found that patients with BD differ from HCs in their differential use of the 6 varieties of Kohlbergian moral reasoning (with BD tending to use the “less advanced” reasoning categories). Epa & Dudek, 2015 reviewed work regarding experience of negative moral emotions (i.e. shame and guilt) and report that patients with BD may have an increased tendency to experience these due to their proclivity for depressive symptomatology. Radaelli et al., (2013) found that depressed BD patients differed from HC in their neural activation patterns (largely in medial prefrontal cortex and anterior cingulate cortex) while engaging in a go-no/go task with morally-valenced words, suggesting a link between mood state and the processing of moral stimuli.
Only one study has used the moral dilemmas methodology in a BD sample (Kim et al., 2015). This study showed that manic mood state was associated with greater likelihood of utilitarian decisions (i.e. manic patients were more likely to respond “yes,” that it was acceptable to cause harm in order to maximize positive consequences). There were no significant differences between euthymic BD patients and healthy controls for any of the dilemma types, suggesting that diagnostic effects were state-dependent; however, the sample was small (n=26) and statistical power was thereby limited.
None of these extant studies took particularly fine-grained approaches to examining clinical variables which may be associated with moral cognition in bipolar illness, focusing instead on broad-stroke diagnostic differences. Childhood trauma is one such important clinical factor, which occurs comorbidly at high rates in BD (approximately 65%) (Aas et al., 2016) and is associated in BD with greater cognitive dysfunction (Jiménez et al., 2017), affective processing deficits (Russo et al., 2015), and an array of negative clinical outcomes (Aas et al., 2016).
Recent work has made important advances in uncovering the psychological mechanisms and neural underpinnings of the long-term effects of childhood trauma. One prospective study of adults who experienced childhood trauma found that participants showed differential brain activation during processing of reward and engaged in greater levels of risk-taking behaviors, both in laboratory and real-world measures (Birn, Roeber, & Pollak, 2017). Significant aberrations in emotional processing have also been associated with childhood adversity, for example in the context of perception of emotion in ‘outgroup’ individuals (Krautheim et al., 2018) as well as attentional avoidance of emotional stimuli during Stroop tasks (England-Mason, Khoury, Atkinson, Hall, & Gonzalez, 2018).
Many of the processes evidently modulated by experiences of childhood adversity are of central importance in generating judgments and behavior in the domain of morality. Studies of moral cognition and decision-making have found that affective and reward processes play integral roles (Decety, Michalska, & Kinzler, 2011; Delgado, Frank, & Phelps, 2005), as does processing related to ingroup and outgroup (Brambilla, Sacchi, Pagliaro, & Ellemers, 2013). This connection between basic processes effected by trauma and those responsible for moral cognition raises questions of whether childhood trauma may exert an influence on moral decision-making. In addition, a recent review showed that childhood trauma (especially childhood neglect) can strongly predict violent behavior in adulthood (Bland, Lambie, & Best, 2018), making it directly relevant to adult moral behavior and decision-making.
Therefore, the present study assessed the effects on moral decision-making of childhood trauma in 62 patients with BD, specifically during the affectively stable phase to expand upon previous work. Additionally, we evaluated clinical correlates of moral decision-making in BD (e.g. duration of illness, number of hospitalizations, history of childhood trauma), as these have, as yet, received limited attention. Although some investigations noted earlier found differences between HC and BD participants on responses to moral stimuli (Epa et al., 2014; Epa & Dudek, 2015; Radaelli et al., 2013), we hypothesized that, in line with findings from Kim et al., (2015), euthymic BD patients would not differ from HC on responses to moral dilemmas; however, as our sample is more than twice the size of prior work, we expected that we might detect more subtle differences that were not previously seen. Because of the comprehensive characterization of our sample, we were also able to evaluate the role that several clinical factors related to BD illness plays in moral decision-making. We hypothesized that history of childhood trauma would have a significant influence on moral dilemma performance.
Methods
Participants
Our sample included 62 patients with bipolar disorder (BD) and 27 healthy controls (HC), all recruited around New York City. Participants were enrolled in a broader study of neurocognitive heterogeneity in BD (R01MH100125 to KEB), approved by the Icahn School of Medicine at Mount Sinai IRB. Written informed consent was obtained from all study participants prior to enrollment. Inclusion criteria were: (1) a DSM-V diagnosis of either BD I or BD II, as confirmed using the SCID-V (First, Williams, Karg, & Spitzer, 2015), (2) current age of 18–65, (3) current euthymic mood state, defined as a score of 3 or less on the Clinical Global Impression for Bipolar Disorder (Spearing, Post, Leverich, Brandt, & Nolen, 1997). Healthy controls were included if they were age 18–65, had no Axis I disorder (as assessed by the non-patient version of the SCID-V), and had no first-degree relative with a history of an Axis I disorder. Exclusion criteria for both BD and HC participants included any history of central nervous system trauma, neurological disorder, any report of a past or present diagnosis of attention deficit hyperactivity disorder (ADHD), a diagnosis of substance use disorder within the past 3 months, or electroconvulsive therapy treatment within the past year. All subjects completed the Wide Range Achievement Test (WRAT) Reading subtest as an estimate of premorbid IQ (Wilkinson, 1993) and only subjects with an IQ>70 were included.
Clinical Assessment
In addition to the SCID-V, measurements of current mood symptoms were administered to both HC and BD participants at study visits. These included the Hamilton Rating Scale for Depression (Hamilton, 1960), and the Clinician Administered Rating Scale for Mania (CARS-M; Altman, Hedeker, Janicak, Peterson, & Davis, 1994). Total scores on the HRSD and the CARS-M indicate the severity of current depression and mania respectively. A history of childhood trauma was assessed using the Childhood Trauma Questionnaire (Bernstein et al., 1994). The CTQ measures the type and the severity of trauma experienced during childhood. The CTQ consists of 28 questions which comprise 5 subscales: Physical Abuse, Physical Neglect, Emotional Abuse, Emotional Neglect, and Sexual Abuse. Participants responded on a scale of 1 to 5, where 1 is “Never” and 5 is “Very Often”. Categorical variables were also computed for the presence or absence of “severe trauma” in each of the five domains, as in prior work (Russo et al., 2015).
Moral Dilemma Task
Our moral dilemmas were adapted from Greene et al (Greene et al., 2009), consisting of 4 scenarios that present the reader with a difficult decision about whether to sacrifice one person’s life in order to save the lives of five others (this type of scenario is sometimes known as a “sacrificial moral dilemma”). The nature of dilemmas was varied on dimensions of personal vs impersonal, and intentional vs unintentional. “Personal” and “impersonal” designations indicate the presence or absence of physical force being used in the scenario. “Intentional” dilemma types are characterized by an action that functions directly as the means to save the five people (e.g. pushing someone in front of a moving trolley so that their death directly results in the saving of five others who would have been hit), while an “unintentional” dilemma type includes an action whose ‘side effect’ results in saving the five people (e.g. smashing open a window to evacuate people from a fire and as a side effect killing one person with the falling glass). Each scenario was classified as either personal or impersonal and as intentional or unintentional based on designations assigned by Greene and colleagues (Greene et al., 2009). Thus, the four scenarios administered were of the following types: personal-intentional (Boxcar), personal-unintentional (Speedboat), impersonal-intentional (Rubble), and impersonal-unintentional (Burning). Participants were asked to respond to each of the four scenarios by indicating whether performing the sacrificial action in question (e.g. pushing a person off a footbridge in order to save the lives of five others) would be “acceptable” (they could circle either “Yes” or “No”). They were then additionally asked to indicate how acceptable or unacceptable the action would be, on a scale from 1 (“completely unacceptable”) to 9 (“completely acceptable”). Each dilemma scenario was presented on a computer screen in two slides, and participants read at their own pace, recording their responses on paper forms. An experimenter was present to carefully monitor the participants’ level of understanding during this process, and also offered to read scenarios aloud to the subject if this was requested (this occurred fewer than five times in present sample).
Aggregate variables were computed for each participant using their responses to the four dilemmas. A ‘personal’ variable was calculated by averaging responses given on the two personal dilemmas, and likewise values were calculated for impersonal, intentional and unintentional variables, each composed of an average of two responses.
Data Analysis
All analyses were conducted using SPSS 23. Descriptive characteristics of the sample were first calculated on all demographic, clinical, trauma, and moral decision measures. BD patients were compared with controls on all measures using Analysis of Variance (ANOVA) and χ2 tests as appropriate. Pearson and/or partial correlations were conducted to determine the relationships among the demographic and clinical measures and moral decision-making performance.
A series of ANOVAs were then conducted to identify main effects and interaction effects among measures of interest and moral dilemma task performance including the 5 measures from the moral dilemma task as dependent variables (ratings on each of 4 dilemma-types as well as an overall mean rating). Independent measures included diagnosis, sex, sex x diagnosis interaction, race, race x diagnosis interaction, race x sex x diagnosis interaction, age, premorbid IQ, education, mood ratings, and CTQ ratings as independent variables. All significance testing utilized a 95% confidence interval unless otherwise noted.
Results
Descriptive characteristics are presented in Table 1. Among BD patients, 85% met criteria for a diagnosis of BD I while the other 15% met for BD II. A history of psychotic features was reported in 50% of patients in the sample. Mean ratings of current mania and depression fell within the euthymic range, but patients still rated significantly higher on CARS-M (F=5.45, p<.01) and HRSD (F=24.80, p<.01) in comparison to HCs. Patients and HC subjects were well-matched on demographics, with the exception of race (χ2=4.54, p=.03).
Table 1:
Descriptive Characteristics of the Sample
| HC (N=27) Mean (SD) | BD Patient (N=62) Mean (SD) | Statistic (p) | Cohen’s d | |
|---|---|---|---|---|
| Age | 35.1 (10.8) | 38.3 (12.6) | F=1.31 (.26) | -- |
| Sex (F) | 16 (59%) | 38 (61%) | X2=.03 (.86) | -- |
| Race (White) | 5 (19%) | 26 (42%) | X2=4.54 (.03)* | -- |
| Premorbid IQ | 105.8 (13.0) | 104.1 (14.0) | F=0.30 (.59) | -- |
| Years of Education | 15.8 (1.8) | 14.8 (3.0) | F=2.35 (.13) | -- |
| CARS-M | 0.4 (1.0) | 2.7 (3.5) | F=5.45 (<.01)* | -- |
| HAM-D | 0.6 (1.2) | 7.3 (7.0) | F=24.4 (<.01)* | -- |
| Psychotic Features (%) | -- | 31 (50%) | -- | -- |
| Lifetime substance abuse (%) | -- | 9 (14.5%) | -- | -- |
| Lifetime anxiety disorder (%) | -- | 13 (21%) | -- | -- |
| Hospitalization Number | -- | 4.0 (4.5) | -- | -- |
| Suicide Attempts | -- | 0.9 (1.2) | -- | -- |
| Manic Number | -- | 10.3 (21.3) | -- | -- |
| Depressed Number | -- | 17.8 (27.8) | -- | -- |
| Med Number | -- | 2.0 (1.4) | -- | -- |
| Emotional Abuse | 7.4 (2.9) | 11.8 (5.4) | F=15.15 (<.01)* | -- |
| Emotional Abuse (Severe) | 2 (7%) | 24 (39%) | X2 =8.91 (<.01)* | -- |
| Physical Abuse | 7.1 (2.5) | 8.4 (4.5) | F=1.93 (.17) | -- |
| Physical Abuse (Severe) | 5 (19%) | 17 (27%) | X2=0.80 (.37) | -- |
| Sexual Abuse | 5.5 (1.7) | 7.6 (4.9) | F=5.0 (.03)* | -- |
| Sexual Abuse (Severe) | 2 (7%) | 17 (27%) | X2 =4.49 (.03)* | -- |
| Emotional Neglect | 9.0 (4.0) | 11.5 (4.9) | F=5.59 (.02)* | -- |
| Emotional Neglect (Severe) | 5 (19%) | 20 (32%) | X2 =1.76 (.18) | -- |
| Physical Neglect | 9.5 (0.9) | 10.3 (2.4) | F=2.32 (.13) | -- |
| Physical Neglect (Severe) | 9 (33%) | 29 (47%) | X2 =1.39 (.24) | -- |
| CTQ Total | 45.6 (8.6) | 58.2 (17.4) | F=12.7 (<.01)* | -- |
| Pers./Int. (Boxcar) (%Yes) | 9 (22%) | 28 (45%) | X2 =4.19 (.04)* | .44 |
| Impers./Int. (Speedboat) (%Yes) | 11 (41%) | 27 (44%) | X2 =.06 (.81) | .05 |
| Pers./Unint. (Rubble) (%Yes) | 14 (52%) | 37 (60%) | X2 =.47 (.49) | .15 |
| Impers./Unint. (Burning) (%Yes) | 20 (74%) | 44 (71%) | X2 =.09 (.76) | .06 |
| Personal Dilemmas | 4.1 (2.3) | 4.7 (2.4) | F=1.39 (.24) | .26 |
| Impersonal Dilemmas | 4.8 (2.1) | 4.9 (2.2) | F=0.07 (.80) | .05 |
| Intentional Dilemmas | 3.8 (2.3) | 4.4 (2.3) | F=1.49 (.23) | .26 |
| Unintentional Dilemmas | 5.1 (2.3) | 5.2 (2.3) | F=0.05 (.82) | .04 |
| Overall Dilemmas | 4.4 (2.1) | 4.8 (2.2) | F=.60 (.44) | .19 |
Note. Diagnostic Group differences were found on race, current mood symptoms, several subtypes of childhood trauma, and the Boxcar (Personal and Intentional) dilemma measured dichotomously (Y/N).
p<.05
Childhood trauma ratings were higher in the BD sample relative to HCs overall (CTQ Total F=12.70, p<.01), as well as in domains of Emotional Abuse (F=15.15, p<.01), Emotional Neglect (F=5.59, p=.02), and Sexual Abuse (F=5.00, p=.03). The CTQ domains of Physical Abuse and Physical Neglect showed non-significant differences between diagnostic groups (p=.17 and p=.13 respectively). Consistent with these ratings, BD patients were more likely than controls to have experienced severe trauma in several categories based upon CTQ cutoff scores (Table 1).
Effects of Diagnosis on Moral Decision-Making
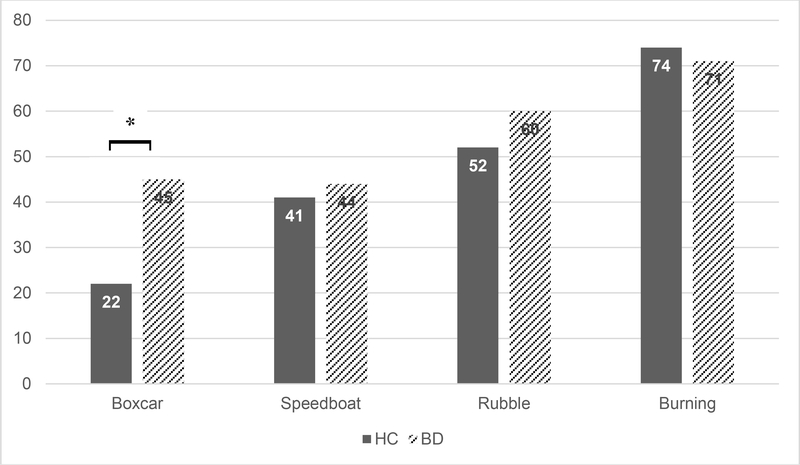
We first compared diagnostic groups on dichotomous (Yes vs No) responses to each of the four dilemmas using χ2. We found a significant difference between BD and HC on the “Boxcar” (personal/intentional) dilemma, such that BD patients were more likely to respond “Yes” endorsing utilitarian action (χ2=4.19, p=.04). None of the three other dilemmas (Speedboat, Rubble, and Burning) showed differences between BD and HC in dichotomous responses (all p > .48; Figure 1).
Figure 1. Percent who endorsed sacrificial action.
Note. Dichotomous responding by group in each scenario. BD patients responded “YES” (endorsed utilitarian sacrificial action) more frequently than did HCs (χ2=4.19, p=.04). No significant group differences were found between diagnostic groups on any of the other three scenarios.
Multivariate ANOVAs indicate no significant main effect of diagnosis on moral dilemma performance when evaluating dimensional ratings of acceptability (F=1.24; p=.30), regardless of dilemma type. The general pattern suggested that BD patients were slightly more utilitarian in their acceptability ratings but none reached even nominal significance (Personal dilemmas F=1.39, p=.24; Impersonal dilemmas F=.07, p=.80; Intentional dilemmas F=1.49, p=.23; Unintentional dilemmas F=.05, p=.82) and effect size estimates were small (range Cohen’s d=.05-.26).
Effects of Demographics on Moral Decision-Making
Partial correlations (controlling for diagnostic status) revealed no significant effects of age (all p-values > 0.15) or education (all p-values > 0.44) on any of the moral dilemma variables of interest. Likewise, there was no significant correlation between premorbid IQ and performance on any of the dilemmas (all p-values > 0.50). Multivariate ANOVA assessing the effects of race on moral dilemma performance revealed no significant main effect of race (F=0.24; p=0.87) and no significant interaction between race and diagnosis (F=0.46; p=0.71) on performance. Likewise, MANOVA assessing the effects of sex on each of the 5 moral decision variables revealed no overall main effect of sex (omnibus F=2.05; p=0.11); however, there was a main effect of sex on Personal dilemma choice (F=4.44, p=.04) and a trend-level effect on Intentional dilemma choice (F=3.81; p=.05), such that male participants found it more acceptable to cause harm when it requires the use of personal force or an intentional act than did female participants. There was no significant sex x diagnosis interaction overall (F=1.88; p=.14) or for any of the specific dilemma types (all p-values > .20).
Effects of Illness Characteristics on Moral Decision-Making
Symptom severity ratings in the BD patient group were not significantly correlated with performance on the dilemma task for any of the types of dilemmas (HRSD total, all p>0.47; CARS-M total all p>0.26). A significant positive relationship was observed in the BD sample between duration of illness and ratings on Intentional dilemmas (r=.282, p=.03) and on Personal dilemmas (r=.274; p=.03). This positive relationship suggests that the longer a person is ill, the more utilitarian they are in their acceptability ratings when the sacrificial action uses personal force or is carried out intentionally. This result remained significant after controlling for age.
MANOVA investigated whether history of psychotic features in BD played a role in moral decisions. A general pattern emerged indicating that those with a history of psychotic features (n=31) showed lower acceptability ratings (i.e. were less utilitarian) than those without psychotic features (n=31); this effect was significant in Overall average (F=4.59, p=.04), Impersonal (F=5.12, p=.03), and Unintentional (F=4.74, p=.03) dilemma ratings. The effect of psychosis history was only trend-level for Intentional (F=3.56 p=.06) and for Personal (F=3.28; p=.08) dilemmas. This suggests that BD patients with a history of psychotic features are less utilitarian than BD patients without psychosis. Other clinical variables including the number of prior episodes of either polarity, age of onset, number of psychotropic medications, and number of suicide attempts were not significantly associated with any of the moral dilemma measures (all p>.10).
Effects of Trauma History on Moral Decision-Making
Multivariate ANOVAs revealed a significant main effect of Physical Neglect (PN) on moral dilemma performance. PN was a significant predictor of Overall choice (F= 4.43; p=.04); Personal dilemma choice (F=4.51; p=0.04); and Unintentional dilemma choice (F= 4.96; p=0.03). Trend-level significant effects of PN were also noted on Intentional and Impersonal dilemma choices (Table 2) – indicative of a global effect of PN across dilemma types. These effects were relatively specific to a history of physical neglect versus other forms of maltreatment, with the exception of a trend-level effect of Emotional Neglect (F=3.16; p=0.08) on Intentional dilemma choice. There was no significant main effect of diagnosis, indicating an effect of prior trauma regardless of case status. Likewise, when trauma type x diagnosis terms were included in the models, all above results remained significant and none of these interaction terms were significant (all p-values > .09).
Table 2.
ANOVA results.
| OVERALL | PERSONAL | UNINTENTIONAL | IMPERSONAL | INTENTIONAL | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| F | p | F | p | F | p | F | p | F | p | |
| Emotional Abuse | .88 | .35 | 1.27 | .27 | .29 | .59 | .44 | .51 | 1.53 | .22 |
| Physical Abuse | .48 | .49 | .17 | .68 | .95 | .33 | .85 | .36 | .11 | .74 |
| Sexual Abuse | .10 | .76 | .18 | .68 | .61 | .44 | .03 | .86 | .04 | .85 |
| Emotional Neglect | 1.22 | .27 | 2.14 | .15 | .10 | .75 | .40 | .53 | 3.16 | .08 |
| Physical Neglect | 4.43* | .04 | 4.51* | .04 | 4.96* | .03 | 3.56 | .06 | 3.04 | .09 |
| HRSD | .18 | .67 | .52 | .47 | .09 | .77 | .01 | .94 | .26 | .62 |
| CARS-M | 1.08 | .30 | 1.31 | .26 | 2.21 | .14 | .69 | .41 | .22 | .64 |
| Diagnostic Group | .001 | .97 | .07 | .80 | .16 | .69 | .11 | .74 | .11 | .74 |
| Premorbid IQ | .41 | .52 | .07 | .80 | 1.07 | .31 | .95 | .33 | .03 | .87 |
| AGE | 1.67 | .20 | 2.35 | .13 | 1.77 | .19 | .85 | .36 | 1.23 | .27 |
| Education | .15 | .70 | .13 | .72 | .15 | .70 | .14 | .71 | .12 | .73 |
| Race | .14 | .71 | .21 | .65 | .09 | .77 | .06 | .80 | .17 | .69 |
| Sex | 1.10 | .30 | 1.49 | .23 | .34 | .56 | .60 | .44 | 1.98 | .16 |
| Diagnosis by Race Int. | .30 | .58 | .16 | .69 | .37 | .54 | .43 | .51 | .18 | .67 |
| Diagnosis by Sex Int. | .13 | .72 | .62 | .43 | .02 | .90 | .01 | .92 | .69 | .41 |
| Race by Sex Int. | .43 | .51 | .42 | .52 | .17 | .68 | .36 | .55 | .69 | .41 |
| Diagnosis by Race by Sex Int. | .12 | .730 | .16 | .69 | .30 | .59 | .07 | .79 | .01 | .91 |
Note.
indicates p<.05
Discussion
The present study compared affectively-stable patients with BD and healthy controls on moral decision-making task performance. We found a significant main effect of diagnosis when comparing patients to controls, using a forced choice (yes/no) measure, that was specific to the “Boxcar” dilemma (characterized by sacrificial action that is both personal and intentional), with patients endorsing a higher rate of utilitarian action in this dilemma. However, there were no significant main effects of diagnostic group on any of the moral dilemma types when examining continuous (1–9) acceptability ratings. The fact that there were group differences that were noted only on the Boxcar dilemma is likely due to the nature of that dilemma (in which endorsement of sacrificial action may require the strongest identification with a utilitarian style). Indeed, past work has reported that effects of intentionality and personal force in moral dilemma scenarios may be strongest when presented together (Greene et al., 2009).
This result extends past work, which found differences between only acutely manic (not between euthymic) patients and controls (Kim et al., 2015), to suggest that some differences may be present even during affective remission (though some appear not to be in our sample, as well). It is possible that this divergence from the Kim et al. (2015) findings is a result of statistical power: that is, it may be that our considerably larger sample was better able to detect the subtle effect that was not seen in the smaller sample. Additionally, the finding of a diagnostic difference aligns with past work which used different methodologies to assess moral cognition and found a number of behavioral and neural differences between BD patients and controls (Epa et al., 2014; Epa & Dudek, 2015; Radaelli et al., 2013).
We found a significant main effect of sex such that male participants reported greater acceptability of using personal force to achieve the morally desirable outcome (saving the five people) than did female participants. This effect was noted regardless of diagnostic status. Sex differences in moral decision-making have been variously interpreted in the past as evidence for different theories. For example, Rota and colleagues (2016) concluded that the difference can be attributed simply to a higher ‘disposition toward action’ in men versus women. In contrast, a recent meta-analytic process dissociation analysis showed that sex differences on moral decision-making tasks were best explained by differing affective responses to harm (with females being more sensitive to harm than males), and not by cognitive assessments of outcomes (Friesdorf, Conway, & Gawronski, 2015). This latter explanation outlines why females may tend to be more deontological in their decision-making, as this approach is thought to be more heavily driven by the emotional components of the decision. This is indeed the pattern that we see in our participants.
We also found that certain illness features influenced performance on the moral dilemma task in our BD patients, namely duration of illness and history of psychosis. The pattern of association suggested that a longer duration of illness is specifically related to higher ratings of acceptability (more utilitarian) when faced with dilemmas that require intentional action or the use of personal force. This result remained significant even when controlling for age. In contrast, a history of psychotic features was associated with a more deontological approach when faced with dilemmas of all types. As these relationships are only correlational, we cannot say if the illness caused changes in the way moral decisions are made or if a tendency toward a certain style (utilitarian vs. deontological) predated the onset of the illness.
Perhaps most interestingly, our data suggest that traumatic experiences during childhood may influence moral decision-making in adult life. We report an important influence of childhood trauma on performance; in particular, higher levels of physical neglect (PN) were associated with greater acceptability in causing harm to utilitarian ends when the action involved personal force or when it involved unintentional action, a pattern which was generally consistent across all four dilemma types.
Explaining effects of physical neglect with dual process theory
In explaining the observed effects of trauma on moral decision-making in our sample, it is useful to employ the commonly-used explanatory framework for decision-making in moral dilemmas noted earlier, known as the “dual process theory” (Greene et al., 2004). DPT posits that utilitarian decisions are characterized primarily by deliberative, controlled cognitive processes, while deontological decisions are characterized primarily by emotional processes activated in response to the prospect of engaging in the harmful sacrificial action. Some empirical evidence in support of DPT has shown that greater experiences of negative emotional arousal are associated with deontological bias (Szekely & Miu, 2015). One explanation for the utilitarian bias in the portion of our sample that experienced severe physical neglect could therefore be that this bias is compensatory. That is, there may be a decreased reliance on affective systems in subjects who experienced neglect, which leads to a tendency to override emotional deontological impulses, or even a failure to produce these impulses in the first place. Decisions would then instead be driven by other competing processes which focus on cognitive assessment of outcomes, leading to greater frequency of utilitarian choice.
Our findings present an inconsistency (at least prima facie) with one past study connecting trauma and morality (in PTSD) which found that childhood trauma can lead to lower likelihood of making utilitarian moral decisions (Nazarov et al., 2016). These authors found that women with PTSD due to prolonged childhood trauma (n=28) were less likely than controls to endorse utilitarian action, a pattern that was exclusively noted on personal dilemmas. The PTSD patients additionally reported higher levels of guilt and shame as consequences of engaging in the sacrificial action relative to the control group. Direct comparison with this study’s findings using our sample is difficult for several reasons even beyond the differences in diagnostic focus: Nazarov and colleagues did not report differential correlations with moral decisions as a function of different types of childhood traumatic experiences (such as physical neglect and emotional neglect); they did not quantify the differences between intentional and unintentional utilitarian harms as we do in the present study; and finally, their sample consisted solely of women as opposed to an equal balance of both sexes. Diagnostically, although our sample reported high rates of childhood trauma, only 6 BD patients reported a history of PTSD. We are thus unable to assess whether BD patients with full syndromal PTSD might respond more similarly to the subjects noted in (Nazarov et al., 2016).
It is tempting to speculate that the utilitarian approach endorsed by our BD subjects with trauma histories may act as (or be associated with) a protective factor against the development of full-blown PTSD in the face of significant traumatic experiences. Indeed, one signature symptom of PTSD is that patients tend to experience heightened emotional arousal and reactivity (APA, 2013). As noted in the discussion of DPT, deontological choice on dilemmas (which was the observed pattern in the PTSD sample) is often associated with increased negative emotional arousal and inability to step outside the emotionally aversive prospect of engaging in the sacrificial action. It may then be the case that the traumatized group in our study has an increased ability to exert control to remove attention from negative emotional stimuli, resulting in a successful cognitive overcoming of the aversion associated with engaging in sacrificial action. To further test this hypothesis, additional work would need to be done to directly compare patients with trauma histories that did develop PTSD against those who experienced similar trauma but were ‗resilient’ to developing PTSD.
Limitations & future work
A variety of factors limit the strength of conclusions which may be drawn from the present findings. First, while our sample was larger than those reported in past work, it was still relatively small. Among the primary measures administered in the study, the Childhood Trauma Questionnaire is limited by its retrospective nature as well as by the fact that traumatic experiences are self-reported in this measure, as opposed to being measured by a clinician or in an objective and potentially more reliable way. The moral dilemmas data is limited by the small number of trials (only four dilemmas were administered to each participant), while past work has typically included 8 or more, with at least two of each type of scenario.
Another limitation is number of variables included in some analyses which, based on our sample size, was relatively high. We elected to err on this side in our analyses as some of these variables are not independent from one another, and the purpose of the analyses was in part to generate hypotheses in this still poorly-circumscribed area of inquiry. However, this practice serves to decrease slightly the confidence we might place in positive findings.
Some have expressed skepticism of the degree to which decision-making in standard sacrificial moral dilemmas may be generalized to real-world situations and thus provide useful practical insight (Bauman, McGraw, Bartels, & Warren, 2014; Bostyn, Sevenhant, & Roets, 2018; Kahane et al., 2018). Nevertheless, moral decisions themselves represent an important category of choices encountered in daily social living (e.g. whether or not to give to charity, how to treat coworkers, family members, strangers, etc.), and sacrificial moral dilemmas provide a clean and easily-manipulated measurement technique to observe granular differences within the discrete cognitive processes responsible for this type of decision-making. In the context of clinical populations, measurement of moral cognition could however be clearly improved through the use of more ecologically-valid stimuli, perhaps containing explicitly clinical or disease-specific content.
In major affective disorders such as BD, it is especially important to further our understanding of moral decision-making due to the centrality of affective processes in moral judgment and therefore the possibility of moral decisions exhibiting modulations specific to affective dysregulation (Kim et al., 2015). In addition to categorical illness-specific differences in BD versus healthy controls, our results suggest significant effects of several illness features including severity of course of illness and childhood trauma on an important variety of affectively-laden social decision making. It remains to be seen whether this effect can have any noteworthy impact on real-world social functioning, and this should be a subject of future work, which should systematically investigate relationships between moral cognition and measures of function.
Despite these limitations, this study constitutes important preliminary evidence that the experience of habitual affective disruption occurring in BD—especially in the presence of comorbid childhood trauma—may exert a modulating force on the way patients process moral stimuli. Such a modulation, if truly present, could have numerous implications for the lives of patients, as moral evaluations and decisions pervade much of everyday life. In addition, a person’s morality has been shown to be at the center of their essential identity (Strohminger & Nichols, 2014)—that is, understanding the moral functioning of a person or group may be essential to understanding them fully and as they understand themselves.
Further work could also benefit from implementing measures that can give insight into neural correlates of the affective processes which we know to be affected in the illness as well as via trauma. For example, past work has already shown that the ventromedial prefrontal cortex (VMPFC) is one particularly important area to moral decision-making processes (Decety and Wheatley, 2015), and that the same region shows modulated activity during episodes of dysregulated mood (Kim et al., 2015). VMPFC and other areas implicated in both moral decision-making and BD illness (including those identified by Radaelli et al., 2013) are thus important targets for future investigation.
Future work attempting to clarify the precise nature of the connection(s) between childhood trauma and moral decision-making ought likely to focus on specific effects of physical and emotional neglect. Due to our divergent findings from past work in PTSD, important questions remain unanswered regarding the way (or ways) in which trauma may exert influence on moral decision-making; we have speculated here that categorical diagnostic differences between subclinical trauma (in BD) and PTSD on decision-making may point to important clinical insights. The present findings may be an important clue supporting the growing body of evidence attempting to explain the factors that mitigate deleterious effects of childhood trauma. For example, a recent nationally-representative study reported that social support is one such factor (Chiang, Chen, & Miller, 2018), and the present evidence may suggest that some factor associated with moral utilitarian decision-making could be another.
Finally, it may also be prudent to explore trauma as a possible mediating factor in work seeking to investigate moral decision making in clinical populations where a high co-occurrence of trauma histories have been noted. For example, in disorders such as psychopathy (where substantial work in this area has already been conducted), it could be the case that group differences on moral decision-making measures are confounded by mediating effects of childhood maltreatment.
HIGHLIGHTS.
Euthymic bipolar patients endorse utilitarian action more frequently than healthy controls on a moral dilemma that is personal and intentional but not on other types
Childhood trauma seems to play an important role in moral decision-making across groups
It is speculated that utilitarian tendencies may protect from PTSD
Acknowledgments
The authors wish to thank Joshua Greene, Julia Christensen and Antoni Gomila for helpful comments in the preliminary stages of the work that is reported here.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Aas M, Henry C, Andreassen OA, Bellivier F, Melle I, & Etain B (2016). The role of childhood trauma in bipolar disorders. International Journal of Bipolar Disorders, 4(1), 2 https://doi.org/10.1186/s40345-015-0042-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Altman EG, Hedeker DR, Janicak PG, Peterson JL, & Davis JM (1994). The clinician-administered rating scale for mania (CARS-M): Development, reliability, and validity. Biological Psychiatry, 36(2), 124–134. https://doi.org/10.1016/0006-3223(94)91193-2 [DOI] [PubMed] [Google Scholar]
- APA, A. P. A. (2013). Diagnostic and Statistical Manual of Mental Disorders (DSM-5®). American Psychiatric Pub. [DOI] [PubMed] [Google Scholar]
- Bauman CW, McGraw AP, Bartels DM, & Warren C (2014). Revisiting External Validity: Concerns about Trolley Problems and Other Sacrificial Dilemmas in Moral Psychology. Social and Personality Psychology Compass, 8(9), 536–554. https://doi.org/10.1111/spc3.12131 [Google Scholar]
- Bernstein DP, Fink L, Handelsman L, Foote J, Lovejoy M, Wenzel K, … Ruggiero J (1994). Initial reliability and validity of a new retrospective measure of child abuse and neglect. The American Journal of Psychiatry, 151(8), 1132–1136. https://doi.org/10.1176/ajp.151.8.1132 [DOI] [PubMed] [Google Scholar]
- Birn RM, Roeber BJ, & Pollak SD (2017). Early childhood stress exposure, reward pathways, and adult decision making. Proceedings of the National Academy of Sciences, 201708791. https://doi.org/10.1073/pnas.1708791114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bland VJ, Lambie I, & Best C (2018). Does childhood neglect contribute to violent behavior in adulthood? A review of possible links. Clinical Psychology Review, 60, 126–135. https://doi.org/10.1016/j.cpr.2018.02.001 [DOI] [PubMed] [Google Scholar]
- Bostyn DH, Sevenhant S, & Roets A (2018). Of Mice, Men, and Trolleys: Hypothetical Judgment Versus Real-Life Behavior in Trolley-Style Moral Dilemmas. Psychological Science, 0956797617752640. https://doi.org/10.1177/0956797617752640 [DOI] [PubMed] [Google Scholar]
- Brambilla M, Sacchi S, Pagliaro S, & Ellemers N (2013). Morality and intergroup relations: Threats to safety and group image predict the desire to interact with outgroup and ingroup members. Journal of Experimental Social Psychology, 49(5), 811–821. https://doi.org/10.1016/j.jesp.2013.04.005 [Google Scholar]
- Burdick KE, Russo M, Frangou S, Mahon K, Braga RJ, Shanahan M, & Malhotra AK (2014). Empirical evidence for discrete neurocognitive subgroups in bipolar disorder: clinical implications. Psychological Medicine, 44(14), 3083–3096. https://doi.org/10.1017/S0033291714000439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiang JJ, Chen E, & Miller GE (2018). Midlife self-reported social support as a buffer against premature mortality risks associated with childhood abuse. Nature Human Behaviour, 2(4), 261–268. https://doi.org/10.1038/s41562-018-0316-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Decety J, Michalska KJ, & Kinzler KD (2011). The Developmental Neuroscience of Moral Sensitivity, The Developmental Neuroscience of Moral Sensitivity. Emotion Review, 3(3), 305–307. https://doi.org/10.1177/1754073911402373 [Google Scholar]
- Decety J, & Wheatley T (2015). The Moral Brain: A Multidisciplinary Perspective. MIT Press. [Google Scholar]
- Delgado MR, Frank RH, & Phelps EA (2005). Perceptions of moral character modulate the neural systems of reward during the trust game. Nature Neuroscience, 8(11), 1611–1618. https://doi.org/10.1038/nn1575 [DOI] [PubMed] [Google Scholar]
- England-Mason G, Khoury J, Atkinson L, Hall GB, & Gonzalez A (2018). Attentional avoidance of emotional stimuli in postpartum women with childhood history of maltreatment and difficulties with emotion regulation. Emotion (Washington, D.C.), 18(3), 424–438. https://doi.org/10.1037/emo0000372 [DOI] [PubMed] [Google Scholar]
- Epa R, Czyzowska N, Dudek D, Siwek M, & Gierowski JK (2014). Profile of moral reasoning in persons with bipolar affective disorder. Psychiatr. Pol, 48(3), 489–502. [PubMed] [Google Scholar]
- Epa R, & Dudek D (2015). Theory of mind, empathy and moral emotions in patients with affective disorders. Archives of Psychiatry and Psychotherapy, 17(2), 49–56. https://doi.org/10.12740/APP/44569 [Google Scholar]
- First MB, Williams JBW, Karg RS, & Spitzer RL (2015). Structured clinical interview for DSM-5—Research version (SCID-5 for DSM-5, research version; SCID-5-RV). Arlington, VA: American Psychiatric Association. [Google Scholar]
- Friesdorf R, Conway P, & Gawronski B (2015). Gender Differences in Responses to Moral Dilemmas: A Process Dissociation Analysis. Personality and Social Psychology Bulletin, 41(5), 696–713. https://doi.org/10.1177/0146167215575731 [DOI] [PubMed] [Google Scholar]
- Greene JD, Cushman FA, Stewart LE, Lowenberg K, Nystrom LE, & Cohen JD (2009). Pushing moral buttons: The interaction between personal force and intention in moral judgment. Cognition, 111(3), 364–371. https://doi.org/10.1016/j.cognition.2009.02.001 [DOI] [PubMed] [Google Scholar]
- Greene JD, Nystrom LE, Engell AD, Darley JM, & Cohen JD (2004). The neural bases of cognitive conflict and control in moral judgment. Neuron, 44(2), 389–400. [DOI] [PubMed] [Google Scholar]
- Hamilton M (1960). A RATING SCALE FOR DEPRESSION. Journal of Neurology, Neurosurgery, and Psychiatry, 23(1), 56–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiménez E, Solé B, Arias B, Mitjans M, Varo C, Reinares M, … Benabarre A (2017). Impact of childhood trauma on cognitive profile in bipolar disorder. Bipolar Disorders, 19(5), 363–374. https://doi.org/10.1111/bdi.12514 [DOI] [PubMed] [Google Scholar]
- Kahane G, Everett JAC, Earp BD, Caviola L, Faber NS, Crockett MJ, & Savulescu J (2018). Beyond sacrificial harm: A two-dimensional model of utilitarian psychology. Psychological Review, 125(2), 131–164. https://doi.org/10.1037/rev0000093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim SH, Kim TY, Ryu V, Ha RY, Lee SJ, Ha K, & Cho H-S (2015). Manic patients exhibit more utilitarian moral judgments in comparison with euthymic bipolar and healthy persons. Comprehensive Psychiatry, 58, 37–44. https://doi.org/10.1016/j.comppsych.2014.12.010 [DOI] [PubMed] [Google Scholar]
- Krautheim JT, Straube B, Dannlowski U, Pyka M, Schneider-Hassloff H, Drexler R, … Kircher T (2018). Outgroup emotion processing in the vACC is modulated by childhood trauma and CACNA1C risk variant. Social Cognitive and Affective Neuroscience, 13(3), 341–348. https://doi.org/10.1093/scan/nsy004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nazarov A, Walaszczyk V, Frewen P, Oremus C, Lanius R, & McKinnon MC (2016). Moral reasoning in women with posttraumatic stress disorder related to childhood abuse. European Journal of Psychotraumatology, 7(1), 31028 https://doi.org/10.3402/ejpt.v7.31028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radaelli D, Dallaspezia S, Poletti S, Smeraldi E, Falini A, Colombo C, & Benedetti F (2013). Different Neural Responses to a Moral Valence Decision Task in Unipolar and Bipolar Depression. ISRN Psychiatry, 2013 https://doi.org/10.1155/2013/568617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rota G, Palumbo S, Lattanzi N, Manfrinati A, Sarlo M, Lotto L, … Pellegrini S (2016). Harm aversion explains utilitarian choices in moral decision-making in males but not in females. Archives Italiennes de Biologie. A Journal of Neuroscience, 154(2/3), 50–58. [DOI] [PubMed] [Google Scholar]
- Russo M, Mahon K, Shanahan M, Solon C, Ramjas E, Turpin J, & E. Burdick K (2015). The association between childhood trauma and facial emotion recognition in adults with bipolar disorder. Psychiatry Research, 229(3), 771–776. https://doi.org/10.1016/j.psychres.2015.08.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spearing MK, Post RM, Leverich GS, Brandt D, & Nolen W (1997). Modification of the Clinical Global Impressions (CGI) scale for use in bipolar illness (BP): the CGI-BP. Psychiatry Research, 73(3), 159–171. https://doi.org/10.1016/S0165-1781(97)00123-6 [DOI] [PubMed] [Google Scholar]
- Strohminger N, & Nichols S (2014). The essential moral self. Cognition, 131(1), 159–171. [DOI] [PubMed] [Google Scholar]
- Szekely RD, & Miu AC (2015). Incidental emotions in moral dilemmas: The influence of emotion regulation. Cognition and Emotion, 29(1), 64–75. https://doi.org/10.1080/02699931.2014.895300 [DOI] [PubMed] [Google Scholar]
- Wilkinson GS (1993). WRAT-3: Wide range achievement test administration manual. Wide Range, Incorporated. [Google Scholar]