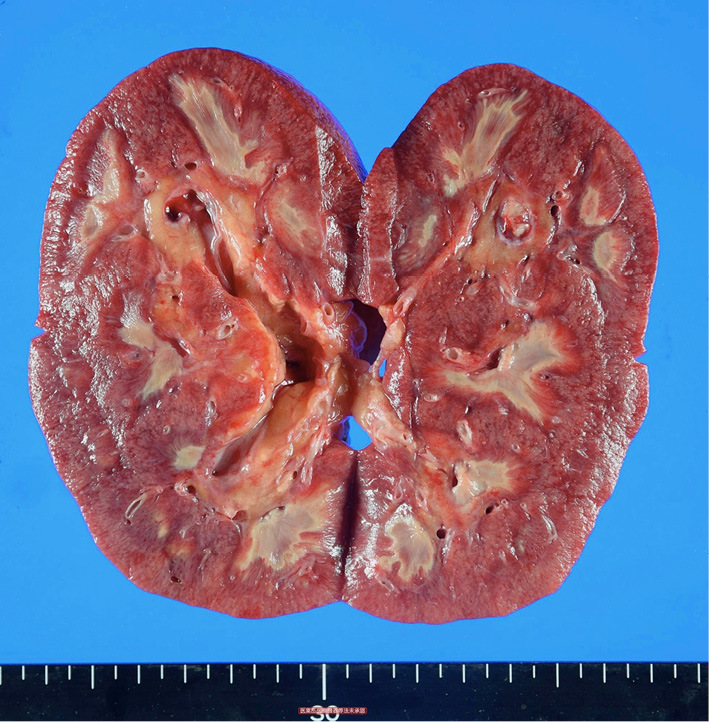
An 85-year-old man with a 7-year history of type 2 diabetes who had no obvious diabetic complications presented with a fever and malaise. He had bilateral costovertebral angle tenderness. Laboratory data showed renal dysfunction. Computed tomography showed bilateral renal enlargement but no obstructive findings. Escherichia coli was detected from blood cultures and urine. We diagnosed the patient with acute pyelonephritis and treated him with antibiotics. However, his condition worsened and he ultimately died. A pathological autopsy showed bilateral renal papillary necrosis (Picture). Renal papillary necrosis is typically thought to be caused by diabetes mellitus and urinary tract infection. The renal papillae are considered to be anatomically vulnerable to ischemic changes, like vascular disorder with diabetes or interstitial edema associated with infection (1). There have been some cases in which rapid deterioration occured (2). In case of acute pyelonephritis with an impaired renal function in patients with diabetes, physicians should consider the possibility of renal papillary necrosis.
Picture.
The authors state that they have no Conflict of Interest (COI).
References
- 1. Jung DC, Kim SH, Jung SI, Hwang SI, Kim SH. Renal papillary necrosis: review and comparison of findings at multi-detector row CT and intravenous urography. Radiographics 26: 1827-1836, 2006. [DOI] [PubMed] [Google Scholar]
- 2. Abdulhayoglu S, Marble A. Necrotizing Renal Papillitis (Papillary Necrosis) in diabetes mellitus. Am J Med Sci 248: 623-632, 1964. [DOI] [PubMed] [Google Scholar]


