Abstract
Purpose
To report a rare case of solitary eyelid schwannoma in a Thai child without clinical manifestation of neurofibromatosis.
Observations
A 9-year-old Thai boy presented with an isolated painless mass on the left lower eyelid. The mass had gradually grown for 2 years. He denied a history of trauma or previous eyelid surgery. A clinical examination revealed no clinical features of neurofibromatosis. The provisional diagnosis at that time was a sebaceous cyst. However, excisional biopsy showed an encapsulated tumor characterized by interlaced spindle-celled fasciculi with focal palisading of nuclei arranging in Antoni A and Antoni B patterns. The immunocytochemistry was strongly positive for S-100 protein reaction. The diagnosis of schwannoma was made, with no recurrence at.
Conclusions and importance
Schwannoma of the eyelid is extremely rare in children, accounting for less than 0.1% of all eyelid tumors. Combined with clinical features, histopathologic and immunohistochemical analyses emphasize the disease entities. These findings may extend the knowledge on experiences of schwannoma in children.
Keywords: Childhood, Eyelid tumor, Schwannoma, Antoni A and B, S-100 protein reaction
1. Introduction
Schwannoma is uncommonly seen in ocular tissue. The eyelid is an extremely rare location for schwannoma, especially in children. The purpose of this article is to report a rare case of an isolated eyelid schwannoma in a Thai child.
2. Case report
A 9-year-old Thai boy presented at the hospital in February 2016 with a painless solitary mass on his left lower eyelid. The patient reported a two-year history of a slowly growing mass. The tumor produced no discharge or redness. He denied a history of previous trauma or surgical excision. The child was otherwise normal, with no clinical finding suggestive of systemic tumor. He had no family history of neurofibromatosis. On examination, there was a round, non-erythematous mass located at the lateral third of lower eyelid margin. The mass was firm, smooth surfaced, and non-tender on palpation. The lesion laid superficially and was movable under the skin. The approximate size on examination was 1 cm in diameter, with minimally visible protrusion from the skin. Other aspects of the ophthalmic exam were within normal limits. The presumptive diagnosis at that time was sebaceous cyst. An excision biopsy was performed via anterior dissection in the skin under local anesthesia. Gross histopathological examination showed well encapsulated, smooth consistency, tan tissue. The mass measured 0.8 × 0.5 × 0.5 cm. Microscopic section revealed a well defined mass with a thin capsule consisting of the spindle to oval nuclei with eosinophilic fibrillar cytoplasm. The histology also showed a dense nuclear palisading area (Antoni A pattern) alternated with a loose hyalinized and fibrillary area (Antoni B pattern). A mitotic figure was not seen. Hyalinized vascular walls were noted. A nerve of origin was not discernible. The immunocytochemistry for S100 protein showed a strongly positive reaction (Fig. 1). The final diagnosis was a benign schwannoma of the eyelid. The post-operative wound healed completely without any postoperative complication. No recurrence was observed at 18-months follow up.
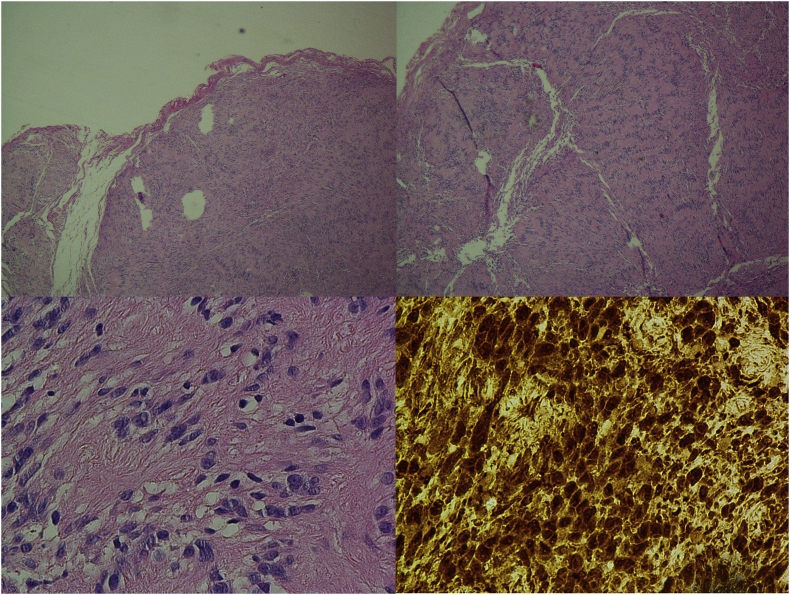
Fig. 1.
Photomicrographs of an Eyelid Schwannoma (Top left) Low magnification photomicrograph showing encapsulated spindle cell tumor (hematoxylin-eosin); (Top right) Low magnification photomicrograph showing benign schwannoma. Antoni A tissue is dense cellular with a hint of nuclear palisading. Antoni B tissue is loose, less cellular area with myxoid change. (hematoxylin-eosin); (Bottom left) High magnification photomicrograph showing monomorphic spindle-shaped Schwann cells with poorly defined eosinophilic cytoplasm and basophilic nuclei. (hematoxylin-eosin); (Bottom right) High magnification photograph showing a positive reaction to S-100 protein (immunohistochemistry for S-100).
3. Discussion
Schwannomas are Schwann-cell tumors that arise from peripheral or cranial nerves. Solitary lesions can occur sporadically; multiple schwannomas can be associated with neurofibromatosis 2. Schwannoma that involves the eye most commonly develops in the orbit, accounting for around 1% of orbital tumors.1 Less frequent involvement has been found in uveal tract, conjunctiva, and sclera.
Eyelid schwannoma is extremely rare. Siddiqui et al. presented 5 cases of eyelid schwannoma. Four out of the five cases were in late adulthood (age 53–63). One case was in young adulthood (age 19).2 Lopez-Tizon et al. reported another 2 adult cases, which they noted as the only 2 cases of schwannoma out of 2400 eyelid neoplasms observed in their 11 years of experience (1995–2005), indicating a prevalence of 0.1% among eyelid tumors.1
Eyelid schwannomas in children are rarer than in adults. Only 3 cases have been published so far. None were from Southeast Asian region. The clinical presentations of all 3 cases and our current case are summarized in Table 1. The diagnosis was confirmed with a strong reactivity to S100 protein, which is considered a hallmark feature of schwannomas.
Table 1.
Summary of published cases of eyelid schwannomas in children.
| Author | Year | Age (years) | Sex | Country of Publish | Laterality | Loca-tion | Duration of symptom | Size of tumor | Associated NF/TS |
Pathology | Recurrent |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Shields et al.3 | 1994 | 8 | M | U.S. | Right | Upper eyelid | 2 year | 9 × 7 × 6 mm | No | Antoni A | N/A |
| Onaran et al.4 | 2008 | 13 | F | Turkey | Right | Lower eyelid | 2 years | 20 mm | No | Antoni A S-100, vimentin positive |
No recurrence 12 months of follow-up |
| Kimura et al.5 | 2010 | 8 | M | Japan | Left | Upper eyelid | 3 years | 10 × 5 × 4 mm | No | Antoni A (predominated) + Antoni B S-100 positive Alpha-smooth muscle actin + desmin negative |
No recurrence 18 moths of follow-up |
| Present report | 2016 | 9 | M | Thailand | Left | Lower eyelid | 2 years | 8 × 5 × 5 mm. | No | Antoni A + Antoni B S-100 positive |
No recurrence 18 months of follow-up |
Abbreviations: F, female; M, male; NF, Neurofibromatosis; TS, Tuberous sclerosis.
The histological finding in our case also followed a previous pattern occurring on eyelid margins reported by Stagner and Jakobiec in 2016.6 It is important to note that, in eyelid peripheral nerve sheath tumors, S100 positivity in immunostaining can be demonstrated, not only in schwannoma, but also in solitary circumscribed neuroma (SCN), another eyelid tumor that has been reported in adults. Schwannoma and SCN share the common characteristic of densely packed spindle-cell and S-100 positivity. However, the SCN histologically presents a more prominent axon, less palisading, and insubstantial capsule; the schwannoma, as in this present report, has a distinct pattern of fascicular cells alternating myxoid areas in conjunction with a complete, thick, and hyalinized capsule.6 Immunostaining for neurofilament antibody and immunostaining for perineurial cells (i.e., epithelial membrane antigen staining or glucose transporter-1 staining) might aid in differentiating these two eyelid nerve sheath tumors.6
Since eyelid schwannomas are rare and without characteristic clinical features, definitive diagnosis depends on histopathology. Fortunately, schwannomas rarely undergo malignant transformation.
4. Conclusions
Schwannoma of the eyelid in children is extremely rare, accounting for less than 0.1% of all eyelid tumors. Combined with clinical features, histopathologic and immunohistochemical analysis emphasize the disease entities. These findings may extend the knowledge on experiences of schwannoma in children.
Patient consent
The patient's assent for publication was obtained from a patient. Written informed consent was also obtained from the parents.
Acknowledgments and disclosures
Funding
No funding support.
Conflicts of interest
The following authors have no financial disclosure.
Authorship
All authors attest that they meet the current ICMJE criteria for Authorship.
Acknowledgements
Phanchanut Mahantassannapong; Pathologist.
References
- 1.Lopez-Tizon E., Mencia-Gutierrez E., Gutierrez-Diaz E., Ricoy J.R. Schwannoma of the eyelid: report of two cases. Dermatol Online J. 2007;13(2):12. [PubMed] [Google Scholar]
- 2.Siddiqui M.A., Leslie T., Scott C., Mackenzie J. Eyelid schwannoma in a male adult. Clin Exp Ophthalmol. 2005;33(4):412–413. doi: 10.1111/j.1442-9071.2005.01035.x. [DOI] [PubMed] [Google Scholar]
- 3.Shields J.A., Kiratli H., Shields C.L., Eagle R.C., Jr., Luo S. Schwannoma of the eyelid in a child. J Pediatr Ophthalmol Strabismus. 1994;31(5):332–333. doi: 10.3928/0191-3913-19940901-15. [DOI] [PubMed] [Google Scholar]
- 4.Onaran Z., Ornek K., Yilmazbas P., Bozdogan O. Schwannoma of the lower eyelid in a 13-year-old girl. Ophthalmic Plast Reconstr Surg. 2009;25(1):50–52. doi: 10.1097/IOP.0b013e3181936826. [DOI] [PubMed] [Google Scholar]
- 5.Kimura K., Tanaka T., Edagawa H., Goto H. A case of eyelid schwannoma in a child. Jpn J Ophthalmol. 2010;54(6):635–636. doi: 10.1007/s10384-010-0880-3. [DOI] [PubMed] [Google Scholar]
- 6.Stagner A.M., Jakobiec F.A. Peripheral nerve sheath tumors of the eyelid dermis: a clinicopathologic and immunohistochemical analysis. Ophthalmic Plast Reconstr Surg. 2016;32(1):40–45. doi: 10.1097/IOP.0000000000000424. [DOI] [PubMed] [Google Scholar]